Abstract
Background
Inter-arm difference in blood pressure of >10 mmHg is associated with peripheral vascular disease, but it is unclear how much of the difference in sequential right and left arm blood pressure measurements might be due to a ‘white-coat’ effect.
Aim
To use ambulatory blood pressure monitoring (ABPM) to better understand the clinical significance of inter-arm differences in blood pressure.
Design and setting
Retrospective study in a teaching hospital in Birmingham.
Method
Anonymised clinical data collected from 784 patients attending a single hospital-based hypertension clinic were retrospectively analysed. Each participant had blood pressure measured sequentially in both arms, followed by ABPM over the subsequent 24 hours.
Result
Data were available for 710 (91%) patients, of whom 39.3% (279) had a blood pressure difference of 10 mmHg or more between each arm. Compared to daytime systolic ABPM, the difference was 25.1 mmHg using the arm with the highest reading, but only 15.5 mmHg if the lower reading was taken (mean difference 9.6 mmHg (95% confidence interval [CI] = 9.0 mmHg to 10.3 mmHg)). However, differences between mean right (20.7 mmHg) or left (19.9 mmHg) arm blood pressure and daytime systolic ABPM were very similar.
Conclusion
Compared with ABPM, use of the higher of the left and right arm readings measured sequentially appears to overestimate true mean blood pressure. As there is no significant difference in the extent of disparity with ABPM by left or right arm, this is unlikely to be due to arm dominance and may be due to the ‘white-coat’ effect reducing blood pressure on repeated measurement. Where a large inter-arm blood pressure difference is detected with sequential measurement, healthcare professionals should re-measure the blood pressure in the original arm.
Keywords: Ambulatory blood pressure, blood pressure monitoring, cardiovascular risk, white coat hypertension
INTRODUCTION
British Hypertension Society guidelines suggest that blood pressure should be measured in both arms.1 The latest guidelines advise clinicians to repeat the measurements if the systolic difference is >20 mmHg between the two arms and to measure subsequent blood pressures in the arm with the higher reading if the difference is confirmed.2 Most international guidelines since 1977 have offered similar advice but there is little evidence that this is followed.3 A questionnaire survey of GPs revealed that although 77% were aware that blood pressure should be measured in both arms, only 30% agreed with this recommendation (95% confidence interval [CI] = 26% to 34%), while over half (54%; 95% CI = 49% to 59%) disagreed, and a mere 13% (95% CI = 10% to 16%) adhered to it.4,5 The study authors suggested that this may be because guidelines often state that the measurements should be taken, but do not explain how or why.4
The prevalence of inter-arm blood pressure differences is uncertain. Reported studies vary in inclusion criteria (age of participants and presence or absence of hypertension), methodology (the device used [mercury or oscillometric]), and whether the readings were taken simultaneously, sequentially, or both.6 The result of this is a wide variation in reported prevalence.7 A recent systematic review highlights the need for repeated simultaneous measurements with automated devices if overestimation of inter-arm differences and observer bias are to be avoided, but such equipment is rarely available in a busy general practice.8 If strict inclusion criteria are applied, then around 1:5 have a systolic inter-arm difference of greater than 10 mmHg and 1:20 have a difference greater than 20 mmHg.6
It has been suggested that differences in right and left arm pressures may be caused by undiagnosed peripheral vascular disease affecting the vasculature of the upper limbs and may therefore predict an increased risk of cardiovascular disease.9 Recently, Clark et al reported that inter-arm differences in systolic blood pressure of ≥10 mmHg were associated with an increased risk of all-cause mortality (adjusted hazard ratio = 3.6; 95% CI = 2.0 to 6.5).10 In a study of patients with renal disease, every 10 mmHg difference in systolic blood pressure between arms conferred a 24% higher mortality hazard after adjusting for average systolic blood pressure and chronic kidney disease.11 A recent systematic review found that a difference of 10 mmHg or higher between arms was associated with peripheral vascular disease (risk ratio = 2.4; 95% CI = 1.5 to 3.9) and a difference of 15 mmHg or more was associated with peripheral vascular disease, pre-existing cerebrovascular disease, and increased cardiovascular mortality.12 It has thus been suggested that routine measurement of the inter-arm difference may provide a simple and effective screening method for the presence of vascular disease.9,12
How this fits in
An inter-arm difference in blood pressure of >10 mmHg is associated with increased risk of peripheral vascular disease. This study used ambulatory blood pressure monitoring to assess the clinical significance of the difference between sequential right and left arm blood pressure measurements, and consider whether part of the disparity might be due to a ‘white-coat’ effect. It was found that use of the higher of the left and right arm measurement, when undertaken sequentially, appears to overestimate true mean blood pressure compared to ambulatory blood pressure measurements. Where a large inter-arm blood pressure difference is detected by sequential measurement, healthcare professionals should re-measure the blood pressure in the original arm to confirm the difference.
Readings from ambulatory devices are generally accepted as the ‘gold standard’ of blood pressure measurement.2 Ambulatory blood pressure monitoring estimates ‘true’ mean blood pressure more accurately than clinic measurement, because multiple readings are taken, and it has been shown to have better correlation with a range of cardiovascular outcomes and end-organ damage.13–18 Ambulatory blood pressure monitoring (ABPM) is typically used where there is uncertainty in diagnosis, resistance to treatment, irregular or diurnal variation, or concerns about variability and ‘white-coat’ effect.19–21 A systematic review22 and modelling study23 found that using ambulatory monitoring as a diagnostic strategy for hypertension after an initial raised reading in the clinic would reduce misdiagnosis and save costs, and this is now recommended by the National Institute for Health and Clinical Excellence (NICE) for the routine diagnosis of hypertension.2
The relationship between inter-arm differences in blood pressure and mean daytime blood pressure measured by ABPM has not been reported previously. The aim of this study was to compare office blood pressure measured in either arm with mean daytime blood pressure measured by ABPM, to establish whether the relationship of ambulatory to single office readings was the same, regardless of which arm the office reading was taken on.
METHOD
Participants
Data were analysed from patients who attended the hypertension clinic at the Wellcome Trust Clinical Research Facility, University Hospital Birmingham over a 2-year period (May 2006 to June 2008). Patients had been referred mainly from primary care and included both those already taking antihypertensive medication and those on no treatment, with a new diagnosis of hypertension.
Procedure
All patients attended a pre-clinic appointment as part of routine clinical care and were assessed by a team of specially trained research nurses experienced in collecting clinical data. Following 5 minutes of rest, blood pressure was measured using a validated monitor (DINAMAP PRO20024) in one arm (either right or left, in no particular order) and in the opposite arm immediately afterwards. All measurements were recorded and kept in the clinical notes. A 24-hour monitor was then fitted (SpaceLabs, Model 9021725) to the non-dominant arm, unless the difference in systolic pressure was >20 mmHg and/or that of diastolic pressure was >10 mmHg, in which case the monitor was fitted to the arm with the higher reading, in line with standard practice in the clinic and NICE guidelines.2 The ABPM measured blood pressure at 30-minute intervals during the day (0700 to 2300) and hourly intervals overnight (2300 to 0700).
Analysis
Anonymised blood pressure data were extracted from the clinical records, along with age and sex, by a member of the clinical team. Only records including all completed readings were included in the analysis. The analysis compared blood pressure in either arm with mean daytime blood pressure from ambulatory readings. A modified Bland–Altman method (using mean ABPM as a ‘gold standard’ for blood pressure) was used to compare the difference between right or left arm blood pressure and mean daytime ABPM with mean daytime ABPM. Estimated differences at different blood pressure levels were derived from a linear regression of blood pressure on ABPM. As the relevant differences in blood pressure did not follow a normal distribution, bootstrap methods were employed to obtain confidence intervals and P-values for the t-test statistics used to compare blood pressure readings.
RESULTS
Results from 710 out of 784 patients were available for analysis. The remainder were excluded because of incomplete records. There were 391 females and 319 males aged (mean ± standard deviation) 53.8 ± 17.7 and 49.8 ± 14.5 years, respectively. Unmedicated, newly diagnosed patients (46%) were referred to the clinic to confirm the diagnosis of hypertension, to clarify whether any treatment was needed, to investigate the underlying cause if appropriate, and/or to exclude ‘white-coat’ hypertension. An additional 54% were on antihypertensive medication and were referred because of poor control despite treatment, drug intolerances, and/or investigation of underlying cause. Patient characteristics are shown in Table 1.
Table 1.
Risk factors for hypertension and cardiovascular disease and patient comorbidities
| Male (n = 319) | Female (n = 391) | Total (n = 710) | ||||
|---|---|---|---|---|---|---|
| Risk factor or comorbidity | n | % | n | % | n | % |
| Smoking | ||||||
| Non-smoker | 212 | 66.5 | 302 | 77.2 | 514 | 72.4 |
| Ex-smoker | ||||||
| < 5 years | 17 | 5.3 | 18 | 4.6 | 35 | 4.9 |
| ≥5 years | 29 | 9.1 | 12 | 3.1 | 41 | 5.8 |
| Current smoker | ||||||
| < 20 per day | 41 | 12.9 | 49 | 12.5 | 90 | 12.7 |
| ≥20 per day | 19 | 6.0 | 10 | 2.6 | 29 | 4.1 |
| Pipe | 1 | 0.3 | 0 | 0.0 | 1 | 0.1 |
| Alcohol consumption | ||||||
| None | 64 | 20.1 | 137 | 35.0 | 201 | 28.3 |
| ≤ recommended limitsa | 152 | 47.6 | 157 | 40.2 | 309 | 43.5 |
| >recommended limits | 62 | 19.4 | 30 | 7.7 | 92 | 13.0 |
| Unknown | 41 | 12.9 | 67 | 17.1 | 108 | 15.2 |
| Excess salt intake | ||||||
| Yes | 147 | 46.1 | 146 | 37.3 | 293 | 41.3 |
| No | 172 | 53.9 | 245 | 62.7 | 417 | 58.7 |
| Exercise level | ||||||
| < 5 × 30 minutes/week | 193 | 60.5 | 261 | 66.8 | 454 | 63.9 |
| >5 × 30 minutes/week | 126 | 39.5 | 130 | 33.2 | 256 | 36.1 |
| Body mass index (kg/m2) | ||||||
| Underweight (< 18.5) | 1 | 0.3 | 2 | 0.5 | 3 | 0.4 |
| Healthy (18.5–24.9) | 64 | 20.1 | 89 | 22.8 | 153 | 21.5 |
| Overweight (25–29.9) | 133 | 41.7 | 150 | 38.4 | 283 | 39.9 |
| Obese (>30) | 117 | 36.7 | 113 | 28.9 | 230 | 32.4 |
| Morbidly obese (>40) | 4 | 1.3 | 37 | 9.5 | 41 | 5.8 |
| Cholesterol:HDL ratio | ||||||
| < 4.5 | 233 | 73.0 | 322 | 82.4 | 555 | 78.2 |
| ≥4.5 | 84 | 26.3 | 68 | 17.4 | 152 | 21.4 |
| Unknown | 2 | 0.6 | 1 | 0.3 | 3 | 0.4 |
| Comorbidities | ||||||
| Type 1 diabetes mellitus | 6 | 1.9 | 2 | 0.5 | 8 | 1.1 |
| Type 2 diabetes mellitus | 23 | 7.2 | 41 | 10.5 | 64 | 9.0 |
| Ischaemic heart disease | 15 | 4.7 | 19 | 4.9 | 34 | 4.8 |
| Transient ischaemic attack/stroke | 9 | 2.8 | 14 | 3.6 | 23 | 3.2 |
| Renal disease | 11 | 3.4 | 10 | 2.6 | 21 | 3.0 |
| Other | 55 | 17.2 | 63 | 16.1 | 118 | 16.6 |
HDL = high-density lipoprotein.
Men up to 21 units per week, women up to 14 units per week.
Systolic blood pressure readings
Mean systolic blood pressure was similar in the right and left arms (161 mmHg versus 160 mmHg, t = 1.78, bootstrap P = 0.074, Table 2). In 279 patients (39.3%), there was a ≥10 mmHg systolic inter-arm difference, with the right arm having the higher reading most often (156/279 [56%] versus 123/279 [44%], Table 3).
Table 2.
Systolic and diastolic blood pressure in the left and right arms and compared to mean daytime pressure measured by ambulatory blood pressure monitor (n = 710)
| Variable | Mean | SE mean | SD | Median |
|---|---|---|---|---|
| Screening SBP and DBP in the left and right arms | ||||
| Right arm SBP | 161.0 | 0.9 | 22.8 | 158.0 |
| Left arm SBP | 160.1 | 0.9 | 23.6 | 157.0 |
| Right — left arm SBP | 0.9 | 0.5 | 12.9 | 1.0 |
| Right arm DBP | 88.7 | 0.5 | 12.9 | 88.0 |
| Left arm DBP | 88.0 | 0.5 | 12.7 | 87.5 |
| Right — left arm DBP | 0.7 | 0.3 | 8.8 | 3.0 |
| Highest and lowest SBP and DBP and right and left arm SBP and DBP versus mean daytime pressure measured by ABPM | ||||
| Higher SBP — daytime ABPM | 25.1 | 0.7 | 18.8 | 23.0 |
| Lower SBP — daytime ABPM | 15.5 | 0.7 | 18.1 | 13.0 |
| Right arm SBP — daytime ABPM | 20.7 | 0.7 | 18.8 | 19.0 |
| Left arm SBP — daytime ABPM | 19.9 | 0.7 | 19.4 | 18.0 |
| Higher DBP — daytime ABPM | 7.7 | 0.4 | 10.8 | 7.0 |
| Lower DBP — daytime ABPM | 1.2 | 0.4 | 10.0 | 1.0 |
| Right arm DBP — daytime ABPM | 4.8 | 0.4 | 11.1 | 4.0 |
| Left arm DBP — daytime ABPM | 4.1 | 0.4 | 10.7 | 3.0 |
ABPM = ambulatory blood pressure monitoring. DBP = diastolic blood pressure. SBP = systolic blood pressure. SD = standard deviation. SE = standard error.
Table 3.
Inter-arm systolic and diastolic blood pressure differences
| Blood pressure difference | Count, n = 710 | % |
|---|---|---|
| Left SBP > right SBP by ≥10 mmHg | 123 | 17.3 |
| < 10 mmHg difference between left and right SBP | 431 | 60.7 |
| Right SBP > left SBP by ≥10 mmHg | 156 | 22.0 |
| Left DBP > right DBP by ≥10 mmHg | 78 | 11.0 |
| < 10 mmHg difference between left and right DBP | 534 | 75.2 |
| Right DBP > left DBP by≥10 mmHg | 98 | 13.8 |
| Absolute systolic inter-arm difference (mmHg) | ||
| 0–4 | 222 | 31.3 |
| 5–9 | 209 | 29.4 |
| 10–19 | 197 | 27.7 |
| >20 | 82 | 11.6 |
| Total | 710 | 100.0 |
DBP = diastolic blood pressure. SBP = systolic blood pressure.
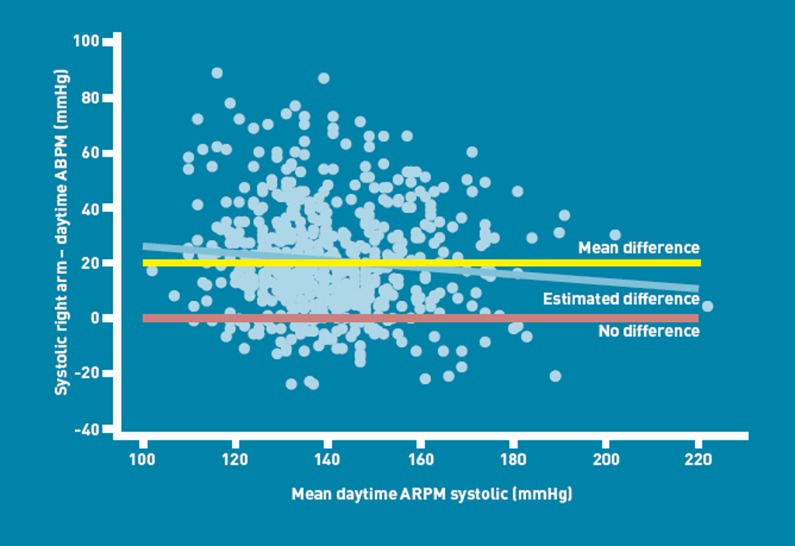
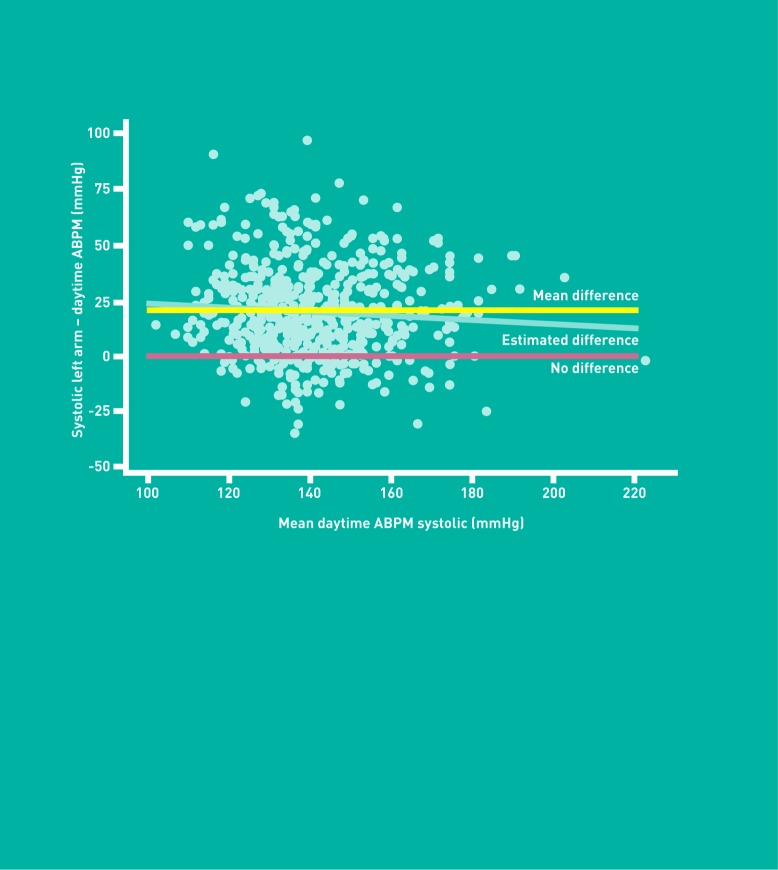
The difference between clinic systolic blood pressure and daytime mean ABPM was compared, using first the arm with the highest reading and then the arm with the lowest reading (Table 2). There was a mean 25.1 mmHg difference between the arm with the highest reading and daytime systolic ABPM, compared with 15.5 mmHg if the arm with the lowest reading was taken. Comparing the blood pressure from the right arm with daytime systolic ABPM found a 20.7 mmHg (bootstrap 95% CI = 19.4 mmHg to 22.0 mmHg) mean difference as opposed to 19.9 mmHg (bootstrap 95% CI = 18.5 mmHg to 21.3 mmHg) mean difference if the left was compared. The mean difference between the highest and lowest systolic blood pressure and associated bootstrap 95% CI was 9.6 mmHg (95% CI = 9.0 mmHg to 10.3 mmHg). There was no significant association between inter-arm difference in systolic pressure and daytime ABPM systolic pressure (P = 0.50).
Modified Bland–Altman plots (Figures 1 and 2) demonstrated that use of a single measurement from the right or left arm will overestimate the systolic blood pressure as determined by mean daytime ABPM pressure. The yellow line indicates the overall difference. However, there is a significant variation (P < 0.01) in difference with blood pressure level (blue line) in the right arm measurements, and a similar, but not quite significant, pattern (P = 0.06) in the left arm.
Figure 1.
Modified Bland-Altman plot of systolic blood pressure measured on the right arm minus mean daytime systolic ambulatory blood pressure versus mean daytime ABPM systolic blood pressure.
Figure 2.
Modified Bland-Altman plot of systolic blood pressure measured on the left arm minus mean daytime systolic ambulatory blood pressure versus mean daytime ABPM systolic blood pressure.
Diastolic blood pressure readings
Similar but smaller differences were seen for diastolic pressure (Tables 2 and 3).
Effect of age and sex on observed differences
There was no significant correlation between age and inter-arm difference in systolic or diastolic blood pressure (correlations 0.045 and 0.037, respectively). Similarly, there was no difference in right and left arm systolic or diastolic blood pressure between males and females (mean difference for systolic pressure [female—male] = 0.44 mmHg [95% CI = –2.32 mmHg to 1.44 mmHg], and for diastolic pressure = 0.01 mmHg [95% CI = –1.2 mmHg to 1.4 mmHg), P = 0.65 and 0.91 respectively; age-corrected P = 0.57 and 0.94).
Despite this, the differences between the clinic systolic blood pressure measurement (either left or right arm) and mean systolic daytime ABPM readings showed a positive correlation with age (correlations 0.340 and 0.308, respectively, P < 0.001). A similar relationship was demonstrated for diastolic measurements (0.245 and 0.204, P < 0.001). On average between the left and right arm, there was a 0.35 mmHg increase in the difference between clinic and mean daytime ABPM readings and a 0.13 mmHg increase for the corresponding diastolic measurements per year increase in age. There were no sex-related differences in these measurements once age had been accounted for.
DISCUSSION
Summary
This study confirms previous findings of significant inter-arm blood pressure difference in daily practice, particularly if a sequential method is used: almost 40% of the patients had a ≥10 mmHg difference between each arm, and the right arm was more likely to give a higher reading than the left. Given that most non-specialists are unlikely to have equipment for simultaneous measurement in both arms, these findings suggest that use of the arm with the higher initial reading to guide clinical decisions may significantly overestimate blood pressure, unless repeated measurements are made as suggested by the recent NICE guidelines.2 This was seen when the arm with the highest reading was compared with the mean daytime pressure calculated from the ABPM, and a 25 mmHg difference was observed. Readings from the arm with the lowest reading were much closer to the ABPM daytime means, particularly if the latter was adjusted upward as per British Hypertension Society guidelines.1 As there was no overall difference in the amount of variation in measurements from the right and left arms compared with ABPM readings, the most likely explanation is that the observed differences in sequential arm pressures are due to a ‘white-coat’ effect, with blood pressure dropping between sequential readings. The results also show that differences in clinic measurements and mean daytime ABPM readings become more pronounced with age.
Strengths and limitations
The key strength of this study was that it was done in a routine clinical setting using conventional monitoring techniques. The cohort of patients was large enough that estimates of the differences between methods can be precise. The sequential nature of the inter-arm measurements could be considered a weakness but this is likely to be the commonest method used in practice, particularly in primary care. It shows the likely outcome of implementation of current guidelines that do not carefully specify technique. The arm used for the first blood pressure measurement using the DINAMAP PRO200 was not randomised. This is potentially a source of bias but reflects the routine nature of this set of clinical data. Following standard procedure in the clinic at the time (and current NICE guideline recommendations), the study only ensured the higher-reading arm was used for ABPM measurement where there were inter-arm differences of 20/10 mmHg. Regarding setting, the study was undertaken in secondary care and so may not be generalisable to primary care, especially as the setting in which blood pressure is measured can itself impact on ‘white-coat’ effects. However, other than the age of participants, which was younger than a typical primary care population, the range of individuals included is likely to be similar to other populations undergoing ambulatory monitoring as part of the investigation or management of hypertension. Finally, no patients were excluded for comorbidities — in theory this means patients with atrial fibrillation (for whom the monitors would not be validated) could have been included, but this is unlikely based on the age profile of patients (Table 1).
Comparison with existing literature
It has been suggested that differences in right and left arm pressures may be caused by peripheral vascular disease affecting the vasculature of the upper limbs.9 There are, however, other non-structural reasons why a difference between arms might be detected. Many studies (including this one) used only a few readings to assess the inter-arm differences on a single occasion and the methods varied to include mercury sphygmomanometers and oscillometric devices.6 Some researchers used sequential measurements, while other investigators believed that readings taken simultaneously in the two arms would be more accurate. For example, Harrison et al showed that 26% of patients had a sequential difference of >10 mmHg, which reduced to 5.3% when simultaneous readings were taken with cuffs joined by a T-tube.26 Gould and coworkers used two cuffs and two observers and found no difference in blood pressure in either arm.27 A major problem is the spontaneous variability of blood pressure, which can produce spurious differences between the two arms if only a few readings are used.28 However, though the prevalence of an inter-arm difference of systolic pressure of 10 mmHg or more is approximately doubled when measuring sequentially, when using a manual instead of an automated device, or when performing only one blood pressure measurement instead of multiple ones,8 other studies indicate that prevalence may be 20% in general and hypertensive populations if the gold-standard method of repeated simultaneous measurements – or even a pragmatic sequential measurement protocol — is used.6
The findings in the current study are consistent with the clinical observations of Gosse, who noted that the main source of differences in readings between the two arms occurs when they are not recorded simultaneously.29 He proposed that in simultaneous measurement there is a lessening of the ‘white-coat’ effect, which usually makes the second reading lower than the first. O’Shea and Murphy determined the effects of routinely selecting the non-dominant arm for ABPM, to evaluate the practice of using manual blood pressure from one arm and ambulatory blood pressure from the other, for estimation of the ‘white-coat’ effect.30 They conducted an observational study in 10 volunteers exhibiting an inter-arm resting clinic systolic blood pressure difference of >10 mmHg. The supine referral clinic systolic blood pressure was 16 ± 6 mmHg higher in the right compared with the left arm but the average 24-hour ambulatory systolic blood pressure was only 6 ± 7 mmHg higher in the right arm (range + 17 to –3 mmHg), P = 0.025, with similar findings for measurements of diastolic blood pressure. The authors concluded that one-third of the ‘white-coat’ effect estimated by current practice could be attributed to inconsistency in the choice of arm for blood pressure measurement. These clinical observations are entirely in keeping with the findings of the present study, which clarifies the relationship of inter-arm differences and ambulatory readings.
In keeping with the study observations that differences in clinic measurements and mean daytime ABPM readings become more pronounced with age, Head et al recently derived age- and sex-related ambulatory blood pressure equivalents to clinic blood pressure thresholds and found that daytime systolic but not diastolic ambulatory blood pressure equivalents were affected by age.31 Ambulatory systolic equivalents were 2–4 mmHg lower in people aged 65 years or older than in individuals aged 25–44 years, when compared with clinic readings, which meant that the difference in clinic readings and ABPM readings became more pronounced with age. In addition, unlike the current study, systolic and diastolic ambulatory equivalents were 3/2 mmHg lower in females than for age-matched males. All measurements were taken by nurses and other non-medical staff as in the current study. When doctors took the measurements, the differences between clinic and ambulatory readings were more pronounced.31
The present study did not demonstrate a significant correlation between age and inter-arm difference in systolic or diastolic blood pressure. Previous studies have varied as to the influence of age on inter-arm blood pressure difference.32 It has been proposed that with advancing age there is loss of vascular elasticity, with a concomitant increase in arterial resistance to compression due to arteriosclerosis, which might account for bilateral differences in blood pressure. Furthermore, asymmetrical atheromatous narrowing of the subclavian or brachial arteries due to asymptomatic peripheral vascular disease would be expected to be more common with increasing age, leading to lower pressures distal to the narrowing.26,33 The findings in the present study, however, are more in keeping with a ‘white-coat’ effect, which is known to progressively increase with age.34,35
Implications for clinical practice
This study highlights the limitations of single clinic readings, which are not accurate when compared with ABPM or other forms of more prolonged monitoring. It reinforces the recent recommendations from NICE that blood pressure should be measured in both arms and should be repeated if the difference in readings between arms is more than 20 mmHg; if the difference remains on the second measurement, then subsequent blood pressures (including ambulatory readings) should be measured in the arm with the highest reading. It also suggests that apparent differences between right and left arm pressures may not necessarily reflect arterial disease,9 but may be due to a ‘white-coat’ effect. Of interest, there have been reports of higher cardiovascular disease event rates in patients with a ‘white-coat’ effect, which might partly explain the reduced cardiovascular event-free survival associated with significant inter-arm difference; a later meta-analysis of outcomes in ‘white-coat’ hypertension did not suggest any adverse cardiovascular association, however.34,36–38
This study therefore does not support routine single measurement of blood pressure in both arms if this is done sequentially, and suggests instead that a significant ‘white-coat’ effect is likely to ensue where such a practice is undertaken in a routine clinical setting. They would recommend that clinicians continue to measure blood pressure in both arms but that this is done simultaneously or, where this is not possible, that differences in right and left arm pressures are checked by repeated measurements in both arms. If a difference of >20 mmHg is found, then all blood pressure measurements, including ambulatory readings, should be taken on the arm with the higher readings.
Acknowledgments
The authors would like to acknowledge the nurses at the Wellcome Clinical Research Facility, Birmingham for undertaking the blood pressure measurements, and the patients, without whom this study would not have been possible. They would also like to acknowledge Megha Agarwal and Louise Beesley for their dedicated hard work extracting the data on population characteristics for Table 1.
Funding
This article presents independent research commissioned by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research funding scheme (RP-PG-0407-10347). The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. Richard McManus is supported by an NIHR Career Development Fellowship.
Ethical approval
This study used anonymised clinical data collected in routine practice and hence was categorised as service evaluation not requiring ethical approval.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Williams B, Poulter N, Brown M, et al. Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society. J Hum Hypertens. 2004;18(3):139–185. doi: 10.1038/sj.jhh.1001683. [DOI] [PubMed] [Google Scholar]
- 2.National Institute for Clinical Excellence. Hypertension: management of hypertension in adults in primary care. Clinical guideline 127. London: NICE; 2011. http://www.nice.org.uk/guidance/CG127/NICEGuidance (accessed 4 Dec 2012) [Google Scholar]
- 3.Parker E, Glasziou P. Use of evidence in hypertension guidelines: should we measure in both arms? Br J Gen Pract. 2009;59(560):e87–e92. doi: 10.3399/bjgp09X395012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heneghan C, Perera R, Mant D, Glasziou P. Hypertension guideline recommendations in general practice: awareness, agreement, adoption, and adherence. Br J Gen Pract. 2007;57(545):948–952. doi: 10.3399/096016407782604965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glasziou P. How much monitoring? Br J Gen Pract. 2007;57(538):350–351. [PMC free article] [PubMed] [Google Scholar]
- 6.Clark CE, Campbell JL, Evans PH, Millward A. Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic review. J Hum Hypertens. 2006;20(12):923–931. doi: 10.1038/sj.jhh.1002093. [DOI] [PubMed] [Google Scholar]
- 7.Clark CE. Difference in blood pressure between arms might reflect peripheral vascular disease. BMJ. 2001;323(7309):399–400. doi: 10.1136/bmj.323.7309.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verberk WJ, Kessels AG, Thien T. Blood pressure measurement method and inter-arm differences: a meta-analysis. Am J Hypertens. 2011;24(11):1201–1208. doi: 10.1038/ajh.2011.125. [DOI] [PubMed] [Google Scholar]
- 9.Clark CE, Campbell JL, Powell RJ, Thompson JF. The inter-arm blood pressure difference and peripheral vascular disease: cross-sectional study. Fam Pract. 2007;24(5):420–426. doi: 10.1093/fampra/cmm035. [DOI] [PubMed] [Google Scholar]
- 10.Clark CE, Taylor RS, Shore AC, Campbell JL. The difference in blood pressure readings between arms and survival: primary care cohort study. BMJ. 2012;344:e1327. doi: 10.1136/bmj.e1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Agarwal R, Bunaye Z, Bekele DM. Prognostic significance of between-arm blood pressure differences. Hypertension. 2008;51(3):657–662. doi: 10.1161/HYPERTENSIONAHA.107.104943. [DOI] [PubMed] [Google Scholar]
- 12.Clark CE, Taylor RS, Shore AC, et al. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet. 2012;379(9819):905–914. doi: 10.1016/S0140-6736(11)61710-8. [DOI] [PubMed] [Google Scholar]
- 13.Ohkubo T, Hozawa A, Nagai K, et al. Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens. 2000;18(7):847–854. doi: 10.1097/00004872-200018070-00005. [DOI] [PubMed] [Google Scholar]
- 14.Mancia G, Zanchetti A, Gabiti-Rosei E, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. SAMPLE Study Group. Study on Ambulatory Monitoring of Blood Pressure and Lisinopril Evaluation. Circulation. 1997;95(6):1464–1470. doi: 10.1161/01.cir.95.6.1464. [DOI] [PubMed] [Google Scholar]
- 15.Verdecchia P. Prognostic value of ambulatory blood pressure: current evidence and clinical implications. Hypertension. 2000;35(3):844–851. doi: 10.1161/01.hyp.35.3.844. [DOI] [PubMed] [Google Scholar]
- 16.Staessen JA, Thijs L, Fagard R, et al. Predicting cardiovascular risk using conventional vs. ambulatory blood pressure in older patients with systolic hypertension. Systolic Hypertension in Europe Trial Investigators. JAMA. 1999;282(6):539–546. doi: 10.1001/jama.282.6.539. [DOI] [PubMed] [Google Scholar]
- 17.Fagard RH, Staessen JA, Thijs L. Prediction of cardiac structure and function by repeated clinic and ambulatory blood pressure. Hypertension. 1997;29(1 Pt 1):22–29. doi: 10.1161/01.hyp.29.1.22. [DOI] [PubMed] [Google Scholar]
- 18.Imai Y, Ohkubo T, Sakuma M, et al. Predictive power of screening blood pressure, ambulatory blood pressure and blood pressure measured at home for overall and cardiovascular mortality: a prospective observation in a cohort from Ohasama, northern Japan. Blood Press Monit. 1996;1(3):251–254. [PubMed] [Google Scholar]
- 19.Whitworth JA. World Health Organization, International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21(11):1983–1992. doi: 10.1097/00004872-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Verdecchia P. Reference values for ambulatory blood pressure and self-measured blood pressure based on prospective outcome data. Blood Press Monit. 2001;6(6):323–327. doi: 10.1097/00126097-200112000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Redon J, Campos C, Naciso ML, et al. Prognostic value of ambulatory blood pressure monitoring in refractory hypertension: a prospective study. Hypertension. 1998;31(2):712–718. doi: 10.1161/01.hyp.31.2.712. [DOI] [PubMed] [Google Scholar]
- 22.Hodgkinson J, Mant J, Martin U, et al. Relative effectiveness of clinic and home blood pressure monitoring compared to ambulatory blood pressure monitoring in the diagnosis of hypertension: a systematic review. BMJ. 2011;342:d3621. doi: 10.1136/bmj.d3621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lovibond K, Jowett S, Barton P, et al. Cost-effectiveness of options for the diagnosis of high blood pressure in primary care: a modelling study. Lancet. 2011;378(9798):1219–1230. doi: 10.1016/S0140-6736(11)61184-7. [DOI] [PubMed] [Google Scholar]
- 24.Reinders A, Reggiori F, Shennan AH. Validation of the Dinamap ProCare blood pressure device according to the International Protocol in an adult population. Blood Press Monit. 2006;11(5):293–296. doi: 10.1097/01.mbp.0000217998.96967.fb. [DOI] [PubMed] [Google Scholar]
- 25.Baumgart P, Kamp J. Accuracy of the SpaceLabs Medical 90217 ambulatory blood pressure monitor. Blood Press Monit. 1998;3(5):303–307. [PubMed] [Google Scholar]
- 26.Harrison EG, Roth GM, Hines EAZ. Bilateral indirect and direct arterial pressure. Circulation. 1960;22:419–435. doi: 10.1161/01.cir.22.3.419. [DOI] [PubMed] [Google Scholar]
- 27.Gould BA, Hornung RS, Kieso HA, et al. Is the blood pressure the same in both arms? Clin Cardiol. 1985;8(8):423–426. doi: 10.1002/clc.4960080803. [DOI] [PubMed] [Google Scholar]
- 28.Egushi K, Yacoub M, Jhalani J, et al. Consistency of blood pressure differences between the left and right arms. Arch Intern Med. 2007;167(4):388–393. doi: 10.1001/archinte.167.4.388. [DOI] [PubMed] [Google Scholar]
- 29.Gosse P. Blood pressure should be measured in both arms on the first consultation. J Hypertens. 2002;20(6):1045–1046. doi: 10.1097/00004872-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 30.O'Shea JC, Murphy MB. Ambulatory blood pressure monitoring: which arm? J Hum Hypertens. 2000;14(4):227–230. doi: 10.1038/sj.jhh.1000998. [DOI] [PubMed] [Google Scholar]
- 31.Head GA, Mihalidou AS, Duggan KA, et al. Definition of ambulatory blood pressure targets for diagnosis and treatment of hypertension in relation to clinic blood pressure: prospective cohort study. BMJ. 2010;340:c1104. doi: 10.1136/bmj.c1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fotherby MD, Panayiotou B, Potter JF. Age-related differences in simultaneous interarm blood pressure measurements. Postgrad Med J. 1993;69(809):194–196. doi: 10.1136/pgmj.69.809.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lane D, Beevers M, Barnes N, et al. Inter-arm differences in blood pressure: when are they clinically significant? J Hypertens. 2002;20(6):1089–1095. doi: 10.1097/00004872-200206000-00019. [DOI] [PubMed] [Google Scholar]
- 34.Pickering TG, Houston Miller N, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008;52(1):1–9. doi: 10.1161/HYPERTENSIONAHA.107.189011. [DOI] [PubMed] [Google Scholar]
- 35.Mansoor G, McCabe EJ, White WB. Determinants of the white-coat effect in hypertensive subjects. J Hum Hypertens. 1996;10(2):87–92. [PubMed] [Google Scholar]
- 36.Verdacchia P, Reboldi GP, Angeli F, et al. Short- and long-term incidence of stroke in white-coat hypertension. Hypertension. 2005;45(2):203–208. doi: 10.1161/01.HYP.0000151623.49780.89. [DOI] [PubMed] [Google Scholar]
- 37.Mancia G, Facchetti R, Bombelli M, et al. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension. 2006;47(5):846–853. doi: 10.1161/01.HYP.0000215363.69793.bb. [DOI] [PubMed] [Google Scholar]
- 38.Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25(11):2193–2198. doi: 10.1097/HJH.0b013e3282ef6185. [DOI] [PubMed] [Google Scholar]