Abstract
Introduction
Obstructive uropathy caused by kidney stones is quite rare in transplant kidneys.
Clinical case
The authors report the case of a patient, previously gastrectomized for gastric carcinoma. He underwent renal transplantation using uretero-ureterostomy, and presented an episode of acute renal failure 7 years after surgery. Ultrasound (US) examination showed no sign of rejection but allowed detection of moderate hydronephrosis in the transplant kidney. Subsequent computed tomography (CT) revealed a kidney stone in the middle ureter at the crossing of the iliac vessels. The patient therefore urgently underwent percutaneous nephrostomy of the graft and recovered diuresis and renal function. The patient was transferred to the Transplant Center where he underwent ureterotomy with removal of the stone and subsequent ureteropyelostomy. Also transureteral resection of the prostate (TURP) was performed due to urinary retention of prostatic origin. Histological examination showed prostate carcinoma, Gleason stage 3, which was treated conservatively using radiotherapy without suspension of the administered low dose of immunotherapy.
Discussion
Calculosis is one of the least common causes of obstructive uropathy in transplant kidneys. In the described case, US examination performed after onset of renal insufficiency led to subsequent radiological investigation and resulting interventional procedures (nephrostomy and surgical removal of the stone) with complete recovery of pre-existing renal function.
Keywords: Kidney transplantation, Obstructive uropathy, Acute renal failure, Ureteral calculus
Sommario
Introduzione
L'uropatia ostruttiva da calcolosi si verifica di rado nel rene trapiantato.
Caso clinico
Gli autori riportano il caso di un paziente trapiantato renale mediante uretero-stomia, già sottoposto a gastrectomia per carcinoma gastrico, che presenta episodio di insufficienza renale acuta 7 anni dopo l'intervento. L'esame ecografico non mostra segni di rigetto e permette di evidenziare viceversa un'idronefrosi di grado non marcato a carico del rene trapiantato. La successiva TC rivela calcolo del tratto medio dell'uretere a livello dell'incrocio con i vasi iliaci. Il paziente viene pertanto sottoposto, in urgenza, a nefrostomia percutanea del graft con buona ripresa della diuresi e della funzionalità renale. Inviato presso il Centro Trapianti di competenza viene sottoposto ad intervento di ureterotomia con asportazione del calcolo e successiva uretero-pielotomia. Per ritenzione urinaria di origine prostatica viene inol-tre sottoposto a TURP. L'esame istologico mostra carcinoma prostatico stadio 3 sec. Gleason, che si decide di trattare in modo conservativo con radioterapia, con mantenimento della già blanda terapia immunodepressiva.
Discussione
La calcolosi viene annoverata tra le cause meno comuni di uropatia ostruttiva del rene trapiantato. Nel caso descritto l'ecografia effettuata dopo l'insorgenza dell'insufficienza renale acuta ha consentito di avviare rapidamente il paziente alle successive indagini radiologiche ed alle conseguenti procedure interventistiche (nefrostomia e bonifica chirurgica del calcolo) con completo ripristino della funzionalità renale pre-esistente.
Introduction
Urological complications in transplant kidneys occur with an incidence ranging from 3% to 20% [1,2]. The most common causes of obstructive uropathy of the graft are classified as renal and extra-renal. Among early renal complications are perirenal fluid collections (lymphocele, hematoma, urinoma), and in the later stage stricture and vescico-ureteral reflux [3]. Among the extra-renal causes there are benign prostatic hypertrophy and ureteral stenosis [2]. Urinary calculosis and particularly obstruction due to a kidney stone in the excretory tract of transplanted kidneys are less frequently reported in literature.
Case report
A 73-year-old male patient was diagnosed mild chronic renal failure (CRF) in 1983 (serum creatinine 1.7 mg/dl) due to adult polycystic kidney disease (APKD). In 1995 he underwent median laparotomy to empty the cysts of the right kidney. In 1997 he was diagnosed as hypertensive. The urologist prescribed alphalytic drug (Xatral 2.5 mg) for a bladder diverticulum originating from the left side bladder wall, detected by cystography. In November of the same year, renal replacement therapy was started using continuous ambulatory peritoneal dialysis (CAPD) due to progressive deterioration of the kidney function.
In 1999 a basal cell epitelioma was excised from the left side of the nose. In October 2000 CAPD was interrupted due to inadequacy of dialysis, and hemodialysis was started three times a week. On 7 July 2001 the patient underwent renal transplantation into the right iliac fossa using the uretero-ureterostomy technique.
Already on the third day, the patient presented transitional obstructive uropathy with ureteral stricture at the bladder neck associated with secondary bladder diverticulum. Immunodepressive therapy was initiated with administration of IL2 anti-receptor antibodies (Simulect), steroids in progressively decreased doses and tacrolimus. At discharge from the Transplant Center, serum creatinine was 1.3 mg/dl. In November 2001, the patient had deep vein thrombosis of the right leg. In 2006, he underwent total gastrectomy and Roux-en-y reconstruction due to gastric adenocarcinoma. At subsequent outpatient controls, the patient presented a stable renal function (serum creatinine 1.6 mg/dl) with normal ultrasound (US) appearance of the transplant kidney (Fig. 1). In November 2008 he was urgently admitted to our Department of Nephrology for the onset of oligoanuric acute renal failure (ARF) associated with elevated serum creatinine (5.89 mg /dl, glomerular filtration (GF) according to MDRD 10 ml/ minute/1.73 sq. m) and azotemia (BUN 66 mg/dl).
Fig. 1.

Renal US using a 3.5 MHz probe. Kidney transplanted into the right iliac fossa 5 years before; volume is slightly increased (longitudinal axis >12 cm) with normal echostructure and no sign of rejection.
US examination using Acuson Antares system and a convex 3.5 MHz probe showed dilation of the excretory tract of the transplant kidney with preserved renal parenchyma (Fig. 2); Color Doppler US (CDUS) showed increased intra-parenchymal resistive index (RI) values (Fig. 3). The presence of meteorism and the patient's poor clinical condition hindered a further study of the extra-renal excretory tract.
Fig. 2.
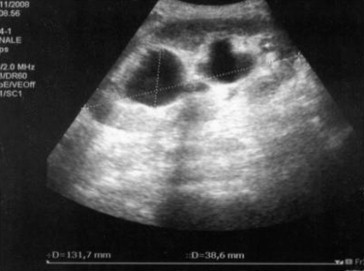
Renal US shows acute renal failure. The volume of the renal graft is increased compared to the previous examination (longitudinal axis >13 cm) with moderate dilation of the upper and lower calyceal system (3.9 cm in diameter) but the parenchyma appears unchanged.
Fig. 3.
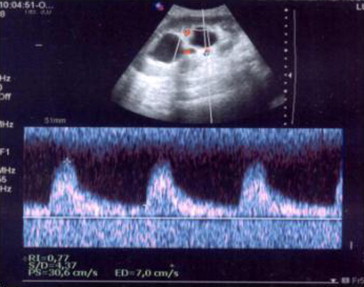
Color Doppler US. Spectral analysis. Acute phase of the obstruction of the excretory tract of the transplant kidney: RI 0.77.
On the basis of US findings, the patient underwent CT with contrast agent (CA), which confirmed the presence of hydroureteronephrosis of the transplant kidney with the ureter folded back on itself at the crossing of the iliac vessels, where a radiopaque stone of 8 mm in diameter was visible (Fig. 4). US-guided puncture of the middle calyx of the transplant kidney was therefore carried out with subsequent pyelography and placement of a percutaneous nephrostomy stent (Fig. 5). This treatment caused an immediate recovery of diuresis up to frank polyuria and lower values of serum creatinine (1.67 mg/dl) and azotemia (BUN 24 mg/dl) similar to pre-existing levels. The patient was subsequently referred to the Transplant Center where the presence of a kidney stone associated with a stenotic lesion and ureteral bending was confirmed. The urinary tract of the transplant kidney was submitted to surgical revision with removal of the stone and utereropyelostomy with insertion of a double J stent. At discharge from hospital serum creatinine value was 1.5 mg/dl; the ureteral stent and the bladder catheter were temporarily left in place.
Fig. 4.
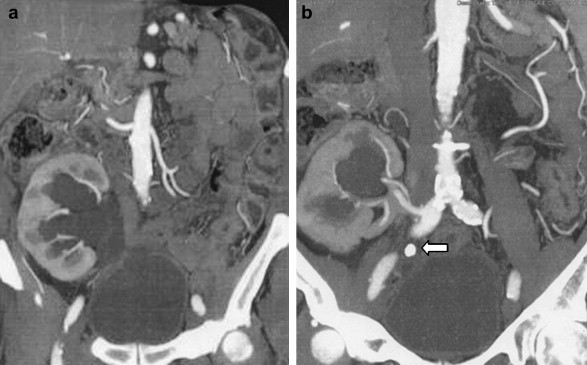
CT using contrast agent and coronal MIP reconstruction. a. the study confirms dilation of the excretory tract of the transplant kidney. b. a kidney stone is visible at the crossing of the iliac vessels (arrow).
Fig. 5.
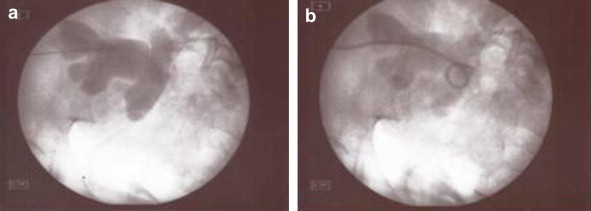
Percutaneous nephrostomy of the transplant kidney. a. pyelography with insertion of the guide wire. b. placement of nephrostomy stent.
In January 2009, a renewed attempt to remove the bladder catheter at the Transplant Center was postponed, because the patient had urinary retention. In February 2009, he had an episode of urinary tract infection, which was treated with ciprofloxacin. In February, the patient was again hospitalized at the Transplant Center for removal of the ureteral stent, but the bladder catheter was still left in place.
In March, transureteral resection of the prostate (TURP) was finally carried out at the Transplant Center. Histological examination showed prostate cancer Gleason stage 3, which was treated only with radiotherapy due to the patient's poor clinical condition. The dose of immunosuppressive therapy was already administered in very small doses due to the previous, removed gastric cancer and was therefore not decreased. At the last US follow-up in our department, serum creatinine value was stable (1.6 mg/dl) and hydronephrosis had completely disappeared (Fig. 6); CDUS yielded normal intra-parenchymal blood flow indices (Fig. 7).
Fig. 6.

US. Hydronephrosis of the transplant kidney has completely resolved after removal of the kidney stone with subsequent uretero-ureterostomy and TURP.
Fig. 7.
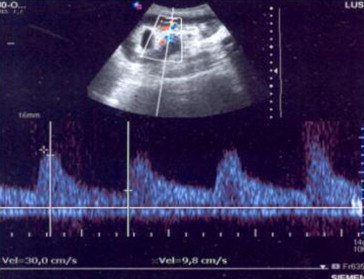
Color Doppler US of the kidney. Spectral analysis. RI value is normal (0.67).
Discussion
The described case is related to a clinically stable patient with a well-functioning renal graft, who presented an episode of acute renal failure due to ureteral obstruction caused by a stone in the excretory tract of the transplant kidney more than 7 years after surgery. Obstructive uropathy occurs in approximately 2% of transplant kidneys, but almost always within the first 6 months after transplantation. The most frequent cause is ureteral stenosis, which in more than 90% of cases involves the distal tract of the ureter. Stricture of the distal ureter is more often due to scarring caused by ischemia or rejection. Less common causes of obstructive uropathy are pelvic fibrosis, compression due to perirenal fluid collections and kidney stones [4]. The latter is a rare complication in transplant kidneys and is reported in less than 2% of cases [5]. Cases of bladder stones have been reported [6] also associated with acute renal insufficiency in patients with renal grafts [7] as well as 4 cases of bladder stones in patients with combined renal/pancreas transplantation [8]. In a more recent study of 1535 patients, only 9 cases of ureteral calculosis were reported [9].
In the described case, transplantation carried out by uretero-ureterostomy (instead of the traditional ureteral neocystostomy) and subsequent ureteral stenosis associated with ureteral bending and narrowing at the crossing of the iliac vessels can have contributed to the stone formation. US examination is used for evidencing urological complications [10–13] in renal grafts and particularly for detecting proximal ureteral stones located under the ureteropelvic junction [14]. However, midureteral tract stones are more effectively detected using computed tomography (CT) or magnetic resonance urography (MRU) [15]. US examination of the transplant kidney carried out as a routine examination at the department of nephrology permitted an early diagnosis of obstructive uropathy caused by acute renal failure which was the basis for the subsequent surgical treatment at the Transplant Center. Subsequent US follow-up provided confirmation of the good outcome of the operation and recovery of pre-existing renal function.
In addition to the causes for obstructive uropathy which are specific in transplant kidneys, also more common causes of obstructive uropathy occurring in normal non-transplanted kidneys, should be considered. In this patient also TURP can have contributed to the recovery of the patency of the urinary tract. The US study was essential to the subsequent radiological investigation, surgical treatment of obstructive uropathy and complete recovery of the renal function.
Conflict of interest statement
The authors have no conflict of interest.
References
- 1.Zavos G., Pappas P., Karatzas N.P. Urological complications: analysis and management of 1525 consecutive renal transplantations. Transplant Proc. 2008;40:1386–1390. doi: 10.1016/j.transproceed.2008.03.103. [DOI] [PubMed] [Google Scholar]
- 2.Pisani F., Iaria G., D'Angelo M. Urologic complications in kidney transplantation. Transplant Proc. 2005;37:2521–2522. doi: 10.1016/j.transproceed.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 3.Dinckan A., Tekin A., Turkyilmaz S. Early and late urological complications corrected surgically following renal transplantation. Transpl Int. 2007;20:702–707. doi: 10.1111/j.1432-2277.2007.00500.x. [DOI] [PubMed] [Google Scholar]
- 4.Akbar S.A., Jafri S.Z., Amendola M.A., Madrazo B.L., Salem R., Bis K.G. Complications of renal transplantation. Radiographics. 2005;25:1335–1356. doi: 10.1148/rg.255045133. [DOI] [PubMed] [Google Scholar]
- 5.Reinberg Y., Bumgardner G.L., Aliabadi H. Urological aspects of renal transplantation. J Urol. 1990;143:1087–1092. doi: 10.1016/s0022-5347(17)40194-7. [DOI] [PubMed] [Google Scholar]
- 6.Klein F.A., Goldman M.H. Vesical calculus: an unusual complication of renal transplantation. Clin Transplant. 1997;11(2):110–112. [PubMed] [Google Scholar]
- 7.Thakar C.V., Lara A., Goel M., Nally J.V., Jr. Staghorn calculus in renal allograft presenting as acute renal failure. Urol Res. 2003;31:414–416. doi: 10.1007/s00240-003-0364-8. [DOI] [PubMed] [Google Scholar]
- 8.Rhee B.K., Bretan P.N., Jr., Stoller M.L. Urolithiasis in renal and combined pancreas/renal transplant recipients. J Urol. 1999;161(5):1458–1462. [PubMed] [Google Scholar]
- 9.Streeter E.H., Little D.M., Cranston D.W., Morris P.J. The urological complications of renal transplantation: a series of 1535 patients. BJU Int. 2002;90:627–634. doi: 10.1046/j.1464-410x.2002.03004.x. [DOI] [PubMed] [Google Scholar]
- 10.O'Neill W.C. WB Saunders Company; Philadelphia: 2001. Urinary obstruction in renal allograft. Atlas of renal ultrasonography. pp. 213–219. [Google Scholar]
- 11.Gottlieb R.H., Voci S.L., Cholewinsky S.P. Sonography: a useful tool to detect the mechanical causes of renal transplant dysfunction. J Clin Ultrasound. 1999;27:325–333. doi: 10.1002/(sici)1097-0096(199907/08)27:6<325::aid-jcu3>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 12.Lusenti T. Ecocolordoppler e mezzi di contrasto in Nefrologia. Bios Ed. Cosenza. 1998. Valutazione degli indici di flusso nel trapianto renale; pp. 63–71. [Google Scholar]
- 13.Brown E.D., Chen M.Y., Wolfman N.T., Ott D.J., Watson N.E., Jr. Complications of renal transplantation: evaluation with US and radionuclide imaging. Radiographics. 2000;20:607–622. doi: 10.1148/radiographics.20.3.g00ma14607. [DOI] [PubMed] [Google Scholar]
- 14.Hélénon O., Correas J.M., Eiss D. Diagnostic imaging of the renal graft and complications of renal transplantation. EMC-Néphrologie. 2005;2:83–102. [Google Scholar]
- 15.Blondin D., Koester A., Andersen K., Kurz K.D., Moedder U., Cohnen M. Renal transplant failure due to urological complications. Comparison of static fluid with contrast-enhanced magnetic resonance urography. Eur J Radiol. 2009:69324–69330. doi: 10.1016/j.ejrad.2007.10.026. [DOI] [PubMed] [Google Scholar]


