Abstract
Purpose
The aim of this study is to demonstrate the diagnostic accuracy of ultrasonography (US) in the diagnosis of rupture of the medial head of the gastrocnemius muscle, also called “tennis leg” (TL).
Materials and methods
Thirty-five consecutive patients with acute traumatic injury of the calf underwent US examination. There were 25 men and 10 women; mean age 47.5 years (range 35–60 years). All examinations were performed using a 5–12 MHz broadband electronic linear array probe.
Results
Thirty-three out of 35 patients had TL; 24 cases of partial rupture and nine cases of complete rupture were diagnosed. In the remaining two cases, both with symptoms suggesting TL, one patient had a tear of the proximal musculotendinous junction and one had a ruptured Baker's cyst. Fluid collections caused by the muscular rupture were visible as hypoechoic areas; in 80% of cases associated by a hyperechoic oval area due to hematoma and local inflammation. The degree of fluid collection in the patients with complete rupture (6–16 mm; mean: 9.7 mm) was significantly greater than the one seen in patients with partial rupture (4–8 mm; mean: 6.8 mm).
Conclusions
US is the imaging modality of choice in clinical suspicion of TL, both in the initial workup of the patient and in the follow-up. US is easy to perform and is particularly useful to distinguish TL from other pathologies, especially ruptured Baker's cyst and deep vein thrombosis, which require a different therapeutic management.
Keywords: Gastrocnemius muscle, Ultrasonography, Tennis leg
Sommario
Scopo
L'obiettivo di tale studio è dimostrare l'accuratezza diagnostica dell'ecografia nella diagnosi della rottura del ventre mediale del muscolo gastrocnemio (Tennis Leg).
Materiali e metodi
Sono stati valutati con esame ecografico 35 pazienti (25 uomini e 10 donne, con un range di età tra i 35 e i 60 anni ed età media di 47,5 anni) con danno acuto traumatico del polpaccio. Gli esami sono stati effettuati usando una sonda elettronica lineare a banda larga da 5–12 MHz.
Risultati
Trentatre dei 35 pazienti presentavano una rottura del ventre mediale del muscolo gastrocnemio (TL): 24 rotture parziali e 9 rotture complete. Nei rimanenti due casi, entrambi con sintomi clinici suggestivi di Tennis Leg, sono stati diagnosticati strappo della giunzione prossimale muscolo-tendinea e rottura di una cisti di Baker. La raccolta fluida, conseguenza della rottura muscolare, si presentava come una zona ipoecogena, con area iperecogena ovalare nel contesto, riferibile a ematoma e alla flogosi locale. L'entità della raccolta fluida nei pazienti con rottura completa (6–16 mm; media: 9.7) era significativamente superiore rispetto ai pazienti con rottura parziale (4–8 mm; media: 6.8).
Conclusioni
L'ecografia è l'indagine di prima scelta nel sospetto clinico di rottura del ventre mediale del muscolo gastrocnemio, non solo per la rapidità di esecuzione e per il follow-up, ma soprattutto per la possibilità di fare diagnosi differenziale con altre patologie, prime tra tutte la rottura di cisti di Baker e le trombosi venose, che richiedono approccio terapeutico diverso.
Introduction
Rupture of the medial head of the gastrocnemius muscle, known as tennis leg (TL), is a common traumatic injury of the calf. It is very frequent in subjects over 40 years of age and it occurs mainly when the muscle is overstretched not only during sports activities such as tennis, skiing, and running, but also during common daily activities [1,2]. An accurate clinical examination is sometimes enough to formulate a hypothesis of likely diagnoses, but it is often difficult to reach a correct diagnosis due to association of other pathologies. Diagnostic imaging is therefore required, and ultrasonography (US) being inexpensive, non-invasive and easy to perform, is considered the gold standard in the diagnosis of TL [1] (Figs. 1–3) for evaluating the degree and extent of the muscular lesion and to exclude other pathologies such as ruptured Baker's cyst and deep vein thrombosis [3]. Deep vein thrombosis needs particular attention as it requires a different therapeutic management also to prevent possible embolic complications, although these are rare.
Fig. 1.
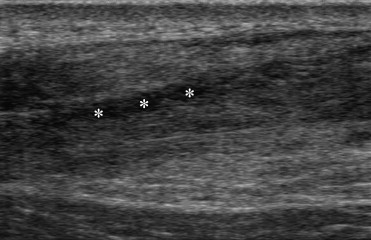
Tennis leg (TL), muscular partial rupture of the medial head of the gastrocnemius. There is visible the discontinuity of muscular fibers and the presence of the hipoechoic fluid collection (*) related to local inflammation.
Fig. 2.
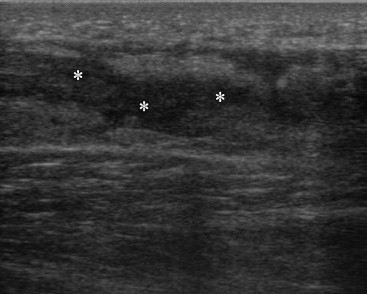
Another case of TL with partial muscular rupture and presence of the hipoechoic fluid collection (*).
Fig. 3.

Same previous case, there is visible the presence of bruise (arrows) related to the muscular rupture and to local inflammation.
US examination evidencing a roundish hyperechoic image in the transverse plane stretching out in the longitudinal plane with absence of color signal at color Doppler suggests thrombosis. On the other hand, an US image characterized by an anechoic area and thin walls communicating with the musculotendinous junction suggests a ruptured Baker's cyst. In any case, US can provide elements for a differential diagnosis of numerous pathologies which can occur in this site. US also makes it possible to extend the scans to the distal zones of the leg near the Achilles tendon, where hematomas deriving from other caudal areas frequently occur due to downward migration by gravity.
Materials and methods
From July 2005 to January 2007, 35 consecutive patients with acute traumatic injury of the calf underwent US examination. There were 25 men and 10 women; mean age 47.5 years (range 35–60 years). Of these patients, 70% had suffered the injury during sports activities (tennis, skiing, and running) and 30% during common daily activities (walking up the stairs, common accidents in the street). All patients presented the following clinical symptoms: acute pain at the level of the medial head of the gastrocnemius muscle followed by a feeling of weakness of the limb and subsequent hematoma and soreness. Ethical approval for this study was granted by the Medical Research Ethics Committee of our university, and informed consent was obtained from all patients.
All examinations were performed using a 5–12 MHz broadband electronic linear array probe. Workup included transverse and longitudinal scans of the gastrocnemius muscle extending the field of view to include the Achilles tendon where hematomas can occur due to downward migration by gravity. The patients were examined in the prone position, with the knees slightly bent (10–15 degrees) and the legs resting on a cushion in order to reduce the strain on the triceps surae muscle and thereby the discomfort during the examination.
Two types of muscular injury were diagnosed: partial rupture of the medial head of the gastrocnemius muscle based on the presence of a localized disruption or discontinuity of the muscular fibers, and complete rupture with total discontinuity of the muscular fibers and retraction of the proximal and distal ends of the muscle.
Rupture is generally associated with the presence of fluid collection between the medial head of the gastrocnemius and soleus muscles with or without hemorrhage, defined by abnormal echogenicity at this location. Measurement of fluid collection in the longitudinal, axial and coronal planes provides information about the extent of the lesion, whereas evaluation of the distance between the two muscles indicates the degree of the lesion.
Results
The patients were examined at an average of 1.5 days following their injury. Of 35 patients, 33 (97%) had TL; 24 had partial rupture and nine had complete rupture (Fig. 4). Of the 24 patients with partial rupture, five had gastrocnemic vein thrombosis in addition to TL. Of these five patients, two had deep vein thrombosis in both veins (Fig. 5) and three had deep vein thrombosis in one vein only (Fig. 6). Two patients out of 35 (3%) had symptoms suggesting TL, but one patient was diagnosed a tear of the proximal musculotendinous junction and one had a ruptured Baker's cyst. The results are shown in Table 1.
Fig. 4.
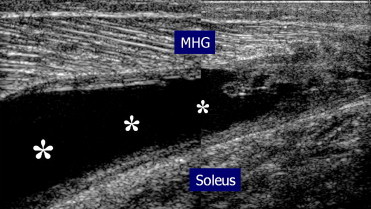
TL: patient with complete rupture (*) of the medial head of gastrocnemius (MHG); there is visible the below soleus (Soleus).
Fig. 5.
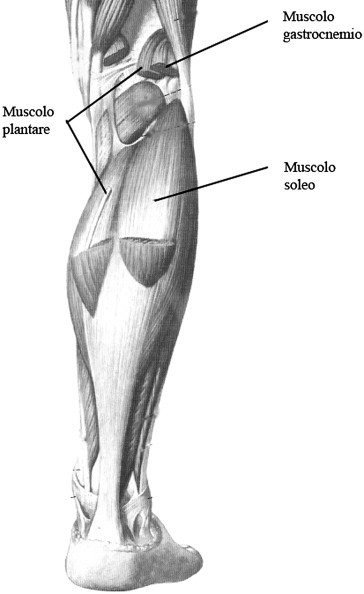
Superficial muscles of the calf.
Fig. 6.
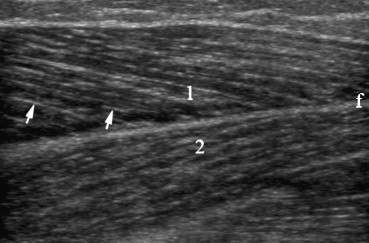
Longitudinal US shows the feather-shape structure of the muscle; the hiperechoic fibroadipose septum (arrows) separate the hipoechoic bundle of muscle; the muscular ring (f) divides the gastrocnemius (1) from the below soleus (2).
Table 1.
The results of US examination of the calf in 35 patients with suspected rupture of the medial head of the gastrocnemius muscle (tennis leg)
| Diagnosis | Patients |
|---|---|
| TL partial rupture | 19 |
| TL complete rupture | 9 |
| TL partial rupture associated with gastrocnemic vein thrombosis (both veins) | 2 |
| TL partial rupture associated with gastrocnemic vein thrombosis (one vein only) | 3 |
| Ruptured Baker's cyst | 1 |
| Proximal muscle strain | 1 |
| Total | 35 |
In the 33 patients affected by TL, US evaluation showed disruption or discontinuity of the normal muscular structure and fluid collection interposed between the medial head of the gastrocnemius muscle and the underlying soleus muscle evidenced by anechoic to hypoechoic areas, which in 80% of cases were associated with a hyperechoic oval area representing a hematoma caused by the injury and local inflammation.
The degree of the fluid collection in the patients with complete rupture (anteroposterior diameter 6–16 mm; mean: 9.7) was significantly greater than the one seen in patients with partial rupture (anteroposterior diameter 4–8; mean: 6.8). The association with deep vein thrombosis confirms that this pathology can be a complication in TL, which is not particularly rare.
The five patients who had both TL and gastrocnemic vein thrombosis were given medication for the muscular pathology, and they also underwent a thorough vascular examination and were given anticoagulation therapy.
A 6-month follow-up, which included monthly US examinations, showed the reparative process of the muscle ruptures and allowed prevention of complications. At the level of the lesion, US examinations evidenced a progressive substitution of anechoic areas representing fluid collections with hyperechoic areas indicating a reparative fibrous process.
Discussion
Tennis leg typically occurs in connection with plantar flexion of the foot with simultaneous extension of the knee, which implies active contraction and passive stretching of the gastrocnemius muscle. Clinical examination reveals a diffuse palpable mass, acute pain and localized soreness in the middle portion of the calf, and the patient is unable to walk or cannot walk without feeling pain. However, the clinical signs of TL can easily be confused with other pathological conditions such as thrombophlebitis [5,6] or ruptured Baker's cyst. An accurate radiological examination is therefore necessary to form a differential diagnosis and make appropriate management decisions. In this case, US is the imaging modality of choice to confirm or exclude TL, to determine the degree of the lesion (partial or complete rupture), to visualize and evaluate hypoechoic fluid collections between the medial head of the gastrocnemius and the underlying soleus muscles as well as possible hematomas and local inflammation [1,4]. TL rarely requires surgery; the lesion normally heals in 3–6 weeks when the patient is treated with ice, rest, and non-steroidal anti-inflammatory drugs [1,3]. In case of thrombophlebitis, the administration of anticoagulation therapy is advisable to avoid possible embolic complications. Anticoagulation therapy can cause hemorrhagic complications, however, misdiagnosis and omitted treatment of deep vein thrombosis can have disastrous consequences, particularly in young, and healthy patients [7].
Deep vein thrombosis as a complication in TL has been widely reported in the literature and it is attributed to the presence of edema or a hematoma which compresses the popliteal veins and the gastrocnemic veins, both at a low pressure [3]. A routine US examination of the deep venous system of the calf can lead to early treatment of this pathology, thus preventing also a chronic venous insufficiency caused by venous valve damage [8]. US is furthermore able to distinguish between different pathologies, and in patients with suspected deep vein thrombosis of the calf, US identifies ruptured Baker's cyst, hematomas, neoplastic lesions or abscesses in 12% of cases [9]. Rupture of the medial head of the gastrocnemius muscle is characterized by disruption of the normal structure of the tendon at its insertion, appearing as parallel hypoechoic and hyperechoic lines, typically accompanied by an indistinct echostructure of the distal end of the tendon at its insertion [1,10].
Axial US scans (Fig. 7) are the most useful for differentiating between partial and complete rupture, as it is possible to depict the whole muscle belly in one single image. In the initial workup of the patient, US is therefore required to confirm suspected TL, evaluate the degree, form a correct differential diagnosis and to exclude associated pathologies. After the initial evaluation, US is essential in the follow-up to determine the stages of recovery. Minimum duration of the follow-up should be 6 months, with monthly examinations to evaluate the healing process characterized by a progressive centripetal reabsorption of the fluid collection (anechoic to hypoechoic image), gradually substituted by fibrous scar tissue which is a sign of the healing of the muscular lesion (Fig. 8).
Fig. 7.
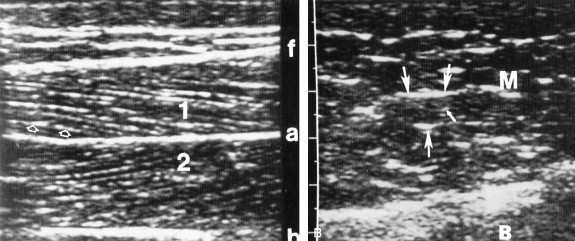
Left: the feather-shape structure of the muscle in a longitudinal US; the hiperechoic fibroadipose septum (open arrows) separate the hipoechoic bundle of muscle; the aponeurosis (a) separate rectum femoral (1) and medial vastus musles (2); the fascia (f) and the bone (b), evident as two highly reflecting lines, separate the muscles. Right: the fibroadipose septum (arrows) of unequal length in an axial US; the feather-shape structure of muscle is not visible.
Fig. 8.
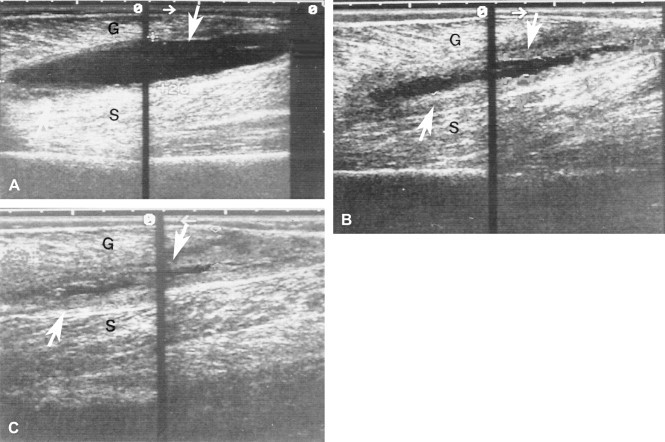
TL Muscular rupture between gastrocnemius (G) and soleus muscle (S). A shows the muscular trauma; arrows show a fusiform hematoma that divides the two muscles. In B and C, in phase of recovery with a six month follow up, the reduction of hematoma size is visible.
In conclusion, we propone US as the gold standard in suspected TL as this examination is non-invasive and easy to perform, because it provides an early diagnosis and because it can exclude other pathologies which require a different therapeutic management.
References
- 1.Bianchi S., Martinoli C., Fikry Abdelwahab I., Derchi L.E., Damiani S. Sonographic evaluation of tears of the gastrocnemius medial head (“tennis leg”) J Ultrasound Med. 1998;17:157–162. doi: 10.7863/jum.1998.17.3.157. [DOI] [PubMed] [Google Scholar]
- 2.Jarolem K.L., Wolinsky P.R., Savenor A., Ben-Yishay A. Tennis leg leading to acute compartment syndrome. Orthopedics. 1994;17:721–723. doi: 10.3928/0147-7447-19940801-12. [DOI] [PubMed] [Google Scholar]
- 3.Slawski D.P. Deep venous thrombosis complicating rupture of the medial head of the gastrocnemius muscle. J Orthop Trauma. 1994;8:263–264. doi: 10.1097/00005131-199406000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Gaulrapp H. “Tennis leg”: ultrasound differential diagnosis and follow up. Sportverletz Sportschaden. 1999;13(2):53–58. doi: 10.1055/s-2007-993314. [DOI] [PubMed] [Google Scholar]
- 5.McClure J.C. Gastrocnemius musculotendinous rupture: a condition confused with thrombophlebitis. South Med J. 1984;77:1143–1145. doi: 10.1097/00007611-198409000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Liu S.H., Chen W.S. Medial gastrocnemius hematoma mimicking deep vein thrombosis: report of a case. Taiwan I Hsueh Hui Tsa Chih. 1989;88:624–630. [PubMed] [Google Scholar]
- 7.Zamorski M.A., Opdycke R.A. Advances in the prevention, diagnosis and treatment of deep venous thrombosis. Am Fam Physician. 1993;47:457–469. [PubMed] [Google Scholar]
- 8.Gottlieb R.H., Widjaja J., Mehra S., Robinette W.B. Clinically important pulmonary emboli: does calf vein US alter outcomes? Radiology. 1999;211:25–29. doi: 10.1148/radiology.211.1.r99ap0125. [DOI] [PubMed] [Google Scholar]
- 9.Vaccaro L.P., Cronan J.J., Dorfman G.S. Outcome analysis of patients with normal compression US examination. Radiology. 1990;179:443–446. doi: 10.1148/radiology.175.3.2188294. [DOI] [PubMed] [Google Scholar]
- 10.Delgado G.J., Chung C.B., Lektrakul N. Tennis leg: clinical US study of 141 patient and anatomic investigation of four cadavers with MR imaging and US. Radiology. 2002;224:112–119. doi: 10.1148/radiol.2241011067. [DOI] [PubMed] [Google Scholar]


