Abstract
A thorough knowledge of the anatomy of the shoulder is essential for the assessment of its condition. The purpose of this article is to provide a useful tool for the ultrasound (US) study of this joint. The shoulder girdle and upper arm are made up of a number of muscles and tendons: rotator cuff (supraspinatus, infraspinatus, teres minor and subscapularis), humeral biceps, deltoid and pectoral muscles, which can all be evaluated at US examination. Various and complex capsular ligamentous structures contribute to the stability of the shoulder, but only a few can be adequately evaluated by US and will therefore receive particular attention. Numerous serous bursae are situated among muscles, skin, subcutaneous tissues, joint capsule structures and bones to prevent friction and they can be evaluated by US only in the presence of pathologies. Subacromial-subdeltoid and subcoracoid bursa are most frequently involved and will therefore be described in detail. There are furthermore nerves and vessels providing the various components of the shoulder with innervation and vascularization, and they can also be studied by US. The shoulder girdle (humerus, scapula, clavicle and sternal manubrium) is situated in the deep layers; only the cortex of the bone can be seen at US as a continuous hyperechoic line. For a better understanding of the location and relationship between the structures which can be studied by US, magnetic resonance imaging (MRI) can be carried out as this method provides a wider and more complete view of the structures.
Keywords: Shoulder, Ultrasound, Rotator cuff, Acromialclavicular joint, Sternoclavicular joint
Sommario
La conoscenza dell’anatomia della spalla è fondamentale per la valutazione della sua patologia. Scopo del presente articolo è di fornire un adeguato strumento per la conoscenza dell’anatomia e dell’anatomia ecografica di quest’articolazione.
Numerosi muscoli e rispettivi tendini partecipano al cingolo scapolo-omerale: i costituenti la cuffia dei rotatori (sovraspinato, sottospinato, piccolo rotondo e sottoscapolare), il bicipite omerale, il deltoide e i muscoli grande e piccolo pettorale, tutti valutabili ecograficamente. Varie e complesse strutture capsulo-legamentose contribuiscono alla stabilità della spalla, solo alcune sono ben valutabili ecograficamente e saranno pertanto prese in considerazione in maniera paticolare. Tra muscoli, cute e sottocute, strutture capsulo-articolari e ossee si trovano numerose borse sierose il cui ruolo è quello di evitare l’attrito, sono valutabili ecograficamente esclusivamente in presenza di patologia; le borse subacromio-deltoidea e sottocoracoidea sono quelle più frequentemente interessate da patologia e saranno, pertanto, descritte dettagliatamente. Sono inoltre presenti nervi e vasi che forniscono innervazione e irrorazione ai vari componenti della spalla, anch’essi valutabili ecograficamente. In profondità si riconoscono le ossa del cingolo (omero, scapola, clavicola e manubrio sternale); dell’osso è valutabile ecograficamente solo la corticale come linea iperecogena continua.
Per una più semplice comprensione della disposizione spaziale e dei rapporti delle strutture valutabili ecograficamente si fa riferimento ad immagini di risonanza magnetica, caratterizzate da una maggiore panoramicità.
Introduction
The shoulder is a complex joint due to its anatomy and versatile range of movement, and it is therefore frequently affected by diseases of complex etiology [1,2]. Ultrasound (US) examination can thus not be exclusively dedicated to the study of the tendons, as tendon pathologies are often closely related to the functionality and stability of the shoulder joint [2]. For this reason, the US operator carrying out the examination of the shoulder must be thoroughly familiar with the anatomy of the structures which are normally studied by US, i.e. tendons and muscles, but also with all the other structures forming the joint such as serous bursae, ligaments, nerves and bones in order to integrate and correctly interpret clinical and instrumental findings [3].
The US operator should furthermore remember that the shoulder is made up not only of the scapulohumeral joint, but also of the acromioclavicular joint and functionally the sternoclavicular joint, where possible pathologies may cause shoulder pain [3].
This article therefore offers a complete revision of the US anatomy of the shoulder with images illustrating the various structures with integration of magnetic resonance imaging (MRI) and arthro-MRI in order to provide a better overall understanding of the anatomy.
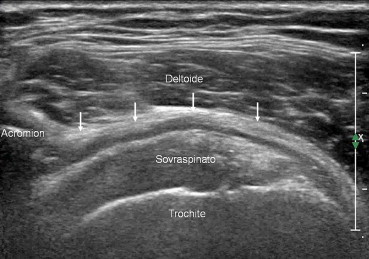
Supraspinatus muscle
The supraspinatus muscle arises from the central part of the supraspinatus fossa of the scapula; it laterally crosses the joint capsule and attaches to it, passes under the acromion and the coracoacromial ligament, then fans out horizontally and inserts to the superior and medial facets of the greater tuberosity of the humerus (Fig. 1A and B) [1,4]. The superficial part of the muscle is covered by the fascia supraspinata and enters in contact with the deltoid and trapezius muscles whereas the deep fascia attaches to the joint capsule. The tendon insertion to the greater tuberosity of the humerus is extended [1,5]. When contracted, it abducts and externally rotates the arm, and together with the deltoid muscle it also contributes to the stabilization of the shoulder joint. It is innervated by the suprascapular nerve [1,4].
Fig. 1.
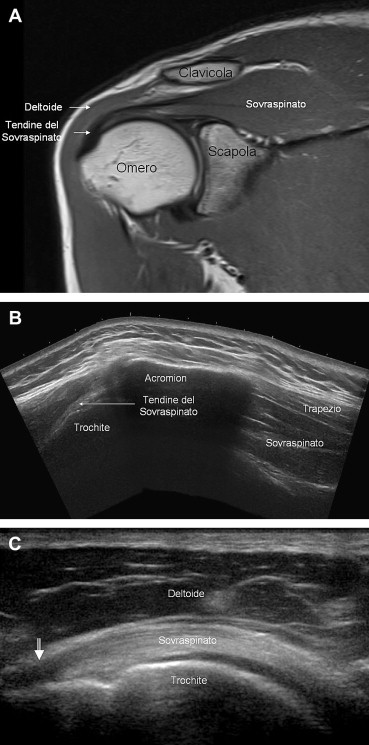
Supraspinatus. The supraspinatus muscle arises from the supraspinatus fossa of the scapula; it laterally crosses the joint capsule and attaches to it, passes under the acromion and the coracoacromial ligament and is inserted as a flattened tendon to the upper and middle facet of the greater tuberosity of the humerus (A, B). US shows normal fibrillar tendon appearance with reduced echogenicity at the insertion (C) which is often due to anisotropy (arrow), an artifact that should not be confused with tendinosis.
US appearance of the supraspinatus tendon and muscle under physiological conditions is the normal image of tendons and muscles; a reduced echogenicity of the tendon at the point of insertion is often due to anisotropy (Fig. 1C) [5], i.e. an artifact which should not be confused with tendinosis.
Infraspinatus muscle
The infraspinatus muscle arises from the central part of the infraspinous fossa, the spine of the scapula, the infraspinatus fascia and the intermuscular septa separating it from the teres minor muscle (Fig. 2 A and B). Its fibers run obliquely upwards ending in a tendon that attaches to the joint capsule and inserts to the middle facet of the greater tuberosity of the humerus. It comes in contact with the trapezius and deltoid muscles as well as the subcutaneous tissue. The deep portion is in close contact with the infraspinatus fossa and the joint capsule, whereas the superficial portion is covered by the infraspinatus fascia. When activated it externally rotates the arm, strengthening and stabilizing the joint capsule. It is innervated by the suprascapular nerve [1,4]. The US image is characterized by a central aponeurosis giving rise to the tendon (Fig. 2B).
Fig. 2.
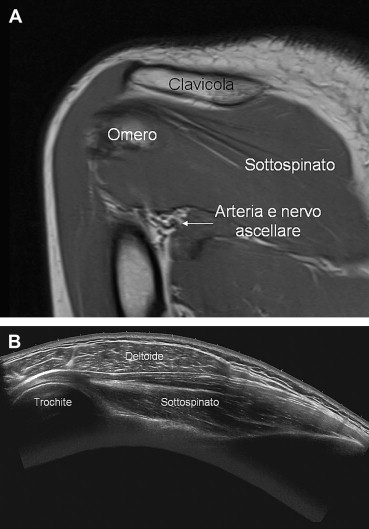
Infraspinatus. The infraspinatus muscle originates from the infraspinatus fossa, the spine of the scapula, the infraspinatus fascia and intermuscular septa; it runs obliquely upwards and ends in a tendon that attaches to the joint capsule and inserts to the middle facet of the greater tuberosity of the humerus (A, B). US image is characterized by the central aponeurosis giving origin to the tendon (B).
Teres minor muscle
The teres minor muscle arises from the infraspinous fossa above the teres major muscle; it runs parallel to the infraspinatus muscle (Fig. 3) and inserts to the inferior facet of the greater tuberosity of the humerus through a short tendon that attaches to the fibrous layer of the joint capsule. The posterior portion is in close contact with the deltoid and teres major muscles, and the anterior portion is in contact with the subscapularis muscle and the joint capsule. It works with the infraspinatus muscle externally rotating the arm and has a stabilizing effect on the shoulder joint. It is innervated by the axillary nerve [1,4]. The US image is similar to that of the infraspinatus muscle characterized by a central aponeurosis ending in a short tendon.
Fig. 3.

Teres minor. The teres minor muscle originates from the infraspinatus fossa; it runs parallel to the infraspinatus and inserts to the lower facet of the greater tuberosity of the humerus through a short tendon attaching to the fibrous joint capsule.
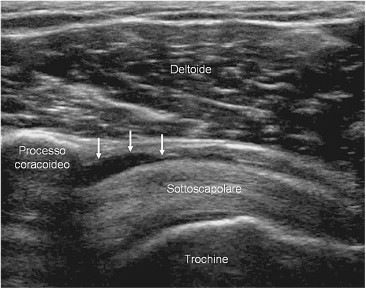
Subscapularis muscle
The subscapularis muscle arises in the subscapular fossa; its four muscle bellies run obliquely upward, converge in a strong tendon that passes below the coracoid process in front of the glenohumeral joint and reaches the lesser tuberosity of the humerus where it is inserted (Fig. 4A and B).Some of the most superficial fibers insert to the crest of the lesser tubercle strengthening the transverse humeral ligament. The posterior portion is in close contact with the subscapular fossa, the anterior portion is in contact with the serratus anterior muscle and the neurovascular bundle. It abducts andinternally rotatesthearm and stabilizes the shoulder [1,4]. It is innervated by the subscapular nerve. The US image is typical of multipennate muscles with aponeuroses ending in a tendon (Fig. 4C).
Fig. 4.
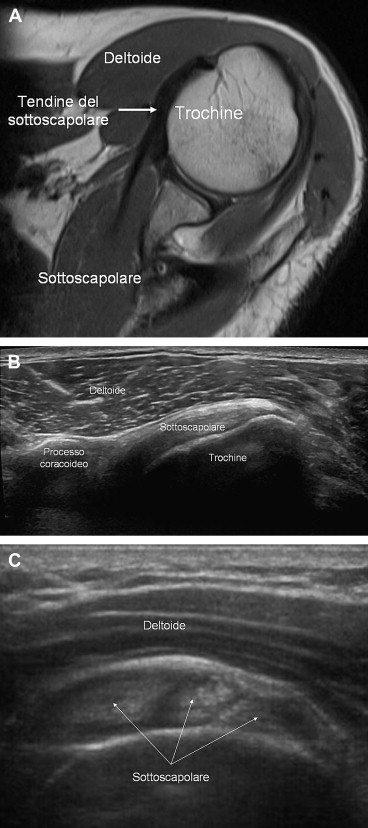
Subscapularis. The subscapularis muscle originates from the subscapular fossa; its four muscle bellies are directed obliquely upward, converging in a strong tendon that passes below the coracoid process in front of the glenohumeral joint and reaches the lesser tuberosity of the humerus where it inserts (A, B). US appearance (C) is typical of multipennate muscles with aponeurosis (arrows) ending in a tendon.
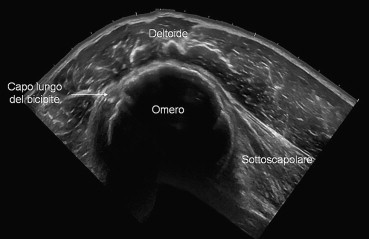
Biceps brachii muscle
The biceps brachii muscle arises from the scapula with two heads: the long and short head.
The long head (Fig. 5) situated on the side originates from the supraglenoid tubercle of the scapula and the adjacent portion of the glenoid labrum. It passes along the shoulder joint, moves into the intertubercular groove of the humerus and becomes extraarticular although surrounded by a serous sheath caused by extroversion of the synovial capsule of the glenohumeral joint [5].
Fig. 5.
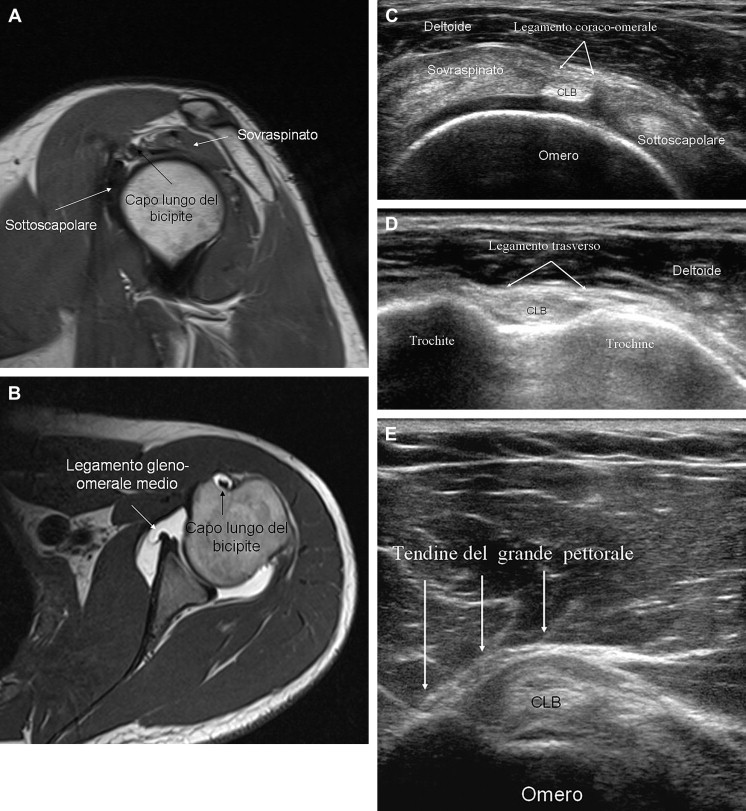
Biceps. The biceps muscle originates from the scapula with two heads: the long and short head. The long head located on the side originates from the supraglenoid tubercle of the scapula and the adjacent portion of the glenoid labrum. It passes along the shoulder joint and moves into the intertubercular groove of the humerus, becomes extraarticular although surrounded by a serous sheath, as an extroversion of the synovial fluid of the glenohumeral joint (A, B). It is stabilized by the coracohumeral ligament (C) through (D) and the tendon of the pectoralis major (E), which crosses it and inserts into the pectoral tubercle of the humerus. US image shows normal fibrillar tendon appearance; in the study of the long head of the biceps, short-axis scans are usually sufficient (C, D, E).
The short head beneath the long head arises from the apex of the coracoid process of the scapula and moves downwards; the two heads are united in a single muscle belly which gives rise to a tendon that inserts to the bicipital tuberosity of the radius and aponeurosis (fibrous tendon), which expands medially and downward and merges with the antebrachial fascia.
The biceps brachii muscle is the main flexor muscle of the arm and forearm and its secondary action is supination. It is also involved in the movements of adduction (short head), abduction and internal rotation (long head); it stabilizes the shoulder joint and is in turn stabilized by the coracohumeral ligament (Fig. 6C) through (Fig. 5D) and by the pectoralis major tendon (Fig. 6E), which crosses it to insert to the pectoral tubercle of the humerus. It is innervated by the musculocutaneous nerve [1,4]. Unlike most tendons that must be evaluated in two orthogonal scans (long-axis and short-axis), short-axis scans are usually sufficient in the study of the long head of the biceps. US appearance is the usual one in tendons, i.e. fibrillar.
Fig. 6.
Deltoid. The deltoid muscle covers the lateral portion of the shoulder. It is a flat, triangular muscle consisting of three parts: the anterior portion originating from the lateral third of the anterior margin of the clavicle, the middle portion originating from the apex and the lateral margin of the acromion and the posterior portion originating from the lower lip of the spine of the scapula; it is inserted at the level of the deltoid tuberosity of the humerus. US appearance is typical of multipennate muscles with aponeurosis and muscle bundles.
Deltoid muscle
The deltoid muscle (Fig. 6) covers the lateral portion of the shoulder joint. It is a flat, triangular muscle consisting of three parts: the anterior portion originating from the lateral third of the anterior margin of the clavicle, the medial portion originating from the apex and lateral margin of the acromion and the posterior portion originating from the lower lip of the spine of the scapula. It inserts to the deltoid tuberosity of the humerus. The surface is covered by the deltoid fascia whereas the deep-lying portion covers the shoulder joint. The deltoid muscle abducts the arm to 90°, and it also has a small role in flexion, adduction and external rotation. It is innervated by the axillary nerve [1,4]. The US image is typical of multipennate muscles showing aponeuroses and muscle bundles.
Pectoralis major muscle
The pectoralis major muscle is situated in front of the chest and forms the anterior axillary wall. It consists of three parts: the clavicular portion originating from the medial two-thirds of the anterior clavicular margin, the sternum-rib portion originating from the anterior surface of the sternum and the cartilage of the first six ribs, and the abdominal portion originating from the anterior leaflet of the rectus abdominis sheath. They all end in a flat tendon which is inserted into the lateral lip of the intertubercular groove of the humerus. The pectoralis major muscle moves forward and rotates within the humerus. It is innervated by the brachial plexus [1,4].
Pectoralis minor muscle
The pectoralis minor muscle is situated deep beneath the pectoralis major muscle. It originates from the external surface of the third, fourth and fifth ribs. The three bundles are united to form a muscle belly that moves laterally upward and is inserted into the apex and the medial margin of the coracoid process of the scapula. Along with pectoralis major, it forms the anterior axillary wall. The pectoralis minor muscle depresses the point of the shoulder and raises the ribs. It is innervated by the brachial plexus [1,4].
Subacromial-subdeltoid bursa and subcoracoid bursa
The subacromial-subdeltoid bursa (Fig. 7) is a synovial structure situated below the clavicle, acromion and coracoacromial ligament and above the rotator cuff [3,5,6]. Under physiological conditions it does not communicate with the glenohumeral joint but it may communicate with the joint cavity after a full-thickness supraspinatus tendon tear [1,3,5,6]. The bursa is surrounded by a thin layer of peribursal fat, and under pathological conditions it is easily detectable at US examination (Fig. 7) [1,6]; it is situated deep beneath the deltoid muscle and under the acromion and coracoacromial ligament in front of the supraspinatus tendon. It extends forward and downward and covers the bicipital groove, while its rear and side boundaries may vary. However, it generally reaches a level situated about 3 cm over the greater tuberosity of the humerus [6]. It may lie in continuity with the subcoracoid bursa.
Fig. 7.
Subacromial-subdeltoid bursa. The subacromial-subdeltoid bursa is a synovial structure situated beneath the clavicle, acromion and coracoacromial ligament and over the rotator cuff.At US examination it is detectable in pathological conditions (arrows).
The subcoracoid bursa (Fig. 8) is situated below and medially to the acromion near the joint capsule and the subscapularis tendon [1]. Under physiological conditions it does not communicate with the joint cavity [6]. Both bursae are there to reduce friction between the tendons and the surrounding osteofibrous structures. In physiological circumstances, bursae cannot be seen directly on the US image, but only the peribursal fat that appears as a hyperechoic line [1,5,7].
Fig. 8.
Subcoracoid bursa. The subcoracoid bursa is situated below the acromion near the underlying joint capsule and the subscapularis tendon. Under physiological conditions it does not communicate with the joint cavity. It can be visualized at US examination when the area is affected by pathology (arrows).
Glenohumeral joint: capsular-ligamentous structures
The glenohumeral joint is an enarthrosis whose articular surface is the humeral head, which appears as a one-third of a sphere, smooth and covered by articular cartilage, which is thicker in the center, and the glenoid cavity, which is oval and shallow and less extended than the humeral head (Fig. 1). Also the latter is covered by articular cartilage, which is thinner at the periphery [1,4,6].
The congruence between the two bone surfaces is increased by the glenoid labrum applied to the glenoid circumference. The glenoid labrum is triangular in section with its inner surface facing the joint cavity, and it is attached to the underlying glenoid cartilage [1,4,6]; its external side provides the insertion into the joint capsule. There are anatomical variants of the glenoid labrum, particularly cranially, where a sublabral foramen sometimes lies between the glenoid labrum and the underlying cartilage [8]. The glenoid labrum is poorly visualized at US examination [1,9,10]. Some authors have described its pathological aspects [10], but currently US cannot be considered as a reliable method for studying it [1].
The joint capsule is loose; it inserts medially at the circumference of the glenoid, and externally it reaches the anatomical neck of the humerus with a number of caudal insertions which varies from patient to patient. Synovium lines the entire inside of the joint and also covers the proximal portion of the long head of the biceps tendon. The joint is stabilized by the capsule, the thickening, the glenohumeral ligaments and a distant ligament, i.e. the coracohumeral ligament [1,4]. There are three glenohumeral ligaments: the upper, the middle, and the lower glenohumeral ligament. The upper glenohumeral ligament is normally thin [1,4,6]; it originates from the top edge of the glenoid labrum and scapular neck and crosses externally below the coracohumeral ligament and inserts to the lesser tuberosity of the humerus. The middle glenohumeral ligament arises from the anterior third of the upper glenoid labrum and from the neck of the scapula; it runs obliquely in the inferior external direction until it inserts to the lower portion of the lesser tuberosity converging with the deep portion of the subscapularis tendon [1,4,6]. The middle glenohumeral ligament may present variants; the best known is hypertrophy with or without hypoplasia or absence of the anterosuperior margin of the glenoid labrum (in case of absence the anatomy is known as the Buford complex) [8]. Between the lower edge of the upper glenohumeral ligament and the upper edge of the middle glenohumeral ligament the Weitbrecht foramen is situated, an opening which connects the joint cavity with the subscapularis recess (virtual under physiological conditions) surrounding the subscapularis tendon below the coracoid [6]. This recess should not be confused with the subcoracoid bursa [1]. The lower glenohumeral ligament is the largest of the glenohumeral ligaments extending from the glenoid labrum and scapular neck for almost the entire circumference to the lesser tuberosity of the humerus. It has an anterior and a posterior arm which delimit the axillary recess. Between the lower edge of the middle glenohumeral ligament and the upper edge of the anterior arm of the lower glenohumeral ligament, the Rouviere foramen is situated which may provide communication between the joint capsule and the subcoracoid bursa [1,4,6].
In addition to the axillary and subscapular recess, the joint capsule has a further anterior biceps recess, i.e. the tendon sheath of the long head of the biceps. The coracohumeral ligament is a distant stabilizer of the scapular-humeral joint; it is a strong fibrous band stretching between the coracoid and the greater tuberosity of the humerus. It forms the roof of the rotator cuff interval consisting of the intra-articular portion of the long head of the biceps tendon and the proximal humerus [1,3]. US examination does not provide an adequate study of most of the articular structures and capsular ligaments which must be assessed using CT arthrography or MR arthrography (Fig. 5B) [1,8].
Coracoacromial ligament
The coracoacromial ligament (Fig. 9) is a triangular fibrous band stretching between the end of the acromion and the coracoid process; it completes the osteofibrous arch above the glenohumeral joint. It is covered by the deltoid muscle and it covers the surface of the rotator cuff [1,4,6]. This ligament can be evaluated at US examination.
Fig. 9.
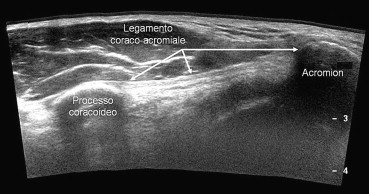
Coracoacromial ligament. The coracoacromial ligament is a triangular fibrous band stretching between the end of the acromion and the external margin of the coracoid process; it completes the osteofibrous surface overlying the glenohumeral joint.
Acromioclavicular joint and coracoclavicular ligament
The acromioclavicular joint is an arthrodial joint connecting the lateral end of the clavicle and the medial end of the acromion (Fig. 10). Both articular bone heads present smooth facets covered in hyaline cartilage and interposition of a fibrous disk [1,4,6]. The joint capsule is reinforced proximally by the acromioclavicular ligament and fibrous bundles of the deltoid and trapezius muscles, and the joint is stabilized by a distant ligament, the coracoclavicular ligament [1,4,6].
Fig. 10.
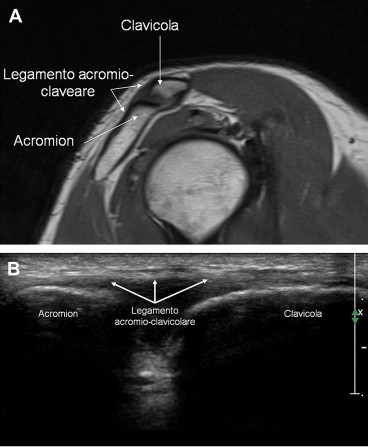
Acromioclavicular joint. The acromioclavicular joint is an arthrodial joint that connects the lateral end of the clavicle with the medial end of the acromion. The joint capsule is reinforced proximally by the acromioclavicular ligament and fibrous bundles of the deltoid and trapezius muscles.
The coracoclavicular ligament consists of two bundles: the trapezoid and conoid ligaments. The trapezoid ligament is a strong quadrilateral fibrous lamina stretching between the upper surface of the coracoid and the coracoid tuberosity of the clavicle. It lies in front of the conoid ligament and is triangular with an apex that attaches to the base of the coracoid and fibers that diverge in a fan and insert into the coracoid tuberosity of the clavicle [4,6].
Sternoclavicular joint
The sternoclavicular joint is the only joint that connects the shoulder girdle and upper arm to the chest [1]. The joint heads involved are the medial end of the clavicle, the manubrium of the sternum and the first rib. The joint surfaces are flat and incongruous with interposition of a fibrous disc dividing the joint into two synovial compartments which do not communicate: the medial and lateral compartment. The joint is reinforced by the joint capsule, the strong sternoclavicular ligament situated anterior cranially, the interclavicular ligaments [1,3,4,6] and, at a distance, the costoclavicular ligament.
Vascular structures
Blood supply to the shoulder girdle and upper arm occurs through the axillary artery which distally, at the lateral margin of the pectoralis minor muscle, is divided into three branches: the anterior humeral circumflex artery (Fig. 11), the artery of the back (Fig. 12) and the subscapular artery. The circumflex arteries cross each other and form an anastomotic ring [1,4].
Fig. 11.
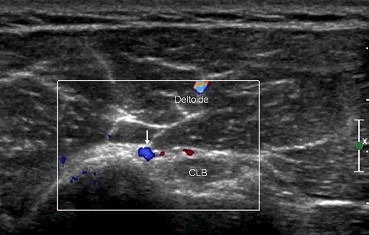
Ascending branch of the anterior circumflex artery. The arcuate artery, anterior branch of the circumflex artery (arrow) passes beneath the transverse ligament and runs parallel to the long head of the biceps tendon. Color Doppler may help identifying it.
Fig. 12.
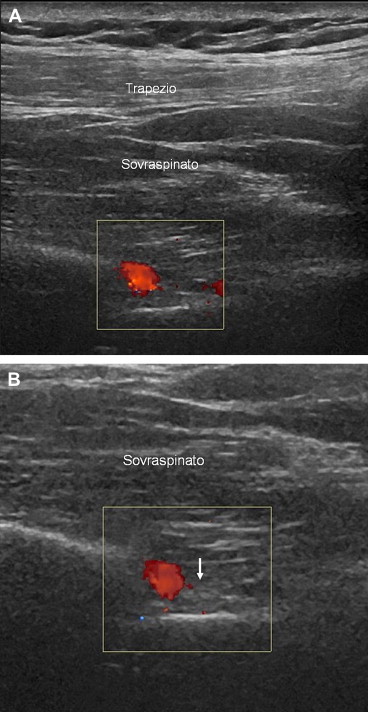
Arteries and suprascapular nerve. At the level of the supraglenoid fossa, US can evidence the suprascapular artery and nerve. Color Doppler is helpful in identifying the artery, while the nerve near the artery (arrow) shows the typical fascicular pattern.
Neural structures
The rotator cuff muscles are innervated by the suprascapular nerve (supra- and infraspinatus), the subscapular nerve (subscapularis) and the axillary nerve (teres minor) [1,4]. It is necessary to know the course of these nerves in the area studied at US examination in order to rule out lesions such compression due to paralabral cysts [1,3]. The suprascapular nerve originates from the brachial plexus upper trunk (C5 C6), runs inferiorly through the suprascapular foramen, whose floor is the supraspinatus notch of the scapula, passes through the supraspinatus fossa through the spinoglenoid notch and finally reaches the infraspinatus fossa [1,3,4].
The axillary nerve originates from the posterior portion of the brachial plexus upper trunk (C5 C6), descends to the inferior, lateral margin of the subscapularis muscle and reaches the bottom margin of the glenohumeral joint capsule where it is runs posteriorly. The nerve, together with the posterior circumflex artery, passes through the quadrilateral space delimited medially by the long head of triceps brachii, laterally by the surgical neck of the humerus, cranially by teres minor and beneath by teres major; its terminal branches innervate teres minor and the deltoid muscle [1,4].
Conclusions
US has for a long time been considered a highly effective means of studying tendon disorders of the shoulder [1,3,5], and medical doctors who carry out US examinations to evaluate osteoarticular diseases must therefore be thoroughly familiar with these anatomical structures. However, it should not be forgotten that also the adjacent structures should be evaluated; they are generally well displayed, but often neglected in daily practice, such as the acromioclavicular joint, blood vessels and nerves [1,3] in order to fully exploit the diagnostic possibilities of the method and identify frequent diseases which are easily diagnosed by US. It is also important to be familiar with the anatomical structures which are poorly evaluated at US, which are more accurately investigated using other diagnostic imaging methods in order to assess not only part of the problem, which often happens in these pathologies, but to identify the disease in a wider context and thereby assist the clinician in a more meaningful way. A US study should not be exclusively dedicated to tendon pathologies as they are often closely related to the functionality and stability of the shoulder joint [2]. A perfect knowledge of the entire anatomy is therefore required of those who carry out US examinations of the shoulder. Familiarity with this anatomy is necessary also to perform US guided interventional procedures [11].
Conflict of interest statement
The authors have no conflict of interest.
References
- 1.Bianchi S., Martinoli C. Springer-Verlag; 2007. Ultrasound of the musculoskeletal system: sholuder. 190–331. [Google Scholar]
- 2.Yin B., Vella J., Levine W.N. Arthroscopic alphabet soup: recognition of normal, normal variants, and pathology. Orthop Clin North Am. 2010 Jul;41(3):297–308. doi: 10.1016/j.ocl.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Martinoli C., Bianchi S., Prato N., Pugliese F., Zamorani M.P., Valle M. US of the shoulder: non-rotator cuff disorders. Radiographics. 2003 Mar-Apr;23(2):381–401. doi: 10.1148/rg.232025100. [DOI] [PubMed] [Google Scholar]
- 4.Aa Vv: Anatomia Umana vol 1. Edi Ermes 1990. 203–265.
- 5.Chevrot A. Masson Ed Italia; 1995. Artro-TC: spalla. 47–56. [Google Scholar]
- 6.Rutten M.J., Jager G.J., Blickman J.G. US of the rotator cuff: pitfalls, limitations and artefacts. Radiographics. 2006;26:589–604. doi: 10.1148/rg.262045719. [DOI] [PubMed] [Google Scholar]
- 7.Van Holsbeeck M., Strouse P.J. Sonography of the shoulder: evaluation of the subacromial-subdeltoid bursa. AJR Am J Roentgenol. 1993;160:561–564. doi: 10.2214/ajr.160.3.8430553. [DOI] [PubMed] [Google Scholar]
- 8.Beltran J., Bencardino J., Mellado J., Rosenberg Z.S., Irish R.D. MR Arthrography of the shoulder: variants and pitfalls. Radiographics. 1997;17:1403–1412. doi: 10.1148/radiographics.17.6.9397454. [DOI] [PubMed] [Google Scholar]
- 9.Rasmussen O.S. Anterior shoulder instability: sonographic evaluation. J Clin Ultrasound. 2004;32:430–437. doi: 10.1002/jcu.20064. [DOI] [PubMed] [Google Scholar]
- 10.Hammar M.V., Wintzell G.B., Åström K.G., Larsson S., Elvin A. Role of US in the preoperative evaluation of patients with anterior shoulder instability. Radiology. 2001;219:29–34. doi: 10.1148/radiology.219.1.r01mr1329. [DOI] [PubMed] [Google Scholar]
- 11.Draghi F., Robotti G., Jacob D., Bianchi S. Interventional musculoskeletal ultrasonography: precautions and contraindications. Journal of Ultrasound. 2010;13(3):126–133. doi: 10.1016/j.jus.2010.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


