Abstract
Introduction
Juvenile idiopathic arthritis (JIA) may cause damage to the temporomandibular joint (TMJ). In oligoarticular forms of JIA, TMJ involvement is often asymptomatic and consequently overlooked. The aim of this study was to evaluate the presence of TMJ joint effusion (JE) by ultrasonography (US) in patients with early arthritis.
Materials and methods
We examined 68 children (57 girls, 11 boys, age range 9.1–16.0 years, mean age 11.0 years) recently diagnosed with JIA. None had received any specific treatment for inflammation. Symptomatic TMJ involvement was diagnosed when one or more of the following were present: 1) recurrent pain (spontaneous or on movement of the jaw); 2) crepitation; 3) feeling of stiffness or fatigue of the jaw; 4) intermittent locking. US of the TMJ was performed in static and dynamic phases with a General Electric LOGIQ7 scanner and a linear transducer (8.5 MHz) positioned along the axis of the mandibular ramus. JE was diagnosed when the joint capsule was ≥1.5 mm thick.
Results
Forty-six out (68%) of 68 children had US evidence of TMJ effusions (bilateral in 16 [35%] cases), but only 2/46 were symptomatic.
Conclusions
These data suggest that children with early stage oligoarticular JIA children are likely to have inflammation of the TMJs even in the absence of symptoms. US is a simple-to-use, noninvasive, radiation-free tool that can provide useful information in the assessment and follow-up of TMJ involvement in children and young adults with JIA.
Keywords: Ultrasonography, TMJ, Oligo-articular onset, Early JIA
Sommario
Introduzione
L'artrite Idiopatica giovanile (AIG) determina alterazioni a carico della testa condilare dell'articolazione temporomandibolare (ATM). Nell'esordio oligo-articolare (OA) l'interessamento dell'ATM viene spesso trascurato perchè può essere asintomatico. Lo scopo di questo studio è quello di valutare la presenza di versamento intrarticolare (V) dell'ATM, mediante esame ecografico (US), nelle fasi precoci di malattia.
Materiale e metodi
Sono stati studiati 68 bambini (57 bambine e 11 bambini, di età compresa tra 9,1 e 16, anni, età media: 11,02 ± 4,2 mesi) con AIG ad esordio OA. I pazienti (pz) erano sintomatici quando uno dei quattro sintomi seguenti era presente: 1) dolore ricorrente (a riposo o durante il movimento di apertura della bocca); 2) presenza di scrosci articolari; 3) presenza di limitazione nell'apertura della bocca; 4) locking intermittente. US è stato eseguito su entrambe le ATM sia in fase statica che dinamica, mediante ecografo General Electric (LOGIQ7) con sonda lineare (8,5 MHz) posizionata lungo l'asse maggiore del ramo condilare. Il V era presente quando lo spessore della capsula articolare era ≥1,5 mm.
Risultati
46/68 (68%) hanno presentato V a carico delle ATM; in 16 (35%) il V era bilaterale. 2/46 con V erano sintomatici, mentre in 44 non erano presenti sintomi.
Conclusioni
Questi dati suggeriscono che un'alta percentuale di bambini e giovani adulti con AIG ad esordio OA, nella fase iniziale della malattia, presenta un interessamento flogistico delle ATM anche in assenza di sintomi. L'US, non invasivo e facilmente ripetibile, ci offre importanti informazioni sul coinvolgimento articolare delle ATM ed è risultato utile nella diagnosi all'esordio.
Introduction
Juvenile idiopathic arthritis (JIA) is characterized by chronic synovitis and extra-articular manifestations, such as fever, lymphadenopathy, pericarditis, and uveitis. JIA is a chronic inflammatory disease that develops for the age of 16 years and persists for more than 6 weeks [1]. It is diagnosed according to criteria established in 1997 in Durban by the International League of Associations for Rheumatology (ILAR) and revised in 2001 in Edmonton [2]. The temporomandibular joint (TMJ) may be affected by JIA. Temporomandibular diseases (TMDs) such as clicking, crepitation, and disk displacement in patients with JIA have been shown to cause inflammation and degeneration of the condylar heads in the TMJs [3–7]. TMJ arthritis may not be associated with pain or other clinical signs or symptoms of altered TMJ function, but, it can lead to impaired facial growth, micrognathia, and mandibulofacial alterations such as a convex facial morphology. The possibility of TMJ involvement in children with JIA has to be carefully assessed at disease onset and during follow-up because TMDs are often masked by antirheumatic therapy. In oligoarticular (OA) forms of JIA, TMJ involvement may be overlooked, and symptoms may be absent even during the acute phase of the disease [8].
Ultrasonography (US) has been shown to be an important diagnostic tool, comparable to magnetic resonance imaging (MRI), for the assessment of TMJ involvement in rheumatoid arthritis and psoriatic arthritis [9]. In this study, we evaluated the usefulness of US in the assessment of TMJ involvement and the detect joint effusion (JE) in a cohort of children with JIA.
Materials and methods
Patients and controls
Patients were recruited from the Section of Rheumatology of the Department of Internal Medicine at the University of Florence. We enrolled 68 children (57 girls, 11 boys; median age 11.0 years, age range 9.1–16.0 years) with early-stage JIA (mean duration from onset, 6 ± 2 weeks) that had not been treated.
According to the ILAR revised criteria for the classification of JIA [1], 6 months after onset, 11 out of 68 children had extended oligoarthritis. ANOVA was used to assess correlations between US findings and ESR, CRP levels, and antinuclear (ANA) antibody titers.
The control group comprised 40 sex- and age-matched healthy children attending the outpatient clinic for musculoskeletal pain. None had any signs of inflammation, and rheumatic, endocrine, and metabolic disease had been excluded in all cases. Informed consent was obtained from the parents or guardians of all patients and controls.
Ultrasonography
Each patient and control underwent US imaging of both TMJs in static and dynamic phases. Examinations were performed with a General Electric LOGIQ7 scanner and a linear transducer (8.5 MHz). The transducer was placed along the axis of the mandibular ramus. For each TMJ, the following parameters were evaluated: 1) joint space; 2) condylar profile; 3) presence of JE; 4) position of the articular disk with the mouth open and closed. All examinations were carried out by the same trained operator (MD), who was blinded to the subject's group origin (patient vs. control) and clinical signs and symptoms.
The joint capsule appeared as a hyperechoic line running parallel to the surface of the condylar head. Capsule thickness was measured as the distance between this line and the bone [4]. The condylar profile was visualized as a hyperechoic line with or without alterations suggestive of erosion, osteophyte formation, or bone remodelling. The presence of JE was diagnosed in the presence of a joint capsule ≥1.5 mm thick (>95th percentile of controls) and a hypoechoic area within the joint space. For each TMJ, capsule thickness was measured 3 times, and the mean of the 3 results was used for analysis.
Statistical analysis
Data are reported as means ± SD and as percentages. ANOVA test was used to assess correlation with serologic profiles. All analyses were performed with the SPSS package for Windows, version 11.0 (SPSS, Inc., Chicago, IL).
Results
In all 40 healthy controls, the TMJ capsule was less than 1.4 mm thick. The highest value observed in the controls was 1.38 mm (1 child). Therefore, the 95th percentile was 1.3 mm. The mean thicknesses of the right and left TMJ capsules were not significantly different in controls (1.01 ± 0.16 mm vs. 1.04 ± 0.25 mm, respectively).
In the JIA group, 46 out of 68 patients (68%) presented TMJ JE (bilateral in 16 [35%] cases, unilateral in 30 [65.2%]) (Figs. 1 and 2, respectively). Only 2 (4.3%) out of 46 children with JE were symptomatic; the other 44 (95.6%) did not complain of joint pain. Condylar remodelling was observed in 62 (91.2%) out of 68 patients (unilateral in 17 cases and bilateral in the other 37). In 18/124 TMJs (14.5%) a cortical “break” was observed in the condyle that could be defined as erosion (Fig. 3), while 14/124 TMJs (11.3%) presented osteophytes. Disk alterations were not observed. No correlation was found between US findings and ESR, CRP, or ANA.
Fig. 1.
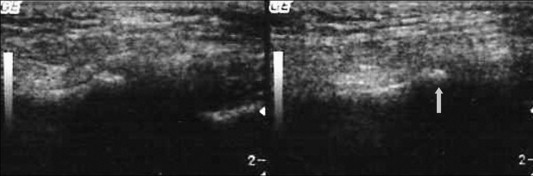
Unilateral joint effusion and bone erosion (see arrow) in JIA.
Fig. 2.
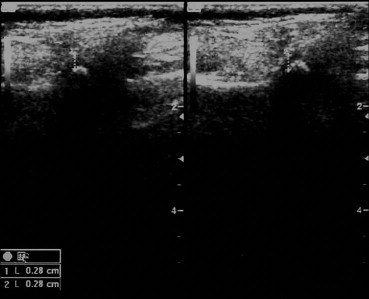
TMJ in JIA, bilateral joint effusion and the thickness of the joint capsule = 2.8 mm.
Fig. 3.
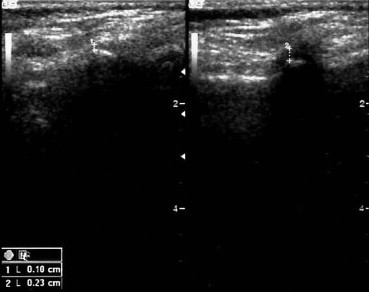
TMJ in JIA, unilateral joint effusion and the thickness of the joint capsule = 2.3 mm.
Discussion
Evaluation of the TMJ is not easy. In JIA, clinical assessment of this joint is insufficient because its involvement is often asymptomatic. Clinical findings must, therefore, be confirmed with imaging studies. MRI is regarded as the gold standard for imaging assessment of the TMJ, but its limited availability and high cost make it unsuitable as a screening or follow-up method [6]. The orthopanogram reveals only late-stage TMJ damage, while computed tomography is not able to visualize the articular disk. US is a widely used diagnostic imaging tool in patients with rheumatic diseases. Recent studies using MRI as a reference method demonstrate that high-resolution US can be a valid alternative for detecting bone damage, effusion (with a concordance rate of 76.1%) and disk displacement in the TMJ [9–15].
In this study we evaluated TMJ involvement in JIA by US imaging. Our preliminary results seem indicate that the US examination is a useful, noninvasive, radiation-free tool for screening JIA patients for TMJ involvement and that it may play an important role in detecting JE. Identifying the presence of JE at an early phase, before symptoms of TNJ dysfunction develop, allows prompt orthodontic therapy that may prevent radiographically evident condylar lesions and impairment of mandibulofacial development.
Conflict of interest statement
The authors have no conflict of interest.
Footnotes
SIUMB 2008 – Award for the best oral communication presented at the 19th National Congress of the SIUMB.
References
- 1.Twilt M., Mobers S.M., Arends L.R., ten Cate R., van Suijlekom-Smit L. Temporomandibular involvement in juvenile idiopathic arthritis. J Rheumatol. 2004;31:1418–1422. [PubMed] [Google Scholar]
- 2.Berntson L., Fasth A., Andersson-Gare B., Svensson, Nordic Study Group Construct Validity of ILAR and EULAR criteria in Juvenile Idiopathic Arthritis: a population based incidence study from the Nordic Countries. J Rheumatol. 2001;28(12):2737–2743. [PubMed] [Google Scholar]
- 3.Kuseler A., Pedersen T.K., Gelineck J., Herlin T. A 2 year followup study of enhanced Magnetic Resonance Imaging and clinical examination of the temporomandibular joint in children with Juvenile idiopathic arthritis. J Rheumatol. 2005;32:162–169. [PubMed] [Google Scholar]
- 4.Wakefield R.J., Gibbon W.W., Conaghan P.G. The value of sonography in the detection of bone erosions in patients with rheumatoid arthritis: a comparison with conventional radiography. Arthritis Rheum. 2000;43:2762–2770. doi: 10.1002/1529-0131(200012)43:12<2762::AID-ANR16>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 5.Dawes P.T. Radiological assessment of outcome in rheumatoid arthritis. Br J Rheumatol. 1988;27(Suppl. 1):21–36. [PubMed] [Google Scholar]
- 6.Jank S., Haase S., Strobl H. Sonographic investigation of the temporomandibular joint in patients with juvenile idiopathic arthritis: a pilot study. Arthritis Rheum. 2007;57:213–218. doi: 10.1002/art.22533. [DOI] [PubMed] [Google Scholar]
- 7.Wolfe F., Sharp J.T. Radiographic outcome of recent-onset rheumatoid arthritis: a 19-year study of radiographic progression. Arthritis Rheum. 1998;41:1571–1582. doi: 10.1002/1529-0131(199809)41:9<1571::AID-ART7>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 8.Bianchi S., Martinoli C., Sureda D., Rizzatto G. Ultrasound of the hand. Eur J Ultrasound. 2001;14:29–34. doi: 10.1016/s0929-8266(01)00143-4. [DOI] [PubMed] [Google Scholar]
- 9.Melchiorre D., Calderazzi A., Maddali Bongi S., Cristofani R., Bazzichi L., Eligi C. A comparison of ultrasonography and magnetic resonance imaging in the evaluation of temporomandibular joint involvement in rheumatoid arthritis and in psoriatic arthritis. Rheumatology. 2003;42:673–676. doi: 10.1093/rheumatology/keg181. [DOI] [PubMed] [Google Scholar]
- 10.Emshoff R., Jank S., Bertram S., Rudisch A., Bodner G. Disk displacement of the temporomandibular joint: sonography versus MR Imaging. AJR Am J Roentgenol. 2002;178:1557–1562. doi: 10.2214/ajr.178.6.1781557. [DOI] [PubMed] [Google Scholar]
- 11.Jank S., Rudisch A., Bodner G., Brandlmaier I., Gerhard S., Emshoff R. High-resolution ultrasonography of the TMJ: helpful diagnostic approach for patients with TMJ disorders? J Cranio-Maxillofac Surg. 2001;29:366–371. doi: 10.1054/jcms.2001.0252. [DOI] [PubMed] [Google Scholar]
- 12.Jank S., Emshoff R., Norer B. Diagnostic quality of dynamic high-resolution ultrasonography of the TMJ-a pilot study. Int J Oral Maxillofac Surg. 2005;34:132–137. doi: 10.1016/j.ijom.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 13.Hoving J.L., Buchbinder R., Hall S. A comparison of Magnetic Resonance Imaging, sonography, and radiagraphy of the hand in patients with early rheumatoid arthritis. J Rheumatol. 2004;31:663–675. [PubMed] [Google Scholar]
- 14.Hermann K.G., Backhaus M., Schneider U. Rheumatoid arthritis of the shoulder joint: comparison of conventional radiography, ultrasound, and dynamic contrast-enhanced magnetic resonance imaging. Arthritis Rheum. 2003;48:3338–3349. doi: 10.1002/art.11349. [DOI] [PubMed] [Google Scholar]
- 15.Combe B., Dougados M., Goupile P. Prognostic factors for radiographic damage in early rheumatoid arthritis: a multiparameter prospective study. Arthritis Rheum. 2001;44:1736–1743. doi: 10.1002/1529-0131(200108)44:8<1736::AID-ART308>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]


