Abstract
Following the international guidelines criteria an adequate “diagnostic conclusion” of inflammatory bowel disease (IBD) can be achieved only if clinical, endoscopic and laboratory findings, together with sample technical adequacy and unequivocal histomorphological signs of the disease are available. Thus, a conclusive diagnosis requires a complex combination of clinical, endoscopic and histological data. A considerable number of endoscopic biopsies obtained from IBD patients do not meet the above-mentioned requirements. The aim of the present proposal is to introduce a binary system of evaluation in the “diagnostic conclusion” of the histopathological report that will help to simplify the clinical decisions and consequent patient management. In patients with no history of disease, the pathologist should classify the biopsies in “Diagnostic”, when the criteria established by the international guidelines are satisfied and “not diagnostic” when one or more of the above-mentioned criteria are not met. The term “not diagnostic” should replace “highly suggestive” and “probable”. This new terminology could avoid ambiguous expressions that encourage the clinician to classify the patient as affected by IBD without fulfilling all of the requirements for an accurate diagnostic approach.
Keywords: Inflammatory bowel disease, Diagnosis, Biopsy
TO THE EDITOR
Various guidelines have defined the criteria used for the diagnostic evaluation of endoscopic biopsies as chronic idiopathic inflammatory bowel disease (IBD)[1-5].
Most of these guidelines include a “preliminary section” of the histological report that includes the evaluation of the different morphological parameters of the biopsy specimen and a final section with the “diagnostic conclusion” derived from the previous synoptic analyses. In practice, the adequate diagnosis of colon biopsy specimens for non-neoplastic disease requires the following parameters: (1) clinical, endoscopic, and laboratory findings; and (2) technical adequacy of endoscopic sampling and histological procedures, particularly a proper orientation of the biopsies[3]; and unequivocal evidence of specific morphological signs of the disease in histological analysis[5-7].
Thus, a conclusive diagnosis requires a complex combination of clinical, endoscopic and histological data. Consequently, a considerable number of endoscopic biopsies obtained from IBD patients do not meet the above-mentioned requirements and cannot receive a definite histological diagnosis. In the more recent guidelines, the categories “highly suggestive[1] and “probable”[6] in the final section of the diagnostic report encompass all of these cases. Although these terms are ambiguous, they are often interpreted as a definitive diagnosis for the clinical management of patients with endoscopy suggestive for IBD.
The aim of the present proposal is to introduce a binary system of evaluation in the “diagnostic conclusion” section that will help to simplify the clinical decisions and consequent patient management. For this purpose, patients without a previous histological diagnosis of IBD and patients with a previous unequivocal diagnosis of IBD should be approached differently.
In patients with no history of disease, the pathologist should use the following terms to classify the biopsies.
Diagnostic, when the criteria established by the international guidelines[1,2] for the diagnosis of IBD are satisfied: (1) complete or extensive mapping of ileo-colonic segments; (2) adequate specimens, correctly oriented; (3) adequate information, including clinical history, laboratory data, and previous histological and/or endoscopic reports; and (4) histological examination of specimens shows unequivocal microscopic signs of the disease (diagnostic for IBD) or definitely rules out the diagnosis of IBD (negative for IBD). If possible, the pathologist should specify the type of the non-IBD colitis (infective, drug-induced, lymphocytic, collagenous, etc.).
Not diagnostic, when one or more of the above-mentioned criteria are not met. The term “not diagnostic” should replace “highly suggestive”[1] and “probable”[6]. After discussion with the gastroenterologist and the endoscopist, these patients should be re-evaluated. In cases with persistent symptoms, the patient should be sent back to endoscopy with the goal of achieving diagnostic biopsies. IBD shows a distinctive microscopic morphology only after 2-3 wk[8], which should be considered in the timing of subsequent biopsies.
In cases of a previous unequivocal diagnosis of IBD performed in the same institution (or in a different center, if specimens are available for revision), the sampling requirements are less stringent and more dependent on endoscopy. The categories “diagnostic/not diagnostic” in the final section of the report are not required, but the report should include an evaluation of disease activity, the presence or absence of dysplasia, and the presence or absence of Cytomegalovirus (follow-up evaluation). Figure 1 provides an example of an algorithm used for this classification.
Figure 1.
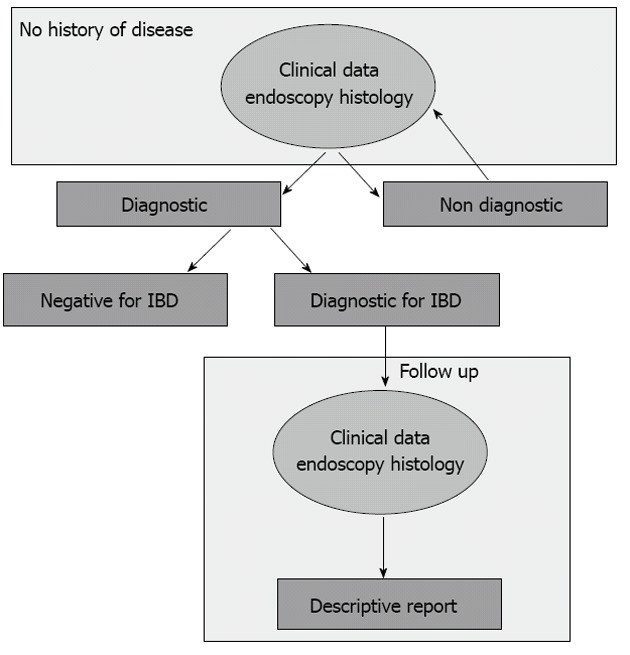
A graphic representation of the described terms (boxes) with suggestions for clinical management. IBD: Inflammatory bowel disease.
In our opinion, the advantages of using this binary system to approach endoscopic biopsies in IBD are the following: (1) this terminology could avoid ambiguous expressions that encourage the clinician to classify the patient as affected by IBD without fulfilling all of the requirements for an accurate diagnostic approach; (2) a second set of biopsies after a “not diagnostic” result should simplify the differential diagnosis from non-IBD colitis. Moreover, after the first set of biopsies, the clinician may be able to collect other data (laboratory data, response to therapy, etc.) that are useful for diagnosis; (3) this approach will reduce the use of inappropriate treatments that might cause mucosal changes, which can complicate the histological evaluation and compromise the correct assessment of the patient[8]; and (4) last, but not least, the quality of clinical and biological studies should be improved by including only case series with a definitive diagnosis.
The final goal of our proposal is to seek comments and suggestions about this topic and share this approach with other authors.
Footnotes
Supported by Fondazione Malattie Infiammatorie Intestinali (IBD) Onlus - Torino; Compagnia San Paolo, Torino
P- Reviewers Rocha R, Tanaka T, Ukleja A, Wirth S S- Editor Song XX L- Editor A E- Editor Li JY
References
- 1.Cornaggia M, Leutner M, Mescoli C, Sturniolo GC, Gullotta R. Chronic idiopathic inflammatory bowel diseases: the histology report. Dig Liver Dis. 2011;43 Suppl 4:S293–S303. doi: 10.1016/S1590-8658(11)60585-9. [DOI] [PubMed] [Google Scholar]
- 2.Van Assche G, Dignass A, Panes J, Beaugerie L, Karagiannis J, Allez M, Ochsenkühn T, Orchard T, Rogler G, Louis E, et al. The second European evidence-based Consensus on the diagnosis and management of Crohn’s disease: Definitions and diagnosis. J Crohns Colitis. 2010;4:7–27. doi: 10.1016/j.crohns.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 3.Bryan F, Warren , Neil A. Sheperd. What are the controversies in histopathological diagnosis ? In: Jewell DP, Warren BF, Mortensen NJ. Challenges in Inflammatory Bowel Disease; 2001. Available from: http: //trove.nla.gov.au/work/20355368?selectedversion=NBD28674755. [Google Scholar]
- 4.Jenkins D, Balsitis M, Gallivan S, Dixon MF, Gilmour HM, Shepherd NA, Theodossi A, Williams GT. Guidelines for the initial biopsy diagnosis of suspected chronic idiopathic inflammatory bowel disease. The British Society of Gastroenterology Initiative. J Clin Pathol. 1997;50:93–105. doi: 10.1136/jcp.50.2.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vilela EG, Torres HO, Martins FP, Ferrari Mde L, Andrade MM, Cunha AS. Evaluation of inflammatory activity in Crohn’s disease and ulcerative colitis. World J Gastroenterol. 2012;18:872–881. doi: 10.3748/wjg.v18.i9.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanaka M, Saito H, Fukuda S, Sasaki Y, Munakata A, Kudo H. Simple mucosal biopsy criteria differentiating among Crohn disease, ulcerative colitis, and other forms of colitis: measurement of validity. Scand J Gastroenterol. 2000;35:281–286. doi: 10.1080/003655200750024155. [DOI] [PubMed] [Google Scholar]
- 7.Tanaka M, Riddell RH, Saito H, Soma Y, Hidaka H, Kudo H. Morphologic criteria applicable to biopsy specimens for effective distinction of inflammatory bowel disease from other forms of colitis and of Crohn’s disease from ulcerative colitis. Scand J Gastroenterol. 1999;34:55–67. doi: 10.1080/00365529950172844. [DOI] [PubMed] [Google Scholar]
- 8.Geboes K. Pathology of inflammatory bowel diseases (IBD): variability with time and treatment. Colorectal Dis. 2001;3:2–12. doi: 10.1046/j.1463-1318.2001.00187.x. [DOI] [PubMed] [Google Scholar]


