LETTER
Mycobacterium abscessus is the most drug-resistant mycobacterial species (1, 2). Combination therapy with intravenous amikacin plus cefoxitin or imipenem and an oral macrolide for 2 to 4 months is recommended (3). Recently, M. abscessus was split into M. abscessus sensu stricto, Mycobacterium massiliense, and Mycobacterium bolletii (4, 5). Effective therapy for M. massiliense lung disease remains elusive but still usually requires parenteral agents (6). We report a case of M. massiliense lung disease that was treated successfully with oral antibiotics only.
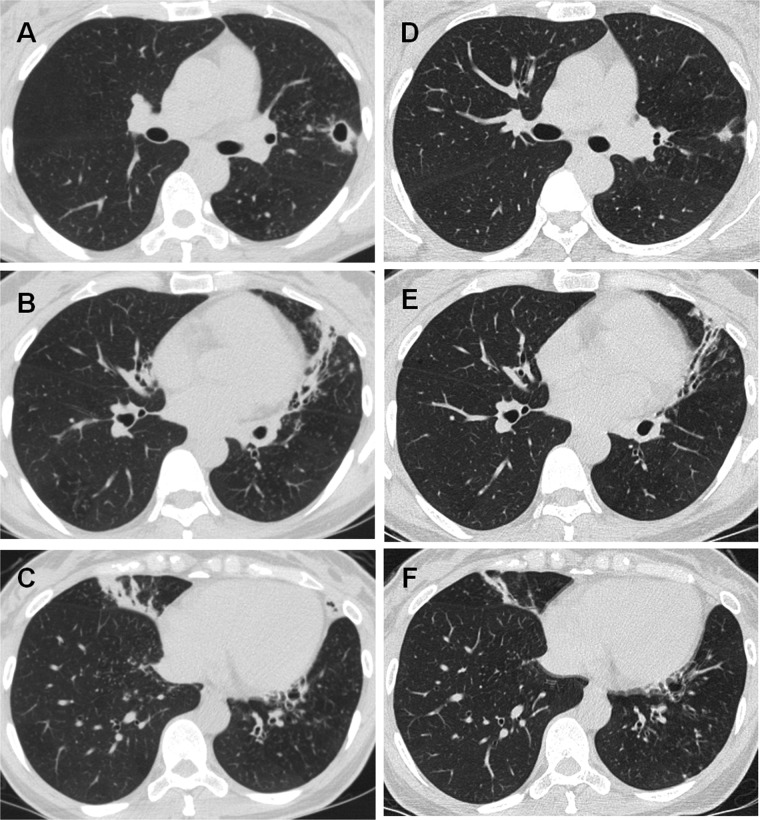
A 43-year-old woman was referred for cough, sputum, and hemoptysis. Computed tomography revealed severe bronchiectasis and peribronchial consolidation in both lungs (Fig. 1A to C). A sputum smear was positive for acid-fast bacilli, and all isolates (>5 sputum specimens) were identified as M. massiliense, using sequence analysis targeting the rpoB and hsp65 genes (6). Other bacterial and mycobacterial pathogens were not found. Drug susceptibility testing demonstrated that the isolates were susceptible to clarithromycin (MIC ≤ 0.5 μg/ml) and amikacin (MIC 16 μg/ml), intermediate to cefoxitin (MIC 64 μg/ml), and resistant to ciprofloxacin (MIC > 16 μg/ml) and moxifloxacin (MIC > 16 μg/ml). We recommended an initial hospital admission for parenteral antibiotic treatment (1, 6). However, the patient could not be admitted because of family problems. Therefore, she was treated with oral clarithromycin (1,000 mg/day) and moxifloxacin (400 mg/day) for 24 months. Moxifloxacin was added because of our concern over the emergence of clarithromycin resistance during clarithromycin monotherapy (1, 6). The treatment outcome was favorable; the patient's symptoms resolved completely, and the radiographic findings improved (Fig. 1D to F). The sputum smear and culture were negative after 4 weeks of antibiotic treatment. She is doing well, with no relapse 40 months after treatment completion.
Fig 1.
Forty-three-year-old woman with M. massiliense lung disease. Computed tomography showed extensive bronchiectasis and peribronchial consolidation in both lungs. (A to C) There was also a 17-mm cavity in the left upper lobe. (D to F) After 12 months of oral antibiotic therapy, the cavity in the left upper lobe was obliterated and the peribronchial consolidation decreased markedly.
This is the first reported case of M. massiliense lung disease that was treated successfully with oral antibiotics only. M. abscessus infection is very difficult to treat. Inducible resistance of M. abscessus to clarithromycin due to expression of the erm(41) gene has been suggested as an explanation for the lack of efficacy of clarithromycin-based treatments of the bacterium (7, 8). In contrast, M. massiliense is susceptible to clarithromycin due to the absence of inducible resistance to macrolides (8). Recently published articles reported that the treatment response to macrolide-based antibiotic therapy including an initial 4 weeks of parenteral therapy is much better in patients with M. massiliense than in those with M. abscessus lung disease (6, 9).
Fluoroquinolones are attractive agents because they can be administered orally for a long time. In fact, fluoroquinolones have been used in many patients during combination treatment of M. abscessus or M. massiliense lung disease in clinical practice (1, 2, 6), but the combined activities of a fluoroquinolone with clarithromycin are still unclear (10). In addition, combination of a macrolide and fluoroquinolone could be a risk factor for macrolide resistance in M. avium complex lung disease (11). In conclusion, our case suggests that a more precise determination of the infecting organism to the species level is important in patients with M. abscessus complex and that M. massiliense lung disease may be treated effectively with oral antibiotics only, including macrolides, without parenteral antibiotics.
Footnotes
Published ahead of print 26 November 2012
REFERENCES
- 1. Jeon K, Kwon OJ, Lee NY, Kim BJ, Kook YH, Lee SH, Park YK, Kim CK, Koh WJ. 2009. Antibiotic treatment of Mycobacterium abscessus lung disease: a retrospective analysis of 65 patients. Am. J. Respir. Crit. Care Med. 180:896–902 [DOI] [PubMed] [Google Scholar]
- 2. Jarand J, Levin A, Zhang L, Huitt G, Mitchell JD, Daley CL. 2011. Clinical and microbiologic outcomes in patients receiving treatment for Mycobacterium abscessus pulmonary disease. Clin. Infect. Dis. 52:565–571 [DOI] [PubMed] [Google Scholar]
- 3. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, Iseman M, Olivier K, Ruoss S, von Reyn CF, Wallace RJ, Jr, Winthrop K. 2007. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am. J. Respir. Crit. Care Med. 175:367–416 [DOI] [PubMed] [Google Scholar]
- 4. Griffith DE. 2011. The talking Mycobacterium abscessus blues. Clin. Infect. Dis. 52:572–574 [DOI] [PubMed] [Google Scholar]
- 5. Griffith DE, Aksamit TR. 2012. Therapy of refractory nontuberculous mycobacterial lung disease. Curr. Opin. Infect. Dis. 25:218–227 [DOI] [PubMed] [Google Scholar]
- 6. Koh WJ, Jeon K, Lee NY, Kim BJ, Kook YH, Lee SH, Park YK, Kim CK, Shin SJ, Huitt GA, Daley CL, Kwon OJ. 2011. Clinical significance of differentiation of Mycobacterium massiliense from Mycobacterium abscessus. Am. J. Respir. Crit. Care Med. 183:405–410 [DOI] [PubMed] [Google Scholar]
- 7. Nash KA, Brown-Elliott BA, Wallace RJ., Jr 2009. A novel gene, erm(41), confers inducible macrolide resistance to clinical isolates of Mycobacterium abscessus but is absent from Mycobacterium chelonae. Antimicrob. Agents Chemother. 53:1367–1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Choi GE, Shin SJ, Won CJ, Min KN, Oh T, Hahn MY, Lee K, Lee SH, Daley CL, Kim S, Jeong BH, Jeon K, Koh WJ. 2012. Macrolide treatment for Mycobacterium abscessus and M. massiliense infection and inducible resistance. Am. J. Respir. Crit. Care Med. 186:917–925 [DOI] [PubMed] [Google Scholar]
- 9. Kim HS, Lee KS, Koh WJ, Jeon K, Lee EJ, Kang H, Ahn J. 2012. Serial CT findings of Mycobacterium massiliense pulmonary disease compared with Mycobacterium abscessus disease after treatment with antibiotic therapy. Radiology 263:260–270 [DOI] [PubMed] [Google Scholar]
- 10. Choi GE, Min KN, Won CJ, Jeon K, Shin SJ, Koh WJ. 2012. Activities of moxifloxacin in combination with macrolides against clinical isolates of Mycobacterium abscessus and Mycobacterium massiliense. Antimicrob. Agents Chemother. 56:3549–3555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Griffith DE, Brown-Elliott BA, Langsjoen B, Zhang Y, Pan X, Girard W, Nelson K, Caccitolo J, Alvarez J, Shepherd S, Wilson R, Graviss EA, Wallace RJ., Jr 2006. Clinical and molecular analysis of macrolide resistance in Mycobacterium avium complex lung disease. Am. J. Respir. Crit. Care Med. 174:928–934 [DOI] [PubMed] [Google Scholar]