Abstract
The increasing availability of human cardiac tissues for study are critically important in increasing our understanding of the impact of gender, age, and other parameters, such as medications and cardiac disease, on arrhythmia susceptibility. In this study, we aimed to compare the mRNA expression of 89 ion channel subunits, calcium handling proteins, and transcription factors important in cardiac conduction and arrhythmogenesis in the left atria (LA) and ventricles (LV) of failing and nonfailing human hearts of both genders. Total RNA samples, prepared from failing male (n = 9) and female (n = 7), and from nonfailing male (n = 9) and female (n = 9) hearts, were probed using custom-designed Taqman gene arrays. Analyses were performed to explore the relationships between gender, failure state, and chamber expression. Hierarchical cluster analysis revealed chamber specific expression patterns, but failed to identify disease- or gender-dependent clustering. Gender-specific analysis showed lower expression levels in transcripts encoding for Kv4.3, KChIP2, Kv1.5, and Kir3.1 in the failing female as compared with the male LA. Analysis of LV transcripts, however, did not reveal significant differences based on gender. Overall, our data highlight the differential expression and transcriptional remodeling of ion channel subunits in the human heart as a function of gender and cardiac disease. Furthermore, the availability of such data sets will allow for the development of disease-, gender-, and, most importantly, patient-specific cardiac models, with the ability to utilize such information as mRNA expression to predict cardiac phenotype.
Introduction
Epidemiologically, there are well-established gender differences in the manifestations of cardiac arrhythmias. Men are more susceptible to the development of atrial fibrillation (AF) [1], [2], whereas women have higher incidence of long-QT syndrome (LQTS) and drug-induced Torsades de Pointes [3], [4]. In addition, men and women exhibit differences in basic electrophysiological parameters during normal sinus rhythm. Women, for example, tend to have increased resting heart rates [5] and longer rate-corrected QT (QTc) intervals [6], whereas men have been reported to have longer P-waves suggesting differences in baseline atrial electrophysiological properties [7]. Interestingly, autonomic blockade does not mask the gender differences in resting heart rate, suggesting that intrinsic sinus node differences, as opposed to gender dependent autonomic tone, are responsible for this variability [5].
Much less is known, however, about the molecular mechanisms underlying observed gender differences in arrhythmia susceptibility and basic electrophysiological parameters in the human heart. Insight has been gained primarily from animal models, particularly studies in the rabbit, dog, and mouse [8]. The rabbit heart has been suggested to be a relevant model for the study of human arrhythmias [9] and female rabbits also exhibit gender dependent differences in QTc intervals [10] similar to that seen in humans [6]. Although mice afford easy genetic manipulations, they manifest profound differences in cardiac electrophysiology compared to humans [11], [12] which must be considered when extending conclusions to human physiology and pathophysiology [13], [14]. Since the expression profile of ion channels and transporters determine cardiac excitability and may also determine arrhythmia susceptibility, several recent studies have explored gene expression patterns in the human heart [15], [16], [17], [18], [19], [20]. As the ever present limitation to detailed human studies is the availability of human tissues for analysis, we have developed the infrastructure necessary to collect and systematically investigate tissues from both failing and nonfailing human hearts suitable for detailed functional and molecular analyses. In addition to investigating the global patterns of mRNA expression relating to gender and heart failure in the human heart, we have also provided a comprehensive set of data which was used to computationally model patient-specific electrophysiology and explore population-dependent variability in action potential morphology by our colleagues Walmsley, et al.
We focused on probing tissues of the left atria (LA) and ventricle (LV), as left-sided heart remodeling and dysfunction are the most common manifestations of heart failure [21], [22]. Specifically, we quantified the transcript expression levels of 89 target genes in the LA and LV of failing and nonfailing human hearts of both genders. In some analyses, tissues isolated from the epicardium and endocardium of the LV were examined separately as we have previously shown that heart failure results in a heterogeneous remodeling of repolarization across the ventricular wall and altered dispersion [23], which may be pro-arrhythmic [24].
Methods
The use of human hearts for research was approved by the Institutional Review Board at Washington University in St. Louis.
Human Tissue Samples
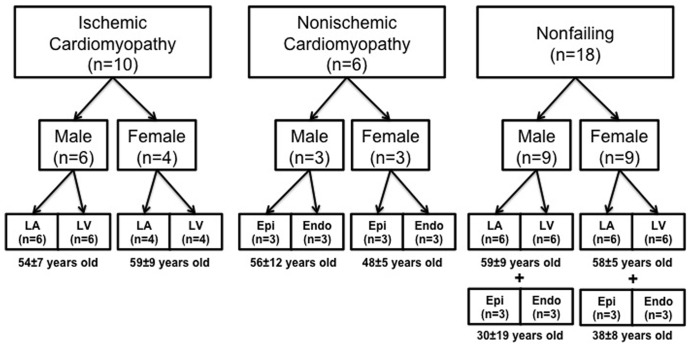
For this study a total of 34 explanted human hearts of both genders (n = 16 women, 52±10 years old; n = 18 men, 52±14 years old) were acquired from two sources (Figure 1). Failing human hearts (n = 16; 9 men, 7 women) were obtained at the time of cardiac transplantation at Barnes-Jewish Hospital (St. Louis, MO) and nonfailing hearts (n = 18; 9 men, 9 women) were provided by Mid-America Transplant Services (St. Louis, MO) after they were deemed unsuitable for cardiac transplantation. Each heart was collected in the operating room after removal from the chest and immediately perfused with and stored in cardioplegic solution (4°C) for preservation during the 15–20 minute delivery from the operating room to the research laboratory. Upon arrival, tissue samples from the LA (n = 22) and LV (n = 22) free walls were immediately harvested and preserved. Epicardial and endocardial samples were also harvested from the LV free wall (n = 12). All tissue samples were preserved and stored in RNAlater (Sigma-Aldrich, St. Louis, MO) at −80°C. Basic clinical characteristics of the patients are shown in Tables 1 and 2.
Figure 1. Study population (n = 34).
Table 1. Clinical characteristics of nonfailing hearts.
| HeartNumber | Gender | Age | Cause of Death | LVEDD* (cm) | EF† (%) |
| 1 | Female | 55 | Stroke | unknown | <20 |
| 2 | Female | 33 | Head Trauma | unknown | unknown |
| 3 | Female | 59 | Anoxic Brain Injury | unknown | unknown |
| 4 | Female | 66 | Stroke | unknown | unknown |
| 5 | Female | 34 | Brain Death | 4.8 | 20 |
| 6 | Female | 58 | Stroke | unknown | 30 |
| 7 | Female | 49 | Anoxia | 4.1 | 65 |
| 8 | Female | 59 | unknown | unknown | unknown |
| 9 | Female | 50 | Anoxia | unknown | 60–65 |
| 10 | Male | 19 | Anoxia | 4.1 | 45 |
| 11 | Male | 60 | Head Trauma | 3.3 | 65 |
| 12 | Male | 55 | Stroke | 4.7 | 35 |
| 13 | Male | 50 | Stroke | unknown | unknown |
| 14 | Male | 52 | Head Trauma | 4.3 | 60–70 |
| 15 | Male | 65 | Stroke | unknown | unknown |
| 16 | Male | 58 | Stroke | unknown | 60–70 |
| 17 | Male | 20 | Drug Overdose | unknown | unknown |
| 18 | Male | 59 | Brain Death | unknown | unknown |
left ventricular end diastolic dimension.
ejection fraction.
Table 2. Clinical characteristics of failing hearts.
| Heart Number | Gender | Age | Diagnosis | Devices | LVEDD* (cm) | EF† (%) | Arrhythmia History |
| 1 | Female | 65 | ICM‡ | ICD§ | 6.4 | 15 | NSVT||, VF# |
| 2 | Female | 49 | ICM | ICD | 5.9 | 25–30 | VT** |
| 3 | Female | 53 | ICM | ICD | 6.5 | 20 | No arrhythmias |
| 4 | Female | 67 | ICM | ICD | 7 | 10 | No arrhythmias |
| 5 | Male | 50 | ICM | PPMa, ICD, BiVb | 7 | <15 | Refractory VT |
| 6 | Male | 44 | ICM | ICD, LVADc | 7 | <15 | No arrhythmias |
| 7 | Male | 69 | ICM | PPM, ICD, BiV | 7.13 | 39 | AFd, VT |
| 8 | Male | 63 | ICM | PPM, ICD, BiV | 7.6 | 15 | No arrhythmias |
| 9 | Male | 50 | ICM | ICD | 6.6 | 30 | NSVT, VF |
| 10 | Male | 67 | ICM | ICD, LVAD | 7.9 | 10 | No arrhythmias |
| 11 | Female | 44 | NICMe | ICD, LVAD | 5.5 | 20–25 | AF |
| 12 | Female | 54 | NICM | ICD | 6.1 | <20 | AF, VT |
| 13 | Female | 46 | NICM | ICD, LVAD | 7.8 | 16 | AF |
| 14 | Male | 70 | NICM | ICD | >6.6 | 16 | AF |
| 15 | Male | 47 | NICM | LVAD | 6.4 | 25 | VT |
| 16 | Male | 53 | NICM | ICD | 8.2 | 16 | VT |
left ventricular end diastolic volume
ventricular tachycardia.
ejection fraction
permanent pacemaker.
ischemic cardiomyopathy
biventricular device.
implantable cardioverter defibrillator
left ventricular assist device.
nonsustained ventricular tachycardia
atrial fibrillation.
ventricular fibrillation
nonischemic cardiomyopathy.
RNA Extraction and Preparation
Total RNA was extracted from 68 samples using the RNEasy Fibrous Tissue Mini Kit (Qiagen, Valencia, CA) according to the manufacturer’s instructions. RNA yield was measured using a Nanodrop 1000 (Thermo Scientific) and quality was assessed by verifying the presence of the 18 S and 28 S bands as run on a 1% agarose gel.
Low-Density Taqman Gene Arrays
Custom-designed low-density Taqman gene arrays (Applied Biosytems, Foster City, CA) were used to probe for the presence of 96 targets in a two-step process as described previously [16], [19], [25]. In short, total RNA (1–2 µg) was first converted to cDNA using the High Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA). Subsequent reactions were performed, using 100 ng of cDNA loaded into each well of our custom-designed gene arrays, with the ABI PRISM 7900 HT Sequence Detection System (Applied Biosystems, Foster City, CA). Genes selected for analysis included 56 ion channels and accessory proteins, 14 calcium-handling proteins, 9 autonomic receptors, 6 transcription factors, 3 signaling proteins, and 8 controls/marker genes and are listed in Table S1.
Statistics and Data Analysis
Data were collected and analyzed by the Applied Biosystems SDS 2.3 software using the threshold cycle (Ct) relative quantification method [26] with GAPDH as an endogenous control. Quantitative data are expressed as mean ± standard deviation. Statistically significant differences were identified using a one-way analysis of variance followed by Tukey-Kramer’s test with a significance level of p<5.6×10−4 based on the Bonferroni correction (GenEx; MultiD, Santa Clara, CA). All quantitative results are available at the NIH GEO database (GEO Accession #GSE33165).
In addition, two-way hierarchical agglomerative cluster analysis was performed using the ΔΔCt of each target. We applied average linkage clustering with calculation of Euclidean distances. Clusters were analyzed and visualized using Cluster 3.0 and Treeview software [27].
Results
Hierarchical Cluster Analysis
Hierarchical cluster analysis was used to determine if strong enough overall trends in transcript expression across gender, disease, and cardiac chambers manifested to create distinct clusters of highly-related samples. As is shown in the Online Data Supplement (Figure S1), LA and LV samples from ischemic and nonfailing hearts of both genders show distinct clustering based on chamber location (Figure S1A). These samples do not cluster, however, based on gender or disease state. We also explored cluster analysis of ischemic, nonischemic, and nonfailing LV samples of both genders (Figure S1B), as well as nonischemic and nonfailing samples from the epicardium and endocardium of the LV (Figure S1C). Clustering of these latter samples based on gender, disease, or cardiac location was not evident.
Ventricular Remodeling in Heart Failure and Differences in Transcript Expression
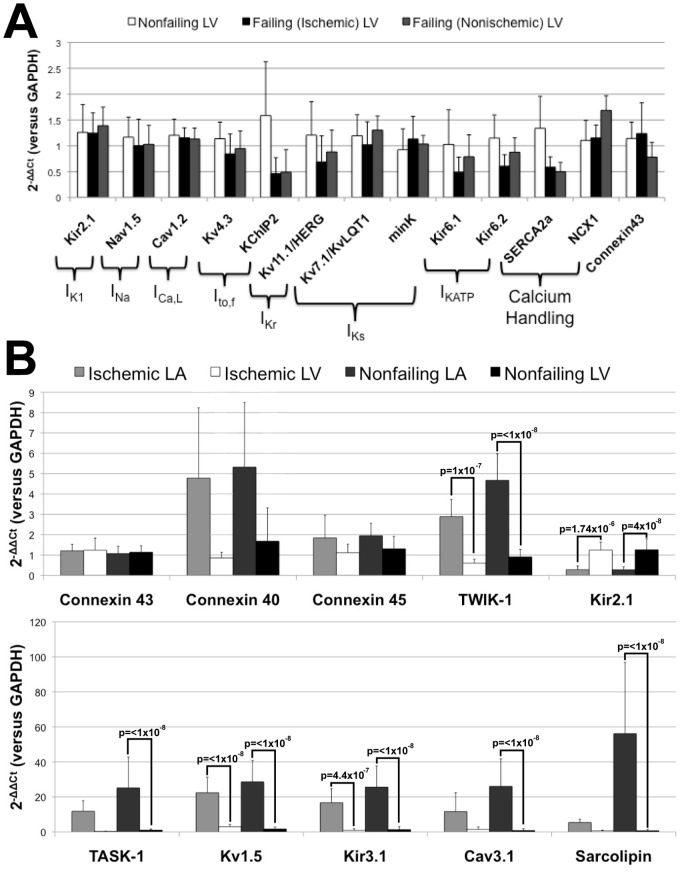
Previous studies have revealed that during the heart failure remodeling process, the cardiac action potential is significantly prolonged and conduction is slowed due to pathological changes in the expression and function of ion channels [28], [29]. As shown in Figure 2A, we observe trends for reduction in the expression of transcripts encoding ion channel subunits that are important in cardiac conduction and repolarization, as well as changes in key calcium handling proteins. Similar to previously reported findings, for example, we observe downregulation of the subunits encoding for IKATP [30] and Ito [31]. Ito,fast channels, in particular, encoded by the pore-forming subunit Kv4.3 and the accessory protein KChIP2, is one of the most consistently altered ion channels during the heart failure remodeling process across species [32]. Consistent with previous suggestions, reductions in Ito,fast density in the failing heart are linked to protein-level downregulation of Kv4.3 and transcript-level downregulation of KChIP2 [33]. We find lower KChIP2 expression in LV samples from failing, compared with nonfailing hearts (Figure 2A). In contrast with the findings for KChIP2, we observe no significant changes in the expression of subunits encoding IK1, INa, and ICa,L channels. There is, however, a trend for lower expression of Kv11.1/HERG, the subunit encoding the rapid component of delayed rectification, IKr, as well as the calcium handling proteins, SERCA2a and NCX1, consistent with recent findings [33]. Finally, we observe a downregulation of connexin 43 in nonischemic, but not ischemic, cardiomyopathy.
Figure 2. Ventricular remodeling in heart failure.
(A) Ventricular remodeling of major ion channel subunits and accessory proteins in heart failure. (B) Regional specificity of targets in failing and nonfailing hearts of both genders.
Major differences in atrial-ventricular transcript expression patterns are shown in Figure 2B. Consistent with previous findings, we observed atrial predominance of several transcripts, such as connexin 40, TASK-1, TWIK-1, Kir2.1, Kv1.5, Kir3.1, Cav3.1, and sarcolipin [18], [34], [35]. In addition, with the exception of connexin 40, we measured similar expression levels of the connexin 40, 45, and 43 transcript in both the LA and LV (Figure 2B).
The general agreement of our findings, regarding both ventricular remodeling during heart failure and atrio-ventricular specificity, with previous studies [18], [30], [31], [34], [35] both supports the validity of our findings and allows for the exploration of other novel gene expression patterns with regard to gender and arrhythmia susceptibility.
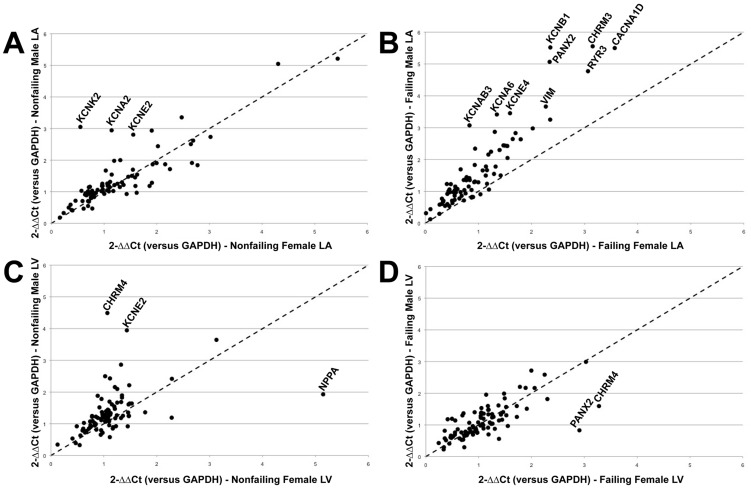
Gender Dependent Atrial/Ventricular Bias
A gender-based comparison of overall relative expression levels for all targets in both failing and nonfailing hearts is shown in Figure 3. As is evident in Figure 3B, there is a distinct atrial gender bias, with males exhibiting overall higher expression levels of almost all transcripts quantified as compared with females. In the ventricles, there is also a slight male bias in overall relative transcript expression levels (Figure 3C), although in contrast with the atria the pattern emerges in nonfailing hearts, as opposed to failing LV. Interestingly, previous studies in wild-type mouse hearts demonstrated a similar male gender bias in overall atrial gene expression [36].
Figure 3. Gender dependent comparison of relative expression levels of all genes.
(A) Nonfailing male versus female LA. (B) Failing male versus female LA showing a distinct male bias. (C) Nonfailing male versus female LV. (D) Failing female versus male LV. The dotted diagonal line represents equal expression levels between genders.
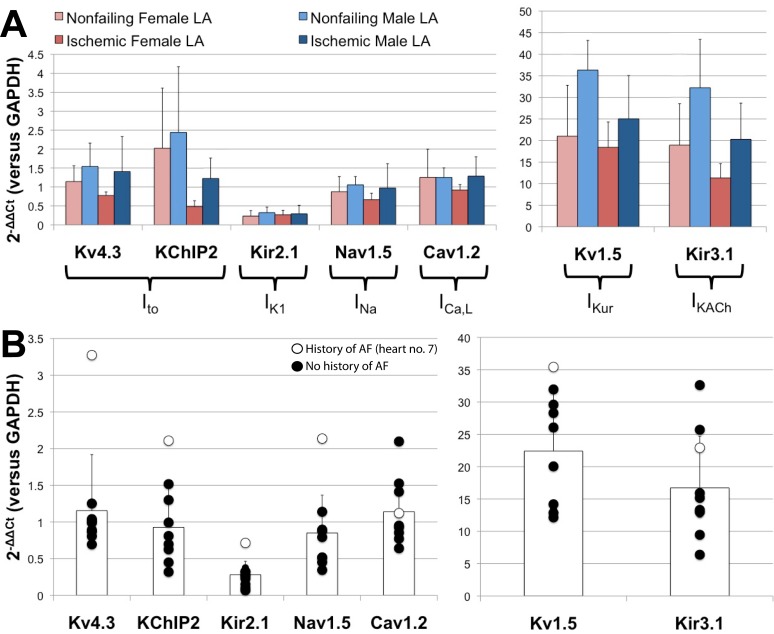
Gender Dependent Atrial Remodeling
Because epidemiological data have revealed that males have an increased overall lifetime risk of developing atrial fibrillation [1], [2], we compared the expression levels of the major ion transcripts that have been shown or are postulated to undergo pathological remodeling [37], [38], [39]. The gender dependent relative expression levels of these transcripts are shown in Figure 4A.
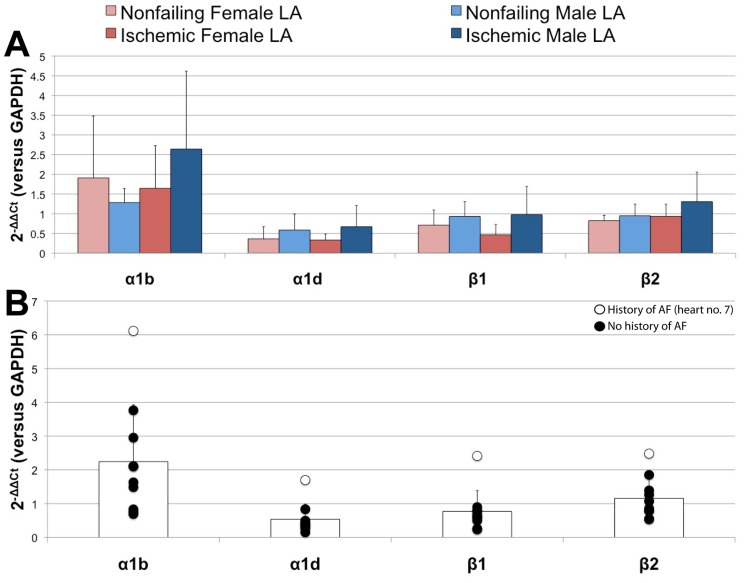
Figure 4. Gender dependent remodeling in the LA.
(A) Gender dependent atrial remodeling of major ion channel subunits and accessory proteins in failing and nonfailing hearts of both genders. (B) Relative expression levels of failing LA samples of both genders. The white data points indicate the patient with a documented history of AF.
Atrial fibrillation has been shown to be associated with significant reductions in Ito [40], IKur [41], IKACh [42], and ICa,L [43], [44], whereas IK1 current tends to be increased in AF patients [42] and INa has been shown to not be significantly altered [45]. Surprisingly, when we assessed the gender dependence of these targets in our overall patient population, we observe patterns consistent with our female population being potentially more susceptible to the development of atrial fibrillation. As seen in Figure 4A, our female subjects exhibit lower expression levels in atrial Kv4.3, KChIP2, Kv1.5, and Kir3.1, as compared with our male subjects. We also see trends for lower expression in Nav1.5 and Cav1.2, with no significant changes or trends in Kir2.1.
Based on the known clinical characteristics of our patient population, we identified one failing human heart (#7) with a documented history of AF from which we analyzed an LA specimen. Contrary to our expectations, as shown in Figure 4B, this particular sample had the highest relative expression levels of Kv4.3, KChIP2, Kir2.1, Nav1.5, and Kv1.5 when compared to all failing LA specimens of both genders. This samples does, however, have a lower relative expression level of Cav1.2 than other male specimens in this group.
We also explored the gender dependence of relative expression levels for adrenergic receptors, as an increased level of adrenergic activity can be associated with the onset of AF [46]. As seen in Figure 5A, we do not observe any significant differences in adrenergic receptor expression in the LA of failing and nonfailing hearts. There is an apparent trend that males tend to exhibit overall higher relative expression levels of α1b, α1d, β1, and β2 adrenergic receptors. This finding, however, may be due to an intrinsically decreased sympathetic tone in women as compared to men [47]. Interestingly, as shown in Figure 5B, the failing heart (#7) with a history of AF displays the highest relative expression levels of all of the adrenergic receptors analyzed.
Figure 5. Gender dependent remodeling of adrenergic receptors.
(A) Gender dependent atrial remodeling of adrenergic receptors in failing and nonfailing hearts of both genders. (B) Relative expression levels of adrenergic receptors in failing LA samples of both genders. The white data points indicate the patient with a documented history of AF.
Gender Dependent Ventricular Remodeling
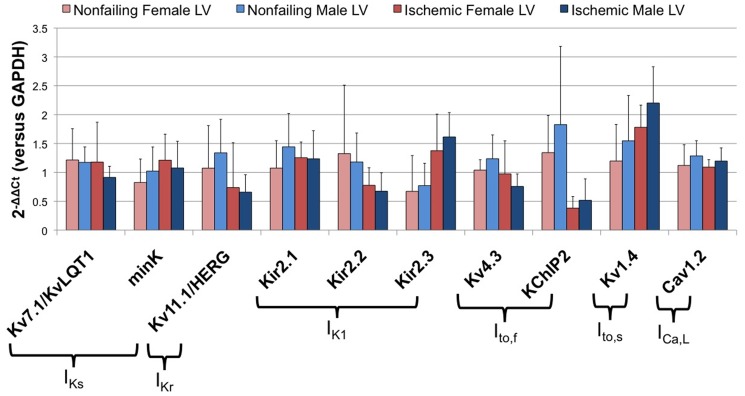
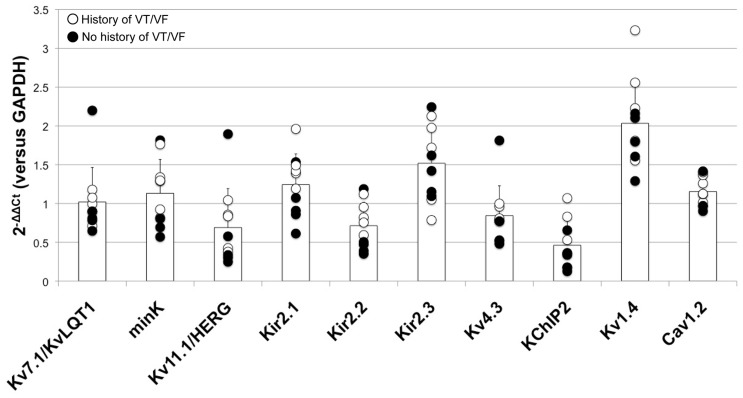
Epidemiologically, females tend have a higher incidence of LQTS and drug-induced Torsades de Pointes [3], [4]. Subsequent analysis therefore focused on a subset of ion channels known to be important in cardiac repolarization [8], [48]. As shown in Figure 6, quantification of the relative expression levels of these transcripts revealed no significant differences in patterns based on gender. In addition, direct comparison of the expression levels of these transcripts linked to repolarization in LV samples from failing hearts with and without histories of ventricular tachyarrhythmias also do not reveal any striking patterns as shown in Figure 7.
Figure 6. Gender dependent ventricular remodeling of major repolarizing ion channel subunits and accessory proteins in failing and nonfailing hearts of both genders.
Figure 7. Relative expression levels of failing LV samples of both genders.
The white data points indicate patients with a documented history of ventricular tachyarrhythmias.
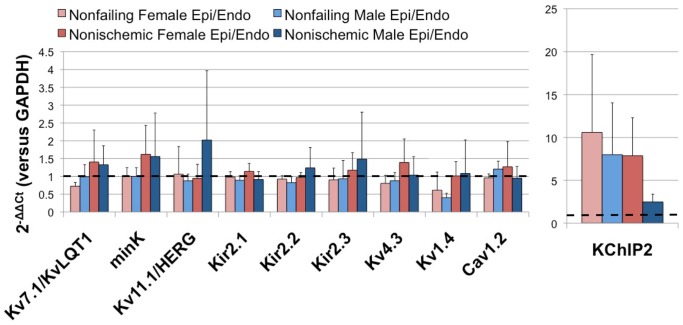
Gender Dependent Transmural Heterogeneity
Transmural heterogeneities in action potential waveforms across the ventricular wall are major determinants of arrhythmia susceptibility [49] and directly alter electrophysiological parameters during heart failure [23] Figure 8 shows the ratios of epicardial to endocardial expression for key transcripts linked to repolarization in failing and nonfailing hearts of both genders. Ratios of around one indicate those transcripts, such as Kv7.1/KvLQT1, mink, Kir2.1, Kir2.2, Kir2.3, Kv4.3, and Cav1.2, that are uniformly expressed across the transmural wall of the LV in both failing and nonfailing hearts. On the other hand, ratios of either greater or less than one represent transcripts that are more heterogeneously expressed across the LV transmural wall. For example, KChIP2, the accessory protein for Ito channels, exhibits a significantly larger ratio than any of the other targets shown in Figure 8. In the failing male heart, however, this heterogeneity is not present as the ratio of epicardial to endocardial expression is one. Kv1.4, a pore-forming subunit for Ito,slow, displays a reduced ratio in nonfailing hearts, but again, as with KChIP2, the transmural expression ratio is one in the failing heart.
Figure 8. Average ratios of epicardial to endocardial expression of repolarization targets in failing and nonfailing hearts of both genders.
The dotted back line represents a ratio of one.
Discussion
In the present study, we explored the impact of gender on the transcript expression levels of the major cardiac ion channels, calcium handling proteins, and transcription factors in the failing and nonfailing human heart. We found gender-specific differences in relative expression levels of ion channel subunits, such as Kv4.3, KChIP2, Kv1.5, and Kir3.1 in the LA, but no significant gender-specific differences in relative expression levels of these subunits in the LV. Analyses of transmural heterogeneities in transcript expression levels in the LV, however, revealed a heterogeneity of expression across the LV wall in of the Ito,slow pore-forming subunit, Kv1.4, as well as with the Ito,fast accessory subunit, KChIP2. In the nonfailing heart, Kv1.4 exhibited higher expression in the epicardium of the nonfailing heart, whereas KChIP2 exhibited a stronger expression in the epicardium across gender and disease state.
Until recently, there has been very limited data available regarding global gender dependent cardiac ion channel gene expression in the human heart. A 2010 study by Gaborit, et al [18] explored gender dependent differences in the nonfailing human ventricle (left and right ventricles) and, unlike in our investigation, found significantly lower expression levels in the female LV of key ion channels and accessory proteins important in cardiac repolarization. Their patient population consisted of 10 men and 10 women with average ages of 38±12 years and 43±13 years, respectively. Our patient population, on the other hand, consisted of both failing and nonfailing human hearts with significantly older average ages (failing females, 54±9 years; failing males, 56±9 years; nonfailing females, 51±11 years, failing males, 50±18 years). The variability of qPCR data has shown to be significantly increased in aged animals [50] and humans [51], which in our case may mask any intrinsic gender dependent expression differences in the LV in our study.
The use of an older patient population may, however, be more representative with respect to the gender dependent analysis of LA targets important in the generation and maintenance of AF, as AF is relatively uncommon before the age of 60 and 10% of the overall population develops AF by 80 years of age [52]. In addition, 1 in 4 heart failure patients develop AF within five years of diagnosis [53], so it is likely that relevant atrial remodeling processes [54] are well underway in our patient population. Interestingly, although overall men are more likely to develop heart failure [55], women diagnosed with heart failure are approximately 1.5 times more likely to develop AF than their male counterparts [56]. Additionally, the overall higher atrial expression levels of almost all transcripts analyzed in this study (Figure 3B) in the failing male hearts, as compared to failing female hearts, may mask any intrinsic gender-based differences.
Interpretation of these results, however, with respect to both the LA and LV must be considered in light of the available clinical information, as shown in Tables 1 and 2. As described in the Results section, we identified one patient (failing heart no. 7) with a history of AF. This patient exhibited high expression levels of Kv4.3, KChIP2, Kir2.1, Nav1.5, and Kv1.5 when compared with all other failing LA specimens of both genders, as shown in Figure 4B. This sample did, however display a relatively lower expression level of Cav1.2 as compared with other specimens in the group, which is likely related to the patient’s four-month history of permanent AF prior to transplantation. It should also be noted that, prior to diagnosis of AF, this patient had been previously diagnosed with ventricular arrhythmias which concurrently played a role in the progression of heart failure and overall arrhythmia history. As previously reported, in human AF the primarily physiological remodeling results from changes in ICa,L and significant reductions of current density have only been reported after 18 months of persistent AF [57]. In addition, as shown in Figure 7, we observed no remarkable expression patterns in key repolarization targets in the LV of failing hearts with and without a history of ventricular tachyarrhythmias, which may in part be due to the individual etiologies of heart failure, which must be elucidated further in future studies.
Prolongation of the cardiac action potential is a hallmark of heart failure [58]. Furthermore, heterogeneous distribution of repolarization transmurally across the ventricular wall manifests as electrophysiological heterogeneities which may also be pro-arrhythmic [49]. In our recent study, we provide direct experimental evidence of transmural heterogeneites in action potential waveforms in the human LV wedge preparation [23]. In the present study, as shown in Figure 8, we explored the potential molecular mechanisms of this functional heterogeneity. The data reveal expression gradients in KChIP2 expression across the transmural wall consistent with differences in Ito [49]. We were unable, however, to pinpoint other channels potentially contributing to action potential heterogeneity as the transcripts encoding the other ion channels prominent in repolarization were found to be more homogenously expressed across the LV wall. In addition, we did not find connexin 43 transcript expression to be heterogeneously expressed, although previous reports have demonstrated significantly lower epicardial connexin 43 protein expression in both failing and nonfailing hearts in our previous study [23]. Patterns of molecular heterogeneity directly affecting action potential durations may either be due to the presence of smaller “islands” of differential gene expression and function [23], [59] not captured in this study or post-translational protein modifications [60] not assessed in our transcript level investigation.
The wealth of information gathered from large-scale gene expression studies such as this and others [17], [19], not only provides insight into the gender dependent, pathological, or regional changes in ion channel expression, but also provides solid physiological data that can be incorporated into computational models. Furthermore, access to detailed clinical information, such as that presented this study, will both assist in interpretation of the molecular mechanisms involved in heart failure and arrhythmogenesis, as well as contribute to the development of tools for patient-specific computational models of cardiac electrophysiology. Constructing models of comprehensive human electromechanical activity requires a thorough understanding of the distribution of ion channels, calcium handling proteins, and other transporters in various regions of the heart, as well as their intrinsic modifications due to disease and gender as we have investigated in this study. Our colleagues Walmsley, et al in their paper “mRNA expression levels in failing human hearts predict cellular electrophysiological remodeling using a population-based simulation study” in this issue of the journal, present a first step towards patient-specific modeling of the action potential and calcium transient based on the comprehensive set of molecular data presented here.
Study Limitations
The study of human hearts, while providing a unique opportunity to explore both the structural and functional mechanisms pertaining to arrhythmias, heart failure, and other pathological conditions, is limited by number of explanted hearts available. Nonfailing, donor hearts are especially precious and cannot be truly considered normal, control hearts due to that fact that they have been rejected for transplantation due to, in some cases, cardiac reasons. In addition, the underlying patient circumstances (i.e. medication, previous cardiac surgery, etc) cannot be controlled for. Thus, the hearts presented in this study represent the best available specimens.
Conclusion
Epidemiologically, it is clear there is a gender disparity in arrhythmia incidence. To attempt to elucidate the underlying molecular mechanisms of these differences, we have explored the gender dependent expression of various ion channels, calcium handling proteins, and other transcription factors in the failing and nonfailing human heart in this study. While we observed significant gender dependent differences in atrial tissues, we did not however observe clear patterns of gender dependent expression in the ventricles. Our data do, however, emphasize the importance of addressing such confounding factors as gender, age, and disease progression when exploring ionic remodeling processes in the human heart and in constructing patient-specific models of cardiac electrophysiology.
Supporting Information
Hierarchical Cluster Analysis. (A) Cluster analysis of ischemic and nonfailing LA/LV samples of both genders showing distinct separation based on cardiac location. (B) Cluster analysis of ischemic, nonischemic, and nonfailing LV samples showing no clustering. (C) Cluster analysis of nonischemic and nonfailing epicardial/endocardial samples also showing no clustering.
(TIF)
Custom-designed Taqman low-density gene array targets.
(DOCX)
Acknowledgments
The authors would like to thank Rebecca Mellor for technical assistance, Drs. Nader Moazami, I-wen Wang, Scott Silvestry, and Michael Pasque for human heart explantations, and Dr. Gregory Ewald and Donna Whitehead for patient consenting and data management.
Funding Statement
This project was supported by National Institutes of Health grants R01-HL114395 and R01-HL085369 from the National Heart, Lung and Blood Institute. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Kannel WB, Wolf PA, Benjamin EJ, Levy D (1998) Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol 82: 2N–9N. [DOI] [PubMed] [Google Scholar]
- 2. Wolbrette D, Naccarelli G, Curtis A, Lehmann M, Kadish A (2002) Gender differences in arrhythmias. Clin Cardiol 25: 49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Locati EH, Zareba W, Moss AJ, Schwartz PJ, Vincent GM, et al. (1998) Age- and sex-related differences in clinical manifestations in patients with congenital long-QT syndrome: findings from the International LQTS Registry. Circulation 97: 2237–2244. [DOI] [PubMed] [Google Scholar]
- 4. Abi-Gerges N, Philp K, Pollard C, Wakefield I, Hammond TG, et al. (2004) Sex differences in ventricular repolarization: from cardiac electrophysiology to Torsades de Pointes. Fundam Clin Pharmacol 18: 139–151. [DOI] [PubMed] [Google Scholar]
- 5. Burke JH, Goldberger JJ, Ehlert FA, Kruse JT, Parker MA, et al. (1996) Gender differences in heart rate before and after autonomic blockade: evidence against an intrinsic gender effect. Am J Med 100: 537–543. [DOI] [PubMed] [Google Scholar]
- 6. Kligfield P, Lax KG, Okin PM (1996) QT interval-heart rate relation during exercise in normal men and women: definition by linear regression analysis. J Am Coll Cardiol 28: 1547–1555. [DOI] [PubMed] [Google Scholar]
- 7. Dhala A, Underwood D, Leman R, Madu E, Baugh D, et al. (2002) Signal-averaged P-wave analysis of normal controls and patients with paroxysmal atrial fibrillation: a study in gender differences, age dependence, and reproducibility. Clin Cardiol 25: 525–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. James AF, Choisy SC, Hancox JC (2007) Recent advances in understanding sex differences in cardiac repolarization. Prog Biophys Mol Biol 94: 265–319. [DOI] [PubMed] [Google Scholar]
- 9. Panfilov AV (2006) Is heart size a factor in ventricular fibrillation? Or how close are rabbit and human hearts? Heart Rhythm 3: 862–864. [DOI] [PubMed] [Google Scholar]
- 10. Ebert SN, Liu XK, Woosley RL (1998) Female gender as a risk factor for drug-induced cardiac arrhythmias: evaluation of clinical and experimental evidence. J Womens Health 7: 547–557. [DOI] [PubMed] [Google Scholar]
- 11. Nerbonne JM (2004) Studying cardiac arrhythmias in the mouse–a reasonable model for probing mechanisms? Trends Cardiovasc Med 14: 83–93. [DOI] [PubMed] [Google Scholar]
- 12. Ahrens-Nicklas RC, Christini DJ (2009) Anthropomorphizing the mouse cardiac action potential via a novel dynamic clamp method. Biophys J 97: 2684–2692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Glukhov AV, Flagg TP, Fedorov VV, Efimov IR, Nichols CG (2010) Differential K(ATP) channel pharmacology in intact mouse heart. J Mol Cell Cardiol 48: 152–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fedorov VV, Glukhov AV, Ambrosi CM, Kostecki G, Chang R, et al. (2011) Effects of K(ATP) channel openers diazoxide and pinacidil in coronary-perfused atria and ventricles from failing and non-failing human hearts. J Mol Cell Cardiol 51: 215–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Borlak J, Thum T (2003) Hallmarks of ion channel gene expression in end-stage heart failure. FASEB J 17: 1592–1608. [DOI] [PubMed] [Google Scholar]
- 16. Gaborit N, Le Bouter S, Szuts V, Varro A, Escande D, et al. (2007) Regional and tissue specific transcript signatures of ion channel genes in the non-diseased human heart. J Physiol 582: 675–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chandler NJ, Greener ID, Tellez JO, Inada S, Musa H, et al. (2009) Molecular architecture of the human sinus node: insights into the function of the cardiac pacemaker. Circulation 119: 1562–1575. [DOI] [PubMed] [Google Scholar]
- 18. Nattel S, Frelin Y, Gaborit N, Louault C, Demolombe S (2009) Ion-channel mRNA-expression profiling: Insights into cardiac remodeling and arrhythmic substrates. J Mol Cell Cardiol 48: 96–105. [DOI] [PubMed] [Google Scholar]
- 19. Gaborit N, Varro A, Le Bouter S, Szuts V, Escande D, et al. (2010) Gender-related differences in ion-channel and transporter subunit expression in non-diseased human hearts. J Mol Cell Cardiol 49: 639–646. [DOI] [PubMed] [Google Scholar]
- 20. Gronich N, Kumar A, Zhang Y, Efimov IR, Soldatov NM (2010) Molecular remodeling of ion channels, exchangers and pumps in atrial and ventricular myocytes in ischemic cardiomyopathy. Channels (Austin) 4: 101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McKee PA, Castelli WP, McNamara PM, Kannel WB (1971) The natural history of congestive heart failure: the Framingham study. N Engl J Med 285: 1441–1446. [DOI] [PubMed] [Google Scholar]
- 22. Hunt SA (2005) ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 46: e1–82. [DOI] [PubMed] [Google Scholar]
- 23. Glukhov AV, Fedorov VV, Lou Q, Ravikumar VK, Kalish PW, et al. (2010) Transmural dispersion of repolarization in failing and nonfailing human ventricle. Circ Res 106: 981–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Antzelevitch C (2007) Heterogeneity and cardiac arrhythmias: an overview. Heart Rhythm 4: 964–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Marionneau C, Couette B, Liu J, Li H, Mangoni ME, et al. (2005) Specific pattern of ionic channel gene expression associated with pacemaker activity in the mouse heart. J Physiol 562: 223–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25: 402–408. [DOI] [PubMed] [Google Scholar]
- 27. Eisen MB, Spellman PT, Brown PO, Botstein D (1998) Cluster analysis and display of genome-wide expression patterns. Proc Natl Acad Sci U S A 95: 14863–14868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Janse MJ (2004) Electrophysiological changes in heart failure and their relationship to arrhythmogenesis. Cardiovasc Res 61: 208–217. [DOI] [PubMed] [Google Scholar]
- 29. Aiba T, Tomaselli GF (2010) Electrical remodeling in the failing heart. Curr Opin Cardiol 25: 29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Flagg TP, Nichols CG (2005) Sarcolemmal K(ATP) channels: what do we really know? J Mol Cell Cardiol 39: 61–70. [DOI] [PubMed] [Google Scholar]
- 31. Kaab S, Dixon J, Duc J, Ashen D, Nabauer M, et al. (1998) Molecular basis of transient outward potassium current downregulation in human heart failure: a decrease in Kv4.3 mRNA correlates with a reduction in current density. Circulation 98: 1383–1393. [DOI] [PubMed] [Google Scholar]
- 32. Zicha S, Xiao L, Stafford S, Cha TJ, Han W, et al. (2004) Transmural expression of transient outward potassium current subunits in normal and failing canine and human hearts. J Physiol 561: 735–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Soltysinska E, Olesen SP, Christ T, Wettwer E, Varro A, et al. (2009) Transmural expression of ion channels and transporters in human nondiseased and end-stage failing hearts. Pflugers Arch 459: 11–23. [DOI] [PubMed] [Google Scholar]
- 34. Ellinghaus P, Scheubel RJ, Dobrev D, Ravens U, Holtz J, et al. (2005) Comparing the global mRNA expression profile of human atrial and ventricular myocardium with high-density oligonucleotide arrays. J Thorac Cardiovasc Surg 129: 1383–1390. [DOI] [PubMed] [Google Scholar]
- 35. Shanmugam M, Molina CE, Gao S, Severac-Bastide R, Fischmeister R, et al. (2011) Decreased sarcolipin protein expression and enhanced sarco(endo)plasmic reticulum Ca(2+) uptake in human atrial fibrillation. Biochem Biophys Res Commun 410: 97–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Iacobas DA, Iacobas S, Thomas N, Spray DC (2010) Sex-dependent gene regulatory networks of the heart rhythm. Funct Integr Genomics 10: 73–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Van Wagoner DR (2003) Electrophysiological remodeling in human atrial fibrillation. Pacing Clin Electrophysiol 26: 1572–1575. [DOI] [PubMed] [Google Scholar]
- 38. Gaborit N, Steenman M, Lamirault G, Le Meur N, Le Bouter S, et al. (2005) Human atrial ion channel and transporter subunit gene-expression remodeling associated with valvular heart disease and atrial fibrillation. Circulation 112: 471–481. [DOI] [PubMed] [Google Scholar]
- 39. Workman AJ, Kane KA, Rankin AC (2008) Cellular bases for human atrial fibrillation. Heart Rhythm 5: S1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Van Wagoner DR, Pond AL, McCarthy PM, Trimmer JS, Nerbonne JM (1997) Outward K+ current densities and Kv1.5 expression are reduced in chronic human atrial fibrillation. Circ Res 80: 772–781. [DOI] [PubMed] [Google Scholar]
- 41. Brandt MC, Priebe L, Bohle T, Sudkamp M, Beuckelmann DJ (2000) The ultrarapid and the transient outward K(+) current in human atrial fibrillation. Their possible role in postoperative atrial fibrillation. J Mol Cell Cardiol 32: 1885–1896. [DOI] [PubMed] [Google Scholar]
- 42. Dobrev D, Wettwer E, Kortner A, Knaut M, Schuler S, et al. (2002) Human inward rectifier potassium channels in chronic and postoperative atrial fibrillation. Cardiovasc Res 54: 397–404. [DOI] [PubMed] [Google Scholar]
- 43. Yue L, Feng J, Gaspo R, Li GR, Wang Z, et al. (1997) Ionic remodeling underlying action potential changes in a canine model of atrial fibrillation. Circ Res 81: 512–525. [DOI] [PubMed] [Google Scholar]
- 44. Van Wagoner DR, Pond AL, Lamorgese M, Rossie SS, McCarthy PM, et al. (1999) Atrial L-type Ca2+ currents and human atrial fibrillation. Circ Res 85: 428–436. [DOI] [PubMed] [Google Scholar]
- 45. Bosch RF, Zeng X, Grammer JB, Popovic K, Mewis C, et al. (1999) Ionic mechanisms of electrical remodeling in human atrial fibrillation. Cardiovasc Res 44: 121–131. [DOI] [PubMed] [Google Scholar]
- 46. Workman AJ (2010) Cardiac adrenergic control and atrial fibrillation. Naunyn Schmiedebergs Arch Pharmacol 381: 235–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ramaekers D, Ector H, Aubert AE, Rubens A, Van de Werf F (1998) Heart rate variability and heart rate in healthy volunteers. Is the female autonomic nervous system cardioprotective? Eur Heart J 19: 1334–1341. [DOI] [PubMed] [Google Scholar]
- 48. Nerbonne JM, Kass RS (2005) Molecular physiology of cardiac repolarization. Physiol Rev 85: 1205–1253. [DOI] [PubMed] [Google Scholar]
- 49. Antzelevitch C, Fish J (2001) Electrical heterogeneity within the ventricular wall. Basic Res Cardiol 96: 517–527. [DOI] [PubMed] [Google Scholar]
- 50.Tellez J, Maczewski M, Yanni J, Sutyagin P, Mackiewicz U, et al. (2011) Ageing-Dependent Remodelling of Ion Channel and Ca2+ Clock Genes UnderlyingSinoatrial Node Pacemaking. Exp Physiol. [DOI] [PubMed]
- 51. Boheler KR, Volkova M, Morrell C, Garg R, Zhu Y, et al. (2003) Sex- and age-dependent human transcriptome variability: implications for chronic heart failure. Proc Natl Acad Sci U S A 100: 2754–2759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, et al. (2001) Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 285: 2370–2375. [DOI] [PubMed] [Google Scholar]
- 53. Wang TJ, Larson MG, Levy D, Vasan RS, Leip EP, et al. (2003) Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: the Framingham Heart Study. Circulation 107: 2920–2925. [DOI] [PubMed] [Google Scholar]
- 54. Nattel S, Burstein B, Dobrev D (2008) Atrial remodeling and atrial fibrillation: mechanisms and implications. Circ Arrhythm Electrophysiol 1: 62–73. [DOI] [PubMed] [Google Scholar]
- 55. Bui AL, Horwich TB, Fonarow GC (2011) Epidemiology and risk profile of heart failure. Nat Rev Cardiol 8: 30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, et al. (1994) Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 271: 840–844. [PubMed] [Google Scholar]
- 57. Brundel BJ, Henning RH, Kampinga HH, Van Gelder IC, Crijns HJ (2002) Molecular mechanisms of remodeling in human atrial fibrillation. Cardiovasc Res 54: 315–324. [DOI] [PubMed] [Google Scholar]
- 58. Tomaselli GF, Marban E (1999) Electrophysiological remodeling in hypertrophy and heart failure. Cardiovasc Res 42: 270–283. [DOI] [PubMed] [Google Scholar]
- 59. Antzelevitch C, Shimizu W, Yan GX, Sicouri S, Weissenburger J, et al. (1999) The M cell: its contribution to the ECG and to normal and abnormal electrical function of the heart. J Cardiovasc Electrophysiol 10: 1124–1152. [DOI] [PubMed] [Google Scholar]
- 60. Roden DM, Kupershmidt S (1999) From genes to channels: normal mechanisms. Cardiovasc Res 42: 318–326. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hierarchical Cluster Analysis. (A) Cluster analysis of ischemic and nonfailing LA/LV samples of both genders showing distinct separation based on cardiac location. (B) Cluster analysis of ischemic, nonischemic, and nonfailing LV samples showing no clustering. (C) Cluster analysis of nonischemic and nonfailing epicardial/endocardial samples also showing no clustering.
(TIF)
Custom-designed Taqman low-density gene array targets.
(DOCX)