Otorrhoea is a common ear, nose, and throat (ENT) symptom, that requires accurate assessment. This article describes the most important causes of a discharging ear and the features that distinguish them to achieve better diagnosis and management.
OTITIS EXTERNA
Otitis externa is an inflammation of the external auditory canal, characterised by erythema and oedema. It has a 12-month period prevalence of 1.3% in females and 1.2% in males.1 Patients typically present with otalgia and an infected discharge. However, there is generally no change in hearing unless the entire canal is obstructed. Movement of the tragus results in significant discomfort. On otoscopy the canal appears narrowed and inflamed, with infected squamous debris lining the walls. Initial treatment centres around the administration of topical medications and, to minimise further irritation, patients should be advised not to poke anything into the ears or get them wet. They should also avoid swimming and getting their head wet. If there is a chance that the ears may get splashed, cotton wool coated with Vaseline® can be used as an ear plug.
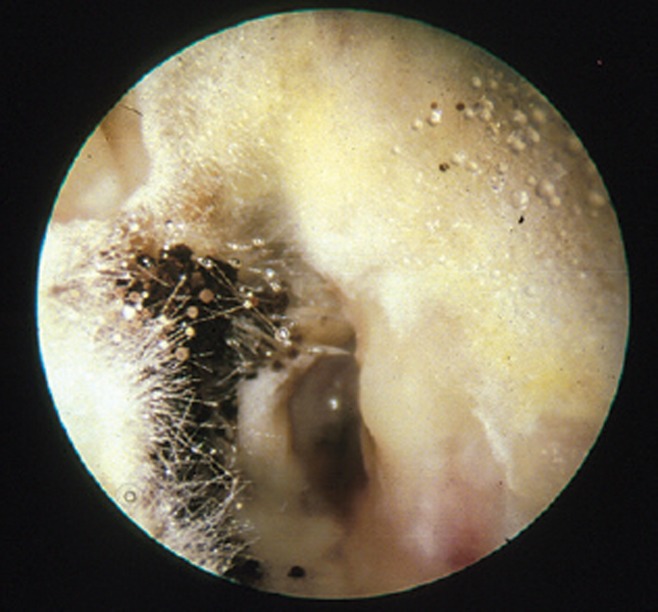
Topical preparations containing an antimicrobial with a steroid are an effective treatment, and in general there is no difference between the various types of preparation.2 However, choice is important if a fungal infection is suspected, on the basis of severe pruritus and hyphae within the external canal. Take a swab for culture and sensitivity, and use a preparation such as Locorten-Vioform®, which treats both bacterial and fungal infections. Provided there is neither systemic infection nor serious underlying disease, there is no need for systemic antibiotics.3
If symptoms do not improve an ENT referral for aural microsuction is appropriate.4 Patients with severe pain may require admission. External ear infection can spread, either as a cellulitis or perichondritis of the outer ear, or to the skull base, causing a condition known as necrotising otitis externa. Both conditions require urgent systemic antibiotics to control the spread of infection. Urgent ENT referral is also needed if a patient with otitis externa has a cranial nerve palsy (indicating potential bone involvement), granulations within the auditory canal, erythema and swelling of the pinna, or where there are worsening symptoms in a vulnerable (for example, a person with diabetes), or immunocompromised patient.
Fungal otitis externa (aspergillus niger)
OTITIS MEDIA
Otitis media (OM) is most common in children, and has an incidence of 11.5% among those in their first year of life.5 It will not cause otorrhoea unless there is a perforation of the tympanic membrane. A history of reduced hearing with pain that is relieved suddenly and followed by otorrhoea is suggestive of acute otitis media; examination will reveal a normal external auditory canal, with signs of perforation of the tympanic membrane and discharge. The otorrhoea tends to be mucopurulent, and can also be blood-stained. Typically otitis media resolves spontaneously within 24 hours. Systemic antibiotics only result in a slight reduction in ongoing symptoms; they are of most benefit for cases of bilateral otitis media in children aged <2 years, and in those with otorrhoea.6 Those older than 2 years without severe illness can be observed for 48–72 hours, with the option of prescribing antibiotics at this later date if their symptoms have not resolved.7 Up until that point the mainstay of treatment is analgesia. Alternatively, providing delayed prescriptions, for use if required 48 hours after the initial assessment, also reduces the use of antibiotics.8 If the patient is systemically well and their only symptom is discharge through a perforation, then consider using topical instead of systemic antibiotics. ENT-UK, the British association for otorhinolaryngologists, advise that aminoglycoside drops can be used in the presence of a perforation for a maximum of 2 weeks provided there is an obvious infection.9 This is because pus in the middle ear is in itself ototoxic. The justification should be explained to the patient and baseline audiometry performed if practical. Alternative drops such as ofloxacin (prescribed as eye drops for use in the ear) could also be used, however this is an unlicensed use in the UK. Persisting otalgia despite antibiotic therapy can be a symptom of subacute mastoiditis, therefore a specialist review is necessary as this condition requires intravenous antibiotics to prevent the development of osteomyelitis and abscess formation.
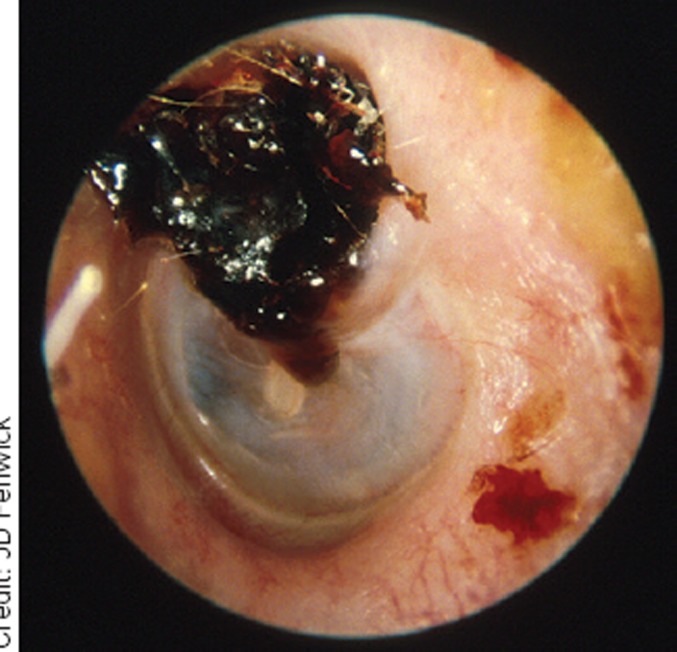
Attic cholesteatoma
A rare complication of otitis media is the development of chronic suppurative otitis media, characterised by chronic otorrhoea with a tympanic membrane perforation. Topical quinolone antibiotics are the most effective at clearing the discharge,10 however if it persists after 2 weeks the patient should be referred to ENT where microsuction, oral antibiotics, and surgical options can be considered.
GROMMET ASSOCIATED DISCHARGE
Grommet insertion is commonly complicated by postoperative discharge. It can be due to either concurrent acute otitis media or a foreign body-associated infection. Generally the management consists of topical antibiotic with steroid drops and microsuction, however there is little evidence to establish what is the most effective treatment.11
CHOLESTEATOMA
Cholesteatoma results from the build up of keratin within the middle ear that can subsequently become infected, as well as eroding through neighbouring structures such as the ossicular chain. Patients with this condition typically present with a scanty, foul smelling otorrhoea and hearing loss. On examination there may be dried discharge in the external auditory canal and crusting over the attic of the tympanic membrane. The appearance of wax deep within the ear, in close association with the drum, should raise the suspicion of cholesteatoma, as it is not normal to see it in this location. Patients with cholesteatoma may also present with facial nerve palsies, vertigo, or nystagmus.
On otoscopy the appearances can be similar to those of otitis externa. In a patient thought to have otitis externa that is not resolving, cholesteatoma should be considered as an alternative diagnosis. The management of this condition is surgical, with the aim being to remove the offending tissue. Suspected cholesteatoma requires urgent outpatient assessment.
CEREBROSPINAL FLUID OTORRHOEA
Cerebrospinal fluid (CSF) otorrhoea is rare and is generally preceded by a clear history of trauma. Patients may present with headache or either periorbital or post-auricular bruising, with bleeding or leakage of CSF from the ear. Urgent inpatient investigation is needed.
CONCLUSION
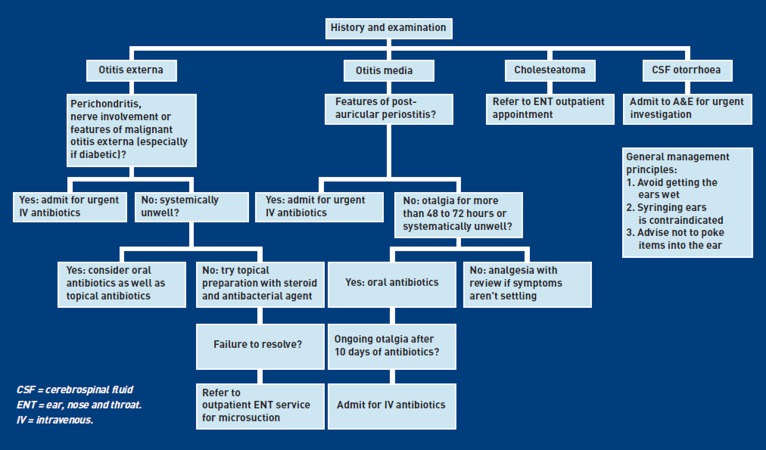
The history and nature of the discharge often establish the diagnosis, however enquiring about ongoing otalgia, hearing loss, vertigo, or trauma may reveal red-flag features and for similar reasons, as well as otoscopy, examination should include an assessment of the cranial nerves. Many of these patients can be managed in the community but it is important to be able to recognise the need for referral to secondary care (Figure 1).
Figure 1.
Flowchart for otorrhoea management
Provenance
Freely submitted; not externally peer reviewed.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Rowlands S, Devalia H, Smith C, et al. Otitis externa in UK general practice: a survey using the UK General Practice Research Database. Br J Gen Pract. 2001;51(468):533–538. [PMC free article] [PubMed] [Google Scholar]
- 2.Kaushik V, Malik T, Saeed SR. Interventions for acute otitis externa. Cochrane Database Syst Rev. 2010;(1):CD004740. doi: 10.1002/14651858.CD004740.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Hannley MT, Denneny JC, 3rd, Holzer SS. Use of ototopical antibiotics in treating 3 common ear diseases. Otolaryngol Head Neck Surg. 2000;122(6):934–940. doi: 10.1067/mhn.2000.107813. [DOI] [PubMed] [Google Scholar]
- 4.Gleeson MJ, Jones NS, Burton MJ, et al. Scott-Brown's otorhinolaryngology, head and neck surgery. 7th edn. Abingdon: CRC Press; 2008. [Google Scholar]
- 5.Ross AK, Croft PR, Collins M. Incidence of acute otitis media in infants in a general practice. J R Coll Gen Pract. 1988;38(307):70–72. [PMC free article] [PubMed] [Google Scholar]
- 6.Sanders S, Glasziou PP, Del Mar CB, Rovers MM. Antibiotics for acute otitis media in children. Cochrane Database Syst Rev. 2004;(1):CD000219. doi: 10.1002/14651858.CD000219.pub2. [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004;113(5):1451–1465. doi: 10.1542/peds.113.5.1451. [DOI] [PubMed] [Google Scholar]
- 8.Spiro DM, Tay K, Arnold DH, et al. Wait-and-see prescription for the treatment of acute otitis media: a randomized controlled trial. JAMA. 2006;296(10):1235–1241. doi: 10.1001/jama.296.10.1235. [DOI] [PubMed] [Google Scholar]
- 9.Phillips JS, Yung MW, Burton MJ, Swan IR. Evidence review and ENT-UK consensus report for the use of aminoglycoside-containing ear drops in the presence of an open middle ear. Clin Otolaryngol. 2007;32(5):330–336. doi: 10.1111/j.1749-4486.2007.01532.x. [DOI] [PubMed] [Google Scholar]
- 10.Macfadyen CA, Acuin JM, Gamble CL. Systemic antibiotics versus topical treatments for chronically discharging ears with underlying eardrum perforations. Cochrane Database Syst Rev. 2006;(1):CD005608. doi: 10.1002/14651858.CD005608. [DOI] [PubMed] [Google Scholar]
- 11.Vaile L, Williamson T, Waddell A, Taylor GJ. Interventions for ear discharge associated with grommets (ventilation tubes). Cochrane Database Syst Rev. 2006;(2):CD001933. doi: 10.1002/14651858.CD001933.pub2. [DOI] [PubMed] [Google Scholar]