Summary
The purpose of this study is to evaluate the mid or long-term angiographical stability of Guglielmi Detachable Coils (GDC) after embolization for cerebral aneurysms.
Between march 1997 and november 2001,164 aneurysms, including 116 ruptured and 48 unruptured aneurysms, were treated using GDC at Mito National Hospital. Cerebral angiograms over one month after embolization were obtained in 111 aneurysms, including 71 ruptured and 40 unruptured aneurysms. At the time of initial GDC embolization of the 71 ruptured aneurysms, complete occlusion was achieved in 31 aneurysms, neck remnant in 18 aneurysms, and body filling in 22 aneurysms. Morphological changes were observed in 26 aneurysms (37% in follow-up. Progressive thrombosis was obtained in 12 out of 71 aneurysms, no changes were shown in 45, and recanalizations occurred in 14. In the initial embolization of the 40 unruptured aneurysms, complete occlusion was achieved in 15 aneurysms, neck remnant in five and body filling in 20 aneurysms respectively. Morphological changes were observed in 12 aneurysms (30%), in which 12 aneurysms showed progressive thrombosis and 28 aneurysms were unchanged.
There were significant differences of the long-term angio graphical stability between ruptured and unruptured aneurysms. Rigorous follow-up angiography is mandatory when complete aneurysm occlusion is not achieved in ruptured aneurysms.
Key words: angiography, cerebral aneurysm, follow-up, Guglielmi detachable coil
Introduction
Guglielmi Detachable Coils (GDC) embolization has become a popular alternative for the treatment of cerebral aneurysms 5,8. The GDC system was clinically introduced in Japan in 1997. GDC embolization was selected as the first choice of treatment for cerebral aneurysms in our institution. However, the long-term stability of GDC in the cerebral aneurysm is still unknown2,4,6. The purpose of this study is to evaluate mid or long-term angiographical results.
Material and Methods
Between march 1997 and november 2001, 164 aneurysms, including 116 ruptured and 48 unruptured aneurysms, were treated with GDC in Mito National Hospital. Patients were scheduled for follow-up angiogram at 1 to three months after the initial treatment. Cerebral angiograms were obtained in 111 aneurysms, including 71 (61%) ruptured and 40 (83%) unruptured aneurysms. In the other 53 aneurysms,follow-up cerebral angiograms were not carried out due to poor medical conditions, death, or transfer to other hospitals.
The state of aneurysmal obliteration was evaluated using follow-up angiography in multiple projection.
The angiographic results of the treatment were categorized as follows: complete occlusion; CO (no contrast filling of the dome, body, or neck of the aneurysm), neck remnant; NR (some contrast filling into the part of the neck of the aneurysm), and body filling; BF (some contrast filling the dome).
Results
Location and Size of Aneurysm
Locations of 111 aneurysms, including 71 ruptured and 40 unruptured aneurysms are listed in table 1. The most common location of ruptured aneurysms was at the anterior communicating artery (ACoA) in 28 aneurysms (39%), followed by the internal carotid artery (ICA) in 21 aneurysms (30%), the middle cerebral artery (MCA) in nine aneurysms (13%), and the vertebro-basilar artery (V-BA) in seven aneurysms (10%).
Table 1.
Location of aneurysms
| Aneurysm Location | No. of ruptured aneurysms (%) | No. of unruptured aneurysms (%) |
|---|---|---|
| ICA | 21 (30) | 19 (47) |
| OphtA segment | 5 (7) | 11 (27) |
| PCoA, AChoA segment | 16 (23) | 8 (20) |
| ACoA | 28 (39) | 4 (10) |
| MCA | 9 (13) | 6 (15) |
| V-BA | 7 (10) | 8 (20) |
| Others | 6 (8) | 3 (8) |
| Total | 71 | 40 |
|
ICA = internal carotid artery, OphtA = ophtalmic artery, PCoA = posterior communicating artery, ACoA = anterior communicating artery, MCA = middle cerebral artery, V-BA = vertebro-basilar artery. | ||
The most common location of unruptured aneurysms was at the ICA in 19 aneurysms (47%), the V-BA in eight aneurysms (20%) and the MCA in six aneurysms (15%).
Concerning the size in all aneurysms, 104 aneurysms (94%) were small (3-10 mm in the largest diameter) and seven (6%) were large (11-25 mm).
Angiographic Results of Ruptured Aneurysm in Follow-up
In the initial embolization for the 71 ruptured aneurysms, CO was achieved in 31 aneurysms, NR in 18 aneurysms, and BF in 22 aneurysms. Morphological changes of aneurysms were observed in 26 (37%). Progressive thrombosis was obtained in 12 of 71 aneurysms, no changes were shown in 45, and recanalizations were shown in 14.
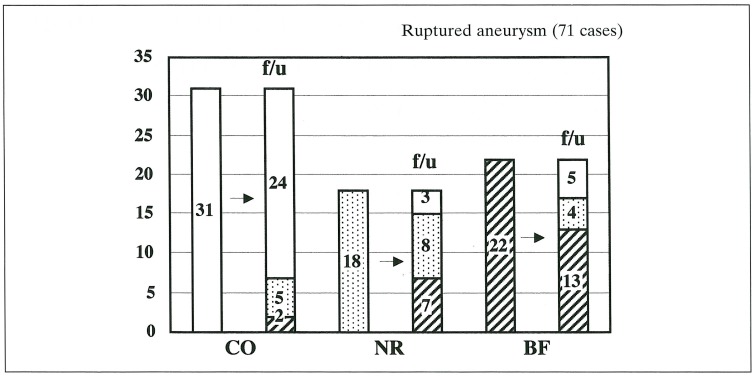
In ruptured aneurysms, CO on initial treatment was achieved in 31, no changes in 24, and seven of them displayed recanalization to NR or BF. In 18 aneurysms of NR on initial treatment, three aneurysms showed progressive thrombosis to CO, no changes in eight, recanalization to BF in seven. In 22 aneurysms of BF on initial treatment, progressive thrombosis to CO or NR were observed in nine, and no changes in 13 (figure 1).
Figure 1.
Angiographic results of ruptured aneurysm in follow-up.
Angiographic Results of Unruptured Aneurysm in Follow-up
In the initial embolization for the 40 unruptured aneurysms, CO was achieved in 15 aneurysms, NR in five aneurysms, and BF in 20 aneurysms. Morphological changes of aneurysms were observed in 12 cases (30%). Progressive thrombosis were obtained in 12 out of 40 aneurysms, no changes were shown in 28.
In unruptured aneurysms, CO on initial treatment was achieved in 15, all of them were unchanged. In five aneurysms of NR on initial treatment, two aneurysms showed progressive thrombosis to CO, and no changes in three. In 20 aneurysms of BF on initial treatment, ten aneurysms showed progressive thrombosis to CO or NR, and no changes in ten (figure 2).
Figure 2.
Angiographic results of unruptured aneurysm in follow-up.
Clinical Follow-up Result
In the 71 ruptured aneurysms, no changes in 45, and recanalization in 14 on follow-up angiogram. Additional treatment was carried out for 16 aneurysms, including re-embolization for 14 aneurysms and clipping for 2 aneurysms. Rerupture occurred in one aneurysm in chronic stage. In this situation, clipping was performed.
In the 40 unruptured aneurysms, no changes were notedin 28. No additional treatment was required, and aneurysm rupture was not observed in the following period.
Discussion
Recent technical developments in the GDC system have led to improved angiographical and clinical outcomes. The endovascular treatment of ruptured cerebral aneurysms using GDC has produced encouraging results in preventing rebleeding in the acute phase of subarachnoid haemorrhage5,8. On the other hand, the long-term outcome of GDC treatment is still unknown.
In this study, there were significant differences of the long-term angiographic stability between ruptured and unruptured aneurysms. If the satisfactory embolization of ruptured aneurysms was not achieved in the acute stage, the recanalization of the aneurysms was frequently observed. On the other hand, although partial embolization was achieved in unruptured aneurysm, progressive thrombosis was sometimes observed.
Recanalization or progressive thrombosis in aneurysms is influenced by many factors. The recanalization of aneurysms is strongly influenced by morphological factors, size, location, the volume embolization ratio, and so on 2,3. These many factors may play an important role in the angiographic changes in the chronic stage. In ruptured aneurysms, the morphology of a rupture point is unstable, so the tight packing of GDC is dangerous and difficult. In such cases, we recommend partial embolization of the aneurysms to prevent the rebleeding from aneurysms with additional treatment in the chronic stage to follow.
The treatment of aneurysms with GDCs appears to be effective in small aneurysms with a small neck. However, the angiographic result in the case of wide neck, large, or giant aneurysms is not satisfactory. Bavinzsky et Al suggested that endothelialization of the aneurysm orifice following placement of GDCs can occur, but it appears to be the exception rather than the rule 1. These clinical and pathological findings disclose the technological limitations of the current platinum GDC system. Bioabsorbable polymeric coils or concepts of bioactive coils have been published 7. Such new technology may improve the long-term stability of aneurysmal obliteration.
Conclusions
here were significant differences in long-term angiographic stability between ruptured and unruptured aneurysms. Rigorous follow-up angiography is mandatory when complete aneurysm occlusion is not achieved in ruptured aneurysms in the acute stage. Further technological and biological developments of the GDC system will improve the present angiographical and clinical outcome.
Abbreviations used in this paper:
ACoA = anterior communicating artery, PCoA = posterior communicating artery, AChoA = anterior choroidal artery, OphtA = ophtalmic artery, ICA = internal carotid artery, MCA = middle cerebral artery, V-BA = vertebro-basilar artery, GDC = Guglielmi Detachable Coil, CO = complete occlusion, NR = neck remnant, BF = body filling.
References
- 1.Bavinzski G, Talazoglu V, et al. Gross and microscopic histopathological findings in aneurysms of the human brain treated with Guglielmi detachable coils. J Neurosurg. 1999;91:284–293. doi: 10.3171/jns.1999.91.2.0284. [DOI] [PubMed] [Google Scholar]
- 2.Hayakawa M, Murayama Y, et al. Natural history of the neck remnant of a cerebral aneurysm treated with the Guglielmi detachable coil system. J Neurosurg. 2000;93:561–568. doi: 10.3171/jns.2000.93.4.0561. [DOI] [PubMed] [Google Scholar]
- 3.Kawanabe Y, Sadato A, et al. Endovascular occlusion of intracranial aneurysms with Guglielmi detachable coils: Correlation between coil packing density and coil compaction. Acta Neurochir - Wien. 2001;143:451–455. doi: 10.1007/s007010170073. [DOI] [PubMed] [Google Scholar]
- 4.Malish TW, Guglielmi G, et al. Intracranial aneurysms treated with the Guglielmi detachable coil: Midterm clinical results in a consecutive series of 100 patients. J Neurosurg. 1997;87:176–183. doi: 10.3171/jns.1997.87.2.0176. [DOI] [PubMed] [Google Scholar]
- 5.Matsumaru Y, Sonobe M, et al. Embolization of ruptured cerebral aneurysms with Guglielmi detachable coils. Surgery for Cerebral. Stroke - Japan. 2000;28:207–212. [Google Scholar]
- 6.Murayama Y, Viñuela F, et al. Embolization of incidental cerebral aneurysms by using the Guglielmi detachable coil system. J Neurosurg. 1999;90:207–214. doi: 10.3171/jns.1999.90.2.0207. [DOI] [PubMed] [Google Scholar]
- 7.Murayama Y, Viñuela F, et al. Bioabsorbable polymeric material coils for embolization of intracranial aneurysms: a preliminary experimental study. J Neurosurg. 2001;94:454–463. doi: 10.3171/jns.2001.94.3.0454. [DOI] [PubMed] [Google Scholar]
- 8.Viñuela F, Duckwiler GR, Mawad M. Guglielmi detachable coil embolization of acute intracranial aneurysm: perioperative anatomical and clinical outcome in 403 patients. J Neurosurg. 1997;86:475–482. doi: 10.3171/jns.1997.86.3.0475. [DOI] [PubMed] [Google Scholar]