Abstract
We report a diabetic patient with bilateral Descemet's membrane (DM) detachment after successive phacoemulsification. The DM detachments were diagnosed and documented in early postoperative period using anterior segment optical coherence tomography (OCT) and managed successfully by descemetopexy using 14% C3F8. This case highlights that some patients may be anatomically predisposed to DM detachment. Careful preoperative examination including specular microscopy should be done preoperatively especially in diabetic patients.
Keywords: Anterior segment optical coherence tomography, Descemet's membrane detachment, diabetes
Descemet's membrane (DM) detachment occurring during cataract surgery is not uncommon. However some patients may be predisposed to it. There have been few case reports of patients developing DM detachment after uneventful cataract surgery, leading to speculation that there may be an anatomic predisposition for this complication.[1,2] We report a patient with diabetes mellitus who developed bilateral DM detachment after uneventful phacoemulsification.
Case Report
A 65-year-old male presented to our clinic for cataract surgery. He was a known case of diabetes mellitus since 5 years that was well controlled with oral antidiabetic drugs. The preoperative fasting and postprandial blood sugar status was found to be within normal limits. The preoperative best corrected visual acuity (BCVA) was 20/120 in the right eye and 20/80 in the left eye. The preoperative slit lamp biomicroscopic examination revealed posterior subcapsular cataract in both eyes. Fundus examination using indirect ophthalmoscope was normal in both eyes. Specular microscopy revealed a cell density of 1984/mm2 in the right eye and 1934/mm2 in the left eye, and coefficient of variation (CV) of 0.35 in the right eye and 0.32 in the left eye. Ultrasonic pachymetry revealed central corneal thickness of 0.57 mm in the right eye and 0.58 mm in the left eye.
Patient underwent phacoemulsification and intraocular lens implantation under peribulbar anesthesia, using a temporal scleral tunnel approach in his right eye. A dispersive viscoelastic (sodium chondroitin sulfate, 4%; sodium hyaluronate, 3%) was used during the surgery considering the low cell count. No intraoperative complications were noted. On postoperative day 1, the BCVA in the right eye was 20/400. Slit lamp examination revealed diffuse corneal edema and DM detachment extending from the temporal sclerocorneal tunnel wound and involving most of the cornea. Anterior segment optical coherence tomography (OCT) was done for documentation [Fig. 1]. The central corneal thickness was unrecordable. Considering the large extent of DM detachment, a decision was taken to do descemetopexy. On the same day, 14% C3F8 was injected into the anterior chamber of the right eye through inferotemporal limbal paracentesis track in the operation room. Visual acuity and central corneal thickness gradually improved to 20/40 and 0.586 mm, respectively, over a period of 3 weeks.
Figure 1.
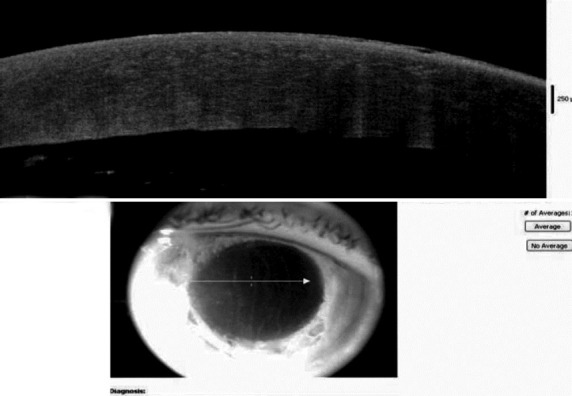
Anterior segment optical coherence tomography photograph of right eye on first postoperative day showing Descemet's membrane detachment
Two months after the first surgery, the patient underwent phacoemulsification and intraocular lens implantation in his left eye. The surgery was performed by the same surgeon with extreme caution, using a temporal scleral tunnel approach. A dispersive viscoelastic (sodium chondroitin sulfate, 4%; sodium hyaluronate, 3%) was used during the surgery. No intraoperative complications were noted. On first postoperative day, the visual acuity in his right eye was 20/40 and in the left eye was counting fingers at 3 feet. Slit lamp examination revealed diffuse corneal edema and DM detachment involving most of the cornea in his left eye. Anterior segment OCT was done for documentation [Fig. 2]. The central corneal thickness was 0.896 mm in the left eye. On the same day, descemetopexy was done using 14% C3F8, injected into the anterior chamber through inferotemporal limbal paracentesis track. Postoperative period was uneventful. Visual acuity and central corneal thickness improved gradually to 20/30 and 0.596 mm, respectively, over a period of 3 weeks. In both eyes, C3F8 bubble took about 2 weeks to disappear completely from the anterior chamber. Anterior segment OCT photograph was taken in both eyes 3 weeks postoperatively [Figs. 3 and 4].
Figure 2.
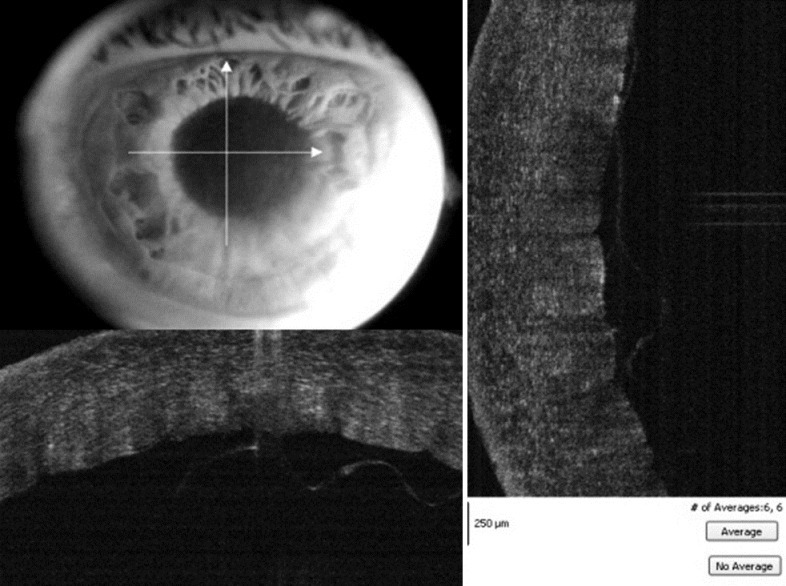
Anterior segment optical coherence tomography photograph of left eye on first postoperative day showing Descemet's membrane detachment
Figure 3.
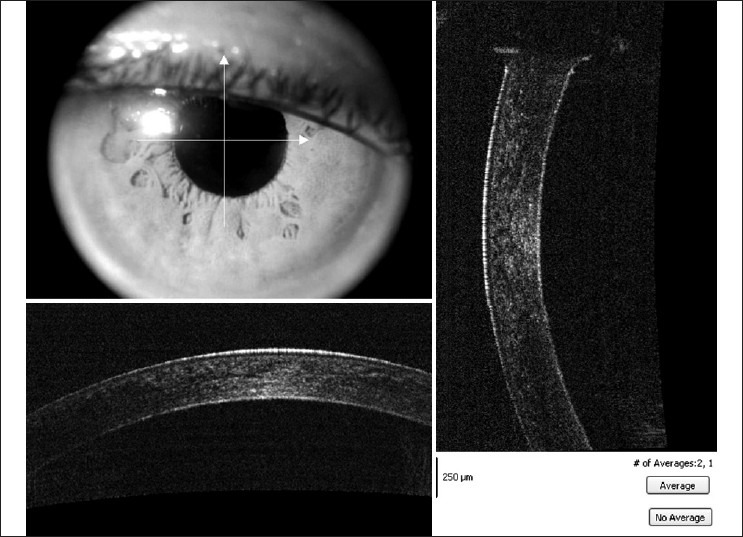
Anterior segment photograph of the right eye 3 weeks postoperatively
Figure 4.
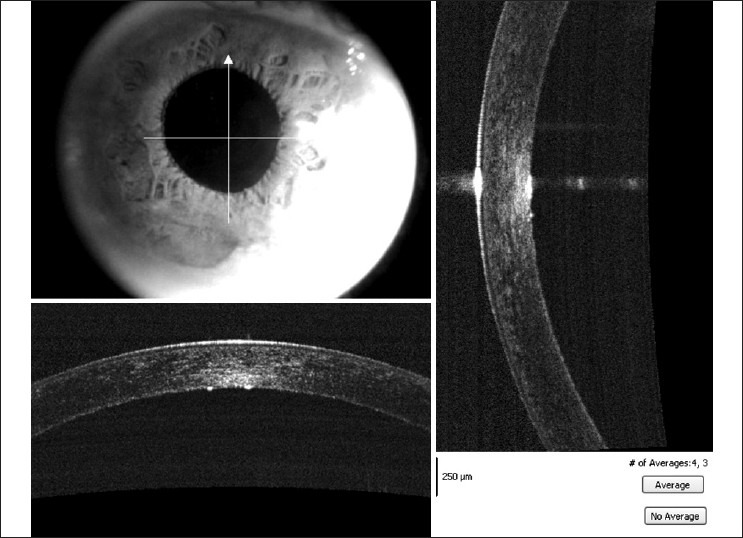
Anterior segment photograph of the left eye 3 weeks postoperatively
Discussion
Bilateral DM detachment after uneventful cataract surgery has been reported in literature.[1,2] An anatomical predisposition to DM detachment possibly because of an abnormality in the fibrillary stromal attachment to DM has been speculated.[1] Fang et al.[3] reported a case of bilateral DM detachment with documented preoperative abnormalities of the corneal endothelium. In our case, we compared the specular microscopic parameters with 10 age-matched healthy controls, coming to our clinic for routine check-up. Both eyes in our patient had a higher mean cell area (0.565 mm2 in the right eye and 0.576 mm2 in the left eye compared with mean ± SD, 0.389 ± 0.47 mm2) and lower cell density (1984/mm2 in right eye and 1934/mm2 in left eye compared with mean ± SD, 2537 ± 536/mm2) as compared to age-matched controls.
Studies have shown that baseline corneal thickness may be increased in diabetes.[4] Waite and Beetham have reported the occurrence of minute folds in Descemet's membrane in diabetic patients.[5] Diabetic corneas may also exhibit increased polymegathism and pleomorphism.[6] Inspite of altered corneal endothelial morphology, a causal correlation between diabetes and DM detachment has never been established.To the best of our knowledge, this is the first reported case of DM detachment after phacoemulsification in a patient of diabetes.
Although bilateral DM detachment after phacoemulsification has been previously reported, our case further supports anatomic predisposition in some patients. We suggest that a careful preoperative examination including specular microscopy should be done, especially in diabetics. Anterior segment OCT has an important role in timely diagnosis and documentation of DM detachment, and early postoperative intervention results in better visual outcome.
Footnotes
Source of Support: Nil.
Conflict of Interest: No.
References
- 1.Kansal S, Sugar J. Consecutive descemet membrane detachment after successive phacoemulsification. Cornea. 2001;20:670–1. doi: 10.1097/00003226-200108000-00025. [DOI] [PubMed] [Google Scholar]
- 2.Kim T, Sorenson A. Bilateral descemet membrane detachments. Arch Ophthalmol. 2000;118:1302–3. doi: 10.1001/archopht.118.9.1302. [DOI] [PubMed] [Google Scholar]
- 3.Fang JP, Amesur KB, Baratz KH. Preexisting endothelial abnormalities in bilateral postoperative Descemet membrane detachment. Arch Ophthalmol. 2003;121:903–4. doi: 10.1001/archopht.121.6.903. [DOI] [PubMed] [Google Scholar]
- 4.Busted N, Olsen T, Schmitz O. Clinical observations on the corneal thickness and the corneal endothelium in diabetes mellitus. Br J Ophthalmol. 1981;65:687–90. doi: 10.1136/bjo.65.10.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waite JH, Beetham WP. The visual mechanism in diabetes mellitus. N Engl J Med. 1935;212:367–429. [Google Scholar]
- 6.Schultz RO, Matsuda M, Yee RW, Edelhauser HF, Schultz KJ. Corneal endothelial changes in type I and type II diabetes mellitus. Am J Ophthalmol. 1984;98:401–10. doi: 10.1016/0002-9394(84)90120-x. [DOI] [PubMed] [Google Scholar]


