Abstract
OBJECTIVE
Certain dietary and physical activity behaviors have been associated with the risk of developing type 2 diabetes, yet little is known about the prevalence of these behaviors among Latinas (Latino women). The purpose of this cross-sectional study was to compare the prevalence of diabetes-related behaviors in Latinas and non-Latinas.
RESEARCH DESIGN AND METHODS
Using data from the 2009 California Health Interview Survey, we compared self-reported diabetes-related behaviors of Latinas (n = 4,321) to non-Latinas (n = 21,112) after excluding women who were pregnant or had diabetes. For six behaviors, we determined the cut point for the least healthy tertile: walking, doing moderate to vigorous physical activity, and consuming fried potatoes, sugar-sweetened beverages (SSBs), desserts, and fast food. We used logistic regression to examine the association between Latina ethnicity and being in the least healthy tertile compared with the other two tertiles for each of these behaviors.
RESULTS
In multivariate models adjusted for age, income, education, marital status, health status, smoking, and acculturation, Latinas had a higher risk (odds ratio [95% CI]) of being in the least healthy tertile for the consumption of fast food (1.94 [1.63–2.31]), SSBs (1.53 [1.29–1.82]), and fried potatoes (1.32 [1.18–1.67]), and lower risk for desserts (0.82 [0.70–0.95]). Latinas and non-Latinas had similar physical activity levels.
CONCLUSIONS
Dietary differences between Latinas and non-Latinas (particularly in the consumption of fast food and SSBs) may be the focus of interventions to prevent diabetes in Latinas. Further research among Latinas is needed to understand and modify these dietary behaviors.
Type 2 diabetes results in a tremendous public health and economic burden, affecting almost 12% of the U.S. adult population (1) and costing ∼$218 billion annually (2). The diabetes epidemic in the U.S. disproportionately affects Latinos, with the prevalence in Mexican-American adults being twice that of whites (3). The incidence and prevalence of diabetes continue to rise (4) along with the size of the Latino population, suggesting that the burden of diabetes on the U.S. health care system will increase in the future. In addition, high rates of overweight and obesity in Latinos confer an increased risk of diabetes in this growing population (5). Compared with all other demographic groups, Latinas (Latino women) have the highest lifetime risk of developing diabetes, estimated at 53% (6). Reducing the burden of diabetes in the U.S. requires a better understanding of the factors underlying Latinas’ high risk for developing this disease.
Numerous epidemiologic studies have identified specific dietary and physical activity behaviors that impact diabetes risk. Dietary risk factors include the consumption of fried potatoes (7), fast food (8), sugar-sweetened beverages (SSBs) (9), and desserts (10). Both observational (11) and experimental studies (12) suggest that physical activity helps prevent diabetes. Many studies have examined the prevalence of these diabetes-related behaviors across racial and ethnic groups (13–24). However, almost none of this research involving Latinos analyzes data separately for Latino women, even though their lifetime risk of diabetes is almost 20% higher than Latino men (6). Data on the prevalence of diabetes-related behaviors in Latinas might improve diabetes prevention efforts in this population. Highly effective lifestyle programs to prevent diabetes by focusing on diet and physical activity already exist and have been studied in diverse populations (25).
Using a population-based sample from California (a state with ∼7 million Latinas) (26), we examined differences between Latinas and non-Latinas in the prevalence of six diabetes-related behaviors: walking, moderate to vigorous physical activity (MVPA), and consumption of fried potatoes, SSBs, desserts, and fast food. To make our findings useful to clinicians seeking to tailor diabetes prevention messages to Latinas, we compared this group to non-Latinas. Based on our literature review, we hypothesized that Latina ethnicity would be associated with less healthy dietary and physical activity behaviors, compared with non-Latina ethnicity.
RESEARCH DESIGN AND METHODS
Study population
We used data from the adult questionnaire of the 2009 California Health Interview Survey (CHIS), which is representative of the state’s noninstitutionalized civilian population 18 years of age or older. CHIS is a statewide, random-digit-dial telephone survey sampling household telephone numbers assigned to both landline and cellular service (27). One adult from each sampled household was randomly selected to complete an interview, conducted either in English, Spanish, Chinese, Vietnamese, or Korean. The overall response rate for the CHIS adult interview was 49% in 2009, which is comparable to other scientific telephone surveys conducted in California (27). Data were collected on 28,186 women, who were identified based on the question “Are you male or female?” After excluding women who reported having doctor-diagnosed diabetes and those currently pregnant, the analytic sample included 25,433 women: 4,321 Latinas (17.0%) and 21,112 non-Latinas (83.0%).
Diabetes-related behaviors
For each of six diabetes-related behaviors, we determined the cut point for the least healthy tertile for the entire analytic sample. We used a cut point to make our analysis of behavior differences between Latinas and non-Latinas more understandable and useful for practitioners. We selected the tertile as the cut point because there is no established level of these behaviors at which the risk of diabetes is known to sharply increase. In the current study, the least healthy tertile was defined as the lowest tertile for physical activity behaviors and the highest tertile for the dietary behaviors examined.
Two physical activity measures were evaluated. Participants were asked two questions about walking during the past week: “How many times did you walk to get some place that took you at least 10 minutes?” and “How many times did you walk for at least 10 minutes for fun, relaxation, exercise, or to walk the dog?” Responses to these two questions were added to make a single variable called “walking,” which was the total number of times per week the participant walked for at least 10 min for any purpose. Participants were asked about moderate physical activity during the previous week, such as bicycling, dancing, swimming, and gardening: “On how many days did you do any moderate physical activities in your free time for at least 10 minutes, other than walking?” In the same manner, participants were asked how many days in the last week they participated for at least 10 min in vigorous physical activities (ones that “take hard physical effort, such as aerobics, running, soccer, fast bicycling, or fast swimming”). Responses to these two questions were added to make a single variable, MVPA.
Four dietary behaviors were examined: consumption of fried potatoes, SSBs, desserts, and fast food. Participants were asked how many times in the last month they ate “any kind of fried potatoes, including French fries, home fries, or hash browns.” The monthly consumption of SSBs was assessed by combining the responses to questions about how many times they drank “regular soda or pop that contains sugar,” “sports or energy drinks such as Gatorade, Red Bull, and Vitamin water,” “sweetened fruit drinks such as Kool-aid, cranberry drink, and lemonade,” and “coffee or tea with sugar or honey added.” For each of these questions, respondents were reminded not to include diet options with artificial sweeteners.
Monthly “desserts” were assessed by combining responses to the following two questions: “How often did you eat cookies, cake, pie, or brownies?” and “How often did you eat ice cream or other frozen desserts?” Participants were instructed to not include sugar-free desserts. For fast food, participants were instructed to “include fast food meals eaten at work, home, or fast food restaurants, carryout or drive through.” The following examples were provided: McDonald’s, Panda Express, and Taco Bell. Participants were asked, “In the past seven days, how many times did you eat fast food?” Responses to this question were multiplied by 4.3 to estimate the total number of times fast food was eaten in the last month.
Latina ethnicity
Latina ethnicity was determined by the question “Are you Latino or Hispanic?” Women who responded “yes” were classified as Latinas, and those who answered “no” were classified as non-Latinas.
Other participant characteristics
We also examined seven characteristics of participants that might be related to both Latino ethnicity and the diabetes-related behaviors. These characteristics, which might confound the primary relationship under study, included the following: age, household income (expressed as percentage of the federal poverty threshold for household size), educational attainment, marital status, health status, smoking, and acculturation. For health status, respondents were asked “Would you say that in general your health is excellent, very good, good, fair, or poor?” Acculturation was assessed using a six-item measure developed and validated for use with CHIS (28). The six items addressed the following domains: 1) language (language spoken at home, language used to complete the survey, and self-reported English proficiency); 2) nativity; 3) duration of U.S. residence; and 4) citizenship status. An acculturation score was calculated according to the methods described by Van Wieren et al. (29), yielding scores that ranged from 6 to 19 in our sample. We divided the subjects into three acculturation levels: low (6–10), medium (11–17), and high (18,19). These cut points divided the Latina sample into tertiles of acculturation.
Data analysis
All analyses were conducted using Stata SE, version 11.0 (Stata Inc., College Station, TX). In all statistical testing, we used Stata survey commands, which adjust variance estimates to account for the complex sample design of the CHIS (30). All reported percentages were weighted. Overall, the proportion of subjects with missing data on any given variable was very low (<2% of sample). The investigators who prepared the publically available CHIS dataset used in our analysis used hotdeck- and regression-based methods to impute missing data for most study variables. Full procedures have been described elsewhere (27).
In all analyses involving the six diabetes-related behaviors, we used binary variables (the least healthy tertile vs. the other two tertiles). Our key independent variable, Latina ethnicity, was also binary (Latina vs. non-Latina). Using χ2 tests, we first examined the association between participant characteristics and Latina ethnicity, followed by the association of diabetes-related behaviors with Latina ethnicity. We then calculated the unadjusted odds of being in the least healthy tertile by each participant characteristic (potentially confounding variables). Using logistic regression models for each diabetes-related behavior, we calculated the odds of Latinas being in the least healthy tertile. These odds were adjusted in successive models, adding groups of potentially confounding variables to the unadjusted model: model 1 (age); model 2 (socioeconomic status; model 1 variable + household income, education, and marital status); model 3 (health-related factors; model 2 variables + health status and smoking status); and model 4 (acculturation; model 3 variables + acculturation). Age was added separately because of the large differences between Latinas and non-Latinas that, alone, might significantly confound the relationships under study. The variables in the socioeconomic and health groups were conceptually related and made a priori. We added these thematic groups of covariates into successive models to highlight their impact on the association between Latina ethnicity and the behavioral outcomes.
The study protocol was approved by the Temple University Institutional Review Board.
RESULTS
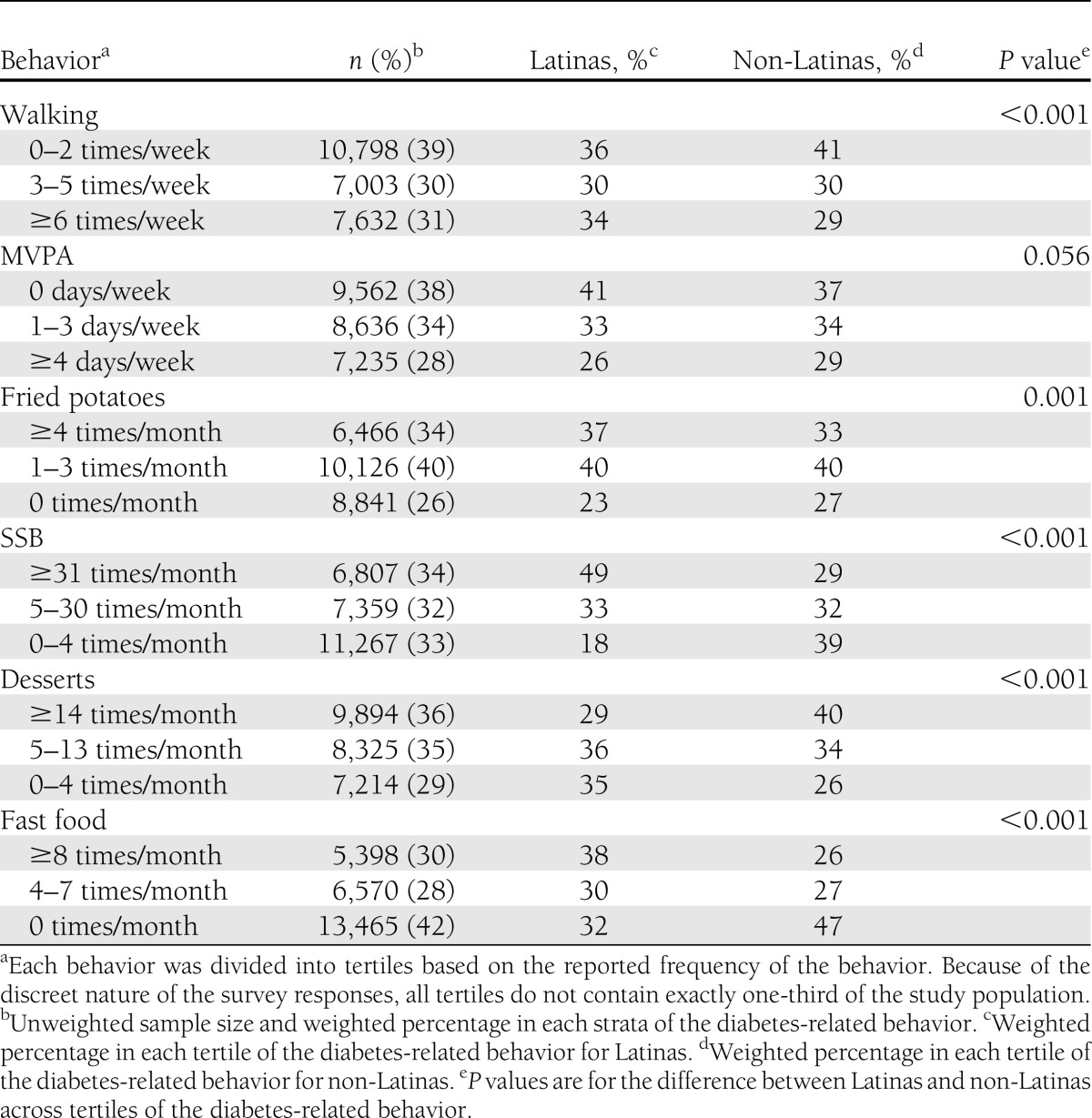
Compared with non-Latinas, Latinas were younger, less educated, had lower income, and reported poorer health (Table 1). Latinas were also less acculturated and less likely to smoke. Latinas were less likely than non-Latinas to be in the least healthy tertile for walking and dessert consumption, but they were more likely to be in the least healthy tertile for MVPA and the three other dietary behaviors: consuming fried potatoes, fast food, and SSBs (Table 2). These three behaviors were weakly correlated. The Spearman correlation coefficients between these behavior variables (continuous measures) were as follows: SSB and fried potato consumption (0.13, P < 0.001), SSB and fast food consumption (0.12, P < 0.001), and fast food and fried potato consumption (0.28, P < 0.001).
Table 1.
Participant characteristics by Latina ethnicity
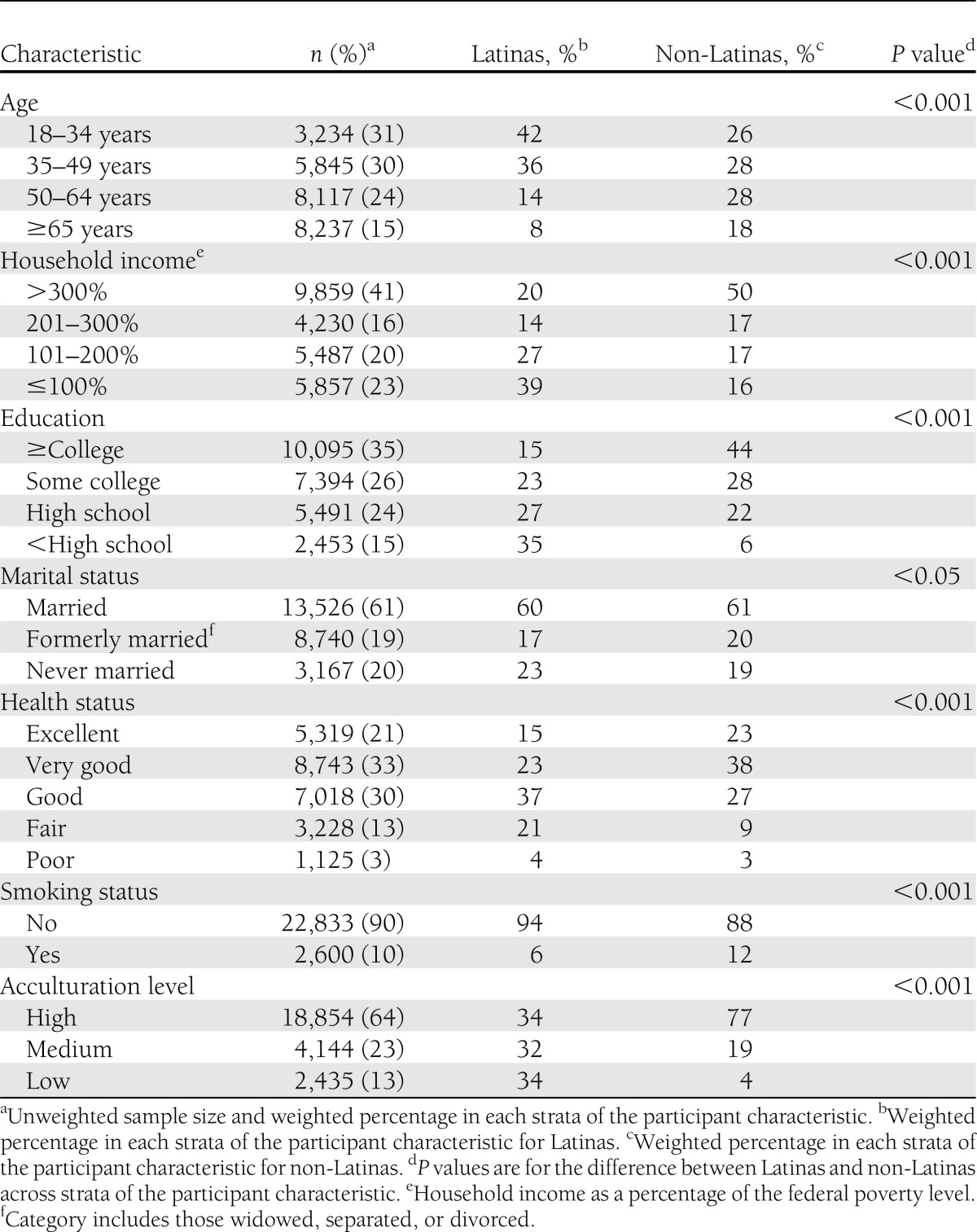
Table 2.
Diabetes-related behaviors by Latina ethnicity
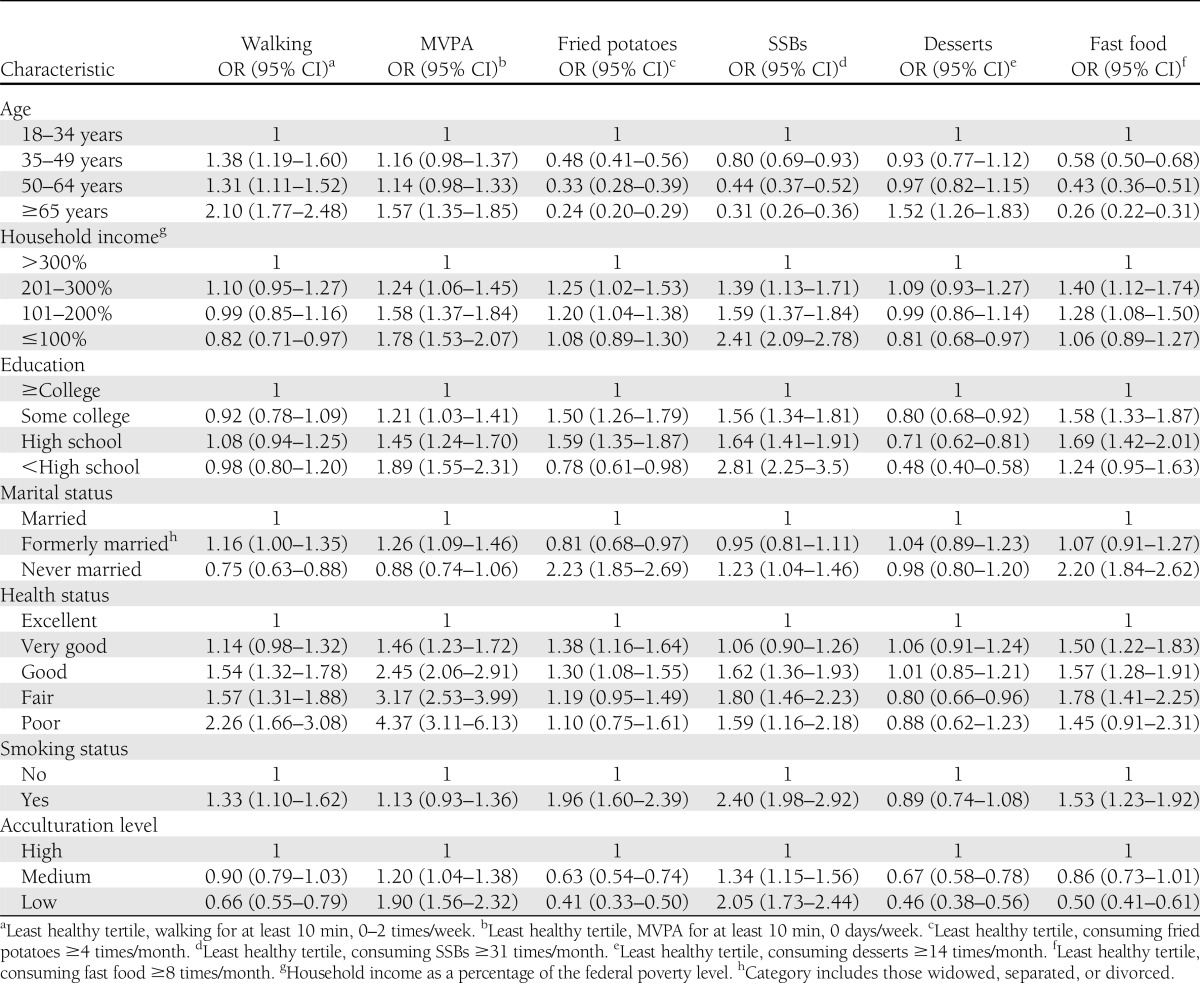
Increasing age was associated with poorer physical activity behaviors and improved dietary behaviors, with the exception of dessert consumption (Table 3). Those with lower incomes, less education, and poorer self-reported health were more likely to be in the least healthy tertile of MVPA and SSB consumption. Those with lower levels of acculturation and smokers were also more likely to be in the least healthy tertile of SSB consumption. However, those with lower levels of acculturation were less likely to be in the unhealthy tertile for fried potato or dessert consumption or for walking.
Table 3.
Unadjusted odds of being in the least healthy tertile for diabetes-related behaviors by participant characteristics
In unadjusted logistic regression analyses, the largest differences between Latinas and non-Latinas in unhealthy, diabetes-related behaviors were seen for SSB and fast food consumption (Table 4). The magnitude of the association between Latina ethnicity and these two dietary behaviors decreased after controlling for age (model 1). For SSBs, the association was further decreased by controlling for income, education, and marital status (model 2). Controlling both associations for health status and smoking (model 3) had little additional impact on the magnitude of these associations. Finally, adjusting for acculturation had different impacts on each of these associations (model 4), as would be predicted by 1) the different relationship of acculturation to fast food and SSB consumption (Table 3) and 2) the lower levels of acculturation among Latinas. In fully adjusted models (model 4), Latinas had a higher risk (odds ratio [OR] [95% CI]) of being in the least healthy tertile of fast food (1.94 [1.63–2.31]), SSB beverage (1.53 [1.29–1.82]), and fried potato consumption (1.32 [1.18–1.67]).
Table 4.
Odds of Latinas, compared with non-Latinas, of being in the least healthy tertile for diabetes-related behaviors
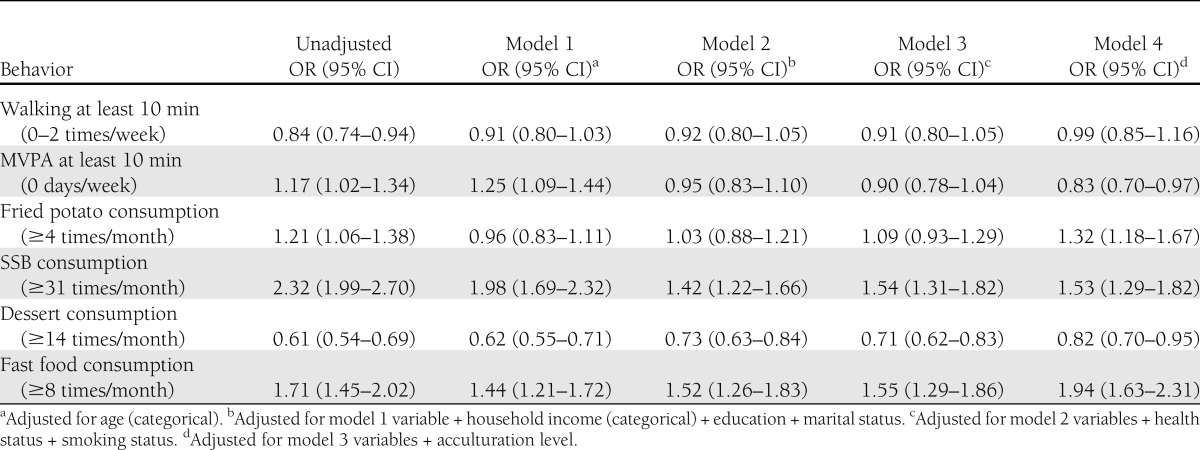
In fully adjusted models, Latinas had lower odds of being in the least healthy tertile for two of the six diabetes-related behaviors: dessert consumption (OR 0.82 [95% CI 0.70–0.95]) and MVPA (0.83 [0.70–0.97]). The latter association emerged only after adjusting for confounding variables. In the fully adjusted model, there was no difference between Latinas and non-Latinas with respect to walking (0.99 [0.85–1.16]).
We conducted several additional analyses for which data are not shown. All of the adjusted differences in diabetes-related behaviors between Latinas and non-Latinas (Table 4) were larger in separate analyses comparing Latinas to non-Latina whites, the largest racial subgroup of non-Latinas. By restricting our multivariate models to Mexican-American Latinas vs. non-Latinas, the results were unchanged from those including all Latinas. We addressed the potential role of obesity as a confounder by controlling our final multivariate models for obesity status, and we assessed obesity as an effect modifier by running these final models separately for obese and nonobese subjects. We found no evidence that obesity was either a confounder or an effect modifier of the relationships between the health behaviors and Latina ethnicity.
CONCLUSIONS
Our study shows significant differences between Latinas and non-Latinas with respect to all diabetes-related behaviors examined, except walking. Compared with non-Latinas, Latinas had higher odds of being frequent consumers of fried potatoes, SSBs, and fast food. Of these unhealthy dietary behaviors, the association with Latina ethnicity was largest for SSBs and fast food. Although age, socioeconomic status, and acculturation confounded these relationships, the fully adjusted association of Latina ethnicity with poor dietary behaviors suggests an independent effect of being Latina on consuming these unhealthy food groups. Latinas had lower odds of eating desserts frequently compared with non-Latinas. After adjusting for all covariates, Latina ethnicity was only modestly associated with MVPA. There was no association of Latina ethnicity with walking in the fully adjusted model.
The greatest strength of this study is its inclusion of a large number of Latinas, who have smaller representation in other large datasets. Studying 4,321 Latinas helped produce reliable estimates of this population’s diabetes-related behaviors, and the association of those behaviors with Latina ethnicity. Using this large Latina cohort, we have produced some of the first reports of the prevalence of six diabetes-related behaviors in this high-risk population. Another strength of our study is the potential clinical utility of the behavioral outcomes examined here. We analyzed these diabetes-related behaviors on a scale that we believe is most meaningful and useful to clinicians, compared with more complex metrics that are difficult to incorporate into lifestyle counseling efforts. Because Latinos’ health behaviors are influenced by acculturation (31), our use of a validated acculturation measure represents another potential strength. However, this measure does not incorporate questions about cognitive, spiritual, or emotional factors, which are part of the acculturation process.
The cross-sectional nature of this study hinders our ability to draw causal inferences about the impact of Latina ethnicity on diabetes-related behaviors. The data are from California, where the proportion of Latinas who are Mexican American (77%) is higher than national estimates (65%), which may limit the ability to generalize our findings (26). The number of Latinas from other countries was too small to permit subgroup analyses in our study. In CHIS, the use of different time frames (week and month) for the dietary measures and the long recall period of one month might have resulted in inaccurate responses. However, we do not have reason to believe that these inaccuracies would have differed between Latinas and non-Latinas.
Our choice of non-Latinas as a comparison group masks differences in diabetes-related behaviors among whites, blacks, and Asians who comprise that group. Including blacks in this group (who exhibit high levels of physical inactivity and consumption of energy-dense, nutrient-poor foods) (32) underestimates differences in diabetes-related behaviors between women at the highest risk (i.e., Latinas) and those at lowest risk (i.e., whites). Our sensitivity analysis comparing behavioral outcomes between Latinas and white women yielded greater differences in the same diabetes-related behaviors than those reported between Latinas and non-Latinas. The observed behavioral differences between Latinas and non-Latinas may be explained, in part, by cultural differences between these groups, which we could not measure in the current study. Some have suggested that Latino Americans consider consuming fast food and SSBs as a status symbol, which may influence their consumption of these foods (33). Cultural perceptions such as these should be explored further in future research.
Although previous studies have examined racial and ethnic differences in the same diabetes-related dietary behaviors studied here, most did not stratify analyses by sex. The only study reporting any of these dietary behaviors in Latinas found that ∼50% of Mexican-American women drink regular soda (13). Latinas in our study consumed more SSBs than non-Latinas. In contrast, a national study by Bleich et al. (14) estimated that Mexican-American adults consume fewer calories from SSBs than whites or African Americans. The different scales used to measure SSB consumption and our exclusion of Latino males may help explain these differences. Other national studies (13,15,17) that have explored SSB consumption in Latinos found similar levels to those reported by Bleich et al. These studies included only Mexican Americans, whereas ours included Latinas from other Latin American countries. However, our results were unchanged when we restricted our analysis to Mexican-American women. Latinos in California may have different patterns of SSB consumption than Latinos in other parts of the country, which may also help explain the observed discrepancy with nationally representative studies.
Almost no research has focused on the differences in fast food consumption between Latinos and non-Latinos. One study reported a lower prevalence of fast food consumption in Latinos compared with non-Hispanic blacks and whites; however the authors did not adjust for potential confounders in their analysis (22). In our study, the association of Latina ethnicity with fast food consumption was higher than for any other dietary behavior we examined. Acculturation was strongly and positively associated with eating fast food in our cohort (Table 3). This finding is consistent with those from the few studies that have examined acculturation and fast food consumption within Latinos (17,34,35). With respect to the other dietary behaviors studied here, we found that Latinas eat desserts less frequently than non-Latinas, which is consistent with previous reports (20,21). However, our study and previous ones have not included questions about culturally specific desserts for Latinas, such as dulce de leche and flan, which could lead to an underestimation of the frequency of consuming desserts among Latinas. We found that Latinas consume fried potatoes more frequently than non-Latinas, in contrast to two previous studies (13,20) that examined French fries as the only form of fried potatoes.
In contrast to the diet literature in U.S. Latinos, the physical activity literature has placed a greater focus on Latinas by either restricting analyses to this group (19,24), stratifying race/ethnicity analyses by sex (16), or stratifying sex-based analyses by race/ethnicity (23). In our analysis (Table 2), 41% of Latinas reported no MVPA, which was almost identical to previous reports (16,23). After adjusting for covariates, however, we found that Latinas were somewhat less likely to have low levels of MVPA than non-Latinas. In our cohort, lower levels of income, educational attainment, health status, and acculturation were associated with less MVPA and Latina ethnicity. Adjusting for these factors in our analysis may explain why Latina ethnicity was associated with a reduced risk of low MVPA. We found that Latinas walked more frequently than non-Latinas in our unadjusted analysis, which may reflect increased active transportation and occupational walking in Latinas (36), in addition to the negative association of acculturation with walking in this population (37). After adjusting for acculturation and other covariates in our multivariate model, there was no association between Latina ethnicity and walking.
In conclusion, our study has identified two diabetes-related behaviors (SSB and fast food consumption) that are more frequently performed by Latinas than non-Latinas, and may therefore represent important behavioral targets for diabetes prevention efforts in Latinas. These specific dietary behaviors may be particularly effective targets for lifestyle counseling by diverse health professionals. Given the limited time they devote to diabetes prevention with at-risk patients (38), physicians may find such discrete dietary targets useful. As another example, certified diabetes educators and nutritionists may choose to focus on fast food and SSB consumption when taking more detailed dietary histories and making dietary recommendations for Latinas. Future research should assess how best to incorporate messages about reducing SSB and fast food consumption into clinical encounters and community-based diabetes prevention programs targeting Latinas. Effectively reducing SSB and fast food consumption among Latinas will also require further qualitative research to understand the social context surrounding these diabetes-related behaviors, and the role that SSBs and fast food play in Latinas’ lives.
Acknowledgments
This study was funded by the Temple University Department of Medicine Faculty Development Research Award.
No potential conflicts of interest relevant to this article were reported.
M.J.O. was responsible for the study concept and design, acquisition of the data, analysis and interpretation of the data, drafting of the manuscript, and critical revision of the manuscript. A.D. helped with the study concept and design, data analysis, and manuscript revision. V.A.A. provided critical revision of the manuscript and prepared the manuscript for submission. R.C.W. contributed to the study concept and design, analysis and interpretation of the data, and critical revision of the manuscript. M.J.O. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This study was presented in abstract form at the 72nd Scientific Sessions of the American Diabetes Association, Philadelphia, Pennsylvania, 8–12 June 2012.
The authors would like to thank Drs. Jennifer O. Fisher and Gary D. Foster (Temple University) for their comments on a previous draft of the manuscript. The authors would also like to thank Sara Shuman (Temple University) for her assistance in preparing the final version of the manuscript.
References
- 1.Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States [article online], 2011. Available from www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf Accessed 23 February 2012
- 2.Dall TM, Zhang YD, Chen YJ, Quick WW, Yang WG, Fogli J. The economic burden of diabetes. Health Aff (Millwood) 2010;29:297–303 [DOI] [PubMed] [Google Scholar]
- 3.Cowie CC, Rust KF, Ford ES, et al. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988-1994 and 2005-2006. Diabetes Care 2009;32:287–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Narayan KM, Boyle JP, Geiss LS, Saaddine JB, Thompson TJ. Impact of recent increase in incidence on future diabetes burden: U.S., 2005-2050. Diabetes Care 2006;29:2114–2116 [DOI] [PubMed] [Google Scholar]
- 5.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA 2010;303:235–241 [DOI] [PubMed] [Google Scholar]
- 6.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA 2003;290:1884–1890 [DOI] [PubMed] [Google Scholar]
- 7.Liese AD, Weis KE, Schulz M, Tooze JA. Food intake patterns associated with incident type 2 diabetes: the Insulin Resistance Atherosclerosis Study. Diabetes Care 2009;32:263–268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pereira MA, Kartashov AI, Ebbeling CB, et al. Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis. Lancet 2005;365:36–42 [DOI] [PubMed] [Google Scholar]
- 9.Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA 2004;292:927–934 [DOI] [PubMed] [Google Scholar]
- 10.Johnson RK, Appel LJ, Brands M, et al. American Heart Association Nutrition Committee of the Council on Nutrition, Physical Activity, and Metabolism and the Council on Epidemiology and Prevention Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 2009;120:1011–1020 [DOI] [PubMed] [Google Scholar]
- 11.Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care 2007;30:744–752 [DOI] [PubMed] [Google Scholar]
- 12.Knowler WC, Barrett-Connor E, Fowler SE, et al. Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Batis C, Hernandez-Barrera L, Barquera S, Rivera JA, Popkin BM. Food acculturation drives dietary differences among Mexicans, Mexican Americans, and Non-Hispanic Whites. J Nutr 2011;141:1898–1906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bleich SN, Wang YC, Wang Y, Gortmaker SL. Increasing consumption of sugar-sweetened beverages among US adults: 1988-1994 to 1999-2004. Am J Clin Nutr 2009;89:372–381 [DOI] [PubMed] [Google Scholar]
- 15.Carrera PM, Gao XA, Tucker KL. A study of dietary patterns in the Mexican-American population and their association with obesity. J Am Diet Assoc 2007;107:1735–1742 [DOI] [PubMed] [Google Scholar]
- 16.Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Prev Med 2000;18:46–53 [DOI] [PubMed] [Google Scholar]
- 17.Duffey KJ, Gordon-Larsen P, Ayala GX, Popkin BM. Birthplace is associated with more adverse dietary profiles for US-born than for foreign-born Latino adults. J Nutr 2008;138:2428–2435 [DOI] [PubMed] [Google Scholar]
- 18.Duffey KJ, Gordon-Larsen P, Steffen LM, Jacobs DR, Jr, Popkin BM. Regular consumption from fast food establishments relative to other restaurants is differentially associated with metabolic outcomes in young adults. J Nutr 2009;139:2113–2118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evenson KR, Sarmiento OL, Tawney KW, Macon ML, Ammerman AS. Personal, social, and environmental correlates of physical activity in North Carolina Latina immigrants. Am J Prev Med 2003;25(Suppl. 1):77–85 [DOI] [PubMed] [Google Scholar]
- 20.Gans KM, Burkholder GJ, Risica PM, Lasater TM. Baseline fat-related dietary behaviors of white, Hispanic, and black participants in a cholesterol screening and education project in New England. J Am Diet Assoc 2003;103:699–706; discussion 706 [DOI] [PubMed] [Google Scholar]
- 21.Kant AK. Consumption of energy-dense, nutrient-poor foods by adult Americans: nutritional and health implications. The third National Health and Nutrition Examination Survey, 1988-1994. Am J Clin Nutr 2000;72:929–936 [DOI] [PubMed] [Google Scholar]
- 22.Paeratakul S, Ferdinand DP, Champagne CM, Ryan DH, Bray GA. Fast-food consumption among US adults and children: dietary and nutrient intake profile. J Am Diet Assoc 2003;103:1332–1338 [DOI] [PubMed] [Google Scholar]
- 23.Sundaram AA, Ayala C, Greenlund KJ, Keenan NL. Differences in the prevalence of self-reported risk factors for coronary heart disease among American women by race/ethnicity and age: Behavioral Risk Factor Surveillance System, 2001. Am J Prev Med 2005;29(Suppl. 1):25–30 [DOI] [PubMed] [Google Scholar]
- 24.Wilbur J, Chandler PJ, Dancy B, Lee H. Correlates of physical activity in urban Midwestern Latinas. Am J Prev Med 2003;25(Suppl. 1):69–76 [DOI] [PubMed] [Google Scholar]
- 25.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff (Millwood) 2012;31:67–75 [DOI] [PubMed] [Google Scholar]
- 26.Ennis S, Ríos-Vargas M, Albert N. The Hispanic Population: 2010 Census Briefs Washington, DC, U.S. Department of Commerce, 2011 (Census publ. no. C2010BR-04) [Google Scholar]
- 27.UCLA Center for Health Policy Research. California Health Interview Survey 2009 Methodology Series: Report 3–data processing procedures [article online], 2011. Available from www.chis.ucla.edu/pdf/CHIS2009_method3.pdf Accessed 14 February 2012
- 28.Johnson-Kozlow M. Colorectal cancer screening of Californian adults of Mexican origin as a function of acculturation. J Immigr Minor Health 2010;12:454–461 [DOI] [PubMed] [Google Scholar]
- 29.Van Wieren AJ, Roberts MB, Arellano N, Feller ER, Diaz JA. Acculturation and cardiovascular behaviors among Latinos in California by country/region of origin. J Immigr Minor Health 2011;13:975–981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.UCLA Center for Health Policy Research. California Health Interview Survey 2009 Methodology Series: Report 5–weighting and variance estimation [article online], 2011. Available from www.chis.ucla.edu/pdf/CHIS2009_method5.pdf Accessed 23 February 2012
- 31.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health 2005;26:367–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berg CJ, Thomas JL, An LC, et al. Change in smoking, diet, and walking for exercise in blacks. Health Educ Behav 2012;39:191–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freeman A. Fast food: oppression through poor nutrition. Calif Law Rev 2007;95:2221–2259 [Google Scholar]
- 34.Unger JB, Reynolds K, Shakib S, Spruijt-Metz D, Sun P, Johnson CA. Acculturation, physical activity, and fast-food consumption among Asian-American and Hispanic adolescents. J Community Health 2004;29:467–481 [DOI] [PubMed] [Google Scholar]
- 35.Sharkey JR, Johnson CM, Dean WR. Nativity is associated with sugar-sweetened beverage and fast-food meal consumption among Mexican-origin women in Texas border colonias. Nutr J 2011;10:101–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bensley L, VanEenwyk J, Centers for Disease Control and Prevention (CDC) Contribution of occupational physical activity toward meeting recommended physical activity guidelines: United States, 2007. MMWR Morb Mortal Wkly Rep 2011;60:656–660 [PubMed] [Google Scholar]
- 37.Berrigan D, Dodd K, Troiano RP, Reeve BB, Ballard-Barbash R. Physical activity and acculturation among adult Hispanics in the United States. Res Q Exerc Sport 2006;77:147–157 [DOI] [PubMed]
- 38.Geiss LS, James C, Gregg EW, Albright A, Williamson DF, Cowie CC. Diabetes risk reduction behaviors among U.S. adults with prediabetes. Am J Prev Med 2010;38:403–409 [DOI] [PubMed] [Google Scholar]


