Abstract
Introduction
Limited provider participation in the Medicaid program is a barrier to access to orthodontic care for Medicaid-eligible patients. The goals of this study were to determine the participation level of North Carolina (NC) orthodontists in the Medicaid program, to examine NC orthodontists’ perceptions of the Medicaid program and its beneficiaries, and to determine whether there are differences between practitioners who do and do not accept Medicaid patients.
Methods
Questionnaires were mailed to all active orthodontists (n = 203) as reported in the NC State Dental Board of Licensing Section of the NC Health Professions Data System. Respondents were categorized as current Medicaid providers, past Medicaid providers, or orthodontists who have never accepted Medicaid.
Results
Forty of 166 respondents were current Medicaid providers, 33 were past providers, and 93 never accepted Medicaid patients. All 3 groups thought that low fee reimbursement is a major problem. Those who have never participated in the Medicaid program were more likely to perceive each barrier as a major problem. Past Medicaid providers saw broken appointments and tardiness to appointments as greater problems than current providers.
Conclusions
Perceptions of Medicaid patients and lack of knowledge appear to be major barriers to provider participation.
In 1965, Medicaid was created as Title XIX of the Social Security Act to provide public health insurance to certain low-income people.1 In 1966, an American Dental Association task force specifically recommended that treatment services should include “treatment of malocclusion with priority provided for interceptive service and disfiguring or handicapping malocclusions.”2 An amendment passed in 1967 established the Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) program, mandating that dental care, including orthodontic treatment for handicapping malocclusion, be made available to Medicaid-eligible children less than 21 years of age.3–5 A significant obstacle in achieving the legislative mandate of the EPSDT program has been limited participation by dentists.
Low participation by dentists in the Medicaid program has been linked to low reimbursement rates, excessive paperwork, need for prior authorization, denial of payment, restrictions in reimbursable services, payment delays, and broken appointments.4–10 Capilouto7 presented other possible dimensions for low provider participation related to peer and professional considerations— eg, the linkage of Medicaid providers with fraud and abuse in the media and the perception that Medicaid providers are held in lower esteem by peers.
In 2002 and 2003, an estimated 480,000 children in North Carolina (NC) were eligible for dental treatment under the Medicaid program. During the same time period, less than 0.5% of these children received orthodontic care (NC DHHS 2004, unpublished data), even though it has been estimated that 29% of adolescents and 14.2% of children have severe to very severe handicapping malocclusions.11,12 The low percentage of Medicaid-eligible children who received orthodontic care in NC in 2003 appears to reflect the level of care in other states.13 In Washington13 and NC (NC DHHS 2003), only a few orthodontists (10 in each state) provided greater than 80% of the orthodontic treatment under the Medicaid program statewide, emphasizing the poor distribution of these patients among practitioners.
The survey of orthodontists in Washington by King et al13 is the only published study that examined orthodontists’ participation in, and attitudes toward, the Medicaid program. The objective of our investigation was to examine NC orthodontists’ perceptions of issues related to Medicaid. Specifically, the goals of this study were to determine the level of participation of NC orthodontists in the Medicaid program. to examine NC orthodontists’ perceptions of and attitudes toward the Medicaid program and its beneficiaries, and to determine whether there are differences between NC practitioners who do and do not accept Medicaid patients. A greater understanding of the barriers to orthodontists’ participation will provide insight into what changes, whether in program policy or in orthodontists’ attitudes, might be needed to improve access to orthodontic care for those who meet Medicaid criteria.
MATERIAL AND METHODS
A cross-sectional census study design was used to assess the level of participation of NC orthodontists in the Medicaid program and their perceptions of the Medicaid system and its clients. The survey instrument, approved by the Institutional Review Board at the University of North Carolina School of Dentistry, consisted of 28 items with Likert-scale responses for most questions.
The survey questions were derived from previously developed and tested instruments,4,13 altered to meet our research aims. The questionnaire was pretested on full-time orthodontic faculty at the University of North Carolina; they were asked to provide open-ended comments about ease of completion, confusing items, and word changes. These persons were excluded from the final study sample.
The survey instrument was divided into 4 domains: patient population, practitioner demographics, practice characteristics, and Medicaid issues. Practice arrangement was categorized as solo practitioner or nonsolo practitioner for analytical purposes. Respondents were asked whether they currently accepted new Medicaid patients and, if yes, what percentage of the active patient population was Medicaid; whether all new Medicaid patients were accepted; and whether the amount of Medicaid revenue resulted in a net profit, breaking even, or a net loss. Respondents who did not currently accept new Medicaid patients were asked whether they had ever accepted Medicaid patients and, if so, in what year they stopped accepting Medicaid patients. Finally, 10 commonly cited problems with the Medicaid program and its patients that were identified as barriers to participation were given. The respondents were then asked to rate each issue as “not a problem,” “a minor problem,” “a major problem,” or “don’t know.”
The survey was mailed to all active orthodontists practicing in NC as reported in the North Carolina State Dental Board of Licensing Section of the North Carolina Health Professions Data System. The sampling frame consisted of 215 orthodontists. Twelve of them were ineligible: 1 was deceased, and 11 were not active practitioners. Thus, the effective sampling frame was 203. The survey methods outlined by Salant and Dillman14 were used as a guide. A cover letter describing the study, the questionnaire, and a postage-paid return envelope was sent to each orthodontist. A follow- up letter, with a replacement questionnaire, was mailed about 2 to 3 weeks later to those who had not responded. A third letter, with another copy of the questionnaire, was sent to nonrespondents 2 to 3 weeks after the second letter. Data were collected between August and November 2005.
Respondents were categorized as current Medicaid providers, providers who had participated in Medicaid at 1 time but did not currently participate, and providers who had never participated in Medicaid. The responses of these 3 groups to all items were compared by using the exact Mantel-Haenszel chi-square test except for questions with continuous responses—eg, percentage of patients with insurance. For these items, the Mantel- Haenszel row-mean score statistic was used to compare the 3 groups. Respondents who specified “don’t know” to the barrier to participation items were excluded to yield a comparison of providers in the 3 groups who expressed an opinion. The number of respondents differed from question to question because some did not answer every question. The level of significance was set at .05 for all analyses.
RESULTS
One hundred sixty-eight eligible orthodontists responded to the survey. Two responded with letters and were excluded from the data analysis, yielding an effective response rate of 166 of 203 (82%). Most respondents were male, white, solo practitioners who had been in practice for an average of 19.5 years.
Only 40 practitioners (24.1%) reported currently accepting new Medicaid patients, and over 80% of these did not accept all new Medicaid patients seeking treatment. New Medicaid patients were more likely to be accepted if referred. Sixteen providers (40%) would accept medically compromised new Medicaid patients. The median percentage of the active patient population covered by Medicaid in these 40 practices was 6%. Only 6 practitioners reported that Medicaid patients made up more than 20% of their practice. Five (12.5%) reported a net profit from these patients. Fifteen (37.5%) reported breaking even, and 20 (50.0%) reported a net loss. Medicaid providers were located in 25 of the 100 counties in NC (Fig). Based on population density and median family income for each county, there was no apparent trend that Medicaid providers were located in counties with lower population densities or lower median family incomes.15
Fig.
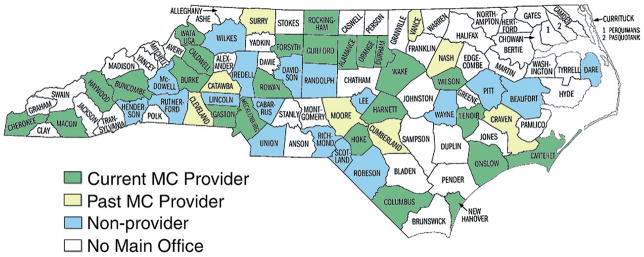
County affiliations for respondents. “No Main Office” indicates counties lacking an orthodontist with a main office, as reported by North Carolina Health Professions Data System.
One hundred twenty-six (75.9%) of the 166 respondents did not currently accept new Medicaid patients. Thirty-three (26.2%) of the nonparticipating orthodontists reported accepting Medicaid in the past but not currently; approximately half of them stopped accepting Medicaid patients in the last 6 years (2000 or later). The county affiliation of respondents who previously accepted Medicaid patients is shown in the Figure. Ninety-three of the 126 nonparticipating orthodontists (73.8%) reported never having accepted Medicaid.
There was no statistically significant difference in provider demographics or non-Medicaid related practice characteristics among the 3 groups (Table I). Medicaid providers did have a significantly higher percentage of referred patients with Medicaid than both groups of nonproviders (P <.0001). Current Medicaid providers, along with those who used to accept Medicaid, also had more Medicaid inquiries in a typical month than nonproviders who have never accepted Medicaid (P = .001).
Table I.
Descriptive statistics for the percentage of patients in each practice who met specific criteria as reported by all practitioners and those in each provider category
| All providers
|
Medicaid providers
|
Accepted Medicaid at1 time
|
Never accepted Medicaid
|
P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | Median (q1-q3) | n | Median (q1-q3) | n | Median (q1-q3) | n | Median (q1-q3) | ||
| New full-treatment cases started in 2004 | 136 | 202 (150–300) | 34 | 212.5 (150–350) | 28 | 205 (150–300) | 74 | 202 (150–300) | .95 |
| Method of payment | |||||||||
| % private insurance | 160 | 50 (38.5–65) | 38 | 44 (30–62) | 33 | 55 (40–70) | 89 | 50 (40–65) | .13 |
| % Medicaid | 130 | 0 (0–5) | 38 | 6 (3–10) | 23 | 0 (0–2) | 69 | 0 (0–0) | — |
| % no insurance | 161 | 50 (30–60) | 38 | 45.5 (27–55) | 33 | 42 (30–59) | 90 | 50 (30–60) | .39 |
| % other funding | 81 | 0 (0–1) | 19 | 0 (0–2) | 12 | 0 (0–0) | 50 | 0 (0–2) | — |
| Percentage of referred patients that have Medicaid | 165 | 2.0 (0–5) | 40 | 10.0 (3.5–20) | 32 | 1.0 (0–5) | 93 | 0.0 (0–2) | <0001 |
| Percentage of new cases with no fee | 83 | 1.0 (1–2) | 20 | 1.0 (1–2) | 15 | 1.0 (0–2) | 48 | 1.0 (1–2) | .29 |
| Percentage of new cases with discounted fee | 102 | 3.0 (2–5) | 28 | 3.0 (2–10) | 22 | 2.0 (1–10) | 52 | 2.5 (1–5) | .61 |
| Number of Medicaid inquiries in typical month | 154 | 5 (2–10) | 37 | 10 (3–20) | 30 | 10 (3–20) | 87 | 4 (1–10) | .001 |
|
| |||||||||
| n (%) | n (%) | n (%) | n (%) | ||||||
|
| |||||||||
| Practice arrangement | |||||||||
| Solo | 121 (73.33) | 30 (75.00) | 25 (78.13) | 66 (70.97) | .60 | ||||
| Nonsolo | 44 (26.67) | 10 (25.00) | 7 (21.88) | 27 (29.03) | |||||
| Busyness | |||||||||
| Too busy | 21 (12.88) | 8 (20.51) | 3 (9.38) | 10 (10.87) | .60 | ||||
| Comfortable load | 98 (60.12) | 20 (51.28) | 20 (62.50) | 58 (63.04) | |||||
| Not busy enough | 44 (26.99) | 11 (28.21) | 9 (28.13) | 24 (26.09) | |||||
| Average fee | |||||||||
| $5000 or less | 101 (61.59) | 28 (70.00) | 22 (68.75) | 51 (55.43) | .09 | ||||
| >$5000 | 63 (38.41) | 12 (30.00) | 10 (31.25) | 41 (44.57) | |||||
| Quoted no fee or reduced fee? | |||||||||
| No | 56 (34.78) | 10 (25.64) | 10 (31.25) | 36 (40.00) | .12 | ||||
| Yes | 105 (65.22) | 29 (74.36) | 22 (68.75) | 54 (60.00) | |||||
q1-q3, Twenty-fifth and 75th percentiles for numbers of cases or percentages of cases who met each criteria.
Many nonproviders who have never accepted Medicaid responded with “don’t know” to questions regarding reasons that orthodontists limit the number of Medicaid patients they treat (Table II). Thus, for the items related to barriers to participation in Medicaid, these respondents were excluded from the analyses.
Table II.
Perceived problems with Medicaid
| C, current Medicaid provider; A, accepted Medicaid at 1 time; N, never accepted Medicaid | Don’t know* (n) | Not problem n (%) | Minor problem n (%) | Major problem n (%) | P value |
|---|---|---|---|---|---|
| Fee reimbursement too low (n = 164) | |||||
| C | 0 | 0 (0) | 8 (20.00) | 32 (80.00) | 1.0 |
| A | 0 | 0 (0) | 7 (21.21) | 26 (78.79) | |
| N | 14 | 3 (3.90) | 9 (11.69) | 65 (84.42) | |
| Difficulty collecting from Medicaid (n = 161) | |||||
| C | 0 | 14 (35.00) | 17 (42.50) | 9 (22.50) | .0003 |
| A | 3 | 7 (24.14) | 12 (41.38) | 10 (34.48) | |
| N | 57 | 2 (6.25) | 11 (34.38) | 19 (59.38) | |
| Loss of coverage during treatment (n = 59) | |||||
| C | 4 | 14 (40.00) | 14 (40.00) | 7 (20.00) | <.0001 |
| A | 4 | 11 (39.29) | 8 (28.57) | 9 (32.14) | |
| N | 51 | 3 (8.11) | 5 (13.51) | 29 (78.38) | |
| Need for prior authorization (n = 161) | |||||
| C | 0 | 10 (25.00) | 19 (47.50) | 11 (27.50) | .001 |
| A | 0 | 5 (15.15) | 11 (33.33) | 17 (51.52) | |
| N | 24 | 4 (6.25) | 24 (37.50) | 36 (56.25) | |
| Difficulty getting billing questions answered (n = 161) | |||||
| C | 2 | 9 (23.68) | 21 (55.26) | 8 (21.05) | <.0001 |
| A | 5 | 6 (21.43) | 12 (42.86) | 10 (35.71) | |
| N | 62 | 0 (0) | 7 (26.92) | 19 (73.08) | |
| Delays in receiving payment (n = 158) | |||||
| C | 1 | 10 (27.03) | 20 (54.05) | 7 (18.92) | .0001 |
| A | 5 | 7 (25.00) | 13 (46.43) | 8 (28.57) | |
| N | 62 | 1 (4.00) | 6 (24.00) | 18 (72.00) | |
| Unruly/uncooperative behavior (n = 160) | |||||
| C | 0 | 11 (28.95) | 17 (44.74) | 10 (26.32) | <.0001 |
| A | 1 | 4 (12.5) | 14 (43.75) | 14 (43.75) | |
| N | 34 | 2 (3.64) | 17 (30.91) | 36 (65.45) | |
| Patients fail to show for appointments (n = 161) | |||||
| C | 0 | 3 (7.69) | 19 (48.72) | 17 (43.59) | <.0001 |
| A | 1 | 0 (0) | 6 (18.75) | 26 (81.25) | |
| N | 21 | 2 (2.94) | 6 (8.82) | 60 (88.24) | |
| Patients often late (n = 161) | |||||
| C | 0 | 7 (17.95) | 20 (51.28) | 12 (30.77) | <.0001 |
| A | 1 | 1 (3.13) | 9 (28.13) | 22 (68.75) | |
| N | 23 | 1 (1.52) | 8 (12.12) | 57 (86.36) | |
| Patients cancel at last minute (n = 161) | |||||
| C | 0 | 8 (20.51) | 22 (56.41) | 9 (23.08) | <.0001 |
| A | 2 | 3 (9.68) | 14 (45.16) | 14 (45.16) | |
| N | 29 | 1 (1.67) | 11 (18.33) | 48 (80.00) | |
Respondents who did not answer question or responded “don’t know” were recoded to missing and not included in calculations.
All 3 groups perceived low fee reimbursement to be a major problem with the Medicaid program (Table II). This was the only issue where the opinions of the 3 groups did not differ significantly. For the remaining issues related to program logistics or patient behaviors (Table II), current Medicaid providers, in general, perceived the issues to be no problem or a minor problem, whereas nonproviders (past and never) tended to report the issues to be minor or major problems. Interestingly, those who never accepted Medicaid and expressed an opinion were more likely to perceive the issues as major problems.
Analyses were conducted to compare current Medicaid providers with those who used to accept Medicaid to see what might have caused the latter group to stop participating. These 2 groups did not differ in any demographic characteristic (P >.59). The only practice characteristic (Table I) that differed between the 2 groups was the average percentage of referred patients covered by Medicaid (P <.0001). The 2 groups did not differ in their opinions of the logistics of the Medicaid program (P >.06) but did differ in their perceptions of Medicaid patients. More past Medicaid providers perceived patient behaviors to be a problem than did current providers (Table II): broken appointments (P = .001), tardiness for appointments (P = .001), last-minute cancellations (P = .05), and uncooperative behavior (P = .07).
DISCUSSION
Level of practitioner participation
Only 61 NC orthodontists participated in the Medicaid program in fiscal year 2003 (NC DHHS 2004, unpublished data) and most of them treated only a few patients. In 2004, 5670 orthodontic cases were submitted for prior authorization, with 64.9% (n = 3680) approved. In 2005, 7924 cases (a 40% increase from the last year) were submitted, and 63.7% (n = 5044) were approved. With less than 25% of practicing orthodontists currently accepting new Medicaid patients, compounded by the low percentage of patients in their practices with Medicaid coverage (median, 6%), we confirmed that low levels of participation by orthodontists and small percentages of Medicaid patients in each practice prevent meeting the goals of the Early and Periodic Screening, Diagnosis, and Treatment program.
In an environment of increasing numbers of Medicaid- eligible patients, barriers to care prevent those of low socioeconomic status from accessing orthodontic treatment and realizing the psychosocial and oral health advantages from improved appearance and oral function. 16,17 Low levels of practitioner participation have also plagued the success of the Medicaid program in other fields of dentistry and medicine nationwide. Since the 1970s, physician participation in Medicaid programs has been declining nationally.18,19 Reasons for this decline include inadequate reimbursement, excessive paperwork/administrative burdens, payment delays, litigation concerns, and patient abuses of the program.19–21 The blame for low participation in dentistry has also been similar.4–10
Practitioner and practice characteristics
Practitioner and practice characteristics do not appear to influence whether an orthodontist in NC participates in the Medicaid program. This is unlike the findings from other areas of medicine and dentistry suggesting that age, number of years in practice, perceptions of how busy the practice is, practice arrangement, and average fees can affect a practitioner’s decision to accept Medicaid.4,5,10,22 The effect of practice location, shown to possibly influence Medicaid participation levels, was not evaluated in depth in this study.5,13,22 However, the Medicaid providers who responded to the survey were located in only 25 of the 100 counties in NC, with the northeastern part of the state having the least access to an orthodontist who accepts Medicaid (Fig). Interestingly, the county with the most current Medicaid providers has the highest population density and the second highest median family income of all NC counties. Thus, there is probably more to the decision to participate in the Medicaid program than practice location: either these practitioners are located where Medicaid-eligible people live, or Medicaid patients are being referred to orthodontists who are known to accept them.
Orthodontists in Washington who accepted Medicaid patients provided more discounted fees, received more inquiries from Medicaid patients, and were more likely to feel overworked.13 In NC, however, the 3 groups of providers did not differ significantly in the average percentages of patients for whom no fee or a discounted fee was quoted. A possible explanation is that nonproviders might be giving back to the community by quoting no fee or a discounted fee to a few Medicaid patients rather than dealing with the “hassle” of the Medicaid system.6 A few respondents who reported not accepting Medicaid payment, even those who reported never accepting Medicaid, did report that a small percentage of their patient population was on Medicaid. Those who previously accepted Medicaid might have Medicaid patients who were not yet finished with treatment, or the provider might not officially participate in the Medicaid program but accept a few referrals or medically compromised patients and offer a discounted fee or no fee.
Perceptions of the Medicaid program and patients
If practitioner and practice characteristics are not related to participation by NC orthodontists in the Medicaid program, what could influence an orthodontist’s decision to participate? All 3 groups believed that the low fee reimbursement was a major problem with the Medicaid program (Table II). This finding is congruent with previous studies.4–10,13,19,21 With reimbursement rates of only 55% to 65% of the customary fee, and coverage limited to severe “handicapping” malocclusions that would most likely require more resources, it is not surprising that this has an effect on orthodontists’ level of participation. Even so, low fee reimbursement and minimal opportunity for profiting financially did not appear to deter those who currently accept Medicaid from treating these patients. This supports the theory that factors affecting providers’ participation in the Medicaid program are more complex than dissatisfaction with low reimbursement fees.8,10,22,23
Most of the orthodontists who had never accepted Medicaid responded with “don’t know” to the questions related to the logistics of the Medicaid system (Table II). This lack of opinion might reflect lack of knowledge about actual procedures and implementation of Medicaid coverage. Margolis et al22 found that pediatricians who knew less about the Medicaid program tended to restrict patient access. Educating practitioners in the logistics of the Medicaid program could help to dispel some of these negative perceptions.
Substantially fewer (less than 40%) of those who had never accepted Medicaid responded with “don’t know” to the patient-related issues (Table II). Of those who gave an opinion, over 80% cited the issues related to disruption of practice efficiency (no show/cancellation/ tardiness) as major problems. Providers who stopped accepting Medicaid did not significantly differ from current providers in their perception of the problems related to the Medicaid program but did differ in their perception of the problem level associated with patient-related behaviors. Past providers thought that broken appointments (44% current vs 81% past) and tardiness (31% vs 69%) were major problems; this might have influenced their decision to discontinue accepting new Medicaid patients. Mirabelli et al24 reported that, although Medicaid patients had more broken appointments and poorer oral hygiene, compliance did not appear to affect the final treatment result. A more comprehensive study comparing Medicaid patients with non-Medicaid patients in terms of cooperation would be beneficial to verify whether commonly held perceptions of Medicaid patients are valid. Incorporating Medicaid patients into residency clinics to give residents hands-on experience with the logistics of the system might give them a more realistic view of the Medicaid program and its patients. Residency training programs can also foster a higher level of altruism and a sense of social responsibility through education about public health principles.
CONCLUSIONS
In this study, we examined participation and perceptions of the Medicaid program among practicing orthodontists in NC. Therefore, broad generalizations of the findings should be made with caution; however, under the conditions of this study, we conclude the following.
Approximately three-quarters of the orthodontists in NC reported that they do not currently accept or have never accepted Medicaid patients.
There appear to be no demographic or practice pattern differences among current Medicaid providers, nonproviders who used to accept Medicaid, and nonproviders who never accepted Medicaid.
Low fee reimbursement is perceived by all provider groups as a major problem with the Medicaid program.
Perceived problems with patient-related issues were more frequently cited by those who never accepted or are not currently accepting Medicaid patients.
Acknowledgments
Supported, in part, by NIH grant R01 DE005215, Influences on Stability Following Orthognathic Surgery.
We thank William Kalsbeek of the Survey Research Unit of the Biostatistics Department and Teresa Edwards at the Odum Institute for Research in Social Science at the University of North Carolina for their assistance with the final questionnaire at the University of North Carolina; Debbie Price for help with data entry and management; and the Policy Unit, Cecil G. Sheps Center for Health Services Research, which, with the North Carolina Area Health Education Centers Program and the independent health professions licensing boards in NC, maintains and assists researchers in accessing the Health Professions Data System.
References
- 1.GAO. Oral health: dental disease is a chronic problem among low-income populations. Washington, DC: General Accounting Office; 2000. [Google Scholar]
- 2.Salzmann JA. Orthodontics under Medicare and Medicaid. Am J Orthod. 1966;52:922–6. doi: 10.1016/0002-9416(66)90194-1. [DOI] [PubMed] [Google Scholar]
- 3.Parker WS. Government and orthodontics in California in 1994. Am J Orthod Dentofacial Orthop. 1995;107(3):22–3A. [PubMed] [Google Scholar]
- 4.Venezie RD, Vann WF., Jr Pediatric dentists’ participation in the North Carolina Medicaid program. Pediatr Dent. 1993;15:175–81. [PubMed] [Google Scholar]
- 5.Lang WP, Weintraub JA. Comparison of Medicaid and non-Medicaid dental providers. J Public Health Dent. 1986;46:207–11. doi: 10.1111/j.1752-7325.1986.tb03143.x. [DOI] [PubMed] [Google Scholar]
- 6.Damiano PC, Brown ER, Johnson JD, Scheetz JP. Factors affecting dentist participation in a state Medicaid program. J Dent Educ. 1990;54:638–43. [PubMed] [Google Scholar]
- 7.Capilouto E. The dentist’s role in access to dental care by Medicaid recipients. J Dent Educ. 1988;52:647–52. [PubMed] [Google Scholar]
- 8.Milgrom P, Riedy C. Survey of Medicaid child dental services in Washington state: preparation for a marketing program. J Am Dent Assoc. 1998;129:753–63. doi: 10.14219/jada.archive.1998.0318. [DOI] [PubMed] [Google Scholar]
- 9.Nainar SM, Tinanoff N. Effect of Medicaid reimbursement rates on children’s access to dental care. Pediatr Dent. 1997;19:315–6. [PubMed] [Google Scholar]
- 10.Shulman JD, Ezemobi EO, Sutherland JN, Barsley R. Louisiana dentists’ attitudes toward the dental Medicaid program. Pediatr Dent. 2001;23:395–400. [PubMed] [Google Scholar]
- 11.Kelly JE, Harvey CR. An assessment of the occlusion of the teeth of youths 12–17 years. Vital Health Stat. 1977;11(162):1–65. [PubMed] [Google Scholar]
- 12.Kelly JE, Sanchez M, Van Kirk LE. An assessment of the occlusion of the teeth of children 6–11 years. Washington, DC: National Center for Health Statistics; 1973. DHEW Publication No. (HRA) 74–1617. [PubMed] [Google Scholar]
- 13.King GJ, Hall CV, Milgrom P, Grembowski DE. Early orthodontic treatment as a means to increase access for children enrolled in Medicaid in Washington state. J Am Dent Assoc. 2006;137:86–94. doi: 10.14219/jada.archive.2006.0026. [DOI] [PubMed] [Google Scholar]
- 14.Salant P, Dillman DA. How to conduct your own survey. New York: Wiley; 1994. [Google Scholar]
- 15.US Census Bureau. [Accessed February 1, 2006.];Your gateway to census 2000. Available at: http://www.census.gov/main/www.cen2000.html.
- 16.Proffit WR. Contemporary orthodontics. 3. St Louis: Mosby; 2000. [Google Scholar]
- 17.McLain JB, Proffit WR. Oral health status in the United States: prevalence of malocclusion. J Dent Educ. 1985;49:386–97. [PubMed] [Google Scholar]
- 18.Mitchell JB. Physician participation in Medicaid revisited. Med Care. 1991;29:645–53. doi: 10.1097/00005650-199107000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Silverstein G. Physicians’ perceptions of commercial and Medicaid managed care plans: a comparison. J Health Polit Policy Law. 1997;22:5–21. doi: 10.1215/03616878-22-1-5. [DOI] [PubMed] [Google Scholar]
- 20.Gold M, Kuo S, Taylor EF. Translating research to action: improving physician access in public insurance. J Ambul Care Manage. 2006;29:36–50. doi: 10.1097/00004479-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Garner DD, Liao WC, Sharpe TR. Factors affecting physician participation in a state Medicaid program. Med Care. 1979;17:43–58. doi: 10.1097/00005650-197901000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Margolis PA, Cook RL, Earp JA, Lannon CM, Keyes LL, Klein JD. Factors associated with pediatricians’ participation in Medicaid in North Carolina. JAMA. 1992;267:1942–6. [PubMed] [Google Scholar]
- 23.Lam M, Riedy CA, Milgrom P. Improving access for Medicaidinsured children: focus on front-office personnel. J Am Dent Assoc. 1999;130:365–73. doi: 10.14219/jada.archive.1999.0206. [DOI] [PubMed] [Google Scholar]
- 24.Mirabelli JT, Huang GJ, Siu CH, King GJ, Omnell L. The effectiveness of phase I orthodontic treatment in a Medicaid population. Am J Orthod Dentofacial Orthop. 2005;127:592–8. doi: 10.1016/j.ajodo.2004.02.016. [DOI] [PubMed] [Google Scholar]


