Abstract
Lesions of the quadriceps muscle (QM) are frequently seen by sonographers, and in most cases they are the result of sports-related trauma. An accurate assessment of the severity of the lesion is essential, particularly when the patient is a professional athlete. In most cases, careful history-taking and a thorough physical examination are sufficient for making the diagnosis and indicating the most suitable imaging studies for each case. Clinical assessment alone, however, may not be sufficient for distinguishing contusions from small, partial tears or for estimating the size of a tear. Therefore, at least in patients who are professional athletes, imaging studies are necessary to plan appropriate therapy that will allow prompt functional recovery. Muscles cannot be visualized with conventional radiography, but it is used routinely in prepubertal patients because it can detect apophyseal detachments, which are the most frequent muscle lesion in this age group. Radiography is also useful when myositis ossificans is suspected. Magnetic resonance imaging, thanks to its excellent tissue contrast, allows simultaneous assessment of muscle, joint, and bone planes. It remains a second-line study due to its high cost and relatively low availability. It is also associated with various contraindications, the most important of which is the presence of a cardiac pacemaker. Ultrasonography has a number of advantages, including widespread availability, absence of contraindications, and low cost. It can also be used for dynamic studies of the muscle during contraction and relaxation, and if doubts arise, scans can easily be obtained of the contralateral muscle for comparison purposes. These qualities make it an excellent tool for follow-up of patients with QM lesions, when follow-up is necessary. This article reviews the anatomy of the QM, the technique used for standard ultrasound examination of this muscle, its normal appearance on ultrasound, and the sonographic characteristics of the most common traumatic lesions that affect it.
Keywords: Quadriceps muscle, Sonography, Trauma, Sports
Sommario
Le lesioni del muscolo quadricipite (MQ) sono frequenti nella pratica ecografica quotidiana e, nella gran maggioranza dei casi, sono secondarie a traumi, per lo più sportivi. Un’accurata valutazione della gravità delle lesioni è necessaria, in particolare quando siano coinvolti sportivi di alto livello.
L’accurata raccolta dell’anamnesi, unitamente ad un esame obiettivo scrupoloso e condotto in una maniera rigorosa, permettono, nella maggior parte dei casi, di porre una diagnosi e di orientare verso l’imaging più idoneo per ciascun paziente. La sola valutazione clinica comunque non è sufficiente per differenziare le contusioni dalle piccole lesione parziali o valutare con precisione le dimensioni delle rotture. Una metodica di imaging è quindi necessaria per lo meno negli sportivi professionisti al fine di programmare una corretta terapia, volta al migliore recupero funzionale nei tempi più brevi. La radiografia tradizionale non consente di visualizzare i muscoli, tuttavia, essa viene realizzata routinariamente nell’età peri-puberale in quanto permette di diagnosticare i distacchi apofisari, più frequenti delle lesioni muscolari in questa fascia d’età. La radiografia è anche utile nel sospetto di ossicalcificazione intramuscolare circoscritta. La risonanza magnetica, grazie al suo ottimo contrasto tissutare, permette di giudicare simultaneamente il piano muscolare, articolare ed osseo. L’esame resta comunque, a causa della reperibilità ancora non ottimale e del suo alto costo, un esame di seconda istanza. Presenta varie controindicazioni di cui la principale è la presenza di uno stimolatore cardiaco. L’ecografia presenta numerosi vantaggi fra cui la larga diffusione, la mancanza di controindicazioni, il basso costo, la possibilità di realizzare un esame dinamico in contrazione e rilassamento del muscolo e di comparare i reperti con il lato sano in caso di dubbi. Le qualità intrinsiche della metodica ne fanno un esame ottimale per il follow-up delle lesioni, quando ciò sia necessario. In questo articolo, dopo aver ricordato l’anatomia del MQ, presentiamo la tecnica di realizzazione standard dell’esame ecografico e l’anatomia ecografica normale, quindi i quadri ecografici delle più comuni lesioni traumatiche.
Normal anatomy of the quadriceps muscle (Figs. 1–3)
Fig. 1.
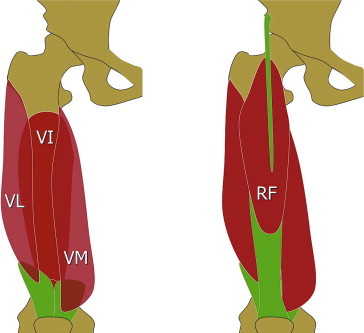
Anatomy of the quadriceps muscle. a = deep plane; b = superficial plane; VL = vastus lateralis; VI = vasto intermedius; VM = vastus medialis; RF = rectus femoris.
Fig. 2.
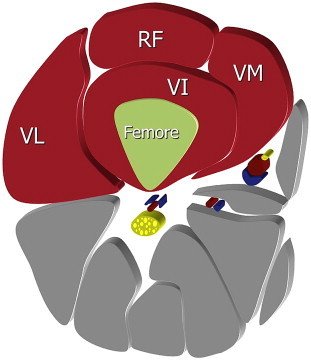
Anatomy of the quadriceps muscle. Axial plane (diagram): VL = vastus lateralis; VI = vasto intermedius; VM = vastus medialis; RF = rectus femoris.
Fig. 3.
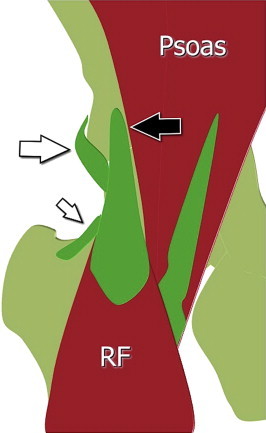
Anatomy of the proximal rectus femoris. RF = rectus femoris; black arrow = direct tendon and its insertion on the anteroinferior iliac spine; white arrow = indrect tendon and its insertion on the lateral aspect of the acetabular rim; small white arrow = reflected tendon and its insertion on the anterior articular plane.
The quadriceps muscle (QM) is located in the anterior compartment of the thigh [1–4]. It is composed of 4 muscle bellies: the rectus femoris (RF), which lies in the anterior portion of the thigh; the vastus medialis (VM) and vastus lateralis (VL) on the inner and outer portions, respectively; and the vastus intermedius (VI), which is located posteriorly [5]. The vastus muscles originate from the anterior, medial, and lateral aspects of the femur. The RF originates from the anterior inferior iliac spine (AIIS), and it has three proximal tendons: the straight or direct tendon, which arises from the AIIS; the indirect tendon that inserts into the superolateral rim of the acetabulum; and a small reflected tendon that inserts into the anterior capsule of the hip joint. The direct and indirect tendons continue in 2 aponeurotic laminae that extend to the lower third of the muscle. The direct tendon continues as the superficial lamina; the indirect tendon as the central sagittal lamina [6].
The 4 bellies of the QM converge distally to form the thick quadriceps tendon, which inserts into the superior pole of the patella. The tendon is composed of multiple laminae positioned one on top of the other. The superficial lamina is continuous with the muscle fibers of the RF. The intermediate lamina receives the fibers of the VM and VL, and the deepest lamina receives the fibers of the VI. A fairly small portion of the fibers of the superficial lamina lies superficial to the patella and merge directly into the patellar tendon. The description supplied above corresponds to that provided by most anatomy textbooks, but recent studies based on anatomical dissections, have revealed considerable variability in the composition of the distal tendon [7].
Sonographic examination of the quadriceps muscle: technique and normal US anatomy (Figs. 4–6)
Fig. 4.
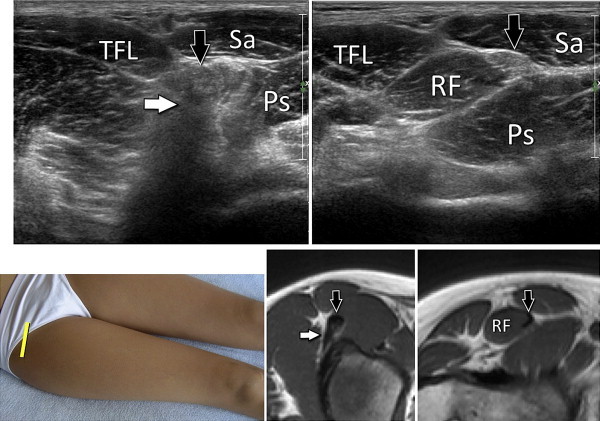
The proximal half of the rectus femoris muscle: sonographic anatomy and MRI correlates. Axial plane. RF = rectus femoris; black arrow = direct tendon; white arrow = indrect tendon. TFL = tensor of the fascia lata, Sa = sartorius, Ps = psoas.
Fig. 5.
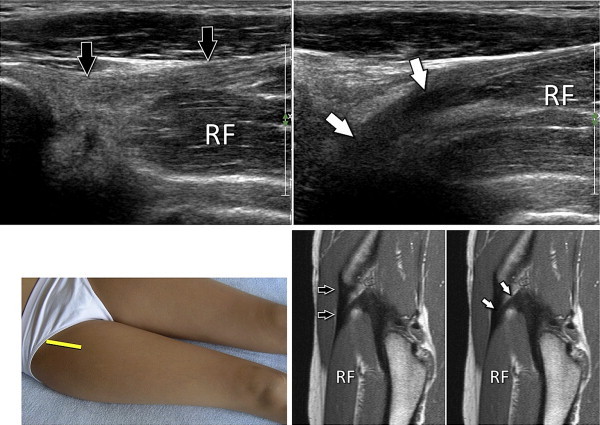
The proximal half of the rectus femoris muscle: sonographic anatomy and MRI correlates. Sagittal plane. RF = rectus femoris; black arrow = direct tendon; white arrow = indrect tendon.
Fig. 6.
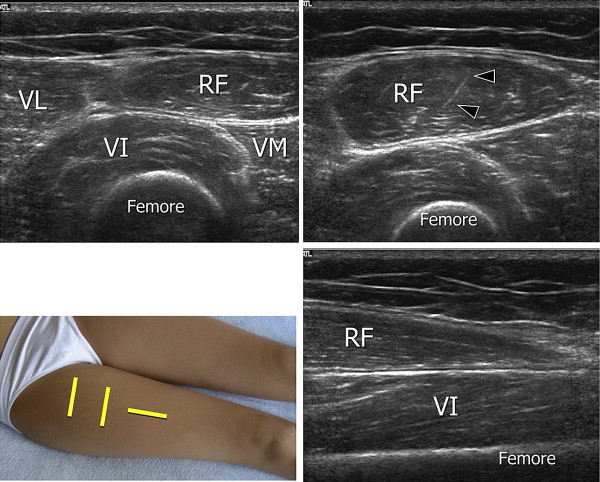
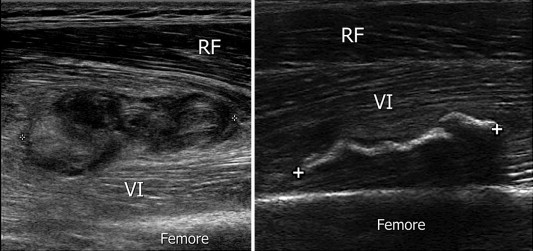
Sonographic anatomy of the middle third of the quadriceps muscle (a,b: axial plane) and the distal portion of the rectus femoris (c: sagittal plane). VL = vastus lateralis; VI = vasto intermedius; VM = vastus medialis; RF = rectus femoris.
The patients are examined in the dorsal decubitus position with the hip and knee in the neutral position [8]. Internal or external rotation of the lower limb is necessary for complete assessment of the lateral or medial aspect of the muscle. The examination can be done with a moderate- to high-frequency transducer, depending on the thickness of the muscle. A good overall evaluation of the QM can usually be achieved with a multifrequency (5–12-MHz) linear transducer. If there is substantial muscle hypertrophy, a 5-MHz transducer is preferable as it offers better visualization of the deep planes. A systematic approach will allow complete exploration of the QM and reveal even small lesions that can easily be missed.
In the first phase, axial scans are made at the level of the RF tendon. As a rule, the examination begins at the proximal end of the muscle and proceeds distally. The axial scans are done first because they provide more panoramic views. Areas of interest are then explored with longitudinal scans [9]. A fundamental landmark in examinations of the cranial portion of the RF is the anterior superior iliac spine, which can be readily identified by palpation. The transducer is placed over this structure on the axial plane and moved distally for 4–5 cm to visualize the AIIS, which is the insertion point for the direct tendon of the RF. The indirect tendon, which follows an oblique course, is examined with an oblique axial scan at the lateral aspect of the uppermost portion of the thigh. The tendon is then examined with oblique coronal scans. The medial and distal portions of the RF are examined with axial scans, advancing the transducer distally. The anterior and central aponeuroses are clearly visualized: the latter is shaped like a comma, the former is visualized as a thickening of the muscle fascia. The examination continues with exploration of the vastus muscles, which are scanned axially and then longitudinally. Information obtained during the static examination can be supplemented with a dynamic examination performed during isometric muscle contraction. This approach is sometimes more suitable for detecting small partial tears. When the muscle plane has been fully explored, the distal tendon is scanned. During this phase, the knee is flexed approximately 30° to straighten the tendon. This eliminates anisotropy artifacts, which result in hypoechoic areas in the distal portion of the tendon that may be mistaken for focal tendinopathy or even partial ruptures. The tendon is examined first with sagittal scans and then in the axial plane.
Ultrasonography allows excellent visualization of the proximal tendons of the RF. The straight tendon is cylindrical with smooth borders. Some degree of thickening at the level of the cranial insertion is normal. The internal structure is homogeneously hyperechoic. On axial scans, the tendon is visualized as a more or less oval-shaped structure located medial to the indirect tendon. The latter tendon, owing to its oblique course, is often associated with substantial posterior shadowing that can be mistaken for intratendinous calcification. Sagittal images allow complete exploration of the direct tendon from its insertion into the AIIS to the myoaponeurotic junction. Moving the transducer laterally reveals the indirect tendon, a hypoechoic band that descends toward the upper rim of the acetabulum. It is visualized best on oblique axial images.
Axial scans of the RF muscle reveal its characteristic internal architecture, which is related to the presence of the vertical aponeurosis [9]. The latter is represented by a mildly curved, comma-shaped hyperechoic structure, which is normally quite distinct from the muscle tissue and extends as far as the lower third of the muscle [9,15]. In the sagittal plane, it appears much more difficult to assess owing to its orientation and thickness. The internal fibers of the vastus muscles are not arranged in any particular manner. They are characterized by the presence of short connective-tissue septa. The fascia that surrounds each of the vastus muscles is clearly visualized as a thin hyperechoic layer. Their presence allows one to distinguish the VI from the VM and RF. Distinguishing the VL from the VI is more difficult because these two muscles merge laterally.
On longitudinal scans the quadriceps tendon appears to be composed of 3 or 4 hyperechoic tendinous laminae separated by thin hypoechoic bands, which represent lax connective tissue. The distal insertion of this tendon into the superior pole of the patella can be well visualized only when the knee is flexed.
Clinical and phatophysiological aspects
Muscle lesions are frequently associated with sports-related or occupational trauma [10–13]. In some sports, like soccer, they account for around 40% of all injuries, and recurrent trauma can keep an athlete off the field for months. Muscle lesions can be divided into 3 main etiopathogenetic groups: lesions caused by direct trauma (contusions); those caused by indirect trauma (sprains), which usually occur during eccentric contraction; and rare lesions caused by cuts (lacerations).
Contusions are classified as mild, moderate, or severe, depending on the limitation of joint movement they cause. Sprains, too, are divided into 3 classes according to the number of muscle fibers involved: first-degree sprains, which involve a few of the fibers within a muscle fascia; second-degree sprains, in which the surface of the damaged fascia represents less than ¾ of the total section of the muscle; and third-degree sprains, in which the surface of the rupture amounts to more than ¾ of the total section and may extend to the entire muscle belly (complete rupture).
Clinically speaking, sprains have three typical characteristics: 1) sharp pain associated with a technical movement, 2) the injured area can be located with precision by the patient and verified by careful palpation; 3) impaired mobility that varies with the severity of the lesion. Within the QM, the VL and VI are the most frequent targets of direct trauma because they are the muscles that are most exposed during sports activities. The RF is the main site of indirect trauma, and in 60% of the cases, the lesion involves the proximal third of the muscle. The distal third is affected in only 10% of the cases, but most of these involve second or third-degree lesions.
As noted above, indirect trauma occurs for the most part as a result of eccentric contractions [9,11,14,15]. This can occur, for example, when soccer or rugby players unexpectedly encounter irregular or slippery turf as they are about to kick a ball. As a result, they miscalculate the position or speed of the ball and try to compensate for their error by extending the hip. The muscle at risk in this situation is the biarticular RF, more specifically the proximal third of the RF. This type of injury can also occur when one loses one’s footing during abrupt deceleration, an event that is common in all sports that involve running. In some cases, the lesion involves the reflected tendon of the RF, which, as we have seen, arises from the acetabular rim. These lesions may mimic hip pain or a lesion of the tensor fascia lata. The athlete reports the sensation that something in the hip was displaced during the trauma and complains of pain in the region of the tensor fascia lata. Together with the long head of the biceps femoris, the RF is the muscle most frequently involved in recurrent indirect trauma, i.e., a new lesion involving the same area of the muscle (or at least the same muscle) that occurs within 6 months of the initial injury. The typical clinical manifestations of the recurrent lesions are similar to those of the primary lesion.
If a muscle lesion is neglected or inappropriately treated, complications can arise. The most common are cicatricial fibrosis, calcification, fluid collections, serohematic pseudocyst formation, and circumscribed intramuscular ossicalcification. The most common complication of direct trauma to the QM (and other muscles as well) is myositis ossificans whereas indirect trauma is more frequently associated with cicatricial fibrosis. In general, the clinical manifestations include pain or discomfort, which is frequently continuous and may be exacerbated by even minor movements. In cases of circumscribed intramuscular ossifcation, the pain, which is often intense and disabling, is associated with palpable thickening of the muscle that lasts days or weeks. It can be aggravated by inappropriate therapy (heat, deep muscle-relaxant massages) and by excessive or premature exertion while the muscle is still painful.
Prompt diagnosis (within a few days of the muscle trauma) is essential to ensure timely and complete healing and to reduce the likelihood of recurrence. For this reason, imaging studies are important. Together with the clinical findings, they help the physician identify the lesion, and they can be repeated as needed to monitor the progress of healing [14].
Pathologic sonographic findings
Pediatric patients (Figs. 7 and 8)
Fig. 7.
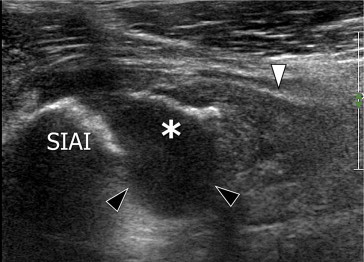
Disinsertion of the anteroinferior iliac spine: Sonographic appearance. This sagittal scan demonstrates avulsion of a fragment (asterisk) of the anterior inferior iliac spine (AIIS). The hematoma caused by the acute avulsion appears as an anechoic fluid collection (black arrowhead). The direct tendon is thickened and hypoechoic (white arrowhead).
Fig. 8.
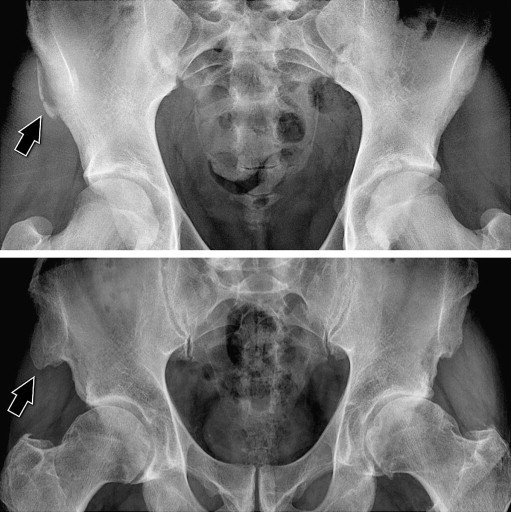
Radiographic appearance of disinsertion of the anteroinferior iliac spine. Acute lesion: This A-P radiograph of the pelvis reveals acute avulsion of the right AIIS (arrow). Chronic lesion: Radiograph of another patient shows hypertrophy of the AIIS.
Owing to the presence of the AIIS growth cartilage, indirect trauma in children usually causes avulsione ossea instead of muscle lesions [16–18]. In young persons, the pain is most intense during palpation of the spina ossea. Anterior-posterior roentgenograms of the pelvis ed eventualmente in obliqua alare posteriore will clearly reveal the avulsion of the cartilage. The degree of retraction and the size of the bone fragment can also be evaluated. X-rays taken in athletes years after an avulsion show hypertrophy of the inferior iliac spine, which appears as a large calcification that projects into the inferior soft tissues. Sonography confirms the diagnosis. The avulsed fragment is seen as a hyperechoic structure of variable size lying at some distance from the AIIS.
When the insertion of the quadriceps tendon on the superior pole of the patella is subjected to excessive traction in a young athlete, it can cause bone avulsion associated with chondral fracture of the retropatellar cartilage (sleeve fracture) [18].
Pathology in adults
Traumatic lesions of the rectus femoris
In adults, after the growth cartilages have undergone ossification, the damage caused by indirect trauma to the muscles is almost always located at the myotendinous junctions. At the level of the QM these lesions almost always involve the distal third of the RF, where the rupture involves the insertion of the muscle fibers on the central sagittal lamina, or at the distal myotendinous insertion [8,9,14,15].
In cases involving mild proximal trauma, the muscle tissue surrounding the central lamina of the tendon appears hyperechoic owing to the presence of a hemorrhagic infiltrate. The volume of the muscle is not increased (grade 1 lesion). Grade 2 lesions are associated with partial rupture of the muscle fibers and a fluid collection (hematoma) surrounding the central aponeurosis, and the muscle tissue surrounding the hematoma itself is infiltrated with blood (Fig. 9). As a result, the belly of the muscle appears enlarged, and this finding may lead to a biopsy for suspected muscle tumor [19]. Type 3 lesions are characterized by complete rupture of the muscle and more or less evident retraction of the muscle bellies. Healing of these lesions is sometimes followed by local retraction secondary to scar formation. The sonogram demonstrates fibrosis reflected by poorly delimited hyperechoic areas associated with focal retractions of the adjacent muscle fibers (Fig. 10) [20].
Fig. 9.
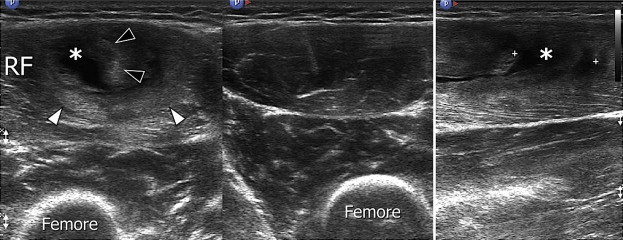
Proximal myoaponeurotic disinsertion of the rectus femoris. Sonographic appearance. Acute lesion. Axial scan (a) reveals a grade 2 lesion. The volume of the muscle is increased compared with that of the contralateral muscle (b). The central lamina (black arrowheads) is surrounded by a hypoechoic hematoma (asterisk). Hemorrhagic infiltration of the peripheral portion of the muscle is reflected by a hyperechoic zone (white arrowheads). Longitudinal scan (c) reveals the hematoma and the retracted proximal stump of the muscle.
Fig. 10.
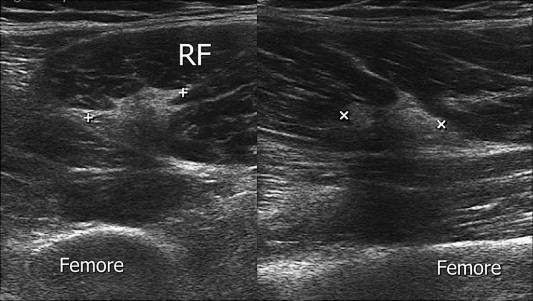
Proximal myoaponeurotic disinsertion of the rectus femoris, chronic lesion. Sonographic appearance in the axial (a) and sagittal (b) planes. The hematoma has been replaced by a fibrocicatricial nodules (calipers), which appears as a star-shaped hyperechoic area and causes retraction of the muscle fibers.
Distal lesions are almost always myoaponeurotic disinsertions of the muscle from the deep lamina of the tendon (Fig. 11). Sonography shows proximal retraction of the muscle, the lower portion of which appears round. Acute lesions are always associated with an anechoic hematoma, which fills the space vacated by the retracted muscles. Longitudinal sonographic images are particularly useful for assessing proximal retraction. Axial images are necessary to distinguish partial from total ruptures. Dynamic studies carried out during muscle contraction reveals retraction of the muscle bellies. If necessary, the hematoma can be drained easily with a 19-gauge needle under real-time ultrasound guidance. Aspiration of the hematoma should be as complete as possible and it must be followed by application of a pressure dressing to prevent recurrence. Color Doppler studies will sometimes reveal a fair amount of perilesional hyperemia. Most distal lesions heal without functional sequelae, and they are associated with a better prognosis than proximal lesions [14]. Ultrasonography allows the physician to monitor in detail the healing process. The hematoma is gradually replaced with fibrotic tissue that appears hyperechoic. In the presence of chronic lesions, the muscle appears hypotrophic with a hyperechoic appearance that reflects fatty infiltration secondary to disuse (Fig. 12).
Fig. 11.
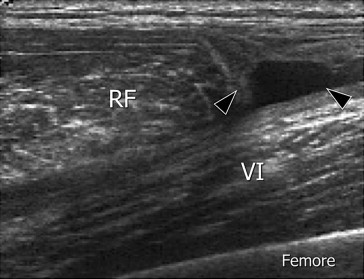
Acute distal myoaponeurotic disinsertion of the RF. Sonographic appearance in the sagittal plane shows proximal retraction of the muscle, which has a rounded shape. The distal hematoma appears as an anechoic fluid collection (black arrowheads). VI = vastus intermedius.
Fig. 12.
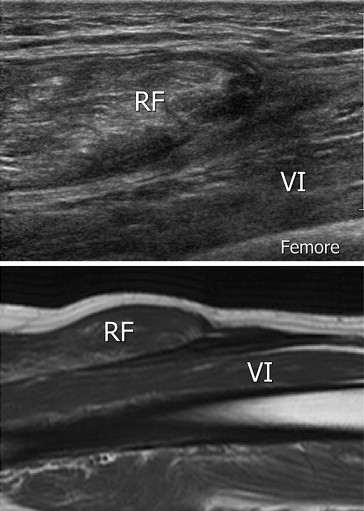
Chronic distal myoaponeurotic disinsertion of the rectus femoris. Appearance on sonography and magnetic resonance imaging. The sagittal US image shows. The distal hematoma presents clear signs of organization and early fibrosis.
Traumatic lesions involving the vastus muscles
In the vast majority of cases, the mechanism underlying lesions involving the three vastus muscles is not intrinsic but extrinsic, that is related to contusions provoked during athletic activities. The most common targets are the VL and the VI, and in most cases the injury consists in partial ruptures, which appear on ultrasonography as discontinuities in the normal striated pattern of the muscle associated with internal hematomas (Fig. 13). In these cases, sonography allows the physician to obtain accurate measurements of the lesions and, if needed, to eliminate the blood collections by means of needle aspiration. Lesions involving the VI are usually larger, and they can result in substantial increases in muscle thickness. Given the depth and increased thickness of the muscle, a 5-MHz transducer will usually be needed to ensure detailed visualization of the structural damage. In the presence of chronic lesions, the sonogram will disclose the presence of an irregularly shaped, hyperechoic, fibrocicatricial nodule. The presence of calcifications in myositis ossificans is visualized on sonography as hyperechoic images with posterior shadowing that interrupt the hyperechoic line corresponding to the anterior cortex of the femur. If the lesions are not mature yet, the sonogram will also reveal significant changes in the muscle structure, and a fair amount of vascularization will be evident on color Doppler studies. Suspicions should always be confirmed with conventional radiographic studies.
Fig. 13.
Acute (a) and chronic (b) traumatic lesions of the vastus intermedius. In the acute lesion, direct trauma caused laceration of the muscle fibers and local hematoma formation, which are reflected by the presence of an irregularly shaped area with echostructural heterogeneity. The deep portion of the vastus intermedius (VI) and rectus femoris (RF) are normal. The chronic lesion appears hyperechoic with posterior shadowing caused by circumscribed intramusclular ossicalcification.
Conclusions
Traumatic lesions of the QM are frequently seen in persons who practice sports. Clinical assessment is indispensable and provides clues as to the most appropriate diagnostic studies. Magnetic resonance imaging allows good visualization of the QM as well as of the coxofemoral region, the knee, and the bone plane, but it is not always available and in any case it is quite costly. When ultrasonography is performed by adequately trained personnel with high-quality equipment, it offers excellent visualization of the QM and the tendon plane. In the vast majority of cases, sonography is the only examination performed. It can also be used during the follow-up phase, when it is quite useful for determining when an athlete can resume agonistic activity. In selected cases, ETG can be used to guide needle aspiration of hematomas.
Conflict of interest
The authors have no conflict of interest.
References
- 1.Standring Susan. 40th British ed. Churchill Livingstone; 2008. Gray’s anatomy, hardback. [Google Scholar]
- 2.Hollinshead W.H., Rosse C. 4th ed. Harpour and Row Publishers; 1985. Textbook of anatomy. pp. 376–77. [Google Scholar]
- 3.Rouvière H. Masson et Cie; 1974. Anatomie humaine, descriptive, topographique et fonctionnelle. Edition. pp. 354. [Google Scholar]
- 4.Mo Chammout, Skinner H.B. The clinical anatomy of commonly injured muscle bellies. J Trauma. 1986;26:549–552. doi: 10.1097/00005373-198606000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Becker I., Woodley S.J., Baxter G.D. Gross morphology of the vastus lateralis muscle: an anatomical review. Clin Anat. 2009;22:436–450. doi: 10.1002/ca.20792. [DOI] [PubMed] [Google Scholar]
- 6.Hasselman C.T., Best T.M., Hughes C., 4th, Martinez S., Garrett W.E., Jr. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med. 1995;23:493–499. doi: 10.1177/036354659502300421. [DOI] [PubMed] [Google Scholar]
- 7.Waligora A.C., Johanson N.A., Hirsch B.E. Clinical anatomy of the quadriceps femoris and extensor apparatus of the knee. Clin Orthop Relat Res. 2009;467:3297–3306. doi: 10.1007/s11999-009-1052-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bianchi S., Martinoli C. Thigh. In: Bianchi S., Martinoli C., editors. Musculoskeletal ultrasound. Springer-Verlag; 2007. p. 974. pp. 611–636. [Google Scholar]
- 9.Bianchi S., Martinoli C., Waser N.P., Bianchi-Zamorani M.P., Federici E., Fasel J. Central aponeurosis tears of the rectus femoris: sonographic findings. Skeletal Radiol. 2002;31:581–586. doi: 10.1007/s00256-002-0559-z. [DOI] [PubMed] [Google Scholar]
- 10.Garrett W.E., Jr. Muscle strain injuries. Am J Sports Med. 1996;24:S2–S8. [PubMed] [Google Scholar]
- 11.Garrett W.E., Jr. Muscle strain injuries: clinical and basic aspects. Med Sci Sports Exerc. 1990;22:436–443. [PubMed] [Google Scholar]
- 12.Brukner P., Khan K. 2nd ed. McGraw-Hill; Sydney, Australia: 2000. Clinical sports medicine. [Google Scholar]
- 13.Weatherall P.T., Crues J.V. Musculotendinous injury. Magn Reson Imaging Clin N Am. 1995;3:753–772. [PubMed] [Google Scholar]
- 14.Balius R., Maestro A., Pedret C., Estruch A., Mota J., Rodríguez L. Central aponeurosis tears of the rectus femoris: practical sonographic prognosis. Br J Sports Med. 2009;43:818–824. doi: 10.1136/bjsm.2008.052332. [DOI] [PubMed] [Google Scholar]
- 15.Hughes C., 4th, Hasselman C.T., Best T.M., Martinez S., Garrett W.E., Jr. Incomplete, intrasubstance strain injuries of the rectus femoris muscle. Am J Sports Med. 1995;23:500–506. doi: 10.1177/036354659502300422. [DOI] [PubMed] [Google Scholar]
- 16.McKinney B.I., Nelson C., Carrion W. Apophyseal avulsion fractures of the hip and pelvis. Orthopedics. 2009;32:42. doi: 10.3928/01477447-20090101-12. [DOI] [PubMed] [Google Scholar]
- 17.Ouellette H., Thomas B.J., Nelson E., Torriani M. MR imaging of rectus femoris origin injuries. Skeletal Radiol. 2006;35:665–672. doi: 10.1007/s00256-006-0162-9. [DOI] [PubMed] [Google Scholar]
- 18.Bates D.G., Hresko M.T., Jaramillo D. Patellar sleeve fracture: demonstration with MR imaging. Radiology. 1994;193:825–827. doi: 10.1148/radiology.193.3.7972832. [DOI] [PubMed] [Google Scholar]
- 19.Temple H.T., Kuklo T.R., Sweet D.E., Gibbons C.L., Murphey M.D. Rectus femoris muscle tear appearing as a pseudotumor. Am J Sports Med. 1998;26:544–548. doi: 10.1177/03635465980260041301. [DOI] [PubMed] [Google Scholar]
- 20.Rask M.R., Lattig G.J. Traumatic fibrosis of the rectus femoris muscle. Report of five cases and treatment. JAMA. 1972;17:268–269. [PubMed] [Google Scholar]


