Abstract
Introduction
In this survey we evaluated the usefulness of ultrasonography (US) in the diagnosis, and in the treatment of complicated hydatid cysts.
Materials and methods
From June 1985 to June 2004, 221 patients with 294 hydatid cysts were examined. Twenty patients (9.0%) presented 22 complicated cysts (7.4%): 9 with infection, 5 ruptured into the bile ducts, 2 bilomas, 2 cysto-pleural fistulas, 2 allergic reactions, 1 rupture into the peritoneum and 1 intrasplenic hematoma. In all cases, US yielded a specific or suspected diagnosis, also in complications affecting non-hepatic sites, confirmed by computed tomography (CT), endoscopic papillotomy or percutaneous US-guided sampling. All patients with complicated cystic echinococcosis were treated with Albendazole 800 mg/day for at least 3 months. In addition to this therapy, 12 underwent US-guided drainage (9 infected cysts, 2 bilomas, 2 cysto-pleural fistulas, 1 intrasplenic hematoma); of these patients 3 subsequently underwent surgery because US-guided treatment was ineffective. Five patients were treated with perendoscopic sphincterotomy for obstruction of the bile passages, while 3 patients received only medical therapy.
Results
Medical, echoguided and surgical treatments led to resolution of the complications and complete remission of the parasitic pathology in 19/20 patients (95%) and in 21/22 cysts (95.4%). There was partial remission in 1 case only. The therapy did not cause major complications and the results were confirmed during follow-up lasting from 5 months to 15 years (mean time 3 years).
Discussion and conclusion
This study shows that the incidence of complications of hydatid cysts is low and that correct echographic management allows a rapid diagnosis and optimization of treatment in most cases.
Keywords: Cystic echinococcosis, Ultrasound, Complications, Diagnosis, Treatment
Sommario
Introduzione
Gli autori valutano in questo lavoro l'utilità dell'ecografia nella diagnosi e nel trattamento ecoguidato delle cisti idatidee complicate.
Materiali e metodi
Dal giugno 1985 al giugno 2004 gli autori hanno seguito 221 pazienti affetti da 294 cisti idatidee. 20 pazienti (9,0%) presentavano 22 cisti complicate (7,4%): 9 erano infettate, 5 rotte nelle vie biliari, 2 bilomi, 2 fistole cisto-pleuriche, 2 reazioni allergiche, 1 rotta in peritoneo ed 1 ematoma intrasplenico. In tutti i casi l'ecografia permise di sospettare la diagnosi, anche per le complicanze extraepatiche, che venivano confermate dalla TC, dalla papillosfinterotomia perendoscopica, o dai prelievi ecoguidati. Tutti i pazienti affetti da cisti idatidee complicate furono trattati con 800 mg/die di albendazolo, per almeno 3 mesi. Oltre a questa terapia 12 furono sottoposti a drenaggio ecoguidato (9 cisti infettate, 2 bilomi, 2 fistole cisto-pleuriche, 1 ematoma intrasplenico); di questi 3 furono successivamente operati in quanto il trattamento ecoguidato era risultato inefficace, 5 pazienti furono trattati con papillosfinterotomia perendoscopica per ostruzione delle vie biliari, mentre 3 pazienti ricevettero solo terapia medica.
Risultati
Il trattamento medico, ecoguidato e chirurgico permisero la risoluzione delle complicazioni e la remissione completa della patologia parassitaria in 19/20 pazienti (95,0%) ed in 21/22 cisti (95,4%); solo in un caso fu ottenuta una remissione parziale. Il trattamento non fu accompagnato da complicanze maggiori ed il risultato è stato confermato da un follow-up della durata minima di 5 mesi e massima di 15 anni (media 3 aa).
Discussione e conclusioni
Questo studio ha mostrato che l'incidenza delle complicanze delle cisti idatidee è bassa e che un corretto management ecografico permette una rapida diagnosi e di ottimizzare il trattamento nella maggior parte dei casi.
Introduction
The incidence of hydatid cysts varies among different regions of the world, with high-, medium- and low-frequency zones. In Italy, an echo-epidemiological investigation in 1990 showed a mean prevalence of 0.18%, with a strong north–south gradient (North 0.07%, Center 0.12%, South 0.39%, Sardinia 2.09%) [1]. A recent study in Argentina compared the incidence of this pathology in asymptomatic and symptomatic patient populations showing liver pathology in 90% of asymptomatic patients but only in 60–70% of symptomatic patients [2]. These data indicate that this liver pathology often evolves without symptoms and that it is more frequent than the pulmonary form.
In addition to being asymptomatic, hepatic echinococcosis often undergoes spontaneous involution. Abdominal, small parts and pleural ultrasonography (US) can evaluate the evolution, involution and degeneration of parasitic cysts, divide evolutionary stages into active, transitional and inactive stages, and classify echographically the various phases of the disease [3–7].
In the phase of active growth, some complications may occur and in most cases US can provide important information about these conditions. Complications of hydatid cysts involve actively growing lesions and are usually caused by the increased pressure of the cystic liquid, which can cause rupture of membranes and pericysts. The objectives of this study were to evaluate the incidence of complications in cystic echinococcosis, the possibility of early diagnosis of these pathologies using US and to establish which complications can be treated using percutaneous US-guided drainage.
Materials and methods
From June 1985 to June 2004, 221 patients with 294 hydatid cysts (213 hepatic, 49 peritoneal, 14 pulmonary, 9 splenic, 4 muscular, 3 renal, 2 vertebral) were observed in our Department Of Infectious Diseases. There were 120 men and 101 women, mean age 49 years (range 18–84 years).
Ethical approval for this study was granted by the Medical Research Ethics Committee of our hospital, and informed consent was obtained from all patients.
In 216 patients (97.8%) with abdominal cysts, diagnosis was made using US (AU4 IDEA-Esaote) and a 3.5-MHz probe. Serology: indirect hemoagglutination reaction (IHA) was positive in 198 patients (89.6%). Diagnosis in the remaining cases required magnetic resonance imaging (MRI) in 2 patients (0.7%), percutaneous US-guided biopsy in 2 solid lesions (0.9%) or percutaneous US-guided aspiration in 2 liquid lesions (0.9%).
Forty-two patients with 106 cysts were administered Albendazole only; 22 patients with 22 cysts underwent percutaneous drainage of echinococcal cysts (PAIR); 55 patients with 57 cysts were administered Albendazole and underwent PAIR, 80 patients were not treated because their 84 cysts were inactive, and 20 patients (9%) had 22 complicated cysts (7.4%) (Table 1).
Table 1.
Cystic echinococcosis: a case study by the Department of Infectious Diseases, Hospital of Arezzo, Italy
| Treatment | Patients | Hydatid cysts |
|---|---|---|
| Albendazole | 42 | 106 |
| PAIR | 22 | 22 |
| Albendazole + PAIR | 55 | 57 |
| Surgery | 2 | 3 |
| Complicated cysts | 20 | 22 |
| No therapy | 80 | 84 |
| Total | 221 | 294 |
Of the 221 patients affected by cystic echinococcosis, 167 (75.6%) underwent US examination for non-specific symptoms of echinococcosis or in the follow-up of other pathologies. Fifty-four patients (24.4%) were symptomatic: 18 underwent abdominal US for slight pain in the right hypochondrium, 10 for a palpable mass in the epigastric region or in the right hypochondrium and 6 for pruritus, but only 20 presented complications. Nine patients (Group I) with 7 hepatic, 2 peritoneal, 1 pulmonary and 1 muscular hydatid cyst, presented fever; 2 patients with hepatic cysts complained of cough and slight fever. Five patients (Group II) with 5 hepatic parasitic cysts presented abdominal pain in the superior right quadrant. Two asymptomatic patients (Group III) showed at US a pericystic collection, while 2 patients (Group IV) with allergic rash had a hydatid cyst with a double-wall appearance. One patient (Group V) with hepatic echinococcosis was referred to US after violent abdominal pain, and a young woman (Group VI) because of pain in the left hypochondrium.
Of 20 patients with complicated cystic echinococcosis, 9 presented fever (45%), 7 abdominal pain (35%) of whom 2 with jaundice (10%), and 2 allergic rash (10%), while 2 patients showed US alterations (10%) without symptoms.
A mean follow-up of 3 years (5 months–15 years) was performed, with clinical and US examinations every 3 months for the first year, every 6 months for the next 5 years and then once a year.
Results
Diagnosis of complications
In all cases US led to a definitive or suspected diagnosis. Nine patients (Group I) with fever had 11 cysts; US showed an encapsulated and inhomogeneous lesion containing stratified echogenic material in the posterior region, with reverberation artifacts in 2 cases. US indicated a diagnosis of superinfection of the cysts also in the patient with communicating hepatic, pulmonary and muscular lesions. Moreover, in 2 patients, the presence of an anechoic pleural area communicating with the cyst by means of an anechoic line suggested a cysto-pleural fistula, later confirmed by computed tomography (CT).
All 9 patients subsequently underwent percutaneous echoguided drainage and/or aspiration, which revealed the presence of purulent material and ruptured cystic membranes. Culture of the pus showed the presence of Pseudomonas aeruginosa in 2 patients, 1 with peritoneal cysts and 1 with communicating hepatic, pulmonary and muscular cysts; coagulase-positive Staphylococcus in 2 patients with suppurative cysts of the liver; Bacteroides fragilis in a peritoneal cyst and in a hepatic cyst complicated by pleural fistulas (these 2 patients showed intracystic reverberation artifacts, a US sign of abscess caused by gas-producing germs); Enterobacter aerogenes in 1 patient with hepatic cysts; apparently sterile pus in 2 patients (Fig. 1a,b).
Fig. 1.
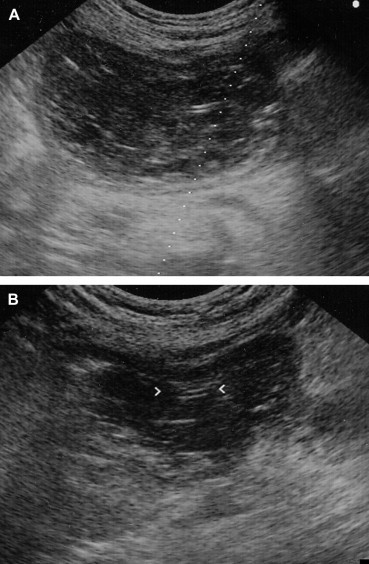
Oblique right subcostal scans. (a) In the left lobe, there is an inhomogeneous oval lesion with a wall and a small “railway track” echogenic structure (arrows). Suppurative hydatid cysts of the liver with echoguided drainage. (b) After 4 days of percutaneous echoguided aspiration, the lesion has an “hourglass” appearance composed only of parasitic membranes. The catheter is visible (arrow). Suppurative hydatid cysts treated with percutaneous US-guided drainage.
In the 5 patients with abdominal pain in the upper right quadrant (Group II), US revealed cysts indirect contact with the bile ducts, dilation of the intra- and extrahepatic bile ducts and the presence of echogenic material inside the common bile duct as an expression of the rupture of the echinococcosis into the bile ducts, subsequently confirmed by perendoscopic sphincterotomy (Fig. 2). In these patients laboratory tests showed increased levels of alkaline phosphatase and gamma glutamyl transpeptidase. However, there was a direct increase of bilirubin in only 2 cases.
Fig. 2.

Longitudinal scan passing through the aorta. Below the left lobe of the liver and head of pancreas and above the aorta, there is a tubular echogenic structure containing echogenic material (arrows). Perendoscopic sphincterotomy confirmed the presence of hydatid material in the common bile duct.
In the 2 patients with pericystic collection (Group III), US showed linear echogenic images inside the pericystic collection. This suggested biloma with almost complete detachment of the cystic membrane floating in the bile, confirmed by percutaneous US-guided aspiration. In 2 patients with double-wall appearance (Group IV), US suggested an early detachment of cystic membranes.
In the patient with abdominal pain (Group V), US revealed a hepatic cyst with intraperitoneal fluid collection containing linear echogenic images and small cysts; this allowed a diagnosis of rupture of the cyst directly into the peritoneum (Fig. 3). The patient with pain in the left hypochondrium (Group VI) had an anechoic lesion of the spleen with small cystic lesions diagnosed as a ruptured hydatid cyst complicated by intrasplenic hematoma, confirmed by percutaneous US-guided aspiration (Table 2).
Fig. 3.

Transverse right subcostal scan. Presence of linear echogenic structures floating in peritoneal fluid, delimiting posteriorly and laterally the right lobe of the liver due to hydatid liquid containing ruptured chitinous and proligerous membranes. Spontaneous rupture of hydatid cysts of the liver into the peritoneum; the diagnosis was confirmed by percutaneous US-guided sampling.
Table 2.
Spontaneous complications of human hydatidosis: a case study by the Department of Infectious Diseases, Hospital of Arezzo, Italy
| Patients with hydatid cysts 221; patients with complications 20 (9.1%) |
| Hydatid cysts 294; cysts with complications 22 (7.4%) |
| Patients with active hydatid cysts 143; cysts with complications 20 (14.0%) |
| Active hydatid cysts 210; with complications 22 (10.5%) |
| Group I |
| HC infected, 9 (40.9%): hepatic 5, peritoneal 2, pulmonary 1, muscular (1) – 7 patients (35%) |
| HC with cysto-pleural fistula 2 (9%) – 2 patients (10%) |
| Group II |
| HC ruptured into the bile ducts 5 (22.7%), with jaundice in 2 cases – 5 patients (25%) |
| Group III |
| HC complicated by spontaneous biloma 2 (9%) – 2 patients (10%) |
| Group IV |
| HC with allergic rash 2 (9%) – 2 patients (10%) |
| Group V |
| HC complicated by direct rupture into the peritoneum 1 (4.5%) – 1 patient (5%) |
| Group VI |
| HC complicated by spontaneous intrasplenic hematoma 1 (4.5%) – 1 patient (5%) |
Treatment of complications
All patients received Albendazole 800 mg/day per os for at least 3 months. In Group I, 9 patients affected by 11 suppurative hydatid cysts also underwent percutaneous US-guided drainage and cleaning of the cyst cavity using physiological solution and received systemic antibiotic therapy. In the patient with 3 cysts, 3 drains were placed: the first in the liver, the second in the lung and the third subcutaneously (Fig. 4a–c).
Fig. 4.
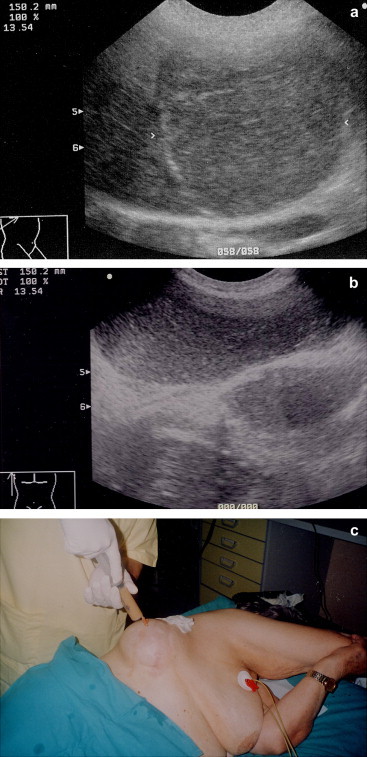
(a) Oblique right subcostal scan. A voluminous inhomogeneous formation with an evident wall (arrows) occupies segment 2–3–4–8 and is in contact with the diaphragm. (b) The right coronal scan reveals an inhomogeneous subcutaneous collection (s) of liquid communicating with a similar collection in the right pleura (p), which in turn communicates with the hepatic lesion (h). (c) Intercostal percutaneous echoguided drainage allowed diagnosis of communicating hepatic, pleural and subcutaneous hydatid cysts infected with Pseudomonas aeruginosa.
In Group II, the 5 patients with rupture of hepatic hydatid cysts into the bile ducts received Albendazole and underwent perendoscopic sphincterotomy.
In Groups III and VI, the 2 patients with bilomas and the patient with intrasplenic hematoma underwent percutaneous US-guided aspiration.
In Groups IV and V, 3 patients (2 with rash and 1 with direct rupture of the cyst into the peritoneum) were treated only with Albendazole 800 mg/day for 6 months.
Eleven of the 14 cysts treated with percutaneous US-guided drainage (78.6%) resolved, but 3 patients treated with percutaneous US-guided therapy (1 suppurative hepatic cyst, 1 suppurative cyst with cysto-pleural fistulas and 1 biloma) relapsed and were treated surgically (21.4%).
Resolution of the complications and complete remission of the hydatid disease occurred in 95% of treated patients (19/20 patients) and in 95.5% of treated cysts (21/22 cysts). After 6 months of therapy, the patient affected by direct rupture of the cyst into the peritoneum showed disappearance of the liquid and reduced number of peritoneal cysts (Table 3).
Table 3.
Treatment of complications in human echinococcosis: case study by the Department of Infectious Diseases, Hospital of Arezzo, Italy
| Percutaneous | US-guided therapy | Surgery | Albendazole | Endoscopic papillotomy | Resolution |
|---|---|---|---|---|---|
| HC infected | 9 (1)a | 1 | 9 | – | 9 (CR) |
| HC ruptured into the bile ducts | – | – | 5 | 5 | 5 (CR) |
| Biloma | 2 (1)a | 1 | 2 | – | 2 (CR) |
| Allergic rash | – | – | 2b | – | 2 (CR) |
| Cysto-pleural fistula | 2 (1)a | 1 | 2 | – | 2 (CR) |
| Rupture into the peritoneum | – | – | 1b | – | 1 (PR) |
| Intrasplenic hematoma | 1 | – | 1 | – | 1 (CR) |
| 11/14 | 3/3 | 2/3 (22)b | 5/5 | 21/22 (CR) | |
| 78.6% | 100% | 66.6% | 100% | 95.45% | |
| 1/22 (PR) | |||||
| 4.55% |
CR = complete remission; PR = partial remission.
Patients treated with percutaneous echoguided aspiration and drainage, who relapsed and subsequently underwent surgery.
All patients (20 with 22 cysts) received Albendazole; 3 (2 with allergic rash and 1 with direct rupture into the peritoneum) received only Albendazole.
Clinical and US follow-up showed relapse of infection in 1 patient affected by previously suppurative peritoneal cysts (4.5%). Further treatment with percutaneous US-guided drainage also resolved this complication.
The therapies used did not cause further complications, except for Albendazole which was responsible for an increase in transaminase (less than 200 UI/dL) in 10% of cases, headache and hair loss in 5% of cases.
Discussion
In the last 10 years, echinococcosis has received a lot of attention internationally. Diagnosis and treatment have greatly changed due to the introduction of new serological and imaging methods, the discovery of effective drugs like Mebendazole and Albendazole and PAIR as an alternative to surgery in the basic disease and perendoscopic sphincterotomy [8–11].
Rupture of the hydatid cyst can be contained, communicating or direct. In the contained rupture, only the cystic membranes break, and the endocystic material remains confined by the host's pericyst; clinical signs are infrequent, characterized mainly by allergic reactions, while infections are rare. In the communicating rupture, due to alteration also of the pericyst, the endocystic contents can empty into the biliary or bronchial tree. In this case, there can be vomica, jaundice and/or biliary colic. Infections of the cyst are frequent and, because of laceration of bile ducts enclosed in the pericystium, collections of bile sometimes form around collapsed cystic membranes (bilomas) [12,13]. If the cyst opens directly into a serous cavity (peritoneum, pleura, pericardium), it can cause secondary colonization and sometimes fistulas, especially cysto-pleural fistulas.
Complications of human cystic echinococcosis do not appear to be very frequent, albeit not rare. Rupture of the cyst affects 3–17% of patients depending on the case study; it mainly involves the bile ducts, where it can exceed 9%, but it also occurs in the thorax, in the abdominal cavity and in subcutaneous and subdiaphragmatic tissues [14–16]. Ruptures into the suprahepatic veins and gastrointestinal tract are rare [17,18].
In this study, the incidence of complications of human cystic echinococcosis in 221 patients was 9% and 7.4% among 294 hydatid cysts. Rupture of cysts was contained in 0.7% of cases (2 cysts in 2 patients with allergic rash), communicating in 4.4% (13 cysts: 6 superinfected cysts, 5 cysts ruptured into the bile ducts, 2 cysts complicated by bilomas) and direct in 2.3% of cases (2 cysts with cysto-pleural fistulas, 1 cyst ruptured into the peritoneum, 1 ruptured in the spleen and 3 communicating hepatic–pulmonary–muscular cysts).
The most frequent complication was superinfection involving 9 patients (45%) of whom 2 (10%) with cysto-pleural fistulas followed by rupture into the bile ducts (25%). Allergic reactions (10%) and bilomas (10%) were infrequent and rupture directly into the peritoneum (5%) was rare.
The incidence of complications evaluated per organ showed high percentages for muscles and spleen (25 and 11.1%, respectively), but these results are not significant because of the small number of patients with lesions in these sites.
In the liver and lungs, complication rates were comparable to those for the total sample (7.9% and 7.1%, respectively), whereas the peritoneum involvement was low. The incidence of complications was higher when only the cysts presenting echographic signs of activity were considered (143 patients with 210 cysts): 14.0% of patients and 10.5% of cysts. Hepatic cysts presented the greatest number of complications, representing 77.2% of all complications (17/22). However, the incidence per organ was not significantly different from that of pulmonary cysts (7.9% versus 7.1%).
Complications of cystic echinococcosis of the peritoneum and spleen were rare, although the latter are particularly important since rupture of the splenic parenchyma can cause life-threatening hemoperitoneum.
In the literature, the most frequently reported complication of human cystic echinococcosis is rupture into the bile ducts. However, in the present study this complication was second to superinfection. This difference is perhaps due to the fact that the present study considered complications of hydatidosis of all organs, whereas most reports in the literature involve surgical case studies that mainly evaluate the complications of parasitic liver infestation. In addition, suppuration of hydatid cysts of the liver is frequently due to ruptures communicating with the bile ducts through which germs can enter the cyst.
In most cases, US yields a diagnosis of the parasitic pathology and the presence of complications, but CT and MR may be required to confirm clinical–echographic suspicions [19,20]. In cases of rupture of the cyst into the bile ducts, US can also reveal indirect signs of complications, such as dilation of the bile ducts and communication of the cyst with a bilio-vascular branch, as well as direct signs characterized by the presence of echogenic material without acoustic shadow in the common bile duct. However, endoscopic papillotomy is the gold standard method to confirm the presence of hydatid material in the common bile duct.
US shows high sensitivity in suspected suppurative hepatic lesions, but a hepatic abscess or parasitic cyst complicated by infection requires confirmation by means of percutaneous US-guided drainage. These considerations are relevant for all the abdominal organs and for all pathologies that cause collections of liquid, such as cysts, pseudocysts and hematomas.
In this study, percutaneous US-guided aspiration was used for diagnostic purposes in 65% of cases, i.e. in all cases of suspected suppuration of the cyst (9 patients), in suspected bilomas (2 patients), suspected rupture into the peritoneum (1 patient) and intrasplenic rupture (1 patient). It allowed rapid confirmation of the diagnosis, and in 9 of the 11 suppurative cysts (81.8%), cultivation of the liquid permitted identification of the germ responsible for the infection and a specific antibiotic therapy. However, it would be particularly interesting to know if US could be used to evaluate the risk of complication of a hydatid cyst.
In the present study, 11 hepatic lesions, i.e. 50% of cysts with complications including 4 suppurative cysts, 5 ruptures into the bile ducts and 2 causing bilomas, were in close contact with the bile ducts, whereas 4 lesions, i.e. 18.1% including cysts fistulated into the pleura, 1 communicating with pulmonary cysts and 1 opening directly into the peritoneum, were subglissonian.
Therefore, particularly in cysts in the active phase, hepatic US can be used to evaluate the site of the lesion (relations with the bile ducts, Glisson's capsule and the diaphragm) and, if necessary, to plan more frequent follow-ups of the treated lesions.
Until a few years ago, treatment of complications in echinococcosis, like that of hydatid disease, was largely surgical [15,20,21], but some recent studies have demonstrated that endoscopic papillotomy is a valid procedure in the rupture of human cystic echinococcosis into the bile passages. It provides a certain diagnosis, shown by hydatid membranes exiting the common bile duct, while the opening of the papilla allows elimination of the membranes and protoscolices and resolution of the biliary obstruction, thus allowing medical treatment of the cyst (Albendazole). This method has furthermore a very low incidence of complications, no mortality and short hospital stays [22].
In the present study, 5 patients with rupture of hydatid cysts into the bile ducts underwent papillosphincterotomy to confirm the US suspicion but particularly to treat the obstruction. This resolved the complication and allowed treatment with Albendazole for 6 months, leading to complete remission of the hepatic parasitic pathology.
Drainage and percutaneous US-guided aspiration have been used for twenty years in clinical practice in the treatment of abdominal abscesses, particularly hepatic abscesses, and lead to resolution of the pathology in over 90% of cases with a low percentage of complications and short hospital stays. This US-guided method is furthermore indicated in the aspiration of non-suppurative fluid collections, such as bilomas, pseudocysts and hematomas. More recently, these therapeutic methods have allowed resolution of suppurative hydatid cysts and collections of bile, either spontaneous or post-surgical, in the course of hydatidosis or not, thus constituting an alternative to surgery in the treatment of complications of echinococcosis.
In this study, drainage and percutaneous US-guided aspiration were of particular therapeutic use, allowing resolution of the drained fluid collections in 78.5% of cysts and in 75% of treated patients. It was ineffective only in 3 patients affected by a suppurative cyst, a cyst fistulated into the pleura and a biloma, subsequently treated with surgery (used in this study in only 15% of patients).
Conclusions
In conclusion, patients affected by abdominal or extra-abdominal cystic hydatidosis in the active phase are at risk of rupture of the cyst due to the increased intracystic pressure. This can in an elevated number of cases give rise to serious complications. Diagnosis is possible in most cases by means of US, a method with high sensitivity and specificity also in these pathologies, particularly if associated with percutaneous US-guided sampling. US-guided and endoscopic diagnostic procedures and interventional therapies can provide confirmation of the diagnosis and often resolution of the complications without the need of surgical therapy (required only in non-responsive or relapsing cases).
References
- 1.Caremani M., Maestrini R., Occhini U. Echographic epidemiology of cystic hydatid disease in Italy. Eur J Epidemiol. 1993;9:401–404. doi: 10.1007/BF00157397. [DOI] [PubMed] [Google Scholar]
- 2.Frider B., Larrieu E., Odriozola M. Long-term outcome of asymptomatic liver hydatidosis. J Hepatol. 1999;30:228–231. doi: 10.1016/s0168-8278(99)80066-x. [DOI] [PubMed] [Google Scholar]
- 3.Gharbi H.A., Hassine W., Brauner M.W., Dupuch K. Ultrasound examination of the hydatid liver. Radiology. 1981;139:459–463. doi: 10.1148/radiology.139.2.7220891. [DOI] [PubMed] [Google Scholar]
- 4.Caremani M., Benci A., Maestrini R., Rosi G., Menchetti D. Abdominal cystic hydatid disease: classification of sonographic aspect and response to treatment. J Clin Ultrasound. 1996;24:491–500. doi: 10.1002/(SICI)1097-0096(199611/12)24:9<491::AID-JCU1>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 5.Caremani M., Benci A., Maestrini R., Accorsi A., Caremani D., Lapini L. Ultrasound imaging in cystic echinococcosis. Proposal of a new sonographic classification. Acta Trop. 1997;67:91–105. doi: 10.1016/s0001-706x(97)00057-0. [DOI] [PubMed] [Google Scholar]
- 6.Macpherson C.N.L. Use of ultrasound in the diagnosis of parasitic disease. Trop Doct. 1992;22:14–20. doi: 10.1177/004947559202200104. [DOI] [PubMed] [Google Scholar]
- 7.Garcia F.J., Marti-Bonmati L., Menor F., Rodriguez B., Ballet A. Echogenic forms of hydatid cysts: sonographic diagnosis. J Clin Ultrasound. 1990;16:305–311. doi: 10.1002/jcu.1870160505. [DOI] [PubMed] [Google Scholar]
- 8.WHO Informal Working Group on Echinococcosis Guidelines for treatment of cystic and alveolar echinococcosis in humans. Bull World Health Organ. 1996;74:231–242. [PMC free article] [PubMed] [Google Scholar]
- 9.Pawlowski Z., Eckert J., Vuitton D. Echinococcosis in humans: clinical aspects, diagnosis and treatment. In: Eckert J., Gemmel M.A., Meslin F., Pawlowski Z., editors. WHO/OIE manual on echinococcosis in humans and animals: a public health problem of global concern. WHO/OIE; Paris, France: 2001. pp. 20–71. [Google Scholar]
- 10.Wen H., New R.R.C., Craig P.S. Diagnosis and treatment of human hydatidosis. Br J Clin Pharmacol. 1993;35:565–574. doi: 10.1111/j.1365-2125.1993.tb04182.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Filice C., Pirola F., Brunetti E., Dughetti S., Strosselli M., Foglieni C.S. A new therapeutic approach for hydatid liver cysts: aspiration and alcohol injection under sonographic guidance. Gastroenterology. 1990;98:1366. doi: 10.1016/0016-5085(90)90358-8. [DOI] [PubMed] [Google Scholar]
- 12.Lewall D.B., McCorkell S.J. Rupture of echinococcal cysts: diagnosis, classification and clinical implication. AJR Am J Roentgenol. 1986;146:391–394. doi: 10.2214/ajr.146.2.391. [DOI] [PubMed] [Google Scholar]
- 13.Murty T.V.M., Sood K.C., Fawzi S.R. Biliary obstruction due to ruptured hydatid cyst. J Pediatr Surg. 1989;24:401–403. doi: 10.1016/s0022-3468(89)80281-7. [DOI] [PubMed] [Google Scholar]
- 14.Becker K., Fieling T., Saleh A., Haussinger D. Resolution of hydatid liver cyst by spontaneous rupture into the biliary tract. J Hepatol. 1997;26:1408–1412. doi: 10.1016/s0168-8278(97)80479-5. [DOI] [PubMed] [Google Scholar]
- 15.Stoianov G., Damianov N., Angelov A., Dimitrov A. Perforations of hepatic hydatid cysts. Khirurgiia. 1997;50:8–10. [PubMed] [Google Scholar]
- 16.Kornaros S.E., Aboul-Nour T.A. Frank intrabiliary rupture of hydatid hepatic cyst: diagnosis and treatment. J Am Coll Surg. 1996;183:466–470. [PubMed] [Google Scholar]
- 17.Diez Valladares L., Sanchez-Pernaute A., Gonzalez O. Hydatid liver cyst perforation into the digestive tract. Hepatogastroenterology. 1998;45:2110–2114. [PubMed] [Google Scholar]
- 18.Coskun I., Esenturk M., Yoruk Y. The rupture of hepatic hydatid disease into the right hepatic vein and bile ducts: a case report. Hepatogastroenterology. 1996;43:1006–1008. [PubMed] [Google Scholar]
- 19.Mazziotti S., Gaeta M., Blandino A., Barone M., Salamone I. Hepatobronchial fistula due to transphrenic migration of hepatic echinococcosis: MR demonstration. Abdom Imaging. 2000;25:497–499. doi: 10.1007/s002610000080. [DOI] [PubMed] [Google Scholar]
- 20.Paksoy M., Karahasanoglu T., Carkman S. Rupture of the hydatid disease of the liver into the biliary tract. Dig Surg. 1998;15:25–29. doi: 10.1159/000018582. [DOI] [PubMed] [Google Scholar]
- 21.Rothlin M.A. Fatal intraoperative pulmonary embolism from a hepatic hydatid cyst. Am J Gastroenterol. 1998;93:2606–2607. doi: 10.1111/j.1572-0241.1998.00562.x. [DOI] [PubMed] [Google Scholar]
- 22.Greulich T., Kohler B. Obstructive jaundice caused by spontaneous rupture of an Echinococcus granulosus cyst into the bile duct system. Z Gastroenterol. 2000;38:301–306. [PubMed] [Google Scholar]


