INTRODUCTION
Up to 30% of people with type 2 diabetes remain undiagnosed in the UK on average for 7 years, and complications are already present at diagnosis in about 50% of people.1,2 Furthermore, impaired glucose regulation or ‘high risk of diabetes’ (prediabetes, impaired glucose tolerance, and.or impaired fasting glucose)1,2 is highly prevalent, at around 15% in adults, and carries an increased risk of progression to type 2 diabetes and vascular complications. Early initiation of lifestyle and therapeutic measures significantly reduces long-term complications of diabetes. Furthermore, intensive lifestyle intervention and/or pharmacotherapy reduce progression to diabetes by 40.60% in individuals at high risk of diabetes. Accurate diagnosis of diabetes and routine screening to identify high-risk individuals is important to improve outcomes. Availability of a simple, accessible, and reliable diagnostic test is crucial.
LIMITATIONS OF CONVENTIONAL GLUCOSE-BASED DIAGNOSTIC TESTS
Diagnosis of diabetes has been traditionally based on plasma glucose measurements.3 The fasting plasma glucose (FPG) test is more commonly used on pragmatic grounds but still involves overnight fasting and has modest sensitivity for detecting diabetes compared to the oral glucose tolerance test (OGTT).4 In contrast, the OGTT is sometimes considered as the ‘gold standard’ test but has poor test reproducibility and is inconvenient and costly.4 Furthermore glucose measurement can be affected by factors such as instability of glucose in blood samples at room temperature and fluctuations in glucose levels during periods of illness.4 Measured glucose levels therefore may not always accurately reflect true blood glycaemia.
THE NEW HbA1c CRITERIA FOR DIAGNOSIS OF DIABETES
In 2011, the World Health Organization (WHO) recommended the use of glycated haemoglobin (HbA1c) as an alternative diagnostic test suggesting an HbA1c level of ≥6.5% (≥48 mmol/mol) as a cut-off for diagnosing type 2 diabetes in non-pregnant adults.5 Although in 2009 an international expert committee advocated that levels of HbA1c between 6.0 and 6.4% (42–47 mmol/ mol) denote high risk of diabetes, the WHO in 2011 did not recommend HbA1c in diagnosing high-risk individuals.4,5 Using HbA1c for diagnosis requires the International Federation of Clinical Chemistry (IFCC) standardised assays for its measurement to ensure the results produced using different assays are equivalent and reliable.
Advantages over the glucose-based tests
HbA1c reflects average glucose levels over the preceding 6–8 week periods and is a better indicator of chronic hyperglycaemia and long-term complications.6 The HbA1c levels are less affected by any short-term, stress-related changes. Measurement of HbA1c is standardised and shows less intraindividual and inter-test variability. An HbA1c test can be performed in a non-fasting state, at any time of the day, and therefore may be more convenient for both healthcare professionals and patients.
HOW TO USE THE NEW HbA1c CRITERIA
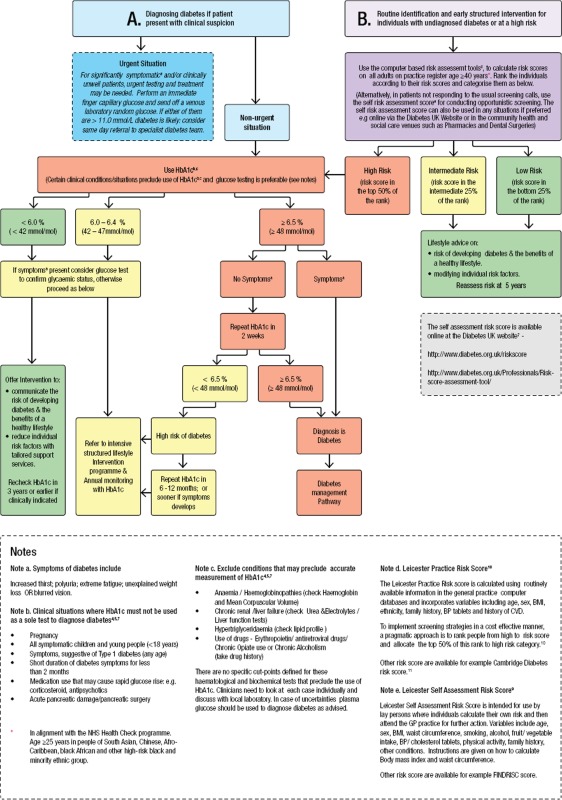
Here we provide algorithms giving practical stepwise advice on interpretation of HbA1c results and further care that partly incorporate UK guidelines published recently7,8 (Appendix 1). The algorithms are for use mainly in the setting of clinical practice in UK.
Algorithm A should be followed when an individual presents with suspected diabetes. In someone with symptoms of diabetes, HbA1c ≥6.5% (≥48 mmol/mol) on a single occasion confirms diagnosis of diabetes. In the absence of symptoms, the HbA1c test should be repeated in 2 weeks to rule out laboratory errors with diagnosis confirmed if repeat HbA1c is also ≥6.5% (≥48 mmol/mol).
Algorithm B should be used while considering routine identification of individuals with undiagnosed diabetes or those at high risk. The National Institute for Health and Clinical Excellence (NICE) recommends risk identification for all non-pregnant adults aged ≥40 years, nonpregnant adults of South Asian and Chinese descent aged 25–39 years, and adults with conditions that increase the risk of type 2 diabetes, using a two.step, targeted screening strategy.8 The strategy involves initial risk stratification using validated diabetes risk assessment tools followed by either the HbA1c or FPG test.8–11 However the HbA1c test alone can be used after the initial risk assessment. HbA1c is a strong predictor of risk of developing diabetes and cardiovascular events, independent of FPG.6 Moreover inconvenience of performing an FPG test can affect the screening uptake.12
PRACTICAL ISSUES IN USING THE HbA1c CRITERIA
HbA1c test may not diagnose the same individuals as the glucose-based tests.13 However the criteria for diagnosing diabetes relates to prediction of the risk of microvascular disease, in particular diabetes-specific retinopathy. In that regard HbA1c performs at least as well as fasting and 2-hour plasma glucose.14 Confirmation of diabetes using glucose tests is therefore only needed when HbA1c is <6.5% (<48 mmol/mol) but a strong clinical suspicion of diabetes remains. Certain clinical conditions preclude use of HbA1c for diagnostic purpose and warrants use of glucose tests (Appendix 1).
In the following clinical situations HbA1c must not be used to diagnose diabetes:4,5,7
pregnancy
all symptomatic children and young people (aged <18 years);
symptoms suggestive of type 1 diabetes (any age);
short duration of diabetes symptoms for <2 months;
medication use that may cause rapid glucose rise: for example, corticosteroid, antipsychotics; and
acute pancreatic damage/pancreatic surgery.
Furthermore the following conditions may preclude accurate measurement of HbA1c:4,5,7
anaemia/haemoglobinopathies (check haemoglobin and mean corpuscular volume);
chronic renal/liver failure (check urea and electrolytes/liver function tests);
hypertriglyceridaemia (check lipid profile); and
use of drugs: erythropoietin/antiretroviral drugs/chronic opiate use, or chronic alcoholism (take drug history).
There are no specific cut-points defined for the above-mentioned haematological and biochemical tests that preclude the use of HbA1c in these conditions. Clinicians need to look at each case individually and discuss with the local laboratory. In case of uncertainties plasma glucose should be used to diagnose diabetes.
Finally it is important that HbA1c is measured on a venous blood sample in the laboratory; point-of-care assays (near testing machines) may not be accurate and should be avoided for diagnostic purpose.15
CONCLUSIONS
The traditional glucose-based tests for diagnosis of type 2 diabetes have shortcomings including inconvenience of fasting, limited sensitivity, and poor test reproducibility. In comparison, an HbA1c test is simple, convenient, and reliable. Use of HbA1c as the preferred diagnostic test may improve early and accurate diagnosis of type 2 diabetes and high-risk individuals. It is crucial that clinicians remain aware of some of the limitations and practical issues in using the HbA1c-based diagnostic criteria.
Appendix 1. Algorithm for using HbA1c in diagnosing diabetes or identifying people at high risk of diabetes.
Provenance
Freely submitted; not externally peer reviewed.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Diabetes UK. State of diabetes care in the UK 2009. London: Diabetes UK; 2010. [Google Scholar]
- 2.Diabetes UK. Prediabetes: preventing the type 2 diabetes epidemic. A report. 2009. http://www.diabetes.org.uk/Documents/Reports/PrediabetesPreventingtheType2diabetesepidemicOct2009report.pdf (accessed 11 Jan 2013)
- 3.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabetic Med. 1998;15(7):539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 4.The International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care. 2009;32(7):1327–1334. doi: 10.2337/dc09-9033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus. Abbreviated report of a WHO consultation. Geneva: WHO; 2011. pp. 1–25. [PubMed] [Google Scholar]
- 6.Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362(9):800–811. doi: 10.1056/NEJMoa0908359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.John WG, Hillson R, Alberti SG. Use of haemoglobin A1c (HbA1c) in the diagnosis of diabetes mellitus. The implementation of World Health Organisation (WHO) guidance 2011. Practical Diabetes. 2012;29:12–12a. doi: 10.1111/j.1464-5491.2012.03762.x. [DOI] [PubMed] [Google Scholar]
- 8.National Institute for Health and Clinical Excellence. Preventing type 2 diabetes — risk identification and interventions for individuals at high risk. Public Health Guidance 38. London: NICE; 2012. http://www.nice.org.uk/guidance/ph38 (accessed 11 Jan 2013) [Google Scholar]
- 9.Gray LJ, Taub NA, Khunti K, et al. The Leicester Risk Assessment score for detecting undiagnosed type 2 diabetes and impaired glucose regulation for use in a multiethnic UK setting. Diabetic Med. 2010;27(8):887–895. doi: 10.1111/j.1464-5491.2010.03037.x. [DOI] [PubMed] [Google Scholar]
- 10.Gray L, Davies M, Hiles S, et al. Detection of impaired glucose regulation and/or type 2 diabetes mellitus, using primary care electronic data, in a multiethnic UK community setting. Diabetologia. 2012;55(4):959–966. doi: 10.1007/s00125-011-2432-x. [DOI] [PubMed] [Google Scholar]
- 11.Griffin SJ, Little PS, Hales CN, et al. Diabetes risk score: towards earlier detection of type 2 diabetes in general practice. Diabetes Metab Res Rev. 2000;16(3):164–171. doi: 10.1002/1520-7560(200005/06)16:3<164::aid-dmrr103>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 12.Eborall H, Stone M, Aujla N, et al. Influences on the uptake of diabetes screening: a qualitative study in primary care. Br J Gen Pract. 2012 doi: 10.3399/bjgp12X630106. DOI: 10.3399/bjgp12X630106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mostafa SA, Davies MJ, Webb D, et al. The potential impact of using glycated haemoglobin as the preferred diagnostic tool for detecting Type 2 diabetes mellitus. Diabetic Med. 2010;27(7):762–769. doi: 10.1111/j.1464-5491.2010.03015.x. [DOI] [PubMed] [Google Scholar]
- 14.Colagiuri S, Lee CMY, Wong TY, et al. Glycemic thresholds for diabetes-specific retinopathy. Diabetes Care. 2011;34(1):145–150. doi: 10.2337/dc10-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Ansary L, Farmer A, Hirst J, et al. Point-of-care testing for HbA1c in the management of diabetes: a systematic review and metaanalysis. Clin Chem. 2011;57(4):568–576. doi: 10.1373/clinchem.2010.157586. [DOI] [PubMed] [Google Scholar]