Abstract
While the facile transmission of chronic wasting disease (CWD) remains incompletely elucidated, studies in rodents suggest that exposure of the respiratory mucosa may be an efficient pathway. The present study was designed to address this question in the native cervid host. Here, we demonstrate aerosol transmission of CWD to deer with a prion dose >20-fold lower than that used in previous oral inoculations. Inhalation of prions may facilitate transmission of CWD and, perhaps, other prion infections.
TEXT
Chronic wasting disease (CWD) is a transmissible fatal neurodegenerative prion disease of cervids. While the mechanisms of natural transmission remain incompletely elucidated, the efficiency by which CWD spreads strongly suggests horizontal spread. In this respect, blood, urine, saliva, and feces from infected cervids have been shown to contain infectious CWD prions (1–3), albeit at concentrations that are minute compared with those in the brain. Nevertheless, both direct and indirect (environmental) contact (4) with excreted prions remain the most probable means whereby CWD is transmitted among cervids. Regardless of source and route, transmission of CWD prions via contact with the alimentary and/or respiratory mucous membranes seems assured.
While the oral susceptibility of cervids to CWD prions is a feature demonstrated in both experimental and natural contexts (5–10), much less is known regarding the respiratory passages as a route of prion uptake. However, inoculation of transmissible mink encephalopathy (TME), scrapie, and CWD prions via the nasal passages of hamsters and mice has produced transmission rates estimated as 10 to 100 times more efficient than oral inoculation (11–13). Moreover, aerosol exposure of transgenic mice to CWD and of mice to scrapie induced infection more efficiently than intranasal or oral inoculation (11, 14). The present study was undertaken to establish whether such experimental observations in rodents apply to the native host—a point pertinent to both the natural biology of the disease and the biosafe handling of prions.
White-tailed deer (WTD) fawns were provided through the collaboration of the Warnell School of Forestry and Natural Resources, University of Georgia, and housed in the indoor CWD research facility at Colorado State University. Protocols to prevent unrelated exposure and cross-contamination between study cohorts were previously described (2). Established inocula were prepared from brains of CWD-infected (deer 104) and naive (deer 123) WTD (2) in 1× phosphate-buffered saline to a final concentration of 5% weight-to-volume (wt/vol). Two cohorts (n = 6 CWD and n = 3 sham) (Table 1) were anesthetized with ketamine and medetomidine and exposed to 1 ml of aerosolized inoculum over a 7-min period using a custom-designed chamber. A second, 1-ml aerosol exposure was administered 7 days later.
Table 1.
Aerosol transmission of CWD to white-tailed deer
| Animal | Result of indicated assay at indicated time (m.p.i.)a |
Presence of early neurologic signs (m.p.i.) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 |
6 |
9 |
12 |
||||||||||||||
| sPMCA |
WB |
IHC |
WB |
IHC |
WB |
IHC |
WB |
IHC |
|||||||||
| T | R | T/R | T/R | T | R | T | R | T | R | T | R | T | R | T | R | ||
| Sham n = 3 | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | None |
| 812 | − | − | − | − | + | − | + | − | + | − | + | − | + | + | + | − | 12 |
| 813 | + | − | − | − | + | − | NF | + | + | + | + | + | + | + | + | NF | 12 |
| 815 | + | − | − | − | + | − | + | + | + | − | + | NF | + | + | + | + | 12 |
| 816b | + | + | + | + | + | + | + | + | 12 | ||||||||
| 817 | − | − | − | − | + | + | + | + | + | + | + | + | + | + | + | + | 12 |
| 818 | + | − | − | − | + | + | + | + | + | + | + | + | + | + | NF | + | 12 |
sPMCA, serial protein misfolding cyclic amplification; WB, Western blot; IHC, immunohistochemistry; T, tonsil; R, RAMALT; m.p.i., months postinoculation; NF, no follicles; +, PrPCWD present; −, PrPCWD not present.
Deer 816 was not sampled at 3 or 6 m.p.i. due to concern over an idiosyncratic anesthetic reaction after the second inoculation. The anesthetic drug combination was changed for the 9-m.p.i. sampling, resulting in no untoward effects.
The exposure chamber consisted of a canine anesthesia mask (catalog no. 014963; MWI Veterinary Supply, Boise, ID) remodeled to accommodate an Omron nebulizer (NEC21; J. Hewitt, Inc., Monarch Beach, CA) and sealed with silicone adhesive (Goop; Eclectic Products, Pineville, LA). A Wye connector (part no. PN173; Sea-Long Medical Systems, Inc., Louisville, KY) with intake (part no. PN174; Sea-Long) and export (part no. PN175; Sea-Long) one-way valves was attached to the anesthesia mask. An anesthesia tube (catalog no. 000338; MWI Veterinary Supply) was connected to the export valve, and an inline filter (part no. PN154; Sea-Long) was attached to a 2-gallon Rubbermaid container fitted with a P100 cartridge (FL1-41590; Lab Safety Supply, Fort Collins, CO) (Fig. 1a). Once the inoculum was loaded into the apparatus, petroleum jelly was applied to the deer's snout. Plastic wrap with ports fashioned over the nostrils permitted nose-only aerosol exposure (Fig. 1b).
Fig 1.
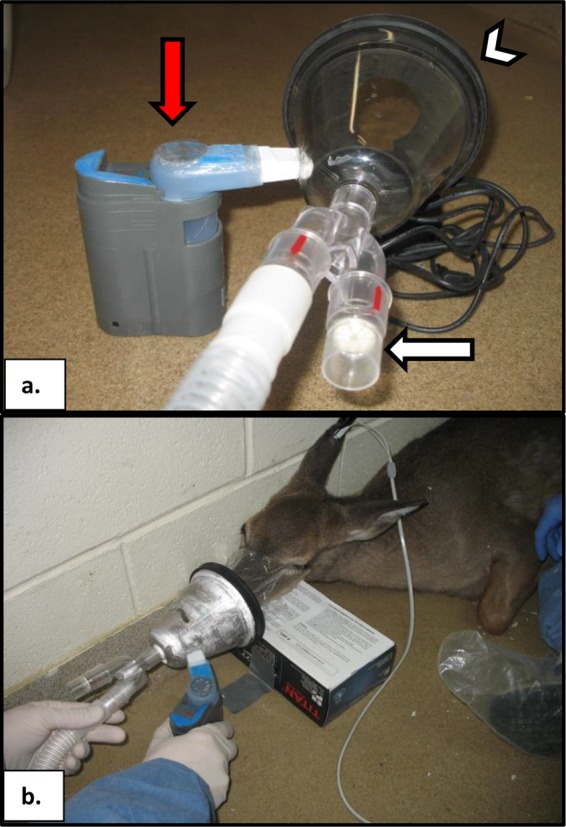
Apparatus used for nose-only aerosol exposure of white-tailed deer (WTD) to CWD prions; (a) exposure chamber showing the nebulizer (red arrow), air ports (white arrow), and mask (white arrowhead); (b) deer muzzle inserted in customized mask to provide nose-only exposure.
WTD were aerosol exposed for 14 min to an estimated total of 100 mg of brain tissue generated from 2 ml of a 5% (wt/vol) brain homogenate. As brain homogenate consists of 10% solid material and inhalation represents half of the respiration cycle (11), the largest possible aerosolized dose of brain tissue inoculated into each deer, assuming all inoculum deposited on the mucous membranes, would be 5 mg.
Tonsil and rectoanal mucosa-associated lymphoid tissue (RAMALT) biopsy specimens were collected at 3, 6, 9, and 12 months postinoculation (m.p.i.) and analyzed by Western blotting (WB), immunohistochemistry (IHC), and serial protein misfolding cyclic amplification (sPMCA). The previously described WB protocol (15) employed Trans-blot Turbo (Bio-Rad) and Snap i.d. systems (Millipore) using antibody BAR-224 (Caymen Chemical) conjugated with horseradish peroxidase (HRP) (1:5,000). The IHC protocol (11) employed BAR-224 (1:1,000 dilution) and the EnVision+ HRP anti-mouse system (Dako) (4, 11).
The sPMCA protocol (1, 16, 17) employed 10-μl test samples added to 50 μl of normal Tg(cerPrP) mouse brain homogenate (NBH) [Tg(cerPrP) mice are transgenic mice expressing cervid prion] in PCR tubes (USA Scientific, St. Louis, MO) with parafilm sealing. Sonicator (Misonix, Inc., Farmingdale, NY) cycles of 10 s were separated by 5-min incubations at 37°C over 24 h, resulting in 288 cycles per round. Ten-microliter aliquots were transferred to 50 μl of fresh NBH for two additional rounds and then analyzed by WB.
Aerosol exposure was efficient in inducing CWD prion infection. At 3 m.p.i., sPMCA amplified PrPCWD, the abnormal isoform of the cellular prion protein (PrPC), from 3 of 5 (60%) tonsil and 0 of 5 (0%) RAMALT biopsy specimens. IHC and WB assays were negative at this time for both tissues. By 6 m.p.i. and 9 m.p.i., IHC and/or WB demonstrated PrPCWD in biopsied tissues from all CWD-exposed deer (100%) examined (Fig. 2 and 3). By 12 m.p.i., early clinical signs of CWD were observed in all 6 CWD-exposed animals (Table 1). Sham-exposed deer (n = 3) remained negative for CWD infection in all samples and by all assays and exhibited no signs of clinical disease (Fig. 2 and 3 and Table 1).
Fig 2.
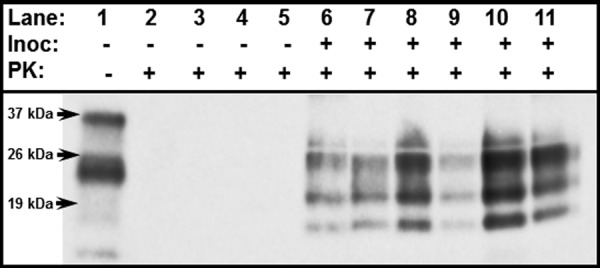
Western blot detection of PrPCWD (lanes 6 to 11) from 8 μl of a 2% tonsil homogenate of WTD exposed to aerosolized CWD prions at 12 m.p.i. Tonsils of deer exposed to sham inoculum (lanes 3 to 5) show no evidence of PrPCWD. PrPC in normal WTD brain controls are shown in lanes 1 and 2. Inoc, CWD inoculum; PK, proteinase K.
Fig 3.
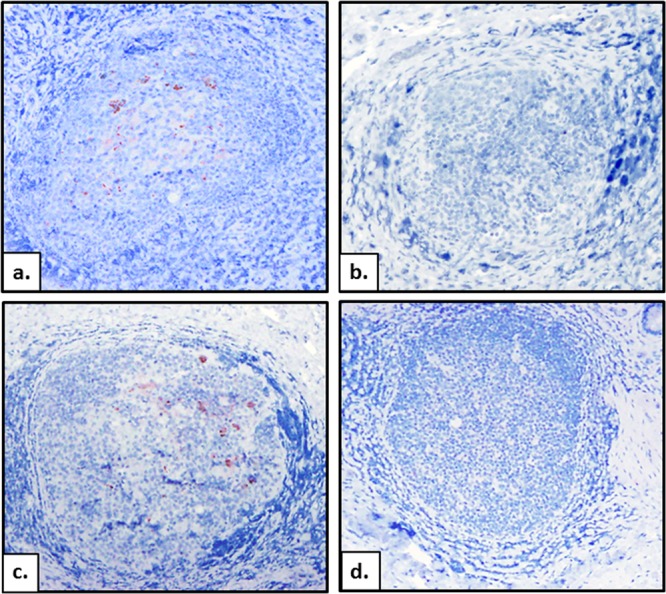
(a, b) PrPCWD in tonsil of WTD exposed to aerosolized CWD prions (PrPCWD) (a) versus tonsil of a sham-aerosol-exposed deer (b). (c, d) PrPCWD in RAMALT from CWD-aerosolized deer (c) versus RAMALT from sham-aerosol control (d). magnification, ×20.
Cervids have a highly sensitive olfactory system to monitor their environment for predators, prey, food, and/or reproductive cues (18, 19), which is also an efficient conduit for airborne pathogens (20, 21). The present results demonstrate aerosol transmission of CWD using a dose at least 20 times lower than those in previous oral inoculation studies, yet with infection kinetics equal to or more rapid than oral exposure (2, 5, 9). Until such time as endpoint titration studies are possible in deer, such dose comparisons must remain relative.
The apparent enhanced efficiency of aerosol transmission could relate to the disruption of prion aggregates into smaller, more infectious particles (22) that travel and disperse more efficiently and/or more deeply into airways. Other studies have shown that inhaled particles and odorants disperse widely in nasal passages and are efficiently endocytosed by epithelia and M cells and then rapidly conveyed to lymph nodes (23–25). Therefore, entry of inhaled droplet- or soil particle-bound CWD prions via multiple mucosal portals is plausible and potentially highly efficient.
Prion uptake in cervids could also be facilitated by the flehmen response; a mechanism used by cervids to identify potential mates by drawing pheromones into the nasal passages for detection by specialized receptors in the vomeronasal organ (26–30). Given that infectious prions are excreted in urine and saliva and bind to soil (2, 31, 32), the flehmen response could also facilitate prion access into the nasal cavity.
In summary, CWD prions are efficiently transmitted to WTD via aerosolization using a delivered dose substantially lower than previously reported by the oral route. Our results provide further evidence that prions delivered to the nasal passages are sufficient to transmit CWD and allow the inference that aerosolization may facilitate the transmission of prions in general.
ACKNOWLEDGMENTS
This work was supported by NIH/NIAID contract HHSN272201000009I (E.A.H. and C.K.M.) and the Prion Research Institute (N.D.D.).
Special thanks to the animal care technicians, Amy V. Nalls for coordinating collections, and Stephanie Fullaway, Alan Elder, and Amber Mayfield for processing samples.
Footnotes
Published ahead of print 21 November 2012
REFERENCES
- 1. Haley NJ, Mathiason CK, Zabel MD, Telling GC, Hoover EA. 2009. Detection of sub-clinical CWD infection in conventional test-negative deer long after oral exposure to urine and feces from CWD+ deer. PLoS One 4:e7990 doi:10.1371/journal.pone.0007990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mathiason CK, Powers JG, Dahmes SJ, Osborn DA, Miller KV, Warren RJ, Mason GL, Hays SA, Hayes-Klug J, Seelig DM, Wild MA, Wolfe LL, Spraker TR, Miller MW, Sigurdson CJ, Telling GC, Hoover EA. 2006. Infectious prions in the saliva and blood of deer with chronic wasting disease. Science 314:133–136 [DOI] [PubMed] [Google Scholar]
- 3. Tamguney G, Miller MW, Wolfe LL, Sirochman TM, Glidden DV, Palmer C, Lemus A, DeArmond SJ, Prusiner SB. 2009. Asymptomatic deer excrete infectious prions in faeces. Nature 461:529–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Miller MW, Williams ES, Hobbs NT, Wolfe LL. 2004. Environmental sources of prion transmission in mule deer. Emerg. Infect. Dis. 10:1003–1006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fox KA, Jewell JE, Williams ES, Miller MW. 2006. Patterns of PrPCWD accumulation during the course of chronic wasting disease infection in orally inoculated mule deer (Odocoileus hemionus). J. Gen. Virol. 87:3451–3461 [DOI] [PubMed] [Google Scholar]
- 6. Hamir AN, Gidlewski T, Spraker TR, Miller JM, Creekmore L, Crocheck M, Cline T, O'Rourke KI. 2006. Preliminary observations of genetic susceptibility of elk (Cervus elaphus nelsoni) to chronic wasting disease by experimental oral inoculation. J. Vet. Diagn. Invest. 18:110–114 [DOI] [PubMed] [Google Scholar]
- 7. Kreeger TJ, Montgomery DL, Jewell JE, Schultz W, Williams ES. 2006. Oral transmission of chronic wasting disease in captive Shira's moose. J. Wildl. Dis. 42:640–645 [DOI] [PubMed] [Google Scholar]
- 8. Seelig DM, Mason GL, Telling GC, Hoover EA. 2010. Pathogenesis of chronic wasting disease in cervidized transgenic mice. Am. J. Pathol. 176:2785–2797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sigurdson CJ, Williams ES, Miller MW, Spraker TR, O'Rourke KI, Hoover EA. 1999. Oral transmission and early lymphoid tropism of chronic wasting disease PrPres in mule deer fawns (Odocoileus hemionus). J. Gen. Virol. 80(Part 10):2757–2764 [DOI] [PubMed] [Google Scholar]
- 10. Trifilo MJ, Ying G, Teng C, Oldstone MB. 2007. Chronic wasting disease of deer and elk in transgenic mice: oral transmission and pathobiology. Virology 365:136–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Denkers ND, Seelig DM, Telling GC, Hoover EA. 2010. Aerosol and nasal transmission of chronic wasting disease in cervidized mice. J. Gen. Virol. 91:1651–1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hamir AN, Kunkle RA, Richt JA, Miller JM, Greenlee JJ. 2008. Experimental transmission of US scrapie agent by nasal, peritoneal, and conjunctival routes to genetically susceptible sheep. Vet. Pathol. 45:7–11 [DOI] [PubMed] [Google Scholar]
- 13. Kincaid AE, Bartz JC. 2007. The nasal cavity is a route for prion infection in hamsters. J. Virol. 81:4482–4491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Haybaeck J, Heikenwalder M, Klevenz B, Schwarz P, Margalith I, Bridel C, Mertz K, Zirdum E, Petsch B, Fuchs TJ, Stitz L, Aguzzi A. 2011. Aerosols transmit prions to immunocompetent and immunodeficient mice. PLoS Pathog. 7:e1001257 doi:10.1371/journal.ppat.1001257 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 15. Denkers ND, Telling GC, Hoover EA. 2011. Minor oral lesions facilitate transmission of chronic wasting disease. J. Virol. 85:1396–1399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Haley NJ, Mathiason CK, Carver S, Zabel M, Telling GC, Hoover EA. 2011. Detection of chronic wasting disease prions in salivary, urinary, and intestinal tissues of deer: potential mechanisms of prion shedding and transmission. J. Virol. 85:6309–6318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Haley NJ, Seelig DM, Zabel MD, Telling GC, Hoover EA. 2009. Detection of CWD prions in urine and saliva of deer by transgenic mouse bioassay. PLoS One 4:e4848 doi:10.1371/journal.pone.0004848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Buck L, Axel R. 1991. A novel multigene family may encode odorant receptors: a molecular basis for odor recognition. Cell 65:175–187 [DOI] [PubMed] [Google Scholar]
- 19. Dulac C. 2000. Sensory coding of pheromone signals in mammals. Curr. Opin. Neurobiol. 10:511–518 [DOI] [PubMed] [Google Scholar]
- 20. Alexandersen S, Zhang Z, Donaldson AI, Garland AJ. 2003. The pathogenesis and diagnosis of foot-and-mouth disease. J. Comp. Pathol. 129:1–36 [DOI] [PubMed] [Google Scholar]
- 21. Palmer MV, Waters WR, Whipple DL. 2003. Aerosol exposure of white-tailed deer (Odocoileus virginianus) to Mycobacterium bovis. J. Wildl. Dis. 39:817–823 [DOI] [PubMed] [Google Scholar]
- 22. Silveira JR, Raymond GJ, Hughson AG, Race RE, Sim VL, Hayes SF, Caughey B. 2005. The most infectious prion protein particles. Nature 437:257–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Casteleyn C, Cornelissen M, Simoens P, Van den Broeck W. 2010. Ultramicroscopic examination of the ovine tonsillar epithelia. Anat. Rec. (Hoboken) 293:879–889 [DOI] [PubMed] [Google Scholar]
- 24. Kincaid AE, Hudson KF, Richey MW, Bartz JC. 2012. Rapid transepithelial transport of prions following inhalation. J. Virol. 86:12731–12740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kraehenbuhl JP, Neutra MR. 2000. Epithelial M cells: differentiation and function. Annu. Rev. Cell Dev. Biol. 16:301–332 [DOI] [PubMed] [Google Scholar]
- 26. Gassett JW, et al. 1998. Stimuli-related variation in urination frequency of female white-tailed deer during the estrous cycle. Appl. Anim. Behav. Sci. 56:71–75 [Google Scholar]
- 27. Kelliher KR, Baum MJ, Meredith M. 2001. The ferret's vomeronasal organ and accessory olfactory bulb: effect of hormone manipulation in adult males and females. Anat. Rec. 263:280–288 [DOI] [PubMed] [Google Scholar]
- 28. Meredith M, O'Connell RJ. 1979. Efferent control of stimulus access to the hamster vomeronasal organ. J. Physiol. 286:301–316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Thorne N, Amrein H. 2003. Vomeronasal organ: pheromone recognition with a twist. Curr. Biol. 13:R220–R222 [DOI] [PubMed] [Google Scholar]
- 30. Vercauteren KC, Burke PW, Phillips GE, Fischer JW, Seward NW, Wunder BA, Lavelle MJ. 2007. Elk use of wallows and potential chronic wasting disease transmission. J. Wildl. Dis. 43:784–788 [DOI] [PubMed] [Google Scholar]
- 31. Johnson CJ, Phillips KE, Schramm PT, McKenzie D, Aiken JM, Pedersen JA. 2006. Prions adhere to soil minerals and remain infectious. PLoS Pathog. 2:e32 doi:10.1371/journal.ppat.0020032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kariv-Inbal Z, Ben-Hur T, Grigoriadis NC, Engelstein R, Gabizon R. 2006. Urine from scrapie-infected hamsters comprises low levels of prion infectivity. Neurodegener. Dis. 3:123–128 [DOI] [PubMed] [Google Scholar]


