Abstract
Introduction
Laparoscopic inspection before pancreatic and liver surgery is a widely accepted approach and has changed the surgical strategy in a growing number of patients for the last 10 years. The addition of intra-operative ultrasound to laparoscopy has further refined surgical judgments. The aim of this study was to evaluate the impact of open (IOUS) or laparoscopic (LIOUS) ultrasound in patients undergoing hepatic or pancreatic resection for benign or malignant lesions.
Materials and methods
In the years 2005–2008, 45 patients (aged 42–75 years) were selected for liver resection, and 48 others (aged 14–72 years) were selected for partial pancreatic resection. Intra-operative ultrasound was performed for surgical staging. An Aloka SSD-5500 scanner (Aloka, Tokyo, Japan) was used with a flexible laparoscopic multifrequency linear and an electronic T-shaped linear probe.
Results
LIOUS prevented useless laparotomies in six patients (13.3%) with liver tumors and, coupled with IOUS, revealed previously undetected tumors that required a change in the surgical strategy in 5 others (11.1%). In patients with pancreatic disease, LIOUS excluded the possibility of radical surgery in 7 patients (14.4%) due to the presence of mesenteric vein infiltration, involvement of the celiac or para-aortic nodes, or the presence of liver or peritoneal micro-metastases. In 11 patients with benign lesions, it defined the lesions’ relation to the Wirsung duct and splenic vessels, and in 6 others it provided guidance for aspiration of fluid for chemical and cytologic analysis.
Conclusions
LIUOS and IOUS can play fundamental roles in selecting patients for resective surgery and in planning the surgical approach. They provided information that affected surgical strategies in 11 patients with liver disease (24.4%) and 13 with pancreas disease (27%).
Keywords: Liver surgery, Pancreas surgery, Laparoscopic ultrasound
Sommario
Introduzione
L’ispezione laparoscopica in chirurgia del pancreas o del fegato è un approccio ampiamente utilizzato. L’aggiunta dell’ecografia intra-operatoria alla laparoscopia ha di recente ulteriormente migliorato la valutazione chirurgica. Lo scopo di questo studio è stato di valutare l’impatto dell’ecografia intra-operatoria open (IOUS) o laparoscopica (LIOUS) in chirurgia del fegato e del pancreas.
Materiali e metodi
Negli anni 2005–2008, 45 pazienti, di età 42–75 anni, sono stati selezionati per chirurgia epatica resettiva e 48 pazienti, di età 14–72 anni, per resezione parziale del pancreas. L’ecografia intra-operatoria è stata effettuata per mezzo di un apparecchio Aloka SSD-550 (Aloka, Tokyo, Giappone), con sonda lineare laparoscopica a punta flessibile e sonda elettronica lineare a T.
Risultati
Tra i pazienti epatici, la LIOUS ha evitato inutili laparotomie in sei pazienti (13,3%) ed, insieme alla IOUS, ha consentito di trovare noduli non diagnosticati ed ha cambiato la strategia chirurgica in cinque pazienti (11,1%). Nel gruppo pancreas, la LIOUS ha escluso 7 pazienti (14,4%) dalla chirurgia radicale, per infiltrazione della vena mesenterica, coinvolgimento dei linfonodi celici o para-aortici, micro-metastasi epatiche e peritoneali. In 11 lesioni benigne, ha consentito la definizione dei rapporti con il dotto di Wirsung ed i vasi splenici, in 6 ha guidato l’aspirazione di liquido per analisi chimiche e citologiche.
Conclusioni
Nella nostra esperienza la LIOUS e la IOUS hanno avuto la massima importanza sia nella selezione dei pazienti per la chirurgia resettiva e nel pianificare l’approccio chirurgico, influenzando la strategia chirurgica in 11 pazienti epatici (24,4%) e 13 pazienti pancreatici (27%).
Introduction
Evaluation of the extension and resectability of lesions is the main goal in liver and pancreas surgery. The sensitivity of pre-operative imaging studies has improved up to 60–75% with spiral CT and 80–85% with MR [1], but the combination of diagnostic laparoscopy and intra-operative ultrasound (LIOUS) has achieved 90–96% accuracy in the staging of liver and pancreatic malignancies. This allows patients who are not candidates for curative surgery to be spared the ordeal of laparotomy [2–4].
According to previous studies, intra-operative sonographic evaluation of abdominal malignancies provides additional information in 30–60% of the cases, and this information results in modification of the surgical strategy in 30–50% [5]. Adding ultrasound to the laparoscopic exploration of the abdominal cavity eliminates the main limitations of laparoscopy, which are:
-
-
underestimation of portal vein and regional lymph node involvement;
-
-
low sensitivity in the detection of liver metastases.
The purpose of this study was to evaluate the effectiveness of laparoscopic and open intra-operative ultrasound on surgical decision making and the staging of hepatic malignancies and benign or malignant pancreatic disease.
Materials and methods
In the years 2005–2008, 45 patients (aged 42–75 years) were selected for resective liver surgery and 48 others (aged 14–72 years) were selected for partial pancreatic resection at the General and Laparoscopic Surgical Dept. of the Monaldi Hospital in Naples, Italy. All the liver resections were for malignancies. The same was true for most of the pancreatic resections; 11 out of 48 (22.9%) were performed for benign pancreatic lesions (nodular or cystic).
All patients had been examined pre-operatively with biphasic contrast-enhanced spiral CT and trans-abdominal ultrasound. Laparoscopic ultrasonography (LIOUS) was done in all the cases. An Aloka SSD-5500 scanner (Aloka, Tokyo, Japan) was used with a flexible-tip, lateral-view multifrequency probe measuring 10 mm in diameter. When laparotomy was performed, intra-operative ultrasound (IOUS) was repeated with an electronic T-shaped linear probe.
Both probes have frequency ranges of 5–10 MHz. The probes were sterilized with hydrogen peroxide (STERRAD*), and no cover was utilized intra-operatively.
Results
In 6 of the 45 patients with liver tumors (13.3%), LIOUS revealed previously undetected bilobar intra-parenchymal nodes, which precluded curative resection. The examination thus spared 6 patients the ordeal of a useless laparotomy. In 5 other patients (11.1%), it provided information that changed the surgical strategy to include larger resections or additional segmentectomies (Figs. 1–3). Ultrasound was also helpful in defining tumor-free resection margins. It revealed insufficient resection in 4 patients (10.2%). Four resections were completed laparoscopically (10.2%); all the others (89.7%) were performed via laparotomy after hepatic pedicle clamping. LIUOS and IOUS were found to be particularly effective in the detection of sub-glissonian secondary lesions (central and peripheral) and in differentiating primary lesions from the regenerative nodules of chronic hepatitis. Moreover, it accurately defined the relationships of the lesions to the main portal pedicles, hepatic veins, and vena cava, thus allowing us to predict which vessels would be sectioned or spared during parenchymal transection.
Fig. 1.
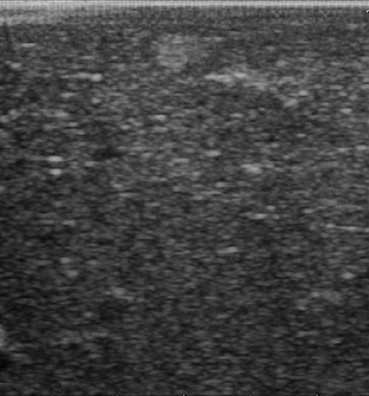
LIOUS revealed occult sub-glissonian metastases in the right hepatic lobe.
Fig. 2.

LIOUS revealed non detected superficial metastases of the right lobe.
Fig. 3.
IOUS revealed metastases of the VII segment of the liver and helped to define their relations to the right lateral portal pedicle and vena cava.
In the 48 patients with pancreatic disease, LIOUS excluded the possibility of curative resection in 7 cases (14.4%), because of mesenteric vein infiltration (4 patients, 8.3%) (Figs. 4,5), involvement of the celiac or para-aortic nodes (2 patients, 4.1%), or liver micro-metastases (1 patient, 2.1%).
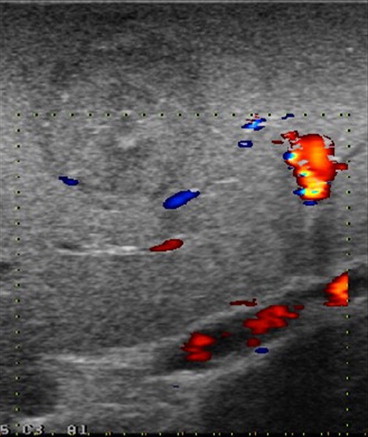
Fig. 4.

LIOUS: Tumors of the head of the pancreas with undetected infiltration of the mesenteric vein.
Fig. 5.
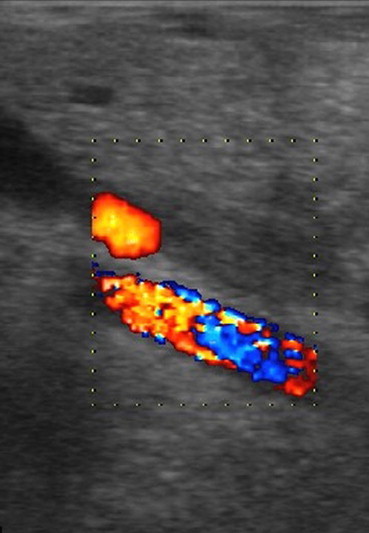
LIOUS: Tumors of the head of the pancreas with undetected infiltration of the mesenteric vein.
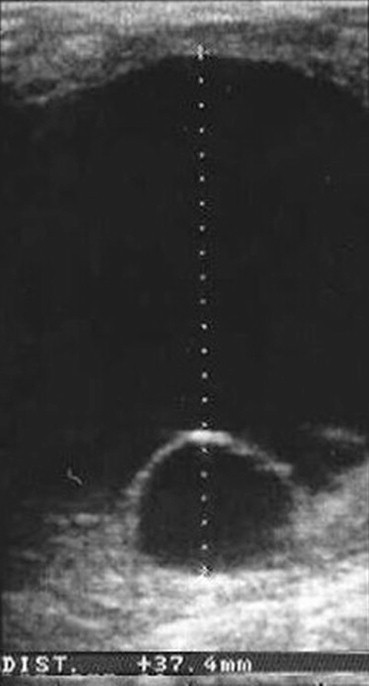
Ultrasound revealed the exact location of 8 cystic lesions and 3 benign endocrine nodules (insulinomas) (Fig. 6) and defined their elations to the Wirsung duct and splenic vessels. Five of the 8 cystic lesions were complex cystadenoma-like lesions (Figs. 7,8), which were subjected to ultrasound-guided aspiration of fluid for chemical and cytologic analysis.
Fig. 6.

LIOUS revealed the location of an insulinoma in the body of the pancreas.
Fig. 7.

Pre-operative ultrasound and LIOUS: Mucinous cystadenoma of the body of the pancreas.
Fig. 8.
Pre-operative ultrasound and LIOUS: Mucinous cystadenoma of the body of the pancreas.
In this study, LIOUS and IOUS played essential roles in the selection of candidates for resective surgery and for planning the surgical approach. The information provided affected the surgical strategy in 11 of the patients with liver disease (24.4%) and 13 of those with pancreatic disease (27%).
Discussion
For over 20 years intra-operative ultrasonography has been considered a useful pre-requisite for liver surgery [6]. It has been shown to change the surgical strategy in 30–50% of patients with liver tumors [5], and it reveals occult liver metastases in 5–10% of operations. Preliminary results with contrast-enhanced intra-operative ultrasound (CEUS) have shown that this approach is more effective for detecting small liver lesions. It provided information not obtainable with conventional intra-operative ultrasound and modified the course of surgery in 79% of patients undergoing resection for hepatocellular carcinoma [7]. In the detection of liver metastases, it attained 96.1% sensitivity vs. 81.5% with plain ultrasound [8].
In another study, LIOUS identified 17% of all undetected HCC nodules in patients undergoing liver resection [9] and allowed 38% of patients with hepatic metastases to avoid needless surgery [10]. Laparotomy was avoided in 63% of patients with unresectable hepatocellular carcinomas [11]. LIOUS identified liver tumors not visible at laparoscopy in 33% of the patients and provided staging information that supplemented laparoscopic findings in 42% [12].
Even with the most advanced imaging techniques (multiphase spiral CT, MRI, FDG-PET), approximately 30% of liver lesions< 2 cm are not visualized, and sensitivity is poor for nodules less than 1 cm in diameter [13].
In a study conducted by Norton et al. [4] on patients with pancreatic and liver malignancies, laparoscopy with ultrasound ruled out the possibility of radical surgery in 44% of the patients.
As for pancreatic surgery, evaluation of mesenteric vein infiltration, involvement of lymph nodes in the hepatic pedicle and celiac area, and detection of intra-hepatic metastases continue to be major hurdles for pre-operative imaging. The sensitivity of contrast-enhanced multiphase CT for diagnosis of vein infiltration has been estimated to be as high as 92%, when diagnosis is based on the criteria of venous obliteration, tumor involvement of more than one half of the vein circumference, vein wall irregularity, or stenosis [14].
With laparoscopic staging, the possibility of radical pancreatic resections was excluded in 24.3% and 26% of the patients in two studies [2,15]. The addition of LIOUS excluded an additional 11.1% of the candidates and increased sensitivity to 100% [2]. Other authors [16] have reported evaluation of the resectability of pancreatic cancer with a sensitivity of 90% for CT, 77% for endoscopic ultrasound, and 78% for LIOUS. John [17] found that LIOUS provided information not provided by laparoscopy in 53% of the cases and changed the decision regarding tumor resectability in 25%.
Evaluation of complex cystic lesions, location of endocrine tumors, and investigation of the relations with blood vessels and the Wirsung duct are possible only with endoscopic [18] and laparoscopic or intra-operative ultrasound (96% localization sensitivity) [19]. These approaches are also used to guide intra-operative aspiration of cyst fluid for chemical analysis.
The purpose of our study was to evaluate the effectiveness of laparoscopy plus laparoscopic ultrasound in staging liver and pancreas malignancies before the selection of a surgical strategy.
All but 4 of the liver resections were performed via laparotomy. LIOUS played a fundamental role in 11 cases (24.4%) by re-defining the disease stage (6 patients) or (coupled with IOUS) modifying the extent of resection (5 patients). In all cases, ultrasound provided important clinical and anatomic information relevant to the radicality of resection and integrity of the remaining parenchyma.
As for the patients with pancreatic disease, LIOUS excluded the possibility of radical resection in 7 of the 37 cases with malignant lesions (14.4%) by revealing infiltration of the mesenteric vessels, involvement of celiac or aortic nodes, or the presence of liver metastases that had been missed on pre-operative imaging studies.
Three insulinomas were located with the laparoscopic probe (in the head, body and tail of the pancreas). Removal of the first required open duodeno-pancreatectomy; the other two nodules were resected laparoscopically with enucleation. The 8 cystic lesions included 3 that proved to be pseudocysts and were drained laparoscopically. The other 5 were serous or mucinous cystadenomas. Two of these were resected laparoscopically with caudal spleno-pancreatectomy, and the other three were enucleated from the pancreatic tissue. In one case LIOUS revealed adherence of the cystic wall to a portion of the Wirsung duct. The patient underwent a second operation for repair of a pancreatic fistula and creation of an open pancreatico-jejunostomy. LIOUS played an essential role in surgical decision making in 13 patients (27%), but it gave important information in all cases.
Given the results of our experience, we believe that laparoscopy with the addition of ultrasound should be used increasingly in the pre-operative work-up of patients with liver tumors or pancreatic disease (benign or malignant). It can provide useful information for staging tumors, defining surgical anatomy, and making surgical decisions.
Conflict of interest statement
The authors have no conflict of interest.
References
- 1.Paulson E.K. Evaluation of the liver for metastatic disease. Semin Liver Dis. 2001;21(2):225–236. doi: 10.1055/s-2001-15498. [DOI] [PubMed] [Google Scholar]
- 2.Menack M.J., Spitz J.D., Arregui M.E. Staging of pancreatic and ampullary cancers for resectability using laparoscopy with laparoscopic ultrasound. Surg Endosc. 2001;15(10):1129–1134. doi: 10.1007/s00464-001-0030-6. [DOI] [PubMed] [Google Scholar]
- 3.Poon R.T. Current role of laparoscopic surgery for liver malignancies. Surg Technol Int. 2007;16:73–81. [PubMed] [Google Scholar]
- 4.Norton J.A. Intraoperative methods to stage and localize pancreatic and duodenal tumors. Ann Oncol. 1999;10(Suppl. 4):182–184. [PubMed] [Google Scholar]
- 5.Machi J.B., Sigel B. Intraoperative and laparoscopic ultrasound: a surgical tool of great versatility. In: Baker R.J., Fischer J.E., editors. Mastery of surgery. 4th. Lippincott Williams and Wilkins; 2001. pp. 226–237. [Google Scholar]
- 6.Bismuth H., Castaing D. Peroperative echography in hepatobiliary surgery. Ann Gastroenterol Hepatol. 1984;20(4):221–223. [PubMed] [Google Scholar]
- 7.Saar B., Kellner-Weldon F. Radiological diagnosis of hepatocellular carcinoma. Liver Int. 2008;28(2):189–199. doi: 10.1111/j.1478-3231.2007.01655.x. [DOI] [PubMed] [Google Scholar]
- 8.Leen E., Ceccotti P., Moug S.J., Glen P., Mac Quarrie J., Angerson W.J. Potential value of contras enhanced intraoperative ultrasonography during partial hepatectomy for metastases: an essential investigation before resection? Ann Surg. 2006;243(2):236–240. doi: 10.1097/01.sla.0000197708.77063.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santambrogio R., Opocher E., Ceretti A.P., Barabino M., Costa M., Leone S. Impact of intraoperative ultrasonography in laparoscopic liver surgery. Surg Endosc. 2007;21(2):181–188. doi: 10.1007/s00464-005-0738-9. [DOI] [PubMed] [Google Scholar]
- 10.Rahusen F.D., Cuesta M.A., Borgstein P.J., Bleichrodt R.P., Barkhof F., Doesburg T. Selection of patients for resection of colorectal metastases to the liver using diagnostic laparoscopy and laparoscopic ultrasonography. Ann Surg. 1999;230(1):31–37. doi: 10.1097/00000658-199907000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lo C.M., Lai E.C.S., Liu C.L., Fan S.T., Wong J. Ann Surg. 1998;227(4):527–532. doi: 10.1097/00000658-199804000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.John T.G., Greig J.D., Crosbie J.L., Miles W.F.A., Garden O.J. Superior staging of liver tumors with laparoscopy and laparoscopic ultrasound. Ann Surg. 1994;220(6):711–719. doi: 10.1097/00000658-199412000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sahani D.V., Kalva S.P. Imaging the liver. Oncologist. 2004;9:385–397. doi: 10.1634/theoncologist.9-4-385. [DOI] [PubMed] [Google Scholar]
- 14.Li H., Zeng M.S., Zhou K.R. Pancreatic adenocarcinoma: the different CT criteria for peri pancreatic major arterial and venous invasion. J Comput Assist Tomogr. 2005;29:170–175. doi: 10.1097/01.rct.0000155060.73107.83. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed S.I., Bochkarev V., Oleynikov D., Sasson A.R. Patients with pancreatic adenocarcinoma benefit from staging laparoscopy. J Laparoendosc Adv Surg Tech. 2006;16(5):458–463. doi: 10.1089/lap.2006.16.458. [DOI] [PubMed] [Google Scholar]
- 16.Long E.E., Van Dam J., Weinstein S., Jeffrey B., Desser T., Norton J.A. Computed tomography, endoscopic, laparoscopic and intra-operative sonography for assessing resectability of pancreatic cancer. Surg Oncol. 2005;14(2):105–113. doi: 10.1016/j.suronc.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 17.John T.G., Greig D.J., Carter D.C., Garden O.J. Carcinoma of the pancreatic head and periampullary region. Tumor staging with laparoscopy and laparoscopic ultrasonography. Ann Surg. 1995;221(2):156–164. doi: 10.1097/00000658-199502000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raj M., Chen R. Interventional applications of endoscopic ultrasound. J Gastroenterol Hepatol. 2006;21(2):348–357. doi: 10.1111/j.1440-1746.2006.04214.x. [DOI] [PubMed] [Google Scholar]
- 19.Pitre J., Soubrane O., Dousset B., Palazzo L., Chapuis Y. Pancreatic echo-endoscopy and preoperative localization of insulinomas. Ann Chir. 1998;52(4):369–373. [PubMed] [Google Scholar]


