Abstract
Resistance of influenza A viruses to neuraminidase inhibitors can arise through mutations in the neuraminidase (NA) gene. We show here that a Q136K mutation in the NA of the 2009 pandemic H1N1 virus confers a high degree of resistance to zanamivir. Resistance is accompanied by reduced numbers of NA molecules in viral particles and reduced intrinsic enzymatic activity of mutant NA. Interestingly, the Q136K mutation strongly impairs viral fitness in the guinea pig transmission model.
TEXT
Neuraminidase (NA) inhibitors, such as oseltamivir and zanamivir, are the most commonly used antiviral drugs for the treatment of severe infections with influenza A virus (FLUAV). Oseltamivir is available only for oral intake (1), whereas zanamivir may be inhaled or given intravenously (2, 3). While oseltamivir resistance has been studied extensively in seasonal H1N1 (sH1N1) (4–7) and pandemic H1N1 (pH1N1) (7–11) FLUAV strains, there are only a few reports of zanamivir resistance. A Q136K mutation in the viral neuraminidase was shown to confer zanamivir resistance in seasonal H1N1 virus strains (12, 13). An I223R mutation in the NA of a clinical pH1N1 isolate was reported to confer resistance to both oseltamivir and zanamivir (14, 15). Both mutant viruses retained good transmissibility in the ferret transmission model (12, 15). Further, E119G or E119V mutations introduced by reverse genetics into the NA of a Canadian pH1N1 virus isolate were shown to confer multidrug resistance. However, both mutants exhibited severely compromised fitness (16). To date, there are no reports on NA mutations in the background of pH1N1 which would solely confer a high degree of resistance to zanamivir. Here, we investigated the potential of the pH1N1 strain A/Hansa Hamburg/01/2009 (identical to A/Hamburg/05/2009; GenBank accession numbers HQ111361 to HQ111368) to acquire zanamivir resistance.
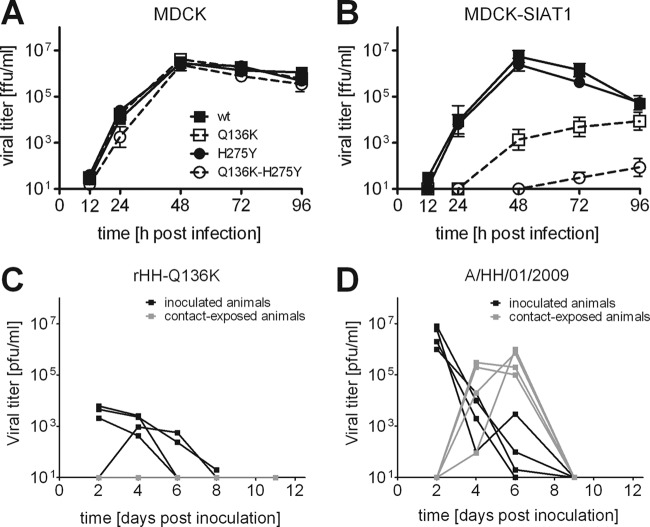
The virus was subjected to 11 serial passages on Madin-Darby canine kidney (MDCK) cells in the presence of escalating concentrations of zanamivir starting from 1 nM up to 2 mM in the final passage. Zanamivir resistance of the passaged viruses was determined by the NA-Star assay (Applied Biosystems) which measures neuraminidase activity with a defined substrate (17). The 50% inhibitory concentration (IC50) values of zanamivir started to rise at passage 8 and reached a value of ∼5 nM at passage 11 (Fig. 1A). Sequencing of plaque-purified viruses from passage 11 revealed a glutamine-to-lysine mutation at amino acid position 136 of NA (Q136K). This mutation, as well as the well-described H275Y oseltamivir resistance mutation in NA, was introduced into the wild-type virus using reverse genetics. We found that the virus carrying the Q136K mutation exhibited an 86-fold increase in the IC50 for zanamivir compared to the wild-type virus (Fig. 1B) but remained sensitive to oseltamivir carboxylic acid (TRC Inc., North York, Canada). In agreement with previous results (11), the H275Y mutant virus exhibited a high degree of resistance to oseltamivir but remained susceptible to zanamivir (Fig. 1B and C). A virus simultaneously carrying both NA mutations (Q136K-H275Y) exhibited increased IC50s for zanamivir and oseltamivir (Fig. 1B and C), although the extent of resistance was less pronounced than in the viruses with single mutations.
Fig 1.
Pandemic 2009 influenza A virus carrying a Q136K mutation in NA exhibits a high degree of resistance to zanamivir but not oseltamivir. (A) Strain A/HH/01/2009 was passaged on MDCK cells in the presence of escalating concentrations of zanamivir (1 nM to 2 mM). The IC50s of zanamivir were determined for passaged viruses using the NA-Star neuraminidase activity assay. (B and C) The IC50s of zanamivir (B) and oseltamivir (C) were determined for recombinant viruses. Wild-type (wt) virus, oseltamivir-resistant virus carrying a H275Y mutation in NA, and the Q136K-H275Y double mutant virus served as controls. Three to six independent measurements per virus were performed. Each symbol shows the value for one measurement. Each short horizontal line shows the mean for that group. Different lowercase letters above the data points for the different groups indicate significant differences between viruses (P < 0.05 by one-way analysis of ariance [ANOVA] and subsequent Tukey's comparison of means).
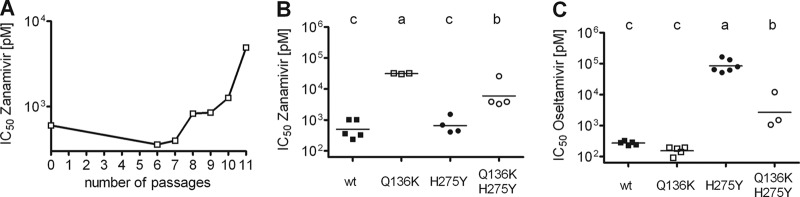
On standard MDCK cells, all mutant viruses showed similar growth kinetics (Fig. 2A). In contrast, the Q136K single mutant virus and the Q136K-H275Y double mutant virus were severely compromised on MDCK-SIAT1 cells (18) that overexpress an α-2-6 sialyltransferase, which results in an enhanced proportion of surface sialic acids being in the α-2-6-linked conformation rather than the α-2-3-linked conformation (Fig. 2B). These differences were confirmed in plaque assays which showed that viruses carrying the Q136K mutation had markedly reduced plaque size in MDCK-SIAT1 cells, but not in standard MDCK cells (data not shown). Using the guinea pig transmission model, we examined whether the Q136K mutation had an impact on viral transmissibility. To do this, four guinea pigs were inoculated intranasally with 104 focus-forming units (FFU) of the Q136K mutant virus. One day later, four naïve guinea pigs were contact exposed to the inoculated animals. Viral titers in nasal washes of all animals were determined by plaque assay on MDCK cells. The zanamivir-resistant Q136K mutant virus reached only very low titers in nasal washings of inoculated animals, and the virus was not transmitted to naïve animals by contact exposure (Fig. 2C). Under such experimental conditions, wild-type virus was readily transmitted (Fig. 2D). These data suggest that the Q136K mutation markedly decreases viral fitness in vitro and in vivo.
Fig 2.
Reduced fitness of viruses with the Q136K mutation in NA in cell culture and guinea pig transmission model. (A and B) Growth kinetics in standard MDCK cells (A) and MDCK-SIAT1 cells overexpressing α-2,6-sialic acids (B) following virus inoculation at a multiplicity of infection (MOI) of 0.001. Wild-type (wt) virus, oseltamivir-resistant virus carrying a H275Y mutation in NA, and Q136K-H275Y double mutant virus served as controls. Results are presented as average log10 titers ± standard errors of means (error bars) of three independent growth kinetic experiments. Viral titers are shown in focus-forming units per milliliter. (C and D) Efficacy of viral transmission in the guinea pig contact model. (C) Four guinea pigs were inoculated intranasally with 104 FFU of the Q136K mutant virus. One day after inoculation, four naïve guinea pigs were exposed to the inoculated animals. Nasal washes were collected at the indicated time points, and viral titers were determined by plaque assay on MDCK cells. Guinea pigs were anesthetized through intramuscular injection of a ketamine-xylazine mixture prior to inoculation and nasal wash treatment. Animal procedures were conducted under biosafety level 3 (BSL3) biocontainment conditions in accordance with local guidelines. (D) Results (adapted from Fig. 3A in reference 11) of a transmission experiment with parental wild-type virus A/HH/01/2009 that was performed under identical animal housing conditions are shown for comparison. pfu, plaque-forming units.
Mutations in the NA gene might confer decreased enzymatic activity, which would compromise virus replication in cells expressing high levels of α-2-6-linked sialic acids and therefore might have an impact on virus transmission (5, 19–21). Alternatively, incorporation of NA into the envelopes of budding viral particles may be reduced. To distinguish between these possibilities, we measured NA levels in viral particles purified from cell culture supernatants by polyethylene glycol (PEG) precipitation (22). Viral nucleoprotein (NP) and NA levels were determined by Western blotting using NP- and NA-specific antisera (23) (Fig. 3A), and NA/NP ratios were calculated for wild-type and mutant viruses by the Odyssey Fc imager system (Li-Cor Biosciences). The NA/NP ratio of mutant virus carrying the Q136K mutation was 3- to 4-fold lower than that of wild-type virus (P < 0.05), indicating that this mutation reduced the level of NA in viral particles (Fig. 3B). In contrast, the NA H275Y mutation did not appear to significantly reduce NA levels in particles (Fig. 3B). The specific activity of NA derived from the different viruses was determined using the NA-Star activity assay. Equal amounts of NA were analyzed using information from NA quantification by Western blotting. We found that NA carrying the Q136K mutation exhibited about 2-fold-lower enzymatic activity with the NA-Star chemiluminescent substrate compared to NA of wild-type virus (Fig. 3C). NA carrying the H275Y mutation alone or in combination with Q136K showed about 5-fold-lower enzymatic activity (Fig. 3C).
Fig 3.
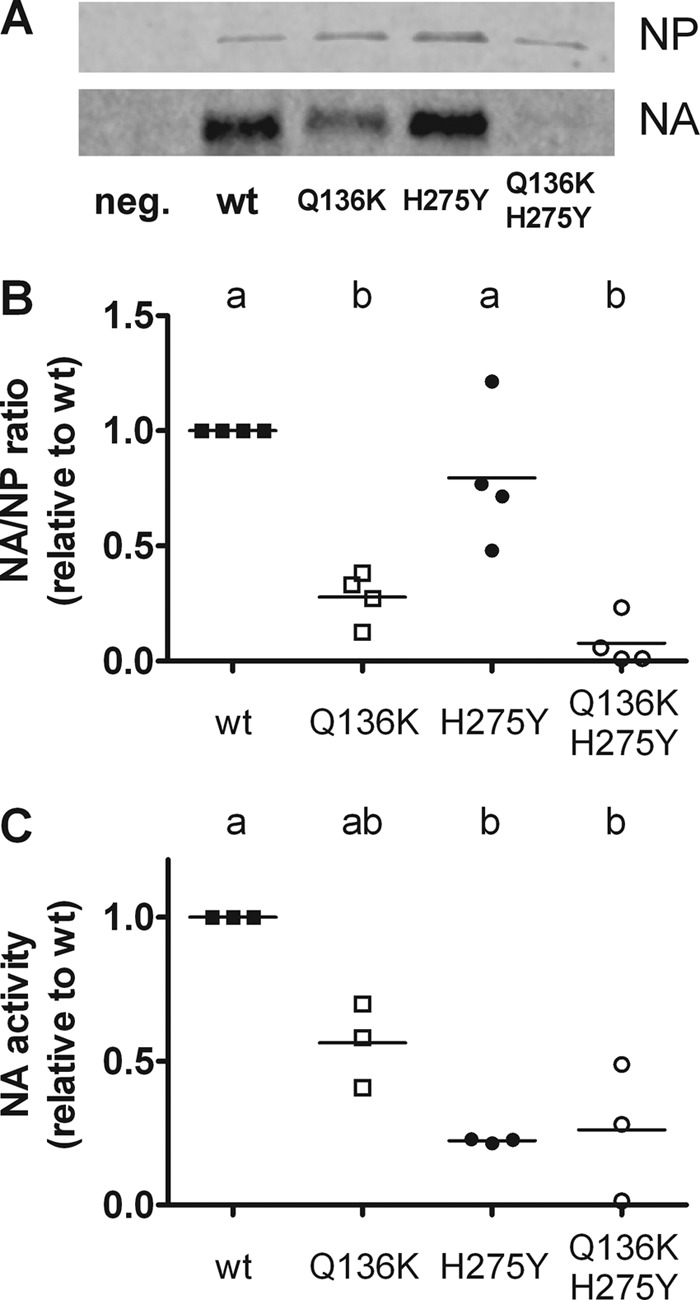
Pronounced effect of the Q136K mutation on NA levels in viral particles. Viruses were grown in MDCK cells, and viral particles were purified by polyethylene glycol precipitation. (A) Levels of NP and NA proteins were visualized by Western blotting utilizing NP- and NA-specific antisera. neg., negative control. (B) Western blot signals were quantified and are presented as NA-to-NP ratios normalized to the wild-type (wt) virus. The data from four independent experiments are shown. (C) Neuraminidase activity was determined by the NA-Star assay. Equal amounts of NA as determined from the Western blot analysis in panel A were used for each virus preparation, and results were normalized against the wt values. The data from three independent experiments are shown. The two different lowercase letters indicate significant differences between viruses (P < 0.05 by one-way ANOVA for repeated measurements and Tukey's comparison of means).
Oseltamivir resistance has become widespread in sH1N1 (24–27) and was described in more than 400 cases of pH1N1 infections up to April 2011 (28). Moreover, oseltamivir has been associated with neuropsychiatric side effects in pediatric settings primarily in Japan, emphasizing the need for alternative antiviral agents (29). To date, the intravenous formulation of zanamivir, which is in phase III clinical development, has been used in cases of oseltamivir resistance in pediatric and intensive care patients (3, 30, 31). In order to optimize therapy in the future, detection and characterization of mutations that confer zanamivir resistance is important. In this study, pH1N1 acquired a Q136K mutation in NA under vigorous selective pressure with zanamivir in cell culture. This is in contrast to a previous study, in which no high-level resistance to zanamivir was observed after serial passaging of a pH1N1 virus in the presence of this compound (32). The Q136K mutation in NA was previously detected in a small number of sH1N1 isolates grown in MDCK cells. Since the mutants outgrew the wild-type viruses in MDCK cells and since Q136K subpopulations were not found in the original patient samples, it remains unclear whether this mutation in NA may occur only during virus growth in MDCK cells (12, 13). In any case, sH1N1 strains carrying the Q136K mutation transmitted efficiently in the ferret model (12).
In our study, the Q136K mutation did not alter the growth kinetics of a pH1N1 strain in conventional MDCK cells, but viral fitness was dramatically reduced in MDCK-SIAT1 cells as well as in the guinea pig transmission model. Amino acid Q136 is located in the periphery of the neuraminic acid binding site of the NA protein. The Q136K mutation was proposed to alter interactions with R156 and D151, thereby disrupting hydrogen bonds between D151 and zanamivir (12). As the structure of zanamivir closely resembles that of natural N-acetyl neuraminic acid (33, 34), it was proposed that NA mutations that prevent zanamivir binding might strongly alter the substrate binding properties of NA and thus result in loss of enzymatic activity (35–37). We found that the Q136K mutation not only reduced the enzymatic activity of NA but also reduced NA levels in viral particles, which readily explains the attenuated phenotype of zanamivir-resistant viruses carrying the Q136K mutation.
The effect of the NA-H275Y mutation on fitness of pandemic H1N1 viruses varied considerably in published studies (7, 28). In our study, the H275Y mutation alone did not negatively affect viral replication in MDCK-SIAT1 cells. However, when introduced together with the Q136K mutation, the H275Y mutation had a pronounced negative effect on virus growth. These various findings suggest that the fitness cost of the H275Y mutation depends heavily on the genetic makeup of the virus.
Taken together, the results presented here suggest that it is rather unlikely that zanamivir-resistant variants of pH1N1 carrying the Q136K mutations will emerge in clinical settings, even if oseltamivir-resistant H275Y variants should become widespread in the human population.
ACKNOWLEDGMENTS
We thank Walter Fuchs for kindly providing the NA-specific antibody, GlaxoSmithKline for providing a free sample of zanamivir, and Mikhail Matrosovich for helpful discussions.
This work was supported by a grant from the German Ministry for Education and Research (FluResearchNet).
Footnotes
Published ahead of print 28 November 2012
REFERENCES
- 1. Brennan BJ, Davies B, Cirrincione-Dall G, Morcos PN, Beryozkina A, Chappey C, Baldo PA, Lennon-Chrimes S, Rayner CR. 2012. Safety, tolerability, and pharmacokinetics of intravenous oseltamivir: single- and multiple-dose phase I studies in healthy volunteers. Antimicrob. Agents Chemother. 56:4729–4737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cass LM, Efthymiopoulos C, Bye A. 1999. Pharmacokinetics of zanamivir after intravenous, oral, inhaled or intranasal administration to healthy volunteers. Clin. Pharmacokinet. 36(Suppl 1):1–11 [DOI] [PubMed] [Google Scholar]
- 3. Gaur AH, Bagga B, Barman S, Hayden R, Lamptey A, Hoffman JM, Bhojwani D, Flynn PM, Tuomanen E, Webby R. 2010. Intravenous zanamivir for oseltamivir-resistant 2009 H1N1 influenza. N. Engl. J. Med. 362:88–89 [DOI] [PubMed] [Google Scholar]
- 4. Bloom JD, Gong LI, Baltimore D. 2010. Permissive secondary mutations enable the evolution of influenza oseltamivir resistance. Science 328:1272–1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carr J, Ives J, Kelly L, Lambkin R, Oxford J, Mendel D, Tai L, Roberts N. 2002. Influenza virus carrying neuraminidase with reduced sensitivity to oseltamivir carboxylate has altered properties in vitro and is compromised for infectivity and replicative ability in vivo. Antiviral Res. 54:79–88 [DOI] [PubMed] [Google Scholar]
- 6. Hurt AC, Holien JK, Parker MW, Barr IG. 2009. Oseltamivir resistance and the H274Y neuraminidase mutation in seasonal, pandemic and highly pathogenic influenza viruses. Drugs 69:2523–2531 [DOI] [PubMed] [Google Scholar]
- 7. Wong DD, Choy KT, Chan RW, Sia SF, Chiu HP, Cheung PP, Chan MC, Peiris JS, Yen HL. 2012. Comparable fitness and transmissibility between oseltamivir-resistant pandemic 2009 and seasonal H1N1 influenza viruses with the H275Y neuraminidase mutation. J. Virol. 86:10558–10570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Duan S, Boltz DA, Seiler P, Li J, Bragstad K, Nielsen LP, Webby RJ, Webster RG, Govorkova EA. 2010. Oseltamivir-resistant pandemic H1N1/2009 influenza virus possesses lower transmissibility and fitness in ferrets. PLoS Pathog. 6:e1001022 doi:10.1371/journal.ppat.1001022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hamelin ME, Baz M, Abed Y, Couture C, Joubert P, Beaulieu E, Bellerose N, Plante M, Mallett C, Schumer G, Kobinger GP, Boivin G. 2010. Oseltamivir-resistant pandemic A/H1N1 virus is as virulent as its wild-type counterpart in mice and ferrets. PLoS Pathog. 6:e1001015 doi:10.1371/journal.ppat.1001015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kiso M, Shinya K, Shimojima M, Takano R, Takahashi K, Katsura H, Kakugawa S, Le MT, Yamashita M, Furuta Y, Ozawa M, Kawaoka Y. 2010. Characterization of oseltamivir-resistant 2009 H1N1 pandemic influenza A viruses. PLoS Pathog. 6:e1001079 doi:10.1371/journal.ppat.1001079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Seibert CW, Kaminski M, Philipp J, Rubbenstroth D, Albrecht RA, Schwalm F, Stertz S, Medina RA, Kochs G, Garcia-Sastre A, Staeheli P, Palese P. 2010. Oseltamivir-resistant variants of the 2009 pandemic H1N1 influenza A virus are not attenuated in the guinea pig and ferret transmission models. J. Virol. 84:11219–11226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hurt AC, Holien JK, Parker M, Kelso A, Barr IG. 2009. Zanamivir-resistant influenza viruses with a novel neuraminidase mutation. J. Virol. 83:10366–10373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Okomo-Adhiambo M, Nguyen HT, Sleeman K, Sheu TG, Deyde VM, Garten RJ, Xu X, Shaw MW, Klimov AI, Gubareva LV. 2010. Host cell selection of influenza neuraminidase variants: implications for drug resistance monitoring in A(H1N1) viruses. Antiviral Res. 85:381–388 [DOI] [PubMed] [Google Scholar]
- 14. van der Vries E, Stelma FF, Boucher CA. 2010. Emergence of a multidrug-resistant pandemic influenza A (H1N1) virus. N. Engl. J. Med. 363:1381–1382 [DOI] [PubMed] [Google Scholar]
- 15. van der Vries E, Veldhuis Kroeze EJ, Stittelaar KJ, Linster M, Van der Linden A, Schrauwen EJ, Leijten LM, van Amerongen G, Schutten M, Kuiken T, Osterhaus AD, Fouchier RA, Boucher CA, Herfst S. 2011. Multidrug resistant 2009 A/H1N1 influenza clinical isolate with a neuraminidase I223R mutation retains its virulence and transmissibility in ferrets. PLoS Pathog. 7:e1002276 doi:10.1371/journal.ppat.1002276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pizzorno A, Bouhy X, Abed Y, Boivin G. 2011. Generation and characterization of recombinant pandemic influenza A(H1N1) viruses resistant to neuraminidase inhibitors. J. Infect. Dis. 203:25–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wetherall NT, Trivedi T, Zeller J, Hodges-Savola C, McKimm-Breschkin JL, Zambon M, Hayden FG. 2003. Evaluation of neuraminidase enzyme assays using different substrates to measure susceptibility of influenza virus clinical isolates to neuraminidase inhibitors: report of the neuraminidase inhibitor susceptibility network. J. Clin. Microbiol. 41:742–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Matrosovich M, Matrosovich T, Carr J, Roberts NA, Klenk HD. 2003. Overexpression of the alpha-2,6-sialyltransferase in MDCK cells increases influenza virus sensitivity to neuraminidase inhibitors. J. Virol. 77:8418–8425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gubareva LV, Robinson MJ, Bethell RC, Webster RG. 1997. Catalytic and framework mutations in the neuraminidase active site of influenza viruses that are resistant to 4-guanidino-Neu5Ac2en. J. Virol. 71:3385–3390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ives JA, Carr JA, Mendel DB, Tai CY, Lambkin R, Kelly L, Oxford JS, Hayden FG, Roberts NA. 2002. The H274Y mutation in the influenza A/H1N1 neuraminidase active site following oseltamivir phosphate treatment leave virus severely compromised both in vitro and in vivo. Antiviral Res. 55:307–317 [DOI] [PubMed] [Google Scholar]
- 21. Yen HL, Herlocher LM, Hoffmann E, Matrosovich MN, Monto AS, Webster RG, Govorkova EA. 2005. Neuraminidase inhibitor-resistant influenza viruses may differ substantially in fitness and transmissibility. Antimicrob. Agents Chemother. 49:4075–4084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Habjan M, Andersson I, Klingstrom J, Schumann M, Martin A, Zimmermann P, Wagner V, Pichlmair A, Schneider U, Muhlberger E, Mirazimi A, Weber F. 2008. Processing of genome 5′ termini as a strategy of negative-strand RNA viruses to avoid RIG-I-dependent interferon induction. PLoS One 3:e2032 doi:10.1371/journal.pone.0002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pavlova SP, Veits J, Keil GM, Mettenleiter TC, Fuchs W. 2009. Protection of chickens against H5N1 highly pathogenic avian influenza virus infection by live vaccination with infectious laryngotracheitis virus recombinants expressing H5 hemagglutinin and N1 neuraminidase. Vaccine 27:773–785 [DOI] [PubMed] [Google Scholar]
- 24. Dharan NJ, Gubareva LV, Meyer JJ, Okomo-Adhiambo M, McClinton RC, Marshall SA, St. George K, Epperson S, Brammer L, Klimov AI, Bresee JS, Fry AM. 2009. Infections with oseltamivir-resistant influenza A(H1N1) virus in the United States. JAMA 301:1034–1041 [DOI] [PubMed] [Google Scholar]
- 25. Hauge SH, Dudman S, Borgen K, Lackenby A, Hungnes O. 2009. Oseltamivir-resistant influenza viruses A (H1N1), Norway, 2007–08. Emerg. Infect. Dis. 15:155–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hurt AC, Ernest J, Deng YM, Iannello P, Besselaar TG, Birch C, Buchy P, Chittaganpitch M, Chiu SC, Dwyer D, Guigon A, Harrower B, Kei IP, Kok T, Lin C, McPhie K, Mohd A, Olveda R, Panayotou T, Rawlinson W, Scott L, Smith D, D'Souza H, Komadina N, Shaw R, Kelso A, Barr IG. 2009. Emergence and spread of oseltamivir-resistant A(H1N1) influenza viruses in Oceania, South East Asia and South Africa. Antiviral Res. 83:90–93 [DOI] [PubMed] [Google Scholar]
- 27. Meijer A, Lackenby A, Hungnes O, Lina B, van der Werf S, Schweiger B, Opp M, Paget J, van de Kassteele J, Hay A, Zambon M, European Influenza Surveillance Scheme 2009. Oseltamivir-resistant influenza virus A (H1N1), Europe, 2007-08 season. Emerg. Infect. Dis. 15:552–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hurt AC, Chotpitayasunondh T, Cox NJ, Daniels R, Fry AM, Gubareva LV, Hayden FG, Hui DS, Hungnes O, Lackenby A, Lim W, Meijer A, Penn C, Tashiro M, Uyeki TM, Zambon M. 2012. Antiviral resistance during the 2009 influenza A H1N1 pandemic: public health, laboratory, and clinical perspectives. Lancet Infect. Dis. 12:240–248 [DOI] [PubMed] [Google Scholar]
- 29. Jefferson T, Jones M, Doshi P, Del Mar C. 2009. Possible harms of oseltamivir–a call for urgent action. Lancet 374:1312–1313 [DOI] [PubMed] [Google Scholar]
- 30. Dulek DE, Williams JV, Creech CB, Schulert AK, Frangoul HA, Domm J, Denison MR, Chappell JD. 2010. Use of intravenous zanamivir after development of oseltamivir resistance in a critically ill immunosuppressed child infected with 2009 pandemic influenza A (H1N1) virus. Clin. Infect. Dis. 50:1493–1496 [DOI] [PubMed] [Google Scholar]
- 31. Elbahlawan L, Gaur AH, Furman W, Jeha S, Woods T, Norris A, Morrison RR. 2011. Severe H1N1-associated acute respiratory failure in immunocompromised children. Pediatr. Blood Cancer 57:625–628 [DOI] [PubMed] [Google Scholar]
- 32. McKimm-Breschkin JL, Rootes C, Mohr PG, Barrett S, Streltsov VA. 2012. In vitro passaging of a pandemic H1N1/09 virus selects for viruses with neuraminidase mutations conferring high-level resistance to oseltamivir and peramivir, but not to zanamivir. J. Antimicrob. Chemother. 67:1874–1883 [DOI] [PubMed] [Google Scholar]
- 33. Varghese JN, McKimm-Breschkin JL, Caldwell JB, Kortt AA, Colman PM. 1992. The structure of the complex between influenza virus neuraminidase and sialic acid, the viral receptor. Proteins 14:327–332 [DOI] [PubMed] [Google Scholar]
- 34. von Itzstein M. 2007. The war against influenza: discovery and development of sialidase inhibitors. Nat. Rev. Drug Discov. 6:967–974 [DOI] [PubMed] [Google Scholar]
- 35. De Clercq E. 2006. Antiviral agents active against influenza A viruses. Nat. Rev. Drug Discov. 5:1015–1025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Moscona A. 2009. Global transmission of oseltamivir-resistant influenza. N. Engl. J. Med. 360:953–956 [DOI] [PubMed] [Google Scholar]
- 37. Zurcher T, Yates PJ, Daly J, Sahasrabudhe A, Walters M, Dash L, Tisdale M, McKimm-Breschkin JL. 2006. Mutations conferring zanamivir resistance in human influenza virus N2 neuraminidases compromise virus fitness and are not stably maintained in vitro. J. Antimicrob. Chemother. 58:723–732 [DOI] [PubMed] [Google Scholar]