Abstract
We describe here the results of antimalarial therapeutic efficacy studies conducted in Cambodia from 2008 to 2010. A total of 15 studies in four sentinel sites were conducted using dihydroartemisinin-piperaquine (DP) for the treatment of Plasmodium falciparum infection and chloroquine (CQ) and DP for the treatment of P. vivax infection. All studies were performed according to the standard World Health Organization protocol for the assessment of antimalarial treatment efficacy. Among the studies of DP for the treatment of P. falciparum, an increase in treatment failure was observed in the western provinces. In 2010, the PCR-corrected treatment failure rates for DP on day 42 were 25% (95% confidence interval [CI] = 10 to 51%) in Pailin and 10.7% (95% CI = 4 to 23%) in Pursat, while the therapeutic efficacy of DP remained high (100%) in Ratanakiri and Preah Vihear provinces, located in northern and eastern Cambodia. For the studies of P. vivax, the day 28 uncorrected treatment failure rate among patients treated with CQ ranged from 4.4 to 17.4%; DP remained 100% effective in all sites. Further study is required to investigate suspected P. falciparum resistance to piperaquine in western Cambodia; the results of in vitro and molecular studies were not found to support the therapeutic efficacy findings. The emergence of artemisinin resistance in this region has likely put additional pressure on piperaquine. Although DP appears to be an appropriate new first-line treatment for P. vivax in Cambodia, alternative treatments are urgently needed for P. falciparum-infected patients in western Cambodia.
INTRODUCTION
Antimalarial drug resistance has been a constant challenge to malaria control in Cambodia. The border area between western Cambodia and Thailand has always been the epicenter of Plasmodium falciparum resistance, starting in the 1960s with chloroquine (CQ), followed by sulfadoxine-pyrimethamine (1970s), mefloquine (1990s), and since 2006, artemisinin (1). The National Center for Parasitology, Entomology, and Malaria Control (CNM) in Cambodia has been monitoring the efficacy of antimalarial treatment since 1991. The findings from therapeutic efficacy studies have facilitated timely and effective changes to national antimalarial drug policy (2, 3). A 3-day course of artesunate combined with mefloquine (ASMQ) was adopted for treatment of uncomplicated falciparum malaria in 2000. However, given the increasingly slow parasite clearance after treatment with ASMQ in Pailin, western Cambodia (4), and the evidence that the efficacy of ASMQ for the treatment of falciparum malaria is declining in several areas of the country (2, 5), CNM decided that a new national malaria treatment policy was needed. In 2008, an international meeting of malaria experts was held to determine the most appropriate treatment for areas where artemisinin resistance to P. falciparum had emerged (6). Dihydroartemisinin-piperaquine (DP) was selected because it had previously demonstrated high efficacy in Cambodia (7–9) and elsewhere in Southeast Asia (10). The treatment's coformulation gave it an added advantage over ASMQ, which, at the time, was only available as a co-package of the two medicines. DP was used at the Cambodia-Thailand border for a large-scale project to contain artemisinin resistance, which started in 2009 (6). A new national treatment policy for P. vivax is also currently being reviewed. CNM has been monitoring the efficacy of CQ against P. vivax since sporadic and isolated failures were detected between 2003 and 2005 in Sampouvloun province (CNM, unpublished data). High chloroquine failure rates (as shown in this article) and demonstrated efficacy of DP elsewhere in the region (11, 12) have led CNM to consider DP as the first-line treatment for P. vivax. A single treatment policy for both P. falciparum and P. vivax could be advantageous in areas where parasitological diagnosis to distinguish Plasmodium species is not available. In addition, the use of artemisinin combination therapy (ACT) for the treatment of P. vivax is considered an appropriate alternative in current World Health Organization (WHO) recommendations (13). We describe here the therapeutic efficacy of DP for the treatment of P. falciparum (from 2008 to 2010) and of CQ (from 2008 to 2009) and DP (in 2010) for the treatment of P. vivax in Cambodia sentinel sites.
MATERIALS AND METHODS
Study sites.
As shown in Fig. 1, the studies were conducted at four health centers through Cambodia (district, province): O Chra (Pailin, Pailin province), Pramoy (Veal Veng, Pursat province), Phnom Dek (Rovieng, Preah Vihear province), and Veun Sai (Veun Sai, Ratanakiri province). The selected sentinel sites were the same sites, which have been monitored by the CNM since 2001. The sites were purposefully selected based on accessibility, population density, and migration at border areas. The studies were conducted during the malaria transmission season between July 2008 and January 2011. Note that while some studies were not finished until early 2011, the vast majority of recruitment occurred in 2010.
Fig 1.
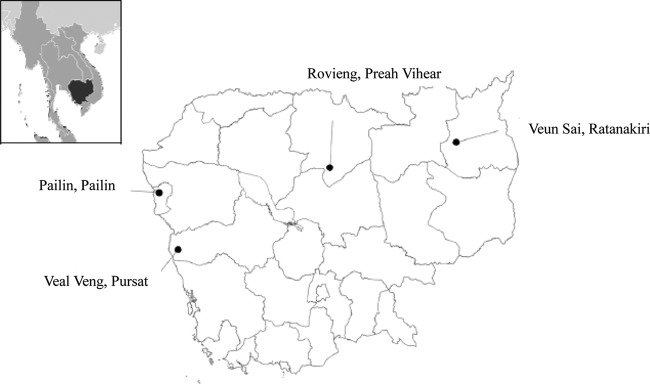
Cambodian sentinel sites (district, province) used for monitoring the efficacy of dihydroartemisinin-piperaquine and chloroquine from 2008 to 2011.
Patients.
The studies were based on the standardized WHO protocol for the assessment of antimalarial treatment efficacy (14). Symptomatic patients were eligible for inclusion if they met the following criteria: over 2 years of age; fever (axillary temperature ≥ 37.5°C) or history of fever in the last 2 days; P. falciparum monoinfection with parasite density between 500 to 200,000 asexual parasites/μl, or ≥250 parasites/μl for P. vivax. Exclusion criteria included the following: pregnancy, one or more signs of severe or complicated malaria, malnutrition, concomitant disease, severe or chronic disease, hypersensitivity, or contraindication to the study treatment.
Study procedures.
At enrolment, patients provided their medical history, and physical, clinical, and biological examinations were performed. Each day, axillary temperature was measured, and blood was taken for thick and thin films to determine asexual parasite counts and parasite species. After the parasites were completely cleared and remained absent for two consecutive days, the patients returned at least once a week, until day 28 for patients with P. vivax and day 42 for patients with P. falciparum. Home visits were made if patients missed appointments. For P. falciparum-infected patients, blood from a finger prick was collected on day 0 and on the day of recrudescence, placed onto Whatman 3MM filter paper, labeled, air dried, and stored in sealed plastic bags. Additional venous blood samples were collected in heparin or acid citrate dextrose tubes and transported to Phnom Penh at 4°C in a cool box within 24 to 48 h of collection for in vitro testing. All studies were approved by the National Ethics Committee at the National Institute of Public Health, Phnom Penh, and the Technical Review Group of the WHO Regional Office for the Western Pacific (ANZCTR registration numbers 12612000184875, 12612000183886, and 12612000181808). The required sample size was calculated according to WHO recommendations (14): a minimum of 50 patients was required for a treatment success of 95%, a confidence level of 95%, and a precision level of 10%.
Treatment regimens.
In 2008 and 2009 (2008/09), DP (Artekin; Holleykin Pharmaceutical Co., Ltd., Guangzhou, China) tablets containing 40 mg of dihydroartemisinin and 320 mg of piperaquine were used. An adult treatment regimen consisted of four doses of two tablets, given at 0, 8, 24, and 48 h. The approximate total adult dose was 6 mg/kg of dihydroartemisinin and 48 mg/kg of piperaquine over 3 days. For children, this dosage was obtained by suspension of a crushed DP tablet in 5 ml of water. In 2009/10 and 2010/11, DP (Duo-Cotecxin; Zhejiang Holley Nanhu Pharmaceutical Co., Ltd., Jiaxing City, China) was used. Each tablet contains the same amount of DP as tablets manufactured by Holleykin. However, the treatment regimen increased from 8 to 9 tablets for an adult, administered as 3 tablets once per day, over 3 days based on WHO recommendations (1). Weight-based dosing was used to yield total doses of ∼7 mg/kg for dihydroartemisinin and 56 mg/kg for piperaquine divided into three doses over 3 days. For the studies of P. vivax, CQ (LaboCreat in 2008; Medopharm in 2009) was administered at a dose of 25 mg/kg (body weight) over three consecutive days, with 10 mg/kg (body weight) administered on days 0 and 1 and 5 mg/kg (body weight) administered on day 2. In 2010, CQ was replaced by DP for treatment of P. vivax, using the same doses described above. All medicines were quality controlled by SGS Netherlands for DP and by North-West University in South Africa for CQ, and the results complied with the certificate of analysis.
Clinical outcomes.
Treatment outcomes were classified based on an assessment of parasitological and clinical outcomes, according to the methods recommended by WHO (14). Therapeutic response was classified on day 28 (P. vivax) and day 42 (P. falciparum) as either early treatment failure (ETF), late clinical failure (LCF), late parasitological failure (LPF), or an adequate clinical and parasitological response (ACPR). All patients failing treatment with DP received quinine and doxycycline for 7 days, starting on the day of failure, except for children younger than 7 years, who received quinine only. Treatment outcomes among patients who took rescue treatment were not assessed. Patients who developed severe malaria during the follow-up were treated with intramuscular artemether. The proportion of cases positive on day 3 was calculated by counting the number of cases with parasites on day 3 divided by the number of patients followed up to day 3. Although not as precise as parasite clearance time, which requires frequent measures of parasitemia, day 3 positivity is considered an appropriate marker of artemisinin resistance for routine monitoring studies (15, 16). Patients who were lost to follow-up, who had protocol violations, or whose treatment failure was due to reinfection or could not be determined were excluded from the per-protocol analysis. For the Kaplan-Meier analysis, patients were included until their last day of follow-up.
Laboratory procedures. (i) Microscopy.
Parasite counts were determined on Giemsa-stained thick films and recorded as the number of parasites per 200 white blood cells, assuming a white blood cell count of 8,000/μl. Two qualified microscopists read the slides, and parasite densities were recorded as the average of these two counts. A third reading was conducted if the discrepancy between parasite density exceeded 50%, or if there were discordant results with regard to positivity.
(ii) In vitro methods.
The in vitro drug sensitivity of the Cambodian isolates was assessed using the classic isotopic 48-h test (17). Artesunate, chloroquine, dihydroartemisinin, mefloquine, and quinine were obtained from Sigma-Aldrich (Singapore) and piperaquine from Yick-Vic Chemicals & Pharmaceuticals (Hong Kong). Stock solutions of antimalarial drugs were prepared in water (Biosedra, France) for chloroquine, 0.5% lactic acid for piperaquine, and methanol for the other drugs. The final plate concentrations ranged from 0.1 to 102.4 nM for artesunate, 5 to 5,120 nM for chloroquine, 0.0625 to 64 nM for dihydroartemisinin, 1 to 1,024 nM for mefloquine, 2 to 2,000 nM for piperaquine, and 6.25 to 6,400 nM for quinine. Each concentration was tested in 11 dilutions and coated in duplicated in a 96-well flat-bottom plate (ATGC, France). Portions (40 μl) of drug solutions were added to each well. Plates were dried into a laminar flow hood (per batch of 30 plates) and kept at 4°C until they were used. Batches of predosed plates were prepared weekly and generally used within 2 weeks after preparation. Their suitability for in vitro testing was monitored regularly (three in vitro testings per batch) using 3D7 reference strain maintained in continuous culture and presenting known responses to the various drugs tested. The results of the in vitro assay were expressed as the 50% inhibitory concentration (IC50), defined as the concentration at which 50% of the incorporation of [3H]hypoxanthine was inhibited, compared to the drug-free control wells. These IC50s are determined by a nonlinear regression using an online IC estimator software called ICEstimator (http://www.antimalarial-icestimator.net/). Fresh clinical isolates of P. falciparum were collected from patients recruited for efficacy studies at the four sentinel sites: Pailin (from 2008 to 2010), Pursat (in 2008 and 2010), Preah Vihear (in 2009), and Ratanakiri (in 2009 and 2010). Each isolate was tested once in duplicate in the microplates with serial dichotomic dilutions of drugs.
(iii) DNA extraction.
Parasite DNA was extracted from blood spots with Instagene matrix (Bio-Rad, Marnes la Coquette, France), according to the manufacturer's instructions.
(iv) Genotyping.
Molecular genotyping techniques were used to distinguish recrudescence from new infection for all patients infected with P. falciparum who failed therapy after day 7. Filter paper blood samples collected on the day of enrolment and on the day of failure were analyzed for polymorphisms in the genes for merozoite surface protein 1 (msp-1), merozoite surface protein 2 (msp-2), and glutamate rich-protein (glurp) using nested-PCR as described elsewhere (18). In accordance with WHO recommendations (19), treatment failure was labeled recrudescence if all msp-1, msp-2, and glurp alleles present at the time of failure had been present at the time of treatment initiation. In all other cases, the failure was considered a new infection.
(v) Pfmdr-1 copy number determination.
The P. falciparum mdr-1 (Pfmdr-1) copy number was measured by using CFX1000 real-time PCR machine (Bio-Rad) relative to the single copy of the β-tubulin (used as a housekeeping gene). Briefly, PCRs were carried out in 25-μl volumes in a 96-well plate containing 1×HOT FIREPol EvaGreen qPCR Mix Plus (Solis BioDyne, Estonia), 0.3 μM concentrations of each forward and reverse primer (mdr-1, 5′-TGCATCTATAAAACGATCAGACAAA-3′ and 5′-TCGTGTGTTCCATGTGACTGT-3′; β-tubulin, 5′-TGATGTGCGCAAGTGATCC-3′ and 5′-TCCTTTGTGGACATTCTTCCTC-3′), and 4 μl of template DNA. Amplifications were performed under the following conditions: 94°C for 15 min, followed by 40 cycles of 94°C for 15 s, 58°C for 20 s, and 72°C for 20 s. For each run, the Pfmdr-1 copy number of each sample was measured in triplicate relative to a standard curve using four standard plasmids (standard 1, a 1:1 ratio of mdr-1 to β-tubulin, to standard 4, a 4:1 ratio of mdr-1 to β-tubulin) and two control parasite clonal lines, the 3D7 Africa line (which has one copy of Pfmdr-1) and line Dd2 (which has three copies of Pfmdr-1), by the ΔΔCT method (where CT is the threshold cycle) (20).
(vi) Pfcrt exon 2 sequences.
Amplifications of Pfcrt exon 2 were performed using PCR conditions previously described (21). Sequencing reactions were carried out with a ABI Prism BigDye terminator cycle sequencing ready reaction kit and were run on a model 3730xl genetic analyzer (Applied Biosystems, Courtaboeuf, France). Electropherograms were visualized and analyzed with CEQ2000 genetic analysis system software (Beckman Coulter, Villepointe, France). The amino acid sequences were compared to the wild-type amino acid sequence (GenBank accession number AF030694). The presence of single nucleotide polymorphisms was confirmed by reading both the forward and the reverse strands.
Statistical analysis.
Data were entered twice in the WHO data entry program for therapeutic efficacy testing, available in a Microsoft Office Excel spreadsheet. The data analysis was conducted using Stata/IC 11.0 software (Stata Corp., College Station, TX). The efficacy data and risk of recrudescence up to day 42, adjusted by PCR genotyping (for P. falciparum only), were evaluated using both per-protocol and Kaplan-Meier analysis. Differences between categorical data were compared using the Fisher exact test (two-sided). Differences in continuous data were first examined using analysis of variance and subsequently compared using a Student t test. Differences in the cumulative treatment failure rate were compared using the log-rank test. In all tests performed, P values of ≤0.05 were considered statistically significant
RESULTS
Treatment outcomes with P. falciparum.
A total of 438 patients infected with P. falciparum were included. The number of patients at each study site ranged from 29 to 80 (Table 1). Among the 438 patients, 5 were censored before day 3. A total of 22 patients were censored from the analysis before day 42, of which 8 were lost to follow-up, 3 had mixed infections at day 0 (detected during quality control), 6 developed vivax malaria during the follow-up; 1 patient withdrew his consent, 3 patients presented treatment failures due to reinfections, and 1 patient had no PCR correction (treatment failure on day 42, Pursat, 2008). Differences in patient characteristics were observed between the studies conducted in the western border area (Pailin and Pursat) and those conducted at the other sites (Preah Vihear and Ratanakiri). The western sites had a higher proportion of males (73% versus 61%, P = 0.01), patients over 15 years of age (77% versus 60%, P < 0.001) and had a higher mean weight (45 kg versus 37 kg, P < 0.001) than the other sites. The geometric mean parasitemia on day 0 in Pailin in 2010/11 (33,744/μl, 95% CI = 21,503 to 52,956/μl) was higher than the geometric mean parasitemia on day 0 in the other studies (14,822/μl, 95% CI = 12,906 to 17,023/μl).
Table 1.
Patient characteristics on admission for treatment of P. falciparum infection with dihydroartemisinin-piperaquine, grouped by year(s), month(s), and site
| Parameter | Pailin, Pailin |
Veal Veng, Pursat |
Rovieng, Preah Vihear 2009, Sep–Oct | Veun Sai, Ratanakiri |
||||
|---|---|---|---|---|---|---|---|---|
| 2008/09, Jul–Jan | 2009/10, Sep–Feb | 2010/11, Aug–Mar | 2008, Jul–Nov | 2010, Aug–Dec | 2009/10, Oct–Jan | 2010, Aug–Sep | ||
| No. of patients | 53 | 39 | 29 | 80 | 60 | 60 | 57 | 60 |
| No. male/no. female | 41/12 | 34/5 | 24/5 | 48/32 | 43/17 | 36/24 | 35/22 | 37/23 |
| Mean age in yrs (SD) | 27.7 (14.2) | 27.7 (11.7) | 25.6 (9.7) | 22.9 (14.2) | 25.1 (14.4) | 22.6 (14.7) | 17.8 (10.7) | 20.9 (15.1) |
| Range | 7–57 | 6–49 | 8–43 | 6–55 | 2–60 | 6–60 | 3–50 | 3–60 |
| Mean wt in kg (SD) | 47 (13.5) | 51.3 (10.9) | 50.9 (10.5) | 40.5 (14.0) | 41.4 (15.3) | 38.6 (15.0) | 36.4 (15.4) | 35.8 (15.9) |
| Range | 15–70 | 15–63 | 20–73 | 14–76 | 11–65 | 11–62 | 12–62 | 11–63 |
| Mean temp in °C (SD) | 38.4 (0.8) | 38.2 (0.9) | 38.6 (1.1) | 38.5 (0.6) | 38.6 (0.4) | 38.5 (0.5) | 38.6 (0.7) | 38.5 (0.6) |
| Range | 36.5–40.3 | 36.1–39.8 | 36–40 | 37.8–40 | 37.9–39.5 | 37.7–40 | 37.5–40.5 | 37.5–40.5 |
| Geometric mean parasitemia/μl | 11,664 | 13,362 | 33,744 | 14,700 | 17,454 | 15,874 | 13,363 | 17,333 |
| 95% CI | 7,924–17,168 | 8,867–20,137 | 21,503–52,956 | 11,287–19,146 | 11,349–26,843 | 11,247–22,404 | 8,892–20,082 | 11,559–25,991 |
The mean (range) total dose of dihydroartemisinin and piperaquine varied over the study period. In 2008/09, the mean (range) total dose among patients was 6.8 (4.2 to 10) mg of dihydroartemisinin/kg and 54.6 (33.7 to 80) mg of piperaquine/kg. Children under 5 years of age were not included in 2008/09. From 2009 to 2010, the mean (range) total dose for children under 5 years of age was 9.6 (7.7 to 10.4) mg of dihydroartemisinin/kg and 76.9 (61.9 to 83.5) mg of piperaquine/kg. Patients 5 years of age and over had a mean (range) total dose of 7.4 (4.9 to 10) mg of dihydroartemisinin/kg and 59.3 (39.5 to 80) mg of piperaquine/kg.
Over the 3-year period, a total of 22 patients had confirmed recrudescence (Table 2). All patients were from the western study sites (22/242, cumulative risk of treatment failure of 8.9% [95% CI = 5.9 to 13.2%]). The majority of patients with recrudescence were in Pailin (n = 15, cumulative risk of treatment failure of 13% [95% CI = 8 to 20.6%]). The other 7 patients were in Pursat (cumulative risk of treatment failure of 5.3% [95% CI = 2.6 to 10.8%]). The median (range) age among patients with recrudescence was 25.7 (10 to 48) years, including two children aged 10 and 11 years. The geometric initial parasitemia (range) was 19,120 (2,108 to 197,487)/μl. Only two adults presented at admission with a parasitemia above 100,000/μl. The mean (range) dosing was 6.9 (5 to 72) mg/kg for piperaquine. None of these parameters differed from the overall study population. In Pursat, none of the patients who presented with treatment failure presented with parasitemia on day 3, whereas in Pailin, 6 of 15 patients who failed treatment were also positive on day 3.
Table 2.
PCR-corrected parasitological and clinical outcomes among patients treated for P. falciparum malaria with dihydroartemisinin-piperaquine, grouped by year(s), month(s), and sitea
| Parameter | Pailin, Pailin |
Veal Veng, Pursat |
Rovieng, Preah Vihear 2009, Sep–Oct | Veun Sai, Ratanakiri |
||||
|---|---|---|---|---|---|---|---|---|
| 2008/09, Jul–Jan | 2009/10, Sep–Feb | 2010/11, Aug–Mar | 2008, Jul–Nov | 2010, Aug–Dec | 2009/10, Oct–Jan | 2010, Aug–Sep | ||
| No. of patients (%) | 53 (100) | 39 (100) | 29 (100) | 80 (100) | 60 (100) | 60 (100) | 57 (100) | 60 (100) |
| Day 1 positive (%) | 51 (100) | 36 (92.3) | 28 (96.5) | 78 (100) | 48 (81.4) | 42 (70.0) | 41 (71.9) | 47 (78.3) |
| Day 2 positive (%) | 34 (66.7) | 25 (64.1) | 21 (75.0) | 51 (65.4) | 17 (28.8) | 9 (15.0) | 2 (3.5) | 6 (10.0) |
| Day 3 positive (%) | 13 (25.5) | 13 (33.3) | 13 (44.8) | 6 (7.7) | 6 (10.2) | 3 (5) | 0 (0) | 0 (0) |
| Dropout by day 42 | 6 (11.3) | 2* (5.1) | 1 (3.5) | 6 (7.5) | 4 (6.7) | 0 (0) | 2** (3.5) | 1** (1.7) |
| LCF (%) | 2 (4.3) | 0 (0) | 1 (3.6) | 1 (1.4) | 6 (10.7) | 0 (0) | 0 (0) | 0 (0) |
| LPF (%) | 3 (6.4) | 3 (8.1) | 6 (21.4) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| ACPR (day 42) (%) | 42 (89.4) | 34 (91.9) | 21 (75.0) | 73 (98.7) | 50 (89.3) | 60 (100) | 55 (100) | 59 (100) |
| Cumulative risk of treatment failure (%) | 10.3 (4.4–22.9) | 7.9 (2.6–22.5) | 24.1 (12.3–44.1) | 1.3 (0.2–9.1) | 10.5 (4.8–21.8) | 0 (0–6.1) | 0 (0–6.1) | 0 (0–6.1) |
LCF, late clinical failure; LPF, late parasitological failure; ACPR, adequate clinical and parasitological response; CI, confidence interval.
, Includes one reinfection on day 35;
, includes one reinfection on day 42.
A significant increase in the cumulative risk of treatment failure after treatment with DP was observed in western sentinel sites (Pailin and Pursat) in 2010/11 compared to the previous years. In Pailin, the proportion of patients with recrudescence on or before day 42 among patients treated with DP increased from 8/84 (cumulative risk of treatment failure of 9.2% [95% CI = 4.7 to 17.6%]) during the first 2 years to 7/28 (cumulative risk of treatment failure of 24.1% [95% CI = 12.3 to 44.1%]) in 2010/11 (P < 0.05). In Pailin, there was a decrease in the median (range) number of days to recrudescence over the study period, from 35 (26 to 42) days in 2008/09, to 21 (21 to 28) days in 2009 and 21 (14 to 28) days in 2010 (P = 0.002). A similar trend in time to recrudescence was not observed in Pursat; however, the proportion of patients with recrudescence increased over the study period, from 1/74 (cumulative risk of treatment failure of 1.3% [95% CI = 0.2 to 9.1%]) in 2008 to 6/56 (cumulative risk of treatment failure of 10.5% [95% CI = 4.8 to 21.8%]) in 2010 (P < 0.05).
The proportion of patients positive on day 3 was higher in western study sites (51/256, 19.9%) than in the other sites (3/177, 1.7%) (P < 0.001). Within the western region, the day 3 positivity rate was higher in Pailin (39/119, 32.8%) than in Pursat (12/137, 8.8%) (P < 0.001). Among studies conducted in western provinces, the day 3 positivity rate was higher among patients who presented with a baseline parasitemia of >100,000/μl (11/26, 42.3%) than among those with a baseline parasitemia which was lower than 100,000/μl (40/230, 17.4%) (P = 0.007).
Treatment outcomes with P. vivax.
A total of 390 patients infected with P. vivax were included (Table 3). The number of patients in each study ranged from 46 to 63. As observed with the studies of patients with P. falciparum, patients included in studies conducted in the western border area had a higher proportion of males (76% versus 65%, P < 0.02), a higher proportion of patients over 15 years of age (81% versus 46%, P < 0.001), and a higher mean weight (47 kg versus 32 kg, P < 0.001) than the other two sites. Differences in baseline patient characteristics observed between studies conducted in west and east were observed for both treatment groups; however, differences in sex were observed for the CQ studies only, which were conducted in 2009 (P < 0.02). A higher geometric mean parasitemia on day 0 was observed among patients included in studies conducted in western provinces (5,129/μl, 95% CI = 4,493 to 5,853/μl) than the other sites (3,538/μl, 95% CI = 2,987 to 4,193/μl); however, significant differences were not observed between the two treatment groups. The treatment failure of CQ for the treatment of P. vivax was higher in Preah Vihear and Ratanakiri (15/106, treatment failure cumulative risk of 14.2% [95% CI = 8.8 to 22.4%]) than in western sites (5/105, treatment failure cumulative risk of 4.8% [95% CI = 2.0 to 11.2%]) (P < 0.05). The efficacy of CQ for the treatment of P. vivax was below 90% in two sites. All five treatment failures occurred at day 28 in Pailin, whereas in the eastern sites failures were reported as early as day 7. Of the 4 patients presenting with parasites at day 3, 3 were classified as late treatment failures. The median number of days to recrudescence for the 15 cases was 17 days (range, 7 to 28 days). In contrast, the ACPR after treatment with DP was 100% in all three sites (Table 4).
Table 3.
Patient characteristics on admission for treatment of P. vivax infection, grouped by treatment, year(s), month(s), and site
| Parameter | Pailin, Pailin |
Veal Veng, Pursat DP, 2010, Aug–Oct | Rovieng, Preah Vihear CQ, 2009, Sep–Dec | Veun Sai, Ratanakiri |
|||
|---|---|---|---|---|---|---|---|
| CQ, 2008/09, Jul–Jan | CQ, 2009/10, Sep–Mar | DP, 2010/11, Aug–Feb | CQ, 2009, Oct–Dec | DP, 2010, Sep–Oct | |||
| No. of patients | 63 | 48 | 53 | 60 | 60 | 46 | 60 |
| No. male/no. female | 45/18 | 42/6 | 42/11 | 41/19 | 37/23 | 30/16 | 41/19 |
| Mean age in yrs (SD) | 21.3 (11.6) | 24.8 (9.8) | 25.7 (11.4) | 25.0 (14.6) | 17.4 (10.0) | 10.9 (9.4) | 18.2 (15.9) |
| Range | 2–60 | 9–57 | 4–60 | 3–60 | 2–40 | 2–45 | 3–57 |
| Mean wt in kg (SD) | 44.0 (14.1) | 51.5 (12.3) | 48.9 (13.9) | 45.1 (15.0) | 37.5 (17) | 25.1 (16.7) | 32 (17.9) |
| Range | 10–63 | 21–89 | 12–72 | 11–75 | 10–64 | 10–69 | 11–63 |
| Mean temp in °C (SD) | 38.5 (0.8) | 38.3 (0.9) | 38.2 (1.0) | 38.4 (0.5) | 38.4 (0.4) | 38.4 (0.6) | 38.4 (0.5) |
| Range | 36.5–39.6 | 36.3–39.8 | 36.1–39.8 | 36.5–39.5 | 37.8–40 | 37.5–40.5 | 37.8–40 |
| Geometric mean parasitemia/μl | 4,461 | 4,224 | 5,571 | 6,445 | 2,997 | 3,088 | 4,640 |
| 95% CI | 3,515–5,663 | 3,115–5,727 | 4,088–7,590 | 5,132–8,092 | 2,305–3,895 | 2,189–4,356 | 3,474–6,196 |
Table 4.
P. vivax treatment outcomes on day 28 (uncorrected), grouped by treatment, year(s), month(s), and site
| Parameter | Pailin, Pailin |
Veal Veng, Pursat DP, 2010, Aug–Oct | Rovieng, Preah Vihear CQ, 2009, Sep–Dec | Veun Sai, Ratanakiri |
|||
|---|---|---|---|---|---|---|---|
| CQ, 2008/09, Jul–Jan | CQ, 2009/10, Sep–Mar | DP, 2010/11, Aug–Feb | CQ, 2009, Oct–Dec | DP, 2010, Sep–Oct | |||
| No. of patients | 63 | 48 | 53 | 60 | 60 | 46 | 60 |
| Day 1 | 58 (92.1) | 36 (75.0) | 0 (0.0) | 8 (13.3) | 44 (73.3) | 38 (82.6) | 17 (28.3) |
| Day 2 | 13 (20.6) | 1 (2.1) | 0 (0.0) | 0 (0.0) | 9 (15) | 12 (26.1) | 0 (0.0) |
| Day 3 | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (3.3) | 2 (4.3) | 0 (0.0) |
| Dropout by day 28 | 3 (4.8) | 3 (4.2) | 2 (3.2) | 3 (5) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| LCF (%) | 2 (3.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 5 (8.3) | 4 (8.7) | 0 (0.0) |
| LPF (%) | 1 (1.7) | 2 (4.4) | 0 (0.0) | 0 (0.0) | 2 (3.3) | 4 (8.7) | 0 (0.0) |
| ACPR (day 28) (%) | 57 (95.0) | 43 (95.6) | 51 (100) | 57 (100.0) | 53 (88.3) | 38 (82.6) | 60 (100) |
| Cumulative risk of treatment failure (%) | 5.1 (1.7–14.9) | 4.4 (1.1–16.6) | 0 (0–6.1) | 0 (0–6.1) | 11.7 (5.7–22.9) | 17.4 (9.1–31.8) | 0 (0–6.1) |
LCF, late clinical failure; LPF, late parasitological failure; ACPR, adequate clinical and parasitological response; CI, confidence interval.
In vitro data.
Among the 587 isolates collected between 2008 and 2010, 484 (82.4%) were adequate for inclusion. These were subsequently examined for their in vitro susceptibility to six antimalarial drugs. Among the 484 isolates that met the inclusion criteria, 292 (60%) gave interpretable results for at least one of the drugs tested. The relatively low success rate for the in vitro assays was likely due to variability in storage conditions, delay and quality of transportation from the study site to the laboratory in Phnom Penh, and possible unreported administration of other antimalarial treatment before collection. The median IC50s (MIC50s) for six antimalarial treatments are presented in Table 5. There were no significant correlations between the MIC50s and the sex, age, parasitemia, or treatment outcomes for any of the drugs tested.
Table 5.
In vitro sensitivity of P. falciparum to artesunate, chloroquine, dihydroartemisinin, mefloquine, piperaquine, and quinine in Cambodia
| Druga | Parameterb | Pailin, Pailin |
Veal Veng, Pursat |
Rovieng, Preah Vihear |
Veun Sai, Ratanakiri |
||||
|---|---|---|---|---|---|---|---|---|---|
| 2008/09, Jul–Mar | 2009/10, Sep–Mar | 2010/11, Aug–Jan | 2008/09, Jul–Jan | 2010, Aug–Dec | 2009/10, Sep–Dec | 2009/10, Oct–Feb | 2010, Aug–Sep | ||
| AS | No. of samples | 19 | 21 | 13 | 79 | 34 | 39 | 13 | 49 |
| Median IC50 (nM) | 1.7 | 2.2 | 1.8 | 2.3 | 1.6 | 1.2 | 2.9 | 1.0 | |
| IQR (nM) | 1.1–2.4 | 1.5–2.6 | 1.3–2.3 | 1.8–3.3 | 1.1–2.2 | 0.9–2.0 | 0.9–4.6 | 0.5–1.6 | |
| Range (nM) | 0.7–4.8 | 0.6–11 | 0.3–4.7 | 0.5–7.6 | 0.6–5.6 | 0.7–7.6 | 0.4–8.2 | 0.3–11 | |
| CQ | No. of samples | 19 | 17 | 9 | 77 | 31 | 36 | 12 | 42 |
| Median IC50 (nM) | 151 | 150 | 151 | 168 | 171 | 83 | 52 | 50 | |
| IQR (nM) | 102–216 | 100–185 | 124–205 | 116–250 | 124–253 | 62–262 | 37–98 | 44–117 | |
| Range (nM) | 83–411 | 56–231 | 99–276 | 45–627 | 33–649 | 25–671 | 22–299 | 18–320 | |
| DHA | No. of samples | 16 | 19 | 12 | 80 | 32 | 34 | 11 | 48 |
| Median IC50 (nM) | 2.6 | 2.8 | 1.5 | 3.9 | 1.9 | 1.7 | 4.0 | 1.2 | |
| IQR (nM) | 1.9–3.2 | 2.1–5.2 | 1.0–2.5 | 2.4–5.7 | 1.1–2.6 | 1.3–2.2 | 1.3–5.5 | 0.7–1.5 | |
| Range (nM) | 0.9–6.4 | 1.1–10 | 0.4–3.5 | 0.7–11 | 0.4–4.2 | 0.5–5.4 | 0.4–11 | 0.2–4.1 | |
| MQ | No. of samples | 18 | 20 | 11 | 79 | 32 | 37 | 12 | 47 |
| Median IC50 (nM) | 27 | 24 | 63 | 85 | 55 | 19 | 13 | 23 | |
| IQR (nM) | 22–38 | 20–48 | 45–108 | 71–118 | 31–96 | 13–44 | 8–27 | 17–31 | |
| Range (nM) | 18–71 | 9–78 | 24–148 | 9–169 | 11–267 | 4–89 | 6–43 | 5–176 | |
| PIP | No. of samples | 16 | 18 | 9 | 67 | 30 | 36 | 12 | 46 |
| Median IC50 (nM) | 63 | 40 | 31 | 80 | 42 | 30 | 35 | 42 | |
| IQR (nM) | 40–103 | 28–47 | 29–40 | 38–115 | 29–56 | 24–47 | 31–38 | 36–47 | |
| Range (nM) | 6.6–125 | 5.0–69 | 20–48 | 7.8–189 | 17–82 | 4.0–77 | 14–51 | 15–107 | |
| QU | No. of samples | 19 | 16 | 9 | 77 | 30 | 32 | 11 | 44 |
| Median IC50 (nM) | 219 | 199 | 358 | 380 | 356 | 92 | 69 | 135 | |
| IQR (nM) | 159–350 | 147–300 | 230–513 | 270–468 | 180–511 | 73–210 | 61–102 | 88–267 | |
| Range (nM) | 66–512 | 127–508 | 135–852 | 69–1121 | 60–958 | 26–895 | 27–205 | 43–822 | |
The in vitro sensitivities of P. falciparum to artesunate (AS), chloroquine (CQ), dihydroartemisinin (DHA), mefloquine (MQ), piperaquine (PIP), and quinine (QU) were evaluated.
IQR, interquartile range.
The MIC50s for CQ, mefloquine (MQ), and quinine (QU) were significantly lower in the eastern study sites compared to the western study sites (P < 0.001). For piperaquine, the MIC50 were significantly higher in Pursat than in Preah Vihear (P = 0.005). For artemisinin derivatives (AS and DHA), no significant differences were found between sites. In Pailin, a significant increase of the IC50 was observed for MQ between 2008/09 and 2010/11 (P < 0.001) while the IC50 of piperaquine decreased (P = 0.01). In Ratanakiri between 2009 and 2010, increases were observed in the IC50 of QU and MQ (P = 0.03 and P = 0.04). In Pailin and Pursat, there were no significant differences in the MIC50 between ACPR patients and treatment failures (ACPR, n = 196, MIC50 = 48.6 nM, range = 5.5 to 190 nM; TF, n = 16, MIC50 = 52.7 nM, range = 19.9 to 88 nM). Positive correlations of IC50 were found between artesunate and dihydroartemisinin (r2 = 0.70, P < 0.0001) and between quinine and mefloquine (r2 = 0.37, P < 0.001).
Molecular markers.
Over the past 3 years (2008 to 2010), the overall proportion of P. falciparum with amplification of Pfmdr-1 was slightly higher in Pursat (22/82, 27%) than in Pailin (20/107, 19%); however, this difference was not significant. Similarly, no significant differences were observed between Pailin and Pursat when studies of the same year were compared to each other. Further, within each site, no significant changes in frequency were observed during this period (Table 6). Amplification of Pfmdr-1 was positively correlated to MQ IC50 (r2 = 0.21, P < 0.0001). Among the 18 DP treatment failure samples analyzed from Pailin and Pursat, 12 of 13 samples from Pailin carried one Pfmdr-1 copy number, and one sample had two Pfmdr-1 copy numbers. In Pursat, all five treatment failure samples were found to carry one Pfmdr-1 copy number. All sequenced samples carried the CVIET haplotype, and none carried a mutation at codon 101.
Table 6.
Pfmdr-1 copy number of P. falciparum samples collected in Pailin and Pursat in Cambodia from 2008 to 2010
| Pfmdr-1 copy no. | No. of samples (%) |
||||
|---|---|---|---|---|---|
| Pailin, Pailin |
Veal Veng, Pursat |
||||
| 2008/09, Jul–Mar | 2009/10, Sep–Mar | 2010/11, Aug–Jan | 2008/09, Jul–Jan | 2010, Aug–Dec | |
| 1 | 29 (83) | 26 (76) | 32 (84) | 15 (68) | 45 (75) |
| 2 | 6 (17)a | 7 (24) | 5 (16) | 3 (32) | 13 (25) |
| 3 | 0 | 1 | 1 | 3 | 2 |
| 4 | 0 | 0 | 0 | 1 | 0 |
These percentages apply to the last 3 rows.
DISCUSSION
Therapeutic efficacy studies of DP conducted between 2008 to 2010 showed significant increases in the proportion of patients positive on day 3 and treatment failure rates in western Cambodia in 2010. DP remains 100% effective for the treatment of P. falciparum in Preah Vihear and Ratanakiri provinces in northern and eastern Cambodia and was 100% effective for the treatment of P. vivax in all sites. Among the studies of CQ for the treatment of P. vivax, which were conducted in Preah Vihear and Ratanakiri in 2009, the treatment failure rates exceeded the treatment policy change threshold of 10%. In vitro studies indicated cross-resistance between artemisinins (artesunate and dihydroartemisinin) and amino-alcohols (quinine and mefloquine) but not between the other antimalarials. Similar to the in vivo data, the in vitro data showed a geographical difference in antimalarial drug resistance.
The high treatment failure rate of 25% observed in Pailin in 2010 is a new development in the sensitivity of P. falciparum to DP, the latest ACT to be recommended by the WHO. These treatment failures suggest that P. falciparum resistance to the partner medicine could be emerging, since it is the role of the partner medicine to clear all remaining parasites from the patient. It is possible that the presence of artemisinin resistance in the region has put an additional burden on the piperaquine component of the combination. Piperaquine is a bisquinoline, and structurally similar to chloroquine, to which there is known resistance in Cambodia, and most other falciparum endemic countries. Piperaquine was developed in the 1960s by the Shanghai Pharmaceutical Industry Research Institute in China and Rhône-Poulenc in France and used as malaria prophylaxis and treatment in China and Indochina for the subsequent 20 years (22). However, widespread use of the drug as monotherapy led to the emergence of resistance in China in the 1980s and 1990s (22). Due to piperaquine's long half-life, the residual antimalarial activity present during the posttreatment period can serve as a selective filter, which prevents infection by sensitive parasites but allows infection by resistant parasites (23). The alleged long-term use of piperaquine as monotherapy in the Pailin area in the 1990s may have also contributed to a rapid decline in P. falciparum sensitivity to piperaquine. In addition, DP was already used for the treatment of P. falciparum malaria in western Cambodia for a pilot project implemented by Médecins Sans Frontières in Pailin province between 2003 and 2005.
DP is one of the five ACTs now recommended by the WHO for the treatment of P. falciparum malaria, and it was the medicine chosen for the first-line treatment in the artemisinin resistance containment project. The DP treatment failure rate in Pailin 2010/11 is the highest ever reported. In a global review of therapeutic efficacy studies conducted between 2000 and 2010, most DP treatment failure rates remained below 10% (1). Two exceptions were Rwanda in 2004 and Papua New Guinea in 2006/07, where ca. 10% of patients failed treatment (11, 24). The study from Papua New Guinea and another study conducted in Papua, Indonesia, found that plasma piperaquine concentration on day 7 below 30 ng/ml were predictive of recrudescence for both P. falciparum and P. vivax (11, 25).
Further study is required to investigate what appears to be the early detection of piperaquine resistance in western Cambodia. Patients from western provinces were more likely to be male, to be older, and to have a higher mean weight than those from the other study sites. These differences likely reflect the fact that many of the malaria patients in western Cambodia are males who work in the forest areas, unlike in eastern Cambodia, where the gender and age distribution is more even, as malaria transmission occurs in the village. The higher baseline parasitemia observed in Pailin may be due to either delay in seeking treatment or to lower immunity as a result of low transmission in Pailin. The high baseline parasitemia was not only associated with a higher day 3 positivity rate but also could have provided a challenge to successful treatment. With the exception of Pailin, all P. falciparum studies reached the minimum required sample of 50 patients. The small sample size in Pailin may have contributed to imprecise estimates of treatment failure, particularly in 2010, where there were only 28 patients on day 42.
Investigation of piperaquine blood levels would help to establish whether poor drug absorption contributed to the treatment failures, since a main determinant of parasitological failure of DP is the plasma concentration of piperaquine on day 7 (12, 25). Despite the high MIC50 value for piperaquine observed in vitro in Pailin in 2008, these results were not sustained over time. However, there is sometimes poor correlation between in vivo and in vitro methods (1), and the sample size in our in vitro study was small (n < 20). Recently, putative molecular markers for piperaquine resistance were found by using in vitro-selected piperaquine-resistant reference clones. Piperaquine resistance was described as linked to deamplification of an 82-kb region of chromosome 5 that includes Pfmdr-1, amplification of an adjacent 63-kb region of chromosome 5, and a novel single-nucleotide polymorphism at Pfcrt codon 101 (26). No assessment of amplification of chromosome 5 was done, except for Pfmdr-1. The molecular marker studies, which were performed during these trials, showed no mutation at Pfcrt codon 101, and one treatment failure carried an increased Pfmdr-1 copy number. Therefore, our results are not consistent with those of Eastman et al. (26).
The increased proportion of patients infected with artemisinin resistant parasites in Pailin and Pursat in 2010/11 supports previous findings of artemisinin resistance in western Cambodia. Evidence of artemisinin resistance in western Cambodia was first suspected following increases in the number of cases positive on day 3 after treatment with ACTs from 2002 to 2005 and subsequently confirmed with additional data from Pailin and Battambang Province collected between 2006 and 2008 (4, 27). An increase in the proportion of patients positive on day 3 over time was not unexpected, given that as the number of cases decrease, there is likely to be a corresponding increase in the selection of resistant strains. However, before the Pailin study in 2010, patients who failed to clear parasites on day 3 did not usually fail treatment, since the partner medicine remained effective. Among the four studies conducted in the western provinces between 2008 and 2010 (excluding Pailin in 2010), 36 patients were positive on day 3; however, only two treatment failures (5.4%) occurred before day 42. These two patients represented only 13.3% of the 15 patients who failed treatment. In contrast, in Pailin in 2010, 4 of the 7 (57%) treatment failures were also positive on day 3. In the same study, the high proportion of patients positive on day 3 (44.8%) increases the probability of experiencing subsequent treatment failure. In short, there appears to be circulating P. falciparum parasites in western Cambodia that may be resistant to both artemisinin and piperaquine.
Western provinces of Cambodia have been found to have more P. falciparum resistance and higher treatment failures than eastern provinces (28, 29). These findings demonstrate that in western provinces, it is becoming increasingly difficult to find a highly effective antimalarial treatment for P. falciparum. Although the sensitivity of P. falciparum to mefloquine has increased following the replacement of artesunate-mefloquine with DP for treatment in Pailin province (4), the in vitro molecular marker data presented here suggest that mefloquine-resistant parasites are still present in Pailin and Pursat. There is an increasingly urgent need for a new antimalarial treatment policy for this population. Treatment options include (i) artesunate-pyronaridine, for which the European Medicines Agency (EMA) recently adopted a positive opinion under article 58 and which was recently registered by the Korean FDA, (ii) quinine-doxycycline over 7 days, and (iii) atovaquone-proguanil. The indications of reduced P. vivax sensitivity to chloroquine in Cambodia can be addressed through a treatment policy change to DP. However, it will be more difficult to find an appropriate solution for the ACT treatment failures in the western provinces.
Failures among P. vivax patients who received treatment with CQ were reported as early as 2003 and 2005 in Sampouvloun, Battambang province (CNM, unpublished data). However, true confirmation of resistance was not possible since blood concentration measures were not available. Although high treatment failure rates indicate reduced susceptibility, CQ resistance can only be confirmed when failure occurs with a CQ blood concentration of ≥100 ng/ml (30). CQ resistance has also been reported in Myanmar and Thailand (31, 32). Since the treatment failure rates were observed to be >10% in two of the study sites (Preah Vihear and Ratanakiri), a new treatment policy is needed. In contrast with P. falciparum resistance, observed mainly in the western provinces, provinces with evidence of P. vivax resistance to chloroquine were located in the eastern part of Cambodia. A limited number of studies have demonstrated the efficacy of ACTs for the treatment of vivax malaria (1, 33); all have found DP to be highly effective (>90%) in Thailand (12), Afghanistan (34), and Indonesia (35). Given that ACTs are now recommended for the treatment of P. vivax (13) and that 100% DP efficacy was demonstrated at all of the study sites reported here, DP seems to be an appropriate new first-line medicine for the treatment of P. vivax in Cambodia. Vanuatu and Solomon Islands have already adopted an ACT (artemether-lumefantrine) for the treatment of both falciparum and vivax malaria (33, 36).
Routine monitoring in Cambodia has played a critical role in the early detection of P. falciparum resistance to mefloquine and artemisinin in the past and now the emergence of treatment failure of P. falciparum to DP and P. vivax to CQ. The early detection of artemisinin resistance on the Cambodia-Thailand border area allowed for the rapid implementation of containment measures, which may have sustained P. falciparum sensitivity to artemisinin in Cambodia's eastern provinces. Routine therapeutic efficacy data remain the gold standard by which national malaria control programs can make effective changes to national treatment policy. Ensuring that such therapeutic efficacy monitoring is performed regularly in all settings where malaria is endemic is a public health imperative and is one of the pillars of the Global Plan for Artemisinin Resistance Containment (16).
ACKNOWLEDGMENTS
This study was supported by USAID, the Global Fund to Fight AIDS, Tuberculosis and Malaria, and the Bill and Melinda Gates Foundation. D.M. was supported by the French Ministry of Foreign Affairs.
We thank the following individuals for providing valuable technical support: Steven Bjorge and Eva-Maria Christophel (WHO), Pheaktra Chim and Sophy Chy (Institut Pasteur du Cambodge), Christiane Bouchier and Magali Tichit (Plate Genomique, Institut Pasteur, Paris, France), and Richard Eastman and David Fidock (Columbia University Medical Center, New York, NY). We are also grateful for the support provided by the provincial health directors and the local health staff at the four sentinel sites.
R.A., A.B., D.M.B., and P.R. are staff members of the WHO. The authors alone are responsible for the views expressed in this publication, and these views do not necessarily represent the decisions, policy, or views of the WHO.
Footnotes
Published ahead of print 3 December 2012
REFERENCES
- 1. World Health Organization 2010. Global report on antimalarial drug efficacy and drug resistance (2000–2010). World Health Organization, Geneva, Switzerland [Google Scholar]
- 2. Denis MB, Tsuyuoka R, Poravuth Y, Narann TS, Seila S, Lim C, Incardona S, Lim P, Sem R, Socheat D, Christophel EM, Ringwald P. 2006. Surveillance of the efficacy of artesunate and mefloquine combination for the treatment of uncomplicated falciparum malaria in Cambodia. Trop. Med. Int. Health 11:1360–1366 [DOI] [PubMed] [Google Scholar]
- 3. Denis MB, Tsuyuoka R, Lim P, Lindegardh N, Yi P, Top SN, Socheat D, Fandeur T, Annerberg A, Christophel EM, Ringwald P. 2006. Efficacy of artemether-lumefantrine for the treatment of uncomplicated falciparum malaria in northwest Cambodia. Trop. Med. Int. Health 11:1800–1807 [DOI] [PubMed] [Google Scholar]
- 4. Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, Lwin KM, Ariey F, Hanpithakpong W, Lee SJ, Ringwald P, Silamut K, Imwong M, Chotivanich K, Lim P, Herdman T, An SS, Yeung S, Singhasivanon P, Day NP, Lindegardh N, Socheat D, White NJ. 2009. Artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 5:455–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rogers WO, Sem R, Tero T, Chim P, Lim P, Muth S, Socheat D, Ariey F, Wongsrichanalai C. 2009. Failure of artesunate-mefloquine combination therapy for uncomplicated Plasmodium falciparum malaria in southern Cambodia. Malar. J. 8:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization 2008. Global malaria control and elimination: report of a meeting on containment of artemisinin tolerance. World Health Organization, Geneva, Switzerland [Google Scholar]
- 7. Denis MB, Davis TM, Hewitt S, Incardona S, Nimol K, Fandeur T, Poravuth Y, Lim C, Socheat D. 2002. Efficacy and safety of dihydroartemisinin-piperaquine (Artekin) in Cambodian children and adults with uncomplicated falciparum malaria. Clin. Infect. Dis. 35:1469–1476 [DOI] [PubMed] [Google Scholar]
- 8. Janssens B, van Herp M, Goubert L, Chan S, Uong S, Nong S, Socheat D, Brockman A, Ashley EA, Van Damme W. 2007. A randomized open study to assess the efficacy and tolerability of dihydroartemisinin piperaquine for the treatment of uncomplicated falciparum malaria in Cambodia. Trop. Med. Int. Health 12:251–259 [DOI] [PubMed] [Google Scholar]
- 9. Karunajeewa H, Lim C, Hung TY, Ilett KF, Denis MB, Socheat D, Davis TM. 2004. Safety evaluation of fixed combination piperaquine plus dihydroartemisinin (Artekin) in Cambodian children and adults with malaria. Br. J. Clin. Pharmacol. 57:93–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Myint HY, Ashley EA, Day NP, Nosten F, White NJ. 2007. Efficacy and safety of dihydroartemisinin-piperaquine. Trans. R. Soc. Trop. Med. Hyg. 101:858–866 [DOI] [PubMed] [Google Scholar]
- 11. Karunajeewa HA, Mueller I, Senn M, Lin E, Law I, Gomorrai PS, Oa O, Griffin S, Kotab K, Suano P, Tarongka N, Ura A, Lautu D, Page-Sharp M, Wong R, Salman S, Siba P, Ilett KF, Davis TM. 2008. A trial of combination antimalarial therapies in children from Papua New Guinea. N. Engl. J. Med. 24:2545–2557 [DOI] [PubMed] [Google Scholar]
- 12. Phyo AP, Lwin KM, Price RN, Ashley EA, Russell B, Sriprawat K, Lindegardh N, Singhasivanon P, White NJ, Nosten F. 2011. Dihydroartemisinin-piperaquine versus chloroquine in the treatment of Plasmodium vivax malaria in Thailand: a randomized controlled trial. Clin. Infect. Dis. 53:977–984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. World Health Organization 2010. Treatment guidelines for malaria, 2nd ed World Health Organization, Geneva, Switzerland [Google Scholar]
- 14. World Health Organization 2009. Methods for surveillance of antimalarial drug efficacy. World Health Organization, Geneva, Switzerland [Google Scholar]
- 15. Stepniewska K, Ashley E, Lee SJ, Anstey N, Barnes KI, Binh TQ, D'Alessandro U, Day NP, de Vries PJ, Dorsey G, Guthmann JP, Mayxay M, Newton PN, Olliaro P, Osorio L, Price RN, Rowland M, Smithuis F, Taylor WR, Nosten F, White NJ. 2010. In vivo parasitological measures of artemisinin susceptibility. J. Infect. Dis. 4:570–579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. World Health Organization 2011. Global plan for artemisinin resistance containment. World Health Organization, Geneva, Switzerland [Google Scholar]
- 17. Desjardins RE, Canfield CJ, Haynes JD, Chulay JD. 1979. Quantitative assessment of antimalarial activity in vitro by a semiautomated microdilution technique. Antimicrob. Agents Chemother. 16:710–718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cattamanchi A, Kyabayinze D, Hubbard A, Rosenthal P, Dorsey G. 2003. Distinguishing recrudescence from reinfection in a longitudinal antimalarial drug-efficacy study: comparison of results based on genotyping of msp-1, msp-2, and glurp. Am. J. Trop. Med. Hyg. 68:133–139 [PubMed] [Google Scholar]
- 19. World Health Organization 2007. Methods and techniques for clinical trials on antimalarial drug efficacy: genotyping to identify parasite populations. World Health Organization, Geneva, Switzerland [Google Scholar]
- 20. Livak KJ, Schmittgen TD. 2001. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods 25:402–408 [DOI] [PubMed] [Google Scholar]
- 21. Andriantsoanirina V, Ratsimbasoa A, Bouchier C, Jahevitra M, Rabearimanana S, Radrianjafy R, Andrianaranjaka V, Randriantsoa T, Rason MA, Tichit M, Rabarijaona LP, Mercereau-Puijalon O, Durand R, Ménard D. 2009. Plasmodium falciparum drug resistance in Madagascar: facing the spread of unusual Pfdhfr and Pfmdr-1 haplotypes and the decrease of dihydroartemisinin susceptibility. Antimicrob. Agents Chemother. 53:4588–4597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Davis TM, Hung TY, Sim IK, Karunajeewa HA, Ilett KF. 2005. Piperaquine: a resurgent antimalarial drug. Drugs 65:75–87 [DOI] [PubMed] [Google Scholar]
- 23. Yeung S, Pongtavornpinyo W, Hastings IM, Mills AJ, White NJ. 2004. Antimalarial drug resistance, artemisinin-based combination therapy, and the contribution of modeling to elucidating policy choices. Am. J. Trop. Med. Hyg. 71 (2S):179. [PubMed] [Google Scholar]
- 24. Karema C, Fanello CI, van Overmeir C, van Geertruyden JP, van Doren W, Ngamije D, D'Alessandro U. 2006. Safety and efficacy of dihydroartemisinin/piperaquine (Artekin) for the treatment of uncomplicated Plasmodium falciparum malaria in Rwandan children. Trans. R. Soc. Trop. Med. Hyg. 12:1105–1111 [DOI] [PubMed] [Google Scholar]
- 25. Price RN, Hasugian AR, Ratcliff A, Siswantoro H, Purba HL, Kenangalem E, Lindegardh N, Penttinen P, Laihad F, Ebsworth EP, Anstey NM, Tjitra E. 2007. Clinical and pharmacological determinants of the therapeutic response to dihydroartemisinin-piperaquine for drug-resistant malaria. Antimicrob. Agents Chemother. 51:4090–4097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Eastman RT, Dharia NV, Winzeler EA, Fidock DA. 2011. Piperaquine resistance is associated with a copy number variation on chromosome 5 in drug-pressured Plasmodium falciparum parasites. Antimicrob. Agents Chemother. 55:3908–3916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM, ARC1 Study Consortium 2008. Evidence of artemisinin-resistant malaria in western Cambodia. N. Engl. J. Med. 359:2619–2620 [DOI] [PubMed] [Google Scholar]
- 28. Lim P, Chim P, Sem R, Nemh S, Poravuth Y, Lim C, Seila S, Tsuyuoka R, Denis MB, Socheat D, Fandeur T. 2005. In vitro monitoring of Plasmodium falciparum susceptibility to artesunate, mefloquine, quinine and chloroquine in Cambodia: 2001–2002. Acta Trop. 93:31–40 [DOI] [PubMed] [Google Scholar]
- 29. Shah NK, Alker AP, Sem R, Susanti AI, Muth S, Maguire JD, Duong S, Ariey F, Meshnick SR, Wongsrichanalai C. 2008. Molecular surveillance for multidrug-resistant Plasmodium falciparum, Cambodia. Emerg. Infect. Dis. 4:1637–1640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Baird JK, Wiady I, Fryauff DJ, Sutanihardja MA, Leksana B, Widjaya H, Kysdarmanto Subianto B. 1997. In vivo resistance to chloroquine by Plasmodium vivax and Plasmodium falciparum at Nabire, Irian Jaya, Indonesia. Am. J. Trop. Med. Hyg. 6:627–631 [DOI] [PubMed] [Google Scholar]
- 31. Guthmann JP, Pittet A, Lesage A, Imwong M, Lindegardh N, Min Lwin M, Zaw T, Annerberg A, de Radiguès X, Nosten F. 2008. Plasmodium vivax resistance to chloroquine in Dawei, southern Myanmar. Trop. Med. Int. Health 13:91–98 [DOI] [PubMed] [Google Scholar]
- 32. Rijken MJ, Boel ME, Russell B, Imwong M, Leimanis ML, Phyo AP, Muehlenbachs A, Lindegardh N, McGready R, Rénia L, Snounou G, Singhasivanon P, Nosten F, Rijken MJ. 2011. Chloroquine resistant vivax malaria in a pregnant woman on the western border of Thailand. Malar. J. 10:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Douglas NM, Anstey NM, Angus BJ, Nosten F, Price RN. 2010. Artemisinin combination therapy for vivax malaria. Lancet Infect. Dis. 10:405–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Awab GR, Pukrittayakamee S, Imwong M, Dondorp AM, Woodrow CJ, Lee SJ, Day NP, Singhasivanon P, White NJ, Kaker F. 2010. Dihydroartemisinin-piperaquine versus chloroquine to treat vivax malaria in Afghanistan: an open randomized, non-inferiority, trial. Malar. J. 9:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ratcliff A, Siswantoro H, Kenangalem E, Maristela R, Wuwung RM, Laihad F, Ebsworth EP, Anstey NM, Tjitra E, Price RN. 2007. Two fixed-dose artemisinin combinations for drug-resistant falciparum and vivax malaria in Papua, Indonesia: an open-label randomised comparison. Lancet 369:757–765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. World Health Organization 2011. World malaria report 2011. World Health Organization, Geneva, Switzerland [Google Scholar]


