Abstract
Efficient workflow is essential for a successful business. However, there is relatively little literature on analytical tools and standards for defining workflow and measuring workflow efficiency. Here, we describe an effort to define a workflow lexicon for medical imaging departments, including the rationale, the process, and the resulting lexicon.
Keywords: Workflow, Cost-effectiveness, Controlled vocabulary, Data mining, Radiology workflow, Workflow re-engineering
Background
About 25 years ago, there was chaos in medical imaging. Each vendor’s CT and MR scanner produced images in a different, proprietary format. Any person wishing to view or further process the images had to either use that vendor’s workstation, or purchase a workstation with the ability to read that make and model’s format (Images were transferred between computers using 0.5-in. tape). This was clearly impeding research and clinical practice, and led the Radiology community to work with vendors to develop open standards for image information exchange, now known as Digital Imaging and Communications in Medicine (DICOM).
Imaging Informatics is moving beyond its foundational role of creating a filmless environment for medical imaging and is increasingly focused on the more ambitious goal of creating tangible, measurable improvements in their imaging operations. Being “Filmless” is no longer sufficient. The expectation now is that electronic systems should improve quality, workflow efficiency, operational efficiency, and the overall patient experience. Just as with imaging standards, there is a similar need for standard methods to exchange information about business processes in medical imaging. Future healthcare public policy will include requirements for national metrics and performance standards, and the pressures for improved cost-effectiveness and quality will continue to mount. At the same time, radiology workflow has become more complex with the incorporation of more types of acquisitions, 3D processing, fusion of multiple modalities, interventions, clinical applications, remote workers, critical and semi-urgent results communications, and electronic distribution of results. Business analytics tools are becoming an essential part of every efficiently run organization, but standards for collecting this information from the component systems in an imaging department are lacking.
Recently, the Society for Imaging Informatics in Medicine (SIIM) launched an effort to define a lexicon for workflow in a medical imaging department. This effort is now referred to as SWIM: the SIIM Workflow Initiative for Medicine. This lexicon was developed by a variety of people working in imaging departments, including physicians, physicists, technologists, and picture archiving and communication system (PACS) administrators. The draft lexicon has been released (http://www.siimweb.org/trip/) and a demonstration project was shown in June of 2011. The purpose of this paper is to provide a more thorough description of the rationale, the content, and the future for business analytic standards. We have not included the lexicon in this paper because of its size, and because changes may be made to the lexicon after this publication.
The Rationale for a Workflow Lexicon
Economic globalization has driven competition to a world-wide scale. The conversion of medical records to digital from paper drives an expectation of immediate access to information critical to an organization’s operations. When these are combined, a need arises to compare information within and between organizations to determine who is most efficient, to understand and model best practices, and to measure what impact changes in work processes are having on a business. These are the core elements of running a modern business. “Business Analytics Tools” provide access to the information about a business. The information for a medical imaging department might include the number of imaging examinations performed, the time it takes the interpreting physician to create a final report, room utilization rate, and patient waiting times and wait queues. This is far from a complete list.
Many organizations are increasingly able to collect at least some of the information they need to run their business electronically, and if not in “real time” at least within clinically relevant times. They can display it in an easy-to-understand format within a web page or computer application. These displays are often known as “dashboards” because much like a car dashboard, it gives a quick view of what is going on. Some indicators are like a speedometer and can show a linear scale of how “fast” you are going. Some indicators are “on–off” and can indicate problems. While most car dashboards don’t allow user interaction, business dashboards usually let the user “drill down” into a reading to understand it better, or to get finer granularity. For instance, if one indicator is “Average Report Turnaround Time”, which shows the mean time for all reports in a department, one might wish to see the times for just 1 building, 1 modality across an enterprise, or for 1 individual. In the case of a binary indicator like “Long Patient Waits”, the indicator might go on when more than 5 % of patients in any area waits more than 30 min from check-in to entering the imaging room. If this indicator light goes on, clicking the light could then display the area(s) with the long wait times, and the actual values.
One of the primary barriers to achieving the goal of improved efficiency and departmental agility through widespread use of these types of business intelligence tools is the lack of a common set of terms (or lexicon) to describe workflow steps in radiology. This becomes particularly important when organizations try to automatically capture data across systems to both measure and understand performance. The same workflow steps (e.g., completing a patient examination) may be called different things in different information systems, or may be “hidden” in proprietary system architectures. For staff members charged with analyzing and reporting on organizational performance across an increasing number of systems, simply mining for data is often a labor-intensive endeavor.
Establishing a lexicon may allow leveraging of workflow management tools to improve the quality and efficiency of imaging departments. Workflow engines are systems that are able to execute defined routines based on a set of conditions. While this capability can be met by lesser technologies, a workflow system has numerous advantages. First, a workflow system allows easier and better creation and maintenance of the rules, often using a graphical user interface. Other important capabilities are: scalability, high availability, and state preservation. In healthcare, it could be disastrous if a workflow engine crashed and was unable to confidently establish the status of all workflows at the time of the crash, as well as their current state. Most workflow engines also provide a wide range of communications methods, including web services, email, and basic web page templates. These workflow engines have been used in other industries for many years and have achieved a high level of maturity. Some workflow engines have also been applied in medicine [1, 2] but we have not found a report in the medical imaging literature. Extending a workflow engine platform to support the data transfer methods described above would be useful. It is likely that it would also need to communicate using DICOM and HL7 if it were to be truly integrated into an imaging department to assist in workflow management.
Status of the SWIM Workflow Lexicon
Lexicon Creation
After the need for better workflow tools was identified, the SIIM Board commissioned the workflow group and as part of its charge its first step was to develop a lexicon of workflow terms. The majority of terms describe workflow events in a medical imaging department—events like the examination being ordered, scheduled, patient arriving in the imaging department, patient entering the imaging suite, examination started, examination completed, final report completed, and billing. Not every step described applies to every examination (e.g., 3D post-processing), and some steps might be done multiple times (e.g., if examination is re-scheduled). Some steps may exist as electronic medical record (EMR) events communicated via HL7 (examination ordered), while others may be DICOM header elements (time when a series is acquired). Similarly different events originate from different components: a PACS event (examination is ready for interpretation) or a radiology information system (RIS) event (final report submitted). Different organizations may accomplish these in different systems. Of greater importance is that even within a complex organization, the same name may reflect different events because of different practices or systems, and different names may be used to reflect the same event. A standard lexicon addresses this problem, by providing a common term for the same event, regardless of the system that generates the event.
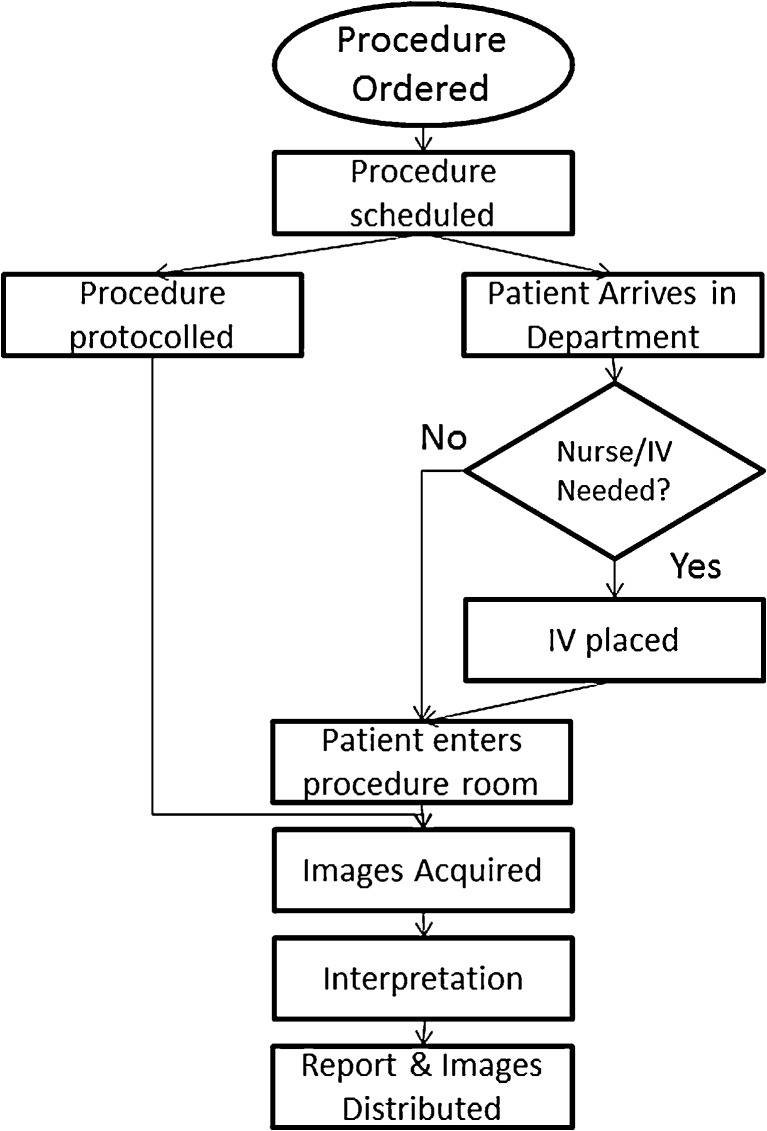
An important part of the effort was determining the correct level of granularity. If too few events were defined, important information might not be available for managing a department. On the other hand, defining too many steps might lead to confusion or be overly complex and burdensome. Ultimately, about 100 steps were defined. Figure 1 shows a simple workflow diagram with far fewer than 100 steps.
Fig. 1.
An example workflow diagram for an imaging examination. This shows only a few steps of the actual workflow. It also does not show such things as resident reporting, PACS preparation steps, or occasional events like report revisions/corrections. However, the lexicon does include all of these steps
After defining some of the events in a department, the group next reviewed some of the commonly used key performance indicators (KPIs) used by departmental administrators for managing their groups. In addition, several “state” events were defined—things like “PACS is down”, “PACS is up”, “RIS is down”, “Room is available”, etc. Seven common KPIs (including ones like report turn-around time, patient wait time, room utilization rate, system uptime) were then defined using the events previously described.
As a final step, the group attempted to define a method for communicating the events to a business intelligence (BI) system. After much discussion, it was determined that relatively simple and lightweight web services would be the easiest model to implement, providing flexibility to adapt the system as the technology and uses develop.
Lexicon Evaluation
Having defined a lexicon and a method for communicating events, the SWIM group set about to create a demonstration of the technology. It was recognized that no system or group of systems created records for all of the approximately 100 events that had been defined—in fact, most departments had only a small fraction. However, they typically did collect the events that allowed them to collect the KPIs they were interested in. Therefore, it was decided to focus on two or three KPIs in the demonstration project—specifically, report turn-around time, patient wait time, and examination volumes. The focus, after all, was on demonstrating interoperability of the BI tools and the systems that supplied the information, much as a PACS can work with modalities from any vendor because of the DICOM standard.
The team from The University of Maryland School of Medicine created a test dataset of approximately 17,000 examinations, and populated timestamps for an important subset of events—events that were both based on the SWIM Lexicon and used in the definition of the three KPIs that were selected. The dataset also had information like time, date, modality, and facility, allowing users of the BI tools to perform subgroup analysis. This test dataset was hosted via SIIM’s cloud-based infrastructure to provide remote access. A representational state transfer (REST)-style data provider service (including an exam query service) was created to provide access to the test dataset, and a query syntax was defined using Javascript Object Notation (JSON). Agfa, General Electric, and the University of Maryland created BI tools that used those web services, providing a demonstration of the ability to use BI tools that were not vendor-specific. Each presented the same information in different ways, much as a PACS presents the same images but in different ways. We should note here that while the initial set of KPIs are rather simple, the lexicon currently includes over 100 steps, including many unique workflows, such as those occurring in academic, teleradiology, and interventional practices.
Next Steps
Lexicon Evaluation
Defining a lexicon is an important step, but it is just the first step. The lexicon represents the impressions/opinions of a few people, and is likely not comprehensive. SIIM recently awarded a grant that will study the coverage of the lexicon within one academic department. Further studies focusing on coverage in such areas as interventional radiology, and other imaging departments like cardiology, surgery, and pathology are important to perform as well. A process of adding terms will include vetting and analysis by the SWIM TRIP Workflow group and this process will be needed as long as innovations occur in medical practice. While we recognize that some terms are like missing, complete coverage is not required for adoption, though a reasonably complete coverage of the events important for business management is required. We believe that is present in the version currently available at the SIIM website.
Standards for Event Access
Just as it was critical to define the way to share imaging data in order to enable PACS and RIS, it is necessary to define ways to exchange event information between systems and dashboarding tools. The value of event information is critically dependent on combining information from many systems, including EMRs, RISes, PACS, modalities, 3D post-processing systems, and perhaps other devices like contrast media injectors. In order to effectively manage a department, one must see the information from all these systems that are used in an imaging department. At present, fairly simple web services have effectively addressed the needs. It is hoped that this will be sufficiently flexible and simple that it will be easy for vendors to adopt and will provide functionality that customers will be willing to pay for.
Like many new technologies, there is a certain “chicken and egg” phenomenon that must be hurdled. There are basic dashboarding tools available, but they will only be valuable to customers that have all one vendor for major systems, or when this exchange system is adopted. As greater convergence ripples through the healthcare system, the likelihood of having uniform vended systems is small, driving greater need for cross-vendor exchange. Further, it will be important that vendors adopt the lexicon, so that events have the same meaning. Without that, the meaning of events in the various parts of a large enterprise will be different, leading to confusion, and reducing the value. It is hoped that since these tools are early in development and implementation, vendors, and customers will adopt common terms where possible, and interact with the workflow group to make necessary adjustments or additions to the lexicon.
Workflow Optimization
Once multiple sites are measuring events in the same way, it should be much easier to compare workflows. Non-standard workflow terms make comparison laborious if not impossible. While it is unlikely that there will be one optimal workflow for all imaging departments, it is possible that optimal workflows will be determined for given situations (e.g., small outpatient CT imaging units or large outpatient screening mammography).
Quality improvement suggests that the steps in a process that have high variability are most likely to degrade quality. Measurement of events, and the variability of the timing of events, should assist in identification of those steps presenting the greatest opportunity for quality improvement
Workflow Automation
It is possible that adoption of a lexicon can go beyond observation of events to automation of some workflows. Other industries use workflow engines to maximize automation of business processes, and to help enforce optimal workflows. Today, workflow is largely provided by RISes or PACS that generally enforce a fairly simple and linear workflow represented by an examination proceeding through several steps (e.g., ordered, scheduled, prepared, are interpreted). Workflow engines can allow for non-linear workflows, and provide far superior exception handling (e.g., if more than X minutes have elapsed after the examination is completed there is no report, please send an alert to Y).
Standardization
Efficient and effective workflow is a requirement for a successful imaging department. Proper management requires that managers have access to accurate information in a timely fashion. Both external and internal forces drive a need to be able to compare workflows within and between departments. A workflow standard is a requirement for this first step. Once a lexicon is agreed upon, there are many possibilities to define and optimize workflows, and improve quality. In turn, this may also assist in the adoption of workflow engines in healthcare.
There is also a need to work with standards bodies and imaging departments on implementation of systems that can collect the workflow events. One example is that DICOM defines a tag for image acquisition time (0008:0032). The exact implementation appears to vary with manufacturers—some appear to use it for the time that the X-ray beam was turned on or RF gradients started. But in the case of MRI with a “prescan”, does that refer to the prescan or the “main” acquisition? For some, this time appears to reflect when the image is reconstructed. It is clearly essential that such definitions be harmonized if they are to be used as uniform workflow events. Even more complex is that different parts of the practice may have workflows that drive different practical implementations of events. For instance, if one part of a practice must use the RIS to signal the end of an examination, while another uses performed procedure step, there will be differences in the actual values. If a patient has multiple examinations scheduled for the same time and location (e.g., a chest X-ray and a knee X-ray) which examination gets the first “arrival time” or do they get the same? We recognize that there are important practical issues that are to be faced, but we must not let the desire for perfection prevent us from accomplishing good.
An important question is whether web services are the correct technology for collecting this information. Some vendors are well positioned to implement this, but older systems are not. Furthermore, not every useful event reflects an activity that is captured electronically by either radiology or other clinical information systems. For instance, examinations that use intravenous contrast may require a need to measure and understand nurse workflow, and include events such as review of the EMR, possible ordering of blood tests, like creatinine, and placement of the intravenous catheter. These are not events recognized by RIS or PACS, but are critical elements of efficient workflow.
There are early discussions with the Integrating the Healthcare Enterprise (http://IHE.net), to propose at least some of event exchange as an IHE profile. Just as adoption of DICOM and HL7 was accelerated when IHE developed its profiles for preferred implementations, we anticipate that having preferred implementations for interchanging workflow event information will promote the adoption of business analytics and workflow management systems in imaging departments. This has also been submitted for inclusion within the RadLEX (http://radlex.org) lexicon.
Finally, a lexicon is only the start of a journey for using technology to improve workflow. Once workflow data is collected across a variety of practices, it should be able to identify optimal pathways for specific types of practices, patients, and examinations. It might be possible to leverage technologies like workflow engines to help implement and “enforce” those optimal pathways by automating steps that don’t require human input, and guiding humans to execute the proper steps. Workflow engines could monitor the status of devices and improve efficiency by maximizing utilization, and improve communications between imaging personnel. Workflow engines are heavily used in some industries where the steps are well documented, and we could likely benefit from that experience.
Conclusions
The adoption of a lexicon for workflow in imaging departments should improve the quality of information available to people managing imaging departments. The advantages include: improve the ability to compare practices and identify inefficient workflows and adjust them to improve efficiency; enable technologies to automate those steps that should not require manual intervention; and improve communication and documentation for those steps that require the human touch. The SWIM project has taken an important first step in defining a workflow lexicon that must now be validated for clinical practices, and implemented in commercial products.
References
- 1.Koster J, Rahmann S: Snakemake—a scalable bioinformatics workflow engine. Bioinformatics, 2012. doi:10.1093/bioinformatics/bts480 [DOI] [PubMed]
- 2.Microsoft Corporation: Cancer Center saves time and money, improves care with medical record solution. Retrieved Aug 27, 2012, 2012, from http://www.microsoft.com/casestudies/Case_Study_Detail.aspx?CaseStudyID=4000000916, 2007