Abstract
A wide variety of atypical presentations with complications affecting multiple organ systems during acute infectious mononucleosis (IM) is described in the literature, with an increase in the number of teenagers who are susceptible to a severe case of the disease. We report a case of a 14-year-old girl with severe IM and acute abdominal pain. Ultrasonographic (US) evaluation showed a marked thickening of the gallbladder wall (GBW) with enlargement of some mesenteric lymph nodes. CT scan showed multiple enlarged lung nodules of various sizes and a small pleural and pericardial effusion; a hypodense solid mass of unknown etiology was detected in the anterior mediastinum, mimicking a malignant tumor. Hematological analysis of peripheral blood smear was performed to exclude neoplastic pathology. IM was identified as the only underlying disease. The patient was carefully monitored: clinical evaluation, laboratory analysis and US examination were repeated at weekly intervals, until recovery.
Keywords: Severe EBV-infection, Adolescents, Gallbladder, Ultrasonography
Sommario
Gli adolescenti possono talvolta presentare forme aggressive di mononucleosi infettiva (MI), che si manifestano con quadri atipici e aspecifici e si accompagnano a complicanze di diversa gravità a carico di vari organi e apparati. Riportiamo il caso di una ragazza di 14 anni, giunta alla nostra osservazione per un quadro di mononucleosi infettiva (MI) e dolore addominale acuto; le indagini diagnostiche evidenziavano all'ecografia addominale la presenza di ispessimento della parete colecistica (>3 mm) con versamento pericolecistico e di linfonodi ingranditi all'ilo epatico; alla TC veniva confermato il quadro ecografico addominale e si evidenziava inoltre una massa solida ipodensa a livello del mediastino anteriore, con versamento pleurico e pericardico e presenza di numerosi linfonodi mediastinici ingranditi. Data la gravità del quadro, è stato necessario escludere patologie neoplastiche. La paziente è stata attentamente monitorizzata durante la degenza, ed ha presentato una completa, ma lenta risoluzione dei sintomi.
Introduction
Infectious mononucleosis (IM) is a typical self-limited lymphoproliferative illness, usually characterized by fever, pharyngitis and lymphadenopathy. Nonetheless, a wide variety of atypical presentations with complications affecting multiple organ systems during acute IM, is described in the literature [1,2] with an increase in the number of teenagers who are susceptible to a severe case of the disease. The great variability of the clinical picture makes the diagnosis difficult and questionable: serological outcome is gold standard, but the radiological spectrum is useful when symptoms persist or are unusually prominent.
Case report
A 14-year-old girl was admitted to the Department of Pediatrics, University of Chieti, Italy, with a 10-day history of persistent fever, cervical and inguinal lymphadenopathy, tonsillar pharyngitis and hepatosplenomegaly. She complained of acute abdominal pain in the upper right quadrant and had a positive Murphy's sign. Clinical features and laboratory findings (71.7% lymphocytes, AST 137 IU/l, ALT 108 IU/l, ALP 353 IU/l, and LDH 2015 IU/l) were compatible with acute-stage of IM. Because of marked hepatosplenomegaly and severe upper right abdominal pain, an ultrasonographic (US) evaluation was performed showing mild hepatosplenomegaly with marked thickening of the gallbladder wall (GBW) greatly exceeding 3 mm, and minimal pericholecystic fluid (Fig. 1). No ductal dilation, gallstones or sludge were noted, and the pancreatic head was unremarkable. Swelling of the lymph nodes at the porta hepatis was detected, measuring up to 10 mm in diameter. A small amount of ascites around the bowel loops and the Douglas' pouch was found. Abdominal CT showed a thickened GBW consisting of multiple layers without distention and with a hypodense outer layer of subserosal edema that mimicked pericolecystic fluid; porta hepatis and portocaval lymphadenopathy was observed. Chest CT showed multiple enlarged lung nodules of various sizes and a small pericardial effusion; a hypodense solid mass of unknown etiology was detected in the anterior mediastinum mimicking a malignant tumor. Hematological analysis of peripheral blood smear was therefore performed, showing an elevated lymphocyte proportion of atypical cells; no malignant leukocytes were seen. Virus-specific IgM antibody levels and PCR provided serologic confirmation of the diagnosis of Epstein-Barr virus (EBV) infection. Viral cultures and serological tests were negative for other organisms. IM was thus identified as the only underlying disease. The patient was carefully monitored: clinical evaluation, laboratory analysis and US examination were repeated at weekly intervals. Her symptoms gradually regressed. US showed disappearance of the gallbladder wall thickening (GBWT) with normal distention, and resolution of the lymph node swelling.
Fig. 1.
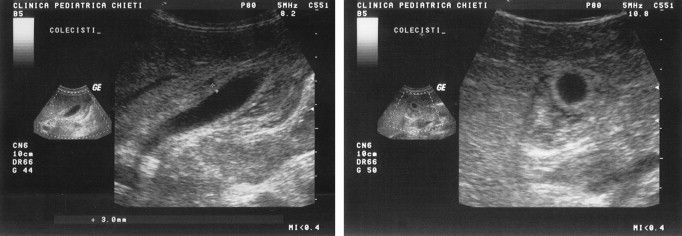
Gallbladder wall thickening (GBWT) with minimal pericholecystic fluid.
Ethical approval for this study was granted by the Medical Research Ethics Committee of our University, and informed consent was obtained from all patients.
Discussion
Only a few cases of GBWT (gall bladder wall thickening) or intrathoracic inflammatory pseudotumor in patients with IM are described in the literature, especially in immunocompetent adolescent patients [2,3]. Normally, GBW appears as a pencil-thin echogenic line at US examination. In our case, abdominal US showed a GBW thickness that greatly exceeded 3 mm, the upper limit of normal range in fasting subjects [2]. Diffuse gallbladder thickening may produce a diagnostic problem; the finding itself is unspecific and may result from a broad spectrum of pathological conditions, intrinsic as well as extrinsic to the biliary tract [4]. When associated with serologic evidence of primary EBV-infection, the finding of GBWT and enlarged nodes at the porta hepatis allows exclusion of other conditions [2].
The pathogenetic mechanism which causes GBWT has not been clarified yet. It is thought to be due to a direct involvement of the wall with infected lymphocytes, severe hypoproteinemia, lymphatic obstruction caused by enlarged nodes at the porta hepatis, and an immunological reaction similar to that which occurs in viral hepatitis [2,5,6]. Although traditionally US is used as the initial imaging technique for evaluating gallbladder diseases, CT may be used as an adjunct to an inconclusive US examination, in the presence of a perplexing clinical presentation, or for disease staging [4].
The presence of pleural effusion or ascites has rarely been reported in IM [3] mainly occurring in non-immunocompetent hosts or patients with concomitant severe hepatic dysfunction. The presence of serosal effusion, often associated with marked systemic lymphadenomegaly, made the diagnosis of IM questionable, requiring exclusion of malignant tumor, lymphoproliferative disease or any other clinicopathologic entity.
Conflict of interest statement
None declared.
References
- 1.Tattevin P., Le Tulzo Y., Minjolle S. Increasing incidence of severe Epstein–Barr virus-related infectious mononucleosis: surveillance study. J Clin Microbiol. 2006;44:1873–1874. doi: 10.1128/JCM.44.5.1873-1874.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoshie K., Ohta M., Okabe N., Komatsu T., Umemura S. Gallbladder wall thickening associated with infectious mononucleosis. Abdom Imaging. 2004;29:694–696. doi: 10.1007/s00261-004-0173-8. [DOI] [PubMed] [Google Scholar]
- 3.Chen J., Konstantinopoulos P.A., Satyal S., Telonis J., Blair D.C. Just another simple case of infectious mononucleosis? Lancet. 2003;361:1182. doi: 10.1016/S0140-6736(03)12953-4. [DOI] [PubMed] [Google Scholar]
- 4.Zissin R., Osadchy A., Shapiro-Feinberg M., Gayer G. CT of thickened-wall gall bladder. Br J Radiol. 2003;76:137–143. doi: 10.1259/bjr/63382740. [DOI] [PubMed] [Google Scholar]
- 5.Sainsbury R., Smith P.K., LeQuesne G., Davidson G.P., Jureidini K.F., Moore D.J. Gallbladder wall thickening with infectious mononucleosis hepatitis in an immunosuppressed adolescent. J Pediatr Gastroenterol Nutr. 1994;19:123–125. doi: 10.1097/00005176-199407000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Hammond D.I., MacLean R.S. Gallbladder wall thickening in an elderly woman with infectious mononucleosis. J Clin Ultrasound. 1987;15:558–560. doi: 10.1002/jcu.1870150811. [DOI] [PubMed] [Google Scholar]


