Abstract
Objective
To explore shortened response formats for use with the Activities-specific Balance Confidence scale and then: 1) evaluate the unidimensionality of the scale; 2) evaluate the item difficulty; 3) evaluate the scale for redundancy and content gaps; and 4) evaluate the item standard error of measurement (SEM) and internal consistency reliability among aging individuals (≥50 years) with a lower-limb amputation living in the community.
Design
Secondary analysis of cross-sectional survey and chart review data.
Setting
Out-patient amputee clinics, Ontario, Canada.
Participants
Four hundred forty eight community living adults, at least 50 years old (mean = 68 years), who have used a prosthesis for at least 6 months for a major unilateral lower limb amputation. Three hundred twenty five (72.5%) were men.
Intervention
N/a
Main Outcome Measure(s)
Activities-specific Balance Confidence Scale.
Results
A 5-option response format outperformed 4- and 6-option formats. Factor analyses confirmed a unidimensional scale. The distance between response options is not the same for all items on the scale, evident by the Partial Credit Model (PCM) having a better fit to the data than the Rating Scale Model. Two items, however, did not fit the PCM within statistical reason. Revising the wording of the two items may resolve the misfit, and improve the construct validity and lower the SEM. Overall, the difficulty of the scale’s items is appropriate for use with aging individuals with lower-limb amputation, and is most reliable (Cronbach ∝ = 0.94) for use with individuals with moderately low balance confidence levels.
Conclusions
The ABC-scale with a simplified 5-option response format is a valid and reliable measure of balance confidence for use with individuals aging with a lower limb amputation.
Keywords: Aging, amputation, self-efficacy, rehabilitation, psychometrics, postural balance
Falling and the consequences of falling are important health issues for older individuals with a lower limb amputation. In Canada, the prevalence of falling among community dwelling individuals with a lower-limb amputation is reported to be as high as 52%.1 Further, the annual incidence of falling among older adults (≥65 years) living in the community is commonly reported to be around 30% to 33% in developed countries.2,3,4 Although most fall-related studies focus on individuals 65 years of age or older, Painter et al.5 found that among community-dwelling individuals, those 50 to 60 years old had a higher prevalence of falls than those aged 61–70, 71–80, and >81 years. The authors speculate that their findings may be due to individuals in the younger age group not yet realizing or accepting their bodies were aging and changing.5
The results of falling include injuries that may lead to functional limitations, loss of independence, and in some cases death. It has been reported that 62% of falls among older adults result in hospitalization,6 and that 20% of those falls resulting in injury lead to death.2 In fact, in 2005, of the 2305 falls that led to death in Canada, 2147 (93.1%) were suffered by adults 50 years of age and older.7 Although fall-related physical morbidities are significant, arguments have been made that the psychological consequences associated with falling, such as developing a fear of falling and/or losing balance confidence, are of equal or greater concern due to their subsequent influence on reduced quality of life and self-imposed avoidance of activities.8,9 Among the psychological consequence of falling, Miller et al.10 found balance confidence, the belief individuals have in their ability to perform daily activities without losing their balance,11 to have a greater influence on mobility and participation in daily and social activities than fear of falling among individuals with a lower-limb amputation. Balance confidence as such is important to assess among those in this population.10,12,13
Balance confidence is an important determinant of social role participation.10,14,15 Because confidence is a modifiable factor according to the tenets of Social Cognitive Theory,16 treatment strategies to address reduced or low levels of balance confidence are necessary given that optimal participation is considered a key goal of rehabilitation. Therefore, research to improve balance confidence measures for use in both clinical and research practices is warranted.
At present there are three balance confidence measures, including, the Activities-specific Balance Confidence (ABC) scale,11 the Confidence in maintaining Balance Scale (CONFbal),17 and the Balance Self-perceptions Test.18 The ABC-scale, however, is by far the most widely used measure to assess balance confidence.19 This scale was developed to assess balance confidence in high functioning older adults.11 It is a 16-item scale requiring respondents to self-rate their balance confidence from 0% to 100% in performing activities of daily living (see table 4 for the ABC-scale items). Averaging the ratings derives total scores, and higher scores reflect higher levels of balance confidence. The ABC-scale has been used with various populations and has psychometric evidence supporting its use with older adults,20 individuals with lower-limb amputations,21 and stroke.22 Several adaptations of the scale also exist, including a six item version,23 two versions utilizing shortened response formats,24,25 and several international versions (United Kingdom,26 French Canadian,22 Icelandic,24 and Chinese27). In a review of the psychological outcomes of falling,28 9 studies published between 1966 and 2003 were identified that assessed the measurement properties of the original ABC-scale using methods based on classical test theory (CTT). Results indicated that the ABC-scale had adequate to good reliability and validity.28 More specifically, the internal consistency reliability (Cronbach ∝) of the ABC-scale among individuals with lower-limb amputation was found to be 0.93, and the 4-week test-retest reliability (intraclass correlation coefficient) was 0.91 (95% CI, 0.84–0.95). Further, the evidence supported the scale’s construct validity in the form of hypothesized relationships.21
Table 4.
Average Item Difficulty in Descending Order and Frequency of Responses for each Option
| Item # | How confident are you that you will not lose your balance of become unsteady when you… | Difficulty (logits) | Frequency of responses (%) | ||||
|---|---|---|---|---|---|---|---|
| No confidence (0) | Low confidence (1) | Moderate confidence (2) | High confidence (3) | Complete confidence (4) | |||
| 16 | …walk on icy sidewalks | 1.75 | 191 (42.6) | 92 (20.5) | 96 (21.4) | 52 (11.6) | 17 (3.8) |
| 6 | …stand on a chair to reach | 1.14 | 211 (47.1) | 50 (11.2) | 70 (15.6) | 66 (14.7) | 51 (11.4) |
| 15 | …ride an escalator not holding the rail | 0.94 | 194 (43.3) | 62 13.8) | 58 (12.9) | 72 (16.1) | 62 (13.8) |
| 5 | …reach while standing on your tiptoes* | 0.40 | 142 (31.7) | 55 (12.3) | 71 (15.8) | 93 (20.8) | 87 (19.4) |
| 13 | …walk in a crowd or get bumped** | 0.02 | 83 (18.5) | 76 (17.0) | 80 (17.9) | 123 (27.5) | 86 (19.2) |
| 14 | …ride an escalator holding the rail | −0.22 | 111 (24.8) | 43 (9.6) | 47 (10.5) | 98 (21.9) | 149 (33.3) |
| 11 | …walk up and down a ramp | −0.42 | 46 (10.3) | 71 (15.8) | 99 (22.1) | 135 (30.1) | 97 (21.7) |
| 12 | …walk in a crowed mall | −0.44 | 69 (15.4) | 58 (12.9) | 65 (14.5) | 124 (27.7) | 132 (29.5) |
| 7 | …sweep the floor | −0.66 | 73 (16.3) | 43 (9.6) | 56 (12.5) | 92 (20.5) | 184 (41.1) |
| 2 | …walk up and down stairs | −0.89 | 33 (7.4) | 51 (11.4) | 82 (18.3) | 148 (33.0) | 134 (29.9) |
| 10 | …walk across a parking lot | −1.11 | 41 (9.2) | 31 (6.9) | 61 (13.6) | 124 (27.7) | 191 (42.6) |
| 3 | …pick up a slipper from the floor | −1.24 | 30 (6.7) | 35 (7.8) | 66 (14.7) | 130 (29.0) | 187 (41.7) |
| 8 | …walk outside to a nearby car | −1.69 | 20 (4.5) | 19 (4.2) | 61 (13.6) | 117 (26.1) | 231 (51.6) |
| 1 | …walk around the house | −1.80 | 13 (2.9) | 18 (4.0) | 70 (15.6) | 145 (32.4) | 202 (45.1) |
| 9 | …get in and out of a car | −2.09 | 10 (2.2) | 16 (3.6) | 56 (12.5) | 127 (28.3) | 239 (53.3) |
| 4 | …reach at eye level | −2.15 | 12 (2.7) | 16 (3.6) | 32 (7.1) | 123 (27.5) | 265 (59.2) |
Items misfitting the Partial Credit Model are bolded.
to address misfit reword to “…stand on your tiptoes”
to address misfit reword to “…get bumped”
Despite positive psychometric evidence supporting the use of the ABC-scale, further evaluation of the scale’s measurement properties is necessary,19,28 and for several reasons this is especially true among individuals aging with a lower-limb amputation. First, the properties of the ABC-scale have only been established in a sample of individuals with a lower-limb amputation who were 20 years of age and older. It is therefore difficult to generalize the results to older individuals especially when given both theory16 and research evidence suggesting that older individuals tend to have lower levels of confidence than younger people. Next, in terms of item difficulty, it is unknown if the items on the ABC-scale are appropriate for use with individuals aging with a lower-limb amputation. It is also unknown how much of the balance confidence construct the ABC-scale actually assesses, and whether or not content gaps and/or redundant items exist. Further, the single internal consistency coefficient derived at the test level assumes each item is equally consistent and error free among individuals with a lower-limb amputation. This assumption, however, is not true because if scores are normally distributed, more people are in the middle range, and therefore item reliability (internal consistency) should be higher in the middle, and decrease with higher and lower scores. Thus, knowledge of the internal consistency reliability of each item would help to revise and improve the ABC-scale. Finally, the ABC-scale uses a 101-point response format. This is notable because evidence shows older adults having difficulties using response formats with many options.24,29 An inability to differentiate between adjacent response options leads to respondent bias arising from an increase in subjectivity.30
Given the current knowledge of the ABC-scale and some of the unanswered questions concerning its applicability among aging individuals with a lower-limb amputation living in the community, the objectives of this study were to: 1) explore shortened response formats for use with the ABC-scale; 2) evaluate the unidimensionality of the scale; 3) evaluate the item difficulty; 4) evaluate the scale for redundancy and content gaps; and 5) evaluate the item standard error of measurement (SEM) and internal consistency reliability.
METHODS
Participants
Cross-sectional survey and chart review data were combined from 3 separate studies of individuals with a lower-limb amputation. The samples from each of the 3 studies were drawn from 2 university-affiliated outpatient amputee clinics in Ontario, Canada, between 1998 and 2001.10,21,31 These clinics provide regular follow-up to patients by the amputee rehabilitation team. Individuals were included in the studies if they were at least 19 years old, had a major unilateral amputation, used their prosthesis on a daily basis for at least 6 months, and lived in the community. Individuals were excluded if they had hip disarticulation or hemipelvictomy, could not speak or write English, or if they could not follow verbal commands. Research Ethics Board for Health Sciences Research Involving Human Subjects at the University of Western Ontario reviewed and approved each of the three studies. For purposes of this study, only data from individuals at least 50 years of age were included for analyses. Descriptive information of the sample used in this study is outlined in table 1. More detailed descriptive information of the samples from each of the 3 studies is reported elsewhere.10,21,31
Table 1.
Sample Characteristics (n = 448)
| Characteristic | Value |
|---|---|
| Age (years) | 68.1 ± 10.3 |
| Sex (men) | 325 (72.5) |
| Cause of amputation: | |
| Vascular | 276 (61.6) |
| Trauma | 122 (27.2) |
| Cancer | 20 (4.5) |
| Other (congenital, pain, infection) | 30 (6.7) |
| Amputation level: | |
| Below knee | 299 (66.7) |
| Above knee | 112 (25.0) |
| Bilateral | 21 (4.7) |
| Other (symes, TK) | 16 (3.6) |
| Amputation side: | |
| Right | 224 (50.0) |
| Left | 203 (45.3) |
| Bilateral | 21 (4.7) |
| Years with amputation | 13.2 ± 17.1 |
| ABC-scale total raw score | 62.2 ± 26.5 |
Values are mean ± standard deviation or frequency (%)
Data Analyses
Modifying the Response Scale
Response options from the original 101-point format were grouped so that each revised response option was chosen by at least 10 participants,32 yet still retained enough options to express distinct differences in balance confidence.33 Four-, 5-, and 6- response formats were derived by keeping the anchors of 0% and 100% as 2 options, and then by evenly grouping the 1 though 99 percentages into the remaining 2, 3, and 4 options. Table 2 shows the groupings of the revised response formats for testing. Data from each of the revised response formats were then entered into both the Partial Credit and Rating Scale Rasch models,34,35 and the resulting fit statistics (weighted mean squares) were analyzed. Fit statistics provide information on how much the residuals vary relative to their expected variance as calculated by the model.36 Items with residual fit statistics less than 0.75 or greater than 1.33 and with t-statistics less than −2.0 or greater than 2.0 were considered poor fitting items.36 Rasch Category Probability Curves (CPC) were also examined to determine the optimal number of responses individuals were able to differentiate between. Each CPC corresponds to a response option and shows the probability of selecting that response option at differing levels of balance confidence. The ideal number of response categories that individuals are able to differentiate between, thus, is the one with each CPC having the highest probability of being selected at differing levels of balance confidence.
Table 2.
Revised Response Formats Tested
| Response option | 0 | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|
| 4 responses | 0% | 1 to 49% | 50 to 99% | 100% | ||
| 5 responses | 0% | 1 to 33% | 34 to 66% | 67 to 99% | 100% | |
| 6 responses | 0% | 1 to 24% | 25 to 49% | 50 to 74% | 75 to 99% | 100% |
The response format with the fewest poor-fitting items and that retained the maximum number of response options individuals were able to differentiate between was deemed the most appropriate to use for further analyses.
Testing for Unidimensionality
Exploratory factor analysis and examination of the scree plot: Both were used to test the unidimensionality of the ABC-scale. Unidimensionality was confirmed if 1 factor explained at least 20% of the variance with item loadings greater than 0.30,33 and if the scree plot showed 1 dominant first factor. SPSS version 15 was used for these analyses.
Rasch Model Fit: The Partial Credit Model (PCM)34 and the Rating Scale Model (RSM)35 are Rasch models used with polytomous data (i.e. data derived from response formats with more than 2 options). The models differ only in their assumptions regarding the distance between response options. The PCM assumes that the distance between the response options is not the same for all items, whereas the RSM assumes the distance is the same. Rasch models were developed using the ConQuest software.37 The best model to use for further analyses was then determined by a likelihood ratio test and item-fit analyses (as discussed above). The likelihood ratio test compared the difference between the models’ deviance parameters.38 Deviance equals twice the log-likelihood and has a chi-square distribution with degrees of freedom equal to the difference in the number of parameters derived by the models.38 The model with significantly less deviance and the fewest poor fitting items was used for further analyses.
Item difficulty, Redundancy, and Content gaps
Item difficulty, redundancy, and content gaps in the ABC-scale were assessed with a Rasch item-person map. The item-person map locates both the items-by-threshold (i.e. the location where the probability of selecting a response option versus all previous options is 0.50) and respondents along a common interval-level continuum (in logits), that represents the construct of interest. Because the continuum has a mean of 0 and standard deviation of 1, ±3 standard deviations (or logits) from the mean represents 99.7% of the construct of interest. Zero logits represents moderate item difficulty and balance confidence. Movement in the positive or negative direction along the continuum indicates greater and lesser item difficulty or balance confidence.
Inspection of the map revealed the difficulty of the ABC-scale’s items relative to the distribution of the population’s confidence levels. Areas along the continuum between ±3 logits that lacked an item-by-threshold were identified as content gaps in the scale, and items that appeared similar in content with similar thresholds were identified as redundant items.
Standard Error of Measurement and Internal Consistency Reliability
Both the SEM and internal consistency reliability were estimated at each location along the confidence continuum between ±3 logits. In Rasch analyses, the SEM are based on different scales (logits) than those estimated in CTT (raw score), but the coefficients are similarly interpreted.36 The SEM derived via Rasch analyses may be converted into coefficients similar to Cronbach ∝ by using the formula, 1/1+SEM2.39 Cronbach ∝ estimates <0.70 are unacceptable and those >0.90 are desirable.40
RESULTS
In total, 448 subjects met the inclusion criteria and their data used for Rasch analyses.
Modifying the response scale
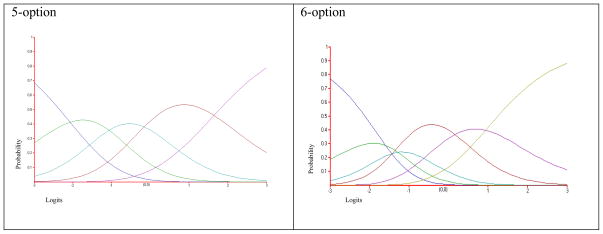
The 5-option response format resulted in the fewest misfitting items in both the PCM (3 misfits) and RSM (8 misfits). Five response options were also the maximum number of options that respondents were able to differentiate between, as shown by the CPCs in figure 1.
Figure 1.
Example of the Partial Credit Model Category Probability Curves for the 5-and 6- option response formats. In the 5-option figure, each curve rises above the other curves at some point along the logit continuum (i.e. x-axis), indicating that each response option at some point along the continuum has the highest probability of being chosen. In the 6-option response format, one of the curves remains below the other curves, indicating that this option is likely to be never selected.
Testing for unidimensionality
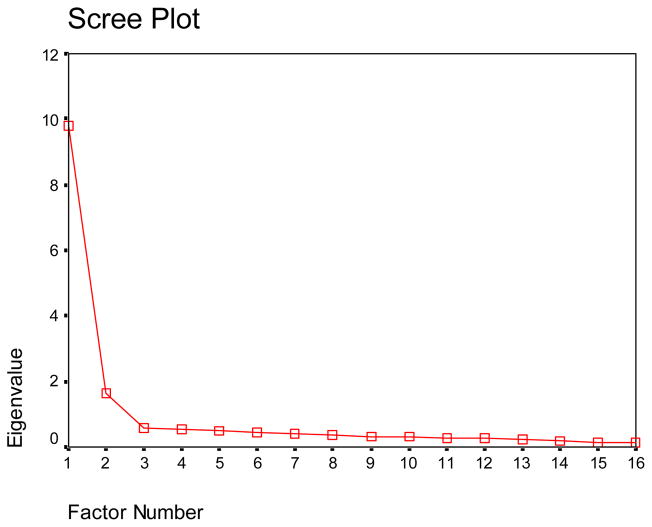
Exploratory factor analysis revealed 1 dominant factor in the ABC-scale with the 5-option response format. All item loadings were above 0.30, and the 1 factor explained 59% of the total variance. The scree plot also confirmed 1 dominant factor, as shown in figure 2.
Figure 2.
The scree plot identifies one dominant first factor with an eigenvalue of 9.8.
The PCM’s deviance was found to be smaller than the RSM’s deviance, and the differential of 278.14 was statistically significant (df = 45; α = 0.05). Further, 3 of the 16 items and all 5 of the item-by-response options misfit the RSM, whereas 2 of the 16 items and 1 of the 80 item-by-response options misfit the PCM. The data therefore fit the PCM significantly better than the RSM. Table 3 shows the deviance and weighted fit statistics for both the PCM and RSM.
Table 3.
Deviance and Weighted Fit Statistics by Model
| Rating Scale Model | Partial Credit Model | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deviance (df) = 15483.56 (20) | Deviance (df) = 15205.42 (65) | |||||||||||
| Infit Statistics | Infit Statistics | |||||||||||
| Item # | Item | Item by response option | Item | Item by response option | ||||||||
| Mnsq (t) | 0 Mnsq (t) | 1 Mnsq (t) | 2 Mnsq (t) | 3 Mnsq (t) | 4 Mnsq (t) | Mnsq (t) | 0 Mnsq (t) | 1 Mnsq (t) | 2 Mnsq (t) | 3 Mnsq (t) | 4 Mnsq (t) | |
| 1 | 0.82 (−2.4) | 2.75 (14.3) | 2.56 (13.7) | 1.93 (10.2) | 3.24 (20.9) | 3.04 (18.3) | 0.91 (−1.2) | 1.04 (0.2) | 0.97 (−0.1) | 0.93 (−1.0) | 0.95 (−1.4) | 0.96 (−0.7) |
| 2 | 0.99 (−0.2) | 1.07 (0.9) | 1.06 (0.5) | 0.96 (−0.4) | 0.96 (−0.6) | 0.98 (−0.5) | 1.11 (1.6) | |||||
| 3 | 0.92 (−1.1) | 0.95 (−0.6) | 0.90 (−0.6) | 0.98 (−0.1) | 1.00 (0.1) | 0.92 (−1.9) | 0.85 (−2.6) | |||||
| 4 | 1.25 (2.6) | 1.32 (3.3) | 1.09 (0.4) | 1.15 (0.8) | 0.98 (−0.1) | 0.97 (−0.6) | 0.93 (−1.2) | |||||
| 5 | 1.42 (5.3) | 1.40 (5.0) | 1.38 (4.8) | 0.98 (−0.2) | 1.03 (0.4) | 1.06 (1.0) | 0.91 (−1.0) | |||||
| 6 | 1.36 (4.4) | 1.33 (4.0) | 1.23 (3.2) | 1.02 (0.2) | 1.00 (0.1) | 1.01 (0.1) | 1.02 (0.2) | |||||
| 7 | 1.24 (3.1) | 1.14 (1.8) | 1.24 (2.4) | 0.99 (−0.1) | 0.98 (−0.2) | 0.93 (−1.3) | 0.80 (−3.3) | |||||
| 8 | 0.78 (−2.9) | 0.78 (−3.0) | 1.07 (0.4) | 0.98 (−0.1) | 0.86 (−1.8) | 0.92 (−1.7) | 0.85 (−2.8) | |||||
| 9 | 0.92 (−0.9) | 0.99 (−0.1) | 0.98 (0.0) | 1.01 (0.1) | 0.92 (−0.9) | 0.96 (−0.9) | 1.02 (0.3) | |||||
| 10 | 0.79 (−3.0) | 0.75 (−3.6) | 0.85 (−1.2) | 0.98 (−0.1) | 0.88 (−1.4) | 0.91 (−2.1) | 0.85 (−2.7) | |||||
| 11 | 0.97 (−0.5) | 1.07 (1.0) | 1.00 (0.0) | 0.97 (−0.4) | 0.99 (−0.1) | 0.93 (−1.7) | 0.99 (−0.1) | |||||
| 12 | 0.76 (−3.7) | 0.77 (−3.5) | 0.87 (−1.5) | 0.93 (−0.9) | 0.93 (−0.8) | 0.89 (−2.6) | 0.86 (−2.1) | |||||
| 13 | 0.61 (−6.5) | 0.68 (−5.2) | 0.92 (−1.0) | 0.90 (−1.5) | 0.91 (−1.2) | 0.81 (−4.6) | 0.85 (−1.9) | |||||
| 14 | 1.33 (4.4) | 1.19 (2.4) | 1.32 (3.6) | 0.98 (−0.1) | 1.01 (0.1) | 0.97 (−0.5) | 0.84 (−2.5) | |||||
| 15 | 1.31 (4.0) | 1.28 (3.4) | 1.16 (2.3) | 1.00 (0.1) | 1.02 (0.3) | 0.97 (−0.4) | 1.15 (1.5) | |||||
| 16 | 1.12 (1.5) | 1.21 (2.8) | 1.05 (0.8) | 1.00 (0.0) | 0.97 (−0.6) | 1.08 (0.9) | 1.27 (1.3) | |||||
Misfitting items bolded. Misfit = Mnsq <0.75 or >1.33 and t-statistic < −2 or >2.
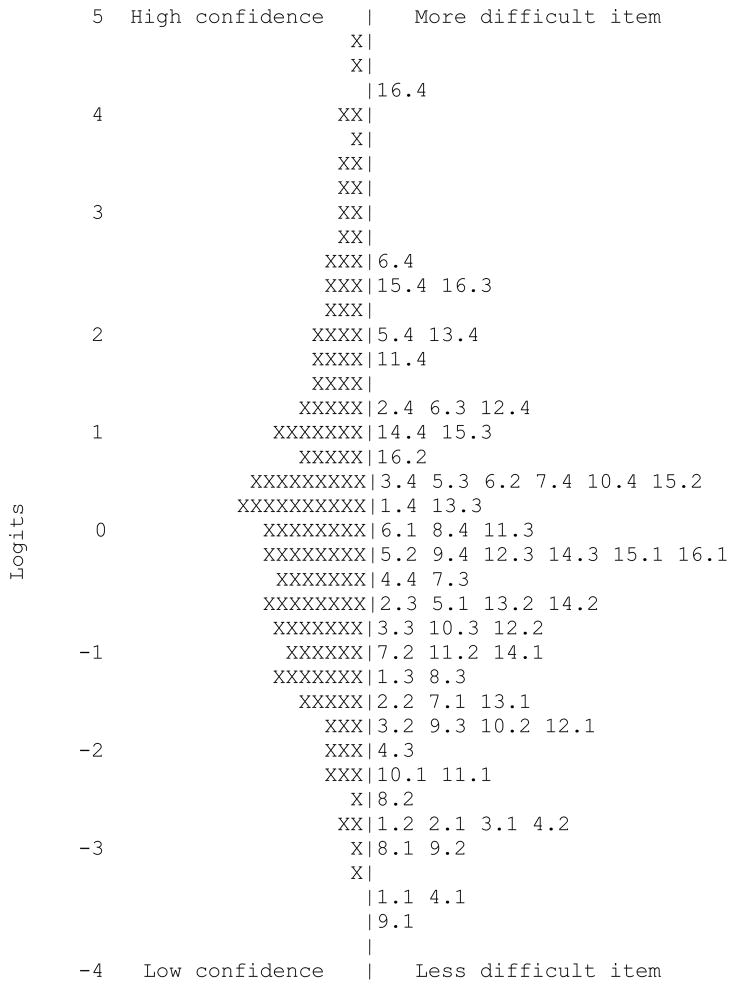
Item difficulty, Redundancy, and Content gaps
The item-person map revealed that the distribution of respondents’ balance confidence levels ranged from −3.3 to 4.8 logits, with most respondents having confidence levels ranging between ±3 logits. Of the 448 subjects in the study, 28 respondents (6%) were above +3 logits, and 3 respondents (0.7%) were below −3 logits. Overall, most respondents reported moderate to moderately low balance confidence levels (i.e. 0.5 to −2 logits) as shown in figure 3.
Figure 3.
The item-person map displaying the balance confidence continuum from −4 to 5 logits on which both the difficulty of items and respondent confidence levels are located. Plus/minus 3 logits represents 99.7% of the construct. Each X represents 3.1 subjects, and ##.# represents each item-by-threshold.
Because the 5-option response format was deemed the most appropriate for use with the ABC-scale, 4 thresholds exist. All the item-by-thresholds ranged from −3.7 to 4.1 logits along the confidence continuum. Although a small content gap in the ABC-scale exists between 2.6 to 3.0 logits, the item-by-thresholds provide good coverage for all other levels of balance confidence between ±3 logits, with the most coverage in the moderate to moderately low balance confidence range, which is also shown in figure 3.
Table 4 shows the average difficulty of the ABC-scale items in logits, and the frequency of responses for each of the 5 options. The item requiring the most balance confidence on average was item 16, walking on an icy sidewalk, and the item requiring the least balance confidence was item 4, reaching at eye level. No items had identical difficulty levels, indicative that none of the items on the ABC-scale are completely redundant, and that each item assesses at least partially a different level of balance confidence.
Standard Error of Measurement and Internal Consistency Reliability
The SEM for the ABC-scale was lowest (0.27) at −0.51 logits and increased to 0.40 and 0.29 with higher and lower confidence levels. In converting the SEM into Cronbach ∝ estimates, internal consistency reliability peaked at 0.94, and decreased to 0.75 and 0.86 at +3 and −3 logits respectively
DISCUSSION
The purpose of this study was to evaluate the construct validity, internal structure, and SEM and internal consistency reliability of shortened response formats for use with the ABC-scale among community living, aging individuals (≥50 years) with a lower-limb amputation.
In terms of response formats, Embretson and Reise30 note that self-report measures should avoid using formats with many options as there is an increase in respondent bias arising from subjectivity due to an inability to differentiate between the multiple response options. Streiner and Norman33 further suggest that the number of response options used with self-report measures should not be more than a person is able to differentiate. They recommend the use of 5 to 9 response options, and advise that the optimal number of options will likely differ depending upon the ability of the population.33
Our analyses revealed a 5-option response format as the most appropriate to use with the ABC-scale. This finding is consistent with the results from another study24 that used a statistical approach to reduce the number of response options. Adjacent options having low frequency of responses were collapsed until the best solution was found. In our study, response options were grouped together based on their similarity, which may be a more clinically appropriate method. Despite differences in modifying the response formats, evidence is accumulating in support of an ABC-scale with a 5-option response format. As a result of our modifications to the response scale, each of the 5 options may be labelled as 0 = ‘no confidence’, 1 = ‘low confidence’, 2 = ‘moderate confidence’, 3 = ‘high confidence’, and 4 = ‘complete confidence’. Such a format may result in improved efficiency of the measure and reduced respondent bias, however, future prospective studies are needed to test the 5-option response format if labelled response options are used.
Exploratory factor analysis revealed an ABC-scale with a unidimensional structure that was then evaluated with two Rasch models. Because the data fit the PCM significantly better than the RSM, the balance confidence needed to transition between each of the 5 response options is not the same for all items. Such a finding is important for the accurate interpretation of total scores into balance confidence levels, as differences exist in the contribution of each items’ response options to balance confidence levels. That is, changes in scores by like amounts have different balance confidence implications for each item. In their analysis, Arnadotirr et al.24 a priori used the RSM thereby perhaps incorrectly assuming that the distance between response options is the same for all items.
Two items were found to misfit the PCM. Item 5, reaching while standing on your tiptoes, had a fit statistic of 1.40, indicating that the item’s variance was higher than expected, and item 13, walking in a crowd or getting bumped, had a fit statistic of 0.68, indicating that the item’s variance was lower than expected. These findings suggest that item 5 should either be removed completely or reworded to improve its fit to the model and the scale’s unidimensionality. Given that it is a double-barrelled question, rewording the item to inquire about balance confidence while only standing on tiptoes or only reaching upwards would be the first step to address the misfit. Rewording item 13 to only inquire about being bumped may similarly resolve its misfit issue especially given that item 12 similarly inquires about walking in crowded places.
Through the use of Rasch modelling, the item and respondent characteristics may be estimated independent of each other.33,38,41 This property of sample invariance allows for the measurement of people to be made independently of the items used, and the characteristics of the items to be evaluated independent of the respondents.42 As a result, one can evaluate the scale’s content representation relative to both the respondentsand the confidence continuum. We found the ABC-scale with a 5-option response format not only has more content representation at the moderate to moderately low levels along the confidence continuum, but also assesses these levels with the highest internal consistency and least error. Because aging individuals with a lower limb amputation on average also have moderate to moderately low balance confidence levels, the ABC-scale is a reliable measure to use with this population. Further, the only levels along the balance confidence continuum that lacked content coverage between ±3 logits was from 2.6 to 3.0 logits. The first step to address this lack of coverage would be to reword the misfitting items noted above. It’s possible a new item may be developed to fit this gap, although it is a relatively small gap in a scale that otherwise exhibits a satisfactory range of content specific to balance confidence.
Study Limitations
Despite the findings in support of the measurement properties of an ABC-scale with a 5-option response format, this study has limitations, including, the methods used assess the structural properties of the scale provide only one form of construct validity, and the generalizability of the findings is restricted to community dwelling individuals aging with a lower-limb amputation. Another limitation to the study is that the cognitive functioning of the subjects was not assessed. Aging influences cognitive functioning, which in turn may have biased the results especially between those individuals 50 to 65 years of age and those older than 65 years. Further, because the data were not stratified by age or time using a prosthesis we do not know how group differences influenced the findings.
CONCLUSION
The findings in this study support the internal consistency reliability and validity of the ABC-scale with a 5-option response format, and identify ways to improve the scale for use with aging individuals with a lower-limb amputation living in the community. The scale was found to be most reliable for use with individuals with moderate to moderately low balance confidence levels. Items measuring higher levels of confidence would benefit the scale by lowering the associated measurement error, thus, rewording the misfitting items is the first step to improve the scale. A key finding of this study was the number of response options that older individuals are able to differentiate. Although evidence is mounting in support of using a simplified response format, prospective studies are warranted to evaluate the properties of the ABC-scale using a response format with 5 options among similar and different patient populations. However, given the results of this study, the preferred version of the ABC-scale is one with a 5-option response format for use with community living, aging individuals with a lower limb amputation who would benefit from a falls prevention programs. Given the simplified response format, the scale may assess balance confidence outcomes without a considerable increase in respondent burden.
Acknowledgments
Financial support: Salary support/scholarship was provided by the Canadian Institutes of Health Research to WCM and BMS (CIHR #72159).
List of Abbreviations
- ABC-scale
Activities-specific Balance Confidence Scale
- SEM
Standard error of measurement
- PCM
Partial Credit Model
- RSM
Rating Scale Model
- CPC
Category Probability Curves
Footnotes
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (eg, NIH or NHS grants) and work are clearly identified in the title page of the manuscript.
The manuscript submitted does not contain information about medical device(s).
Reprints are not available from the authors
References
- 1.Miller WC, Speechley M, Deathe B. The prevalence and risk factors of falling and fear of falling among lower extremity amputee. Arch Phys Med Rehabil. 2001;82:1031–1037. doi: 10.1053/apmr.2001.24295. [DOI] [PubMed] [Google Scholar]
- 2.Health Canada. Seniors and aging – preventing falls in and around your home. Ottawa: 2006. Catalogue no. H13-7/10-2006E-PDF. [Google Scholar]
- 3.Schiller J, Kramarow E, Dey A. Centers for Disease Control and Prevention, Advance Data From Vital and Health Statistics 2007. Vol. 392. Hyattsville, MD: National Center for Health Statistics; 2007. Fall injury episodes among noninstitutionalized older adults: United States, 2001–2003. [PubMed] [Google Scholar]
- 4.Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: A systematic review and meta-analysis. Epidemiology. 2010;21:658–668. doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]
- 5.Painter JA, Elliott SJ, Hudson S. Falls in community-dwelling adults aged 50 years and older. J Allied Health. 2009;38:201–207. [PubMed] [Google Scholar]
- 6.Canadian Institute for Health Information. National trauma registry 2004 report: Injury hospitalizations (includes 2002–2003 data) Ottawa: 2004. [Google Scholar]
- 7.Statistics Canada. Mortality, Summary of causes. Ottawa: 2005. Catalogue no. 84F0209X. [Google Scholar]
- 8.Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist. 2002;42:17–23. doi: 10.1093/geront/42.1.17. [DOI] [PubMed] [Google Scholar]
- 9.Cumming RG, Salkeld G, Thomas M, et al. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A Biol Sci Med Sci. 2000;55A:M299–M305. doi: 10.1093/gerona/55.5.m299. [DOI] [PubMed] [Google Scholar]
- 10.Miller WC, Speechley M, Deathe AB, Koval J. The influence of falling, fear of falling and balance confidence on prosthetic mobility and social activity among individuals with a lower extremity amputation. Arch Phys Med Rehabil. 2001;82:1238–44. doi: 10.1053/apmr.2001.25079. [DOI] [PubMed] [Google Scholar]
- 11.Powell LE, Myers A. The Activities-specific Balance Confidence (ABC) scale. Journal of Gerontology. 1995;50A:M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 12.Miller WC, Speechley M, Deathe B. Balance confidence among people with lower-limb amputations. Physical Therapy. 2002;82(9):856–865. [PubMed] [Google Scholar]
- 13.Miller WC, Deathe AB. A prospective study examining balance confidence among individuals with lower limb amputation. Disability and Rehabilitation. 2004;26:875–881. doi: 10.1080/09638280410001708887. [DOI] [PubMed] [Google Scholar]
- 14.Anaby D, Miller WC, Eng JJ, Jarus T, Noreau L and the PACC Research Group. Can personal and environmental factors explain participation of older adults? Disability & Rehabilitation. 2009:1–8. doi: 10.1080/09638280802572940. [DOI] [PubMed] [Google Scholar]
- 15.Pang YC, Eng JJ, Miller WC. Determinants of satisfaction with community reintegration in older adults with chronic stroke: Role of balance self efficacy. Physical Therapy. 2007;87:282–291. doi: 10.2522/ptj.20060142. [DOI] [PubMed] [Google Scholar]
- 16.Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- 17.Simpson JM, Worsfold C, Hawke J. Balance confidence in elderly people: The CONFbal scale. Age Ageing. 1998;27(Suppl 2):57. [Google Scholar]
- 18.Shumway-Cook A, Gruber W, Baldwin M, Liao S. The effect of multidimensional exercises on balance, mobility, and fall risk in community-dwelling older adults. Physical Therapy. 1997;77:46–57. doi: 10.1093/ptj/77.1.46. [DOI] [PubMed] [Google Scholar]
- 19.Moore DS, Ellis R. Measurement of fall-related psychological constructs among independent-living older adults: A review of the research literature. Aging & Mental Health. 2008;12(6):684–699. doi: 10.1080/13607860802148855. [DOI] [PubMed] [Google Scholar]
- 20.Huang T-T, Wang W-S. Comparison of three established measures of fear of falling in community dwelling older adults: Psychometric testing. Int J Nurs Stud. 2009;46(10):1313–1319. doi: 10.1016/j.ijnurstu.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 21.Miller WC, Deathe AB, Speechley M. Psychometric properties of the Activities-specific Balance Confidence Scale among individuals with a lower-limb amputation. Arch Phys Med Rehabil. 2003;84(5):656–661. doi: 10.1016/s0003-9993(02)04807-4. [DOI] [PubMed] [Google Scholar]
- 22.Salbach NM, Mayo NE, Hanley JA, Richards CL, Wood-Dauphinee S. Psychometric evaluation of the original and Canadian French version of the Activities-specific Balance Confidence Scale among people with stroke. Arch Phys Med Rehabil. 2006;87:1597–1604. doi: 10.1016/j.apmr.2006.08.336. [DOI] [PubMed] [Google Scholar]
- 23.Peretz C, Herman T, Hausdorff JM, Giladi N. Assessing fear of falling: Can a short version of the Activities-specific Balance Confidence Scale be useful? Movement Disorders. 2006;21:2101–2105. doi: 10.1002/mds.21113. [DOI] [PubMed] [Google Scholar]
- 24.Arnadottir SA, Lundin-Olsson L, Gunnarsdottir ED, Fisher AG. Application of Rasch analysis to examine the psychometric aspects of the Activities-Specific Balance Confidence Scale when used in a new cultural context. Arch Phys Med Rehabil. 2010;91:156–163. doi: 10.1016/j.apmr.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 25.Filiatrault J, Gauvin L, Fournier M, Parisien M, Robitaille Y, Laforest S, Corriveau H, Richard L. Evidence of the psychometric qualities of a simplified version of the Activities-specific Balance Confidence Scale for community dwelling seniors. Arch Phys Med Rehabil. 2007;88:664–672. doi: 10.1016/j.apmr.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 26.Parry SE, Steen N, Galloway SR, Kenny RA, Bond J. Falls and confidence related to quality of life outcome measures in an older British cohort. Postgraduate Medical Journal. 2001;77:103–108. doi: 10.1136/pmj.77.904.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hsu PC, Miller WC. Reliability of the Chinese version of the Activities-specific Balance Confidence Scale. Disability and Rehabilitation. 2006;28:1287–1292. doi: 10.1080/09638280600638414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jorstad EC, Haueer K, Becker C, Lamb SE the ProFaNE Group. Measuring the psychological outcomes of falling: A systematic review. J Am Geriatr Soc. 2005;53:501–510. doi: 10.1111/j.1532-5415.2005.53172.x. [DOI] [PubMed] [Google Scholar]
- 29.Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction: the Survey of Activities and Fear of Falling in the Elderly (SAFE) J Gerontol B Psychol Sci Soc Sci. 1998;53:P43–50. doi: 10.1093/geronb/53b.1.p43. [DOI] [PubMed] [Google Scholar]
- 30.Embretson SE, Reise SP. Item Response Theory for Psychologists. 2. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2000. [Google Scholar]
- 31.Deathe AB, Miller WC. The L Test of Functional Mobility: Measurement properties of a modified version of the Timed “Up & Go” test designed for people with lower-limb amputations. Physical Therapy. 2005;85(7):626–635. [PubMed] [Google Scholar]
- 32.Linacre JM. Optimizing rating scale category effectiveness. J Appl Meas. 2002;3:85–106. [PubMed] [Google Scholar]
- 33.Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to Their Development and Use. 4. Oxford: Oxford University Press; 2008. [Google Scholar]
- 34.Masters GN. A Rasch model for partial credit scoring. Psychometrika. 1992;47:149–174. [Google Scholar]
- 35.Andrich D. A rating formulation for ordered response categories. Psychometrika. 1978;43:561–573. [Google Scholar]
- 36.Wilson M, Allen DD, Corser Li J. Improving measurement in health education and health behavior research using item response modeling: introducing item response modeling. Health Education Research. 2006;21(S1):i4–i18. doi: 10.1093/her/cyl108. [DOI] [PubMed] [Google Scholar]
- 37.Wu ML, Adams RJ, Wilson MR. Acer Conquest: Generalized Item Response Modeling Software. Melbourne, Australia: ACER; 1998. [Google Scholar]
- 38.Wilson M, Allen DD, Corser Li J. Improving measurement in health education and health behavior research using items response modeling: comparison with the classical test theory approach. Health Education Research. 2006;21(S1):i19–i32. doi: 10.1093/her/cyl053. [DOI] [PubMed] [Google Scholar]
- 39.Masse LC, Heesch KC, Eason KE, Wilson M. Evaluating the properties of a stage-specific self-efficacy scale for physical activity using classical test theory, confirmatory factor analysis and item response modeling. Health Education Research. 2006;21(S1):i33–i46. doi: 10.1093/her/cyl106. [DOI] [PubMed] [Google Scholar]
- 40.Nunally JC, Bernstein IH. Psychometric Theory. 3. New York, NY: McGraw-Hill; 1994. [Google Scholar]
- 41.de Ayala RJ. The theory and practice of item response theory. New York, NY: The Guildford Press; 2009. [Google Scholar]
- 42.Hobart J, Cano S. Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods. Health Technology Assessment. 2009;13(12):1–200. doi: 10.3310/hta13120. [DOI] [PubMed] [Google Scholar]