Abstract
Optimal management of menopause requires the expertise of a multi-disciplinary health team, each equipped with different skills necessary for the patient to enjoy optimal quality of life. A holistic approach is required to manage menopause. Holistic approach conceptualizes the involvement of patient's physical, psychological and social needs while planning therapy. It not only includes the biological aspect of menopause, but also the impact of psychosocial factors on diagnosis and therapy, as well as diet, exercise, nutraceuticals and other forms of therapy. Holistic care of menopause implies a patient centered approach which utilizes available health care resources to meet all medical, surgical, and psychological needs of the patient, using a variety of non pharmacological and drug therapies, while involving all concerned stakeholders to optimize the patient's micro and macro-environment.
Keywords: Menopause, nutraceuticals, patient centric care, patient empowerment, quality of life
INTRODUCTION
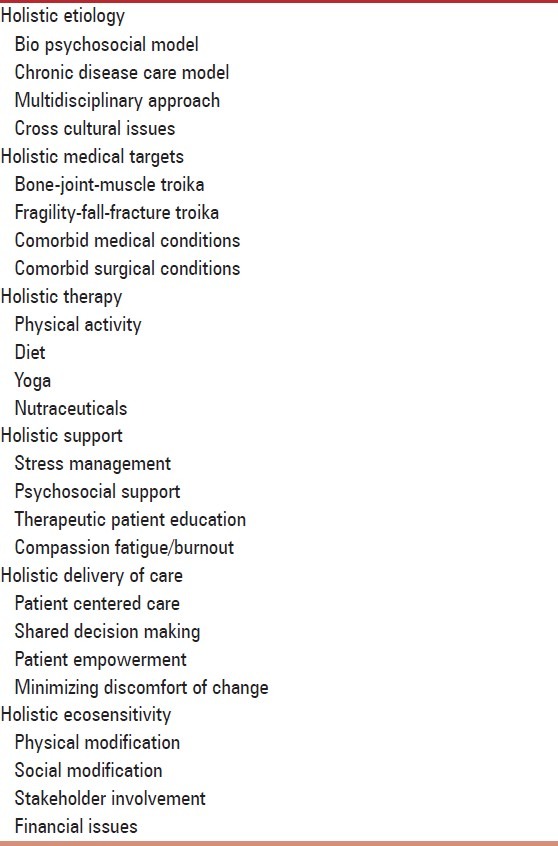
Optimal management of menopause requires the expertise of a multi-disciplinary health team, each equipped with different skills necessary for the patient to enjoy optimal quality of life. Menopause changes the lifestyle of patients in multiple ways and impacts physical, emotional, social and financial quality of life.[1] Keeping these factors in mind, a holistic approach is required to manage menopause. This review analyses various concepts embedded in the umbrella term ‘holistic approach’, to create a framework for menopause practitioners with which to approach their patients. Appropriate use of these concepts will help improve quality of care for patients, and integrate various qualitative aspects of health care into a unified ‘holistic’ management strategy [Table 1].
Table 1.
Holistic care of menopause
HOLISTIC APPROACH TO ETIOLOGY
Holistic approach conceptualizes the involvement of patient's physical, psychological and social needs while planning therapy. It not only includes the biological aspect of menopause, but also the impact of psychosocial factors on diagnosis and therapy, as well as diet, exercise, nutraceuticals and other forms of therapy.
The bio-psycho-social model
Menopause is much more than a purely biological disease. It has important psychosocial components and implications as well. The social and emotional environment of the patient influences her response to menopause in a significant manner. Inappropriate psychosocial environment discourages adherence to therapy, and may prevent participation in outdoor physical activity.[2]
The chronic disease care model
Menopause is a chronic condition, rather than an acute illness. It needs long term therapy, which will be adhered to only if the patient becomes an active and willing partner in her management, with the health care professional taking on a more humble, relatively passive, role of a supporter or facilitator. This model, too, needs to be understood if holistic treatment is to be planned.[3]
Multidisciplinary approach
No single specialty “owns” menopause. A multidisciplinary approach, involving concerted, continuous teamwork, is required to provide holistic care of menopause. While the contribution of each medical, surgical, and paramedical discipline is equally important, an individual patient may require more or less of a particular professional's skill and attention.
To provide a holistic management cover, menopause needs to be managed by gynecologists, endocrinologists, exercise counselors, public health specialists, and orthopedic surgeons. Help is needed from diagnostic specialties such as biochemistry, laboratory medicine, radiology and nuclear medicine to aid in diagnosis. It is understandable that few menopausal women will have access to all super specialties mentioned above.
It makes sense, therefore, for medical professionals to seek certification as menopause practitioners, after being trained in the holistic management of menopausal complaints.
Cross cultural issues
The symptoms of menopause vary across cultures. This should be understood by doctors, who should strive for cultural competence, especially when dealing with multiethnic patient populations.
HOLISTIC APPROACH TO MEDICAL TARGETS
The bone-joint-muscle troika
Holistic care of menopause is not limited to bone health alone. Apart from osteoporosis, osteoarthritis and sarcopenia prevention and management are equally important. The concept of comprehensive management of bone, joint and muscle health has been propagated by the International Osteoporosis Foundation.[4]
Holistic approach of menopause includes assessment of factors which (may) lead to osteoarthritis and sacropenia, their prevention, minimization and management as necessary. This is important as joint integrity and muscle strength are important determinants of propensity to fall and injure oneself.
The fragility-fall-fracture troika
Fragility of bone or osteoporosis is usually not enough to cause a fracture on its own. Fractures are caused by at least minimal trauma, which may be self-sustained or due to external sources.
Holistic approach to menopause implies focusing not only upon the fragility of the bone and its propensity to fracture, but also upon other factors which promote falls and trauma. Biological issues such as muscle mass and strength, and joint health also contribute to risk of falling and hence risk of fractures.
Co morbid medical and surgical conditions
The postmenopausal person will usually have multiple co morbid medical conditions. These may include other symptomatic manifestations of the menopausal syndrome; associated musculoskeletal and rheumatologic complaints; medical co morbidity such as cardiovascular and endocrine disease; as well as surgical morbidity like cataract. While some of these comorbid illnesses directly impact the risk of mortality, all of them impair the person's feeling of well being and quality of life. All relevant complaints and co morbid diseases must be addressed as part of holistic menopausal care. Support from other specialties may be taken if required.
HOLISTIC APPROACH TO THERAPY
Physical activity and diet
Holistic management of menopause implies equal attention to non pharmacological and pharmacological therapy. The menopausal patient must be offered detailed dietary advice, an appropriate exercise prescription, as well as other necessary support and therapy, in an individualized manner. Providing generic diet charts or a printed list of do and do not in small, difficult to read font is not enough. The eight A's of geriatric dietary prescription should be followed while dealing with menopausal patients.[5]
Yoga
Yoga is an ancient Indian system of fitness which promotes healthy living. It helps menopause by improving muscle strength and increasing range of movement at joints, as well as quality of life. Yoga should be included as part of spectrum of holistic management.
Nutraceuticals
Apart from appropriate medical therapy, menopause benefits from adjuvant treatment with nutraceuticals. Relevant nutraceuticals such as isoflavones, calcium and vitamin D form an integral part of prescription for menopausal patients.
HOLISTIC APPROACH TO SUPPORT
Stress management
Menopause may be associated with significant stress, especially if function-limiting or quality of life limiting complications occur.
Medical management must be combined with stress management and coping skills training to minimize the psychological impact of the disease.
Psychosocial support
The concept of psychosocial support extends beyond, and includes, stress management, support is offered as an ongoing, integral part of therapy in menopause, conveying to the patient that she is not alone. Support does not have to be limited to a psychologist's work description; rather, it is part and parcel of every health care practitioner's duty. Active provision of psychological support underpins the holistic approach to menopause care.
Therapeutic patient education
The concept of therapeutic patient education (TPE) originated from chronic disease such as diabetes and asthma. TPE aims to educate patients about their condition, thus causing clinical benefits per se and also improving outcomes associated with use of other treatment modalities.[6] Information about healthy nutrition, sunlight exposure and physical activity is a part of TPE as well. TPE is essential in menopause, as patients need to be aware of their body's limitations and the activities they can perform to improve quality of life.
Compassion fatigue and burnout
Menopause practitioners should guard against compassion fatigue and burnout, which is common in health care professionals dealing with chronic disease.[7]
HOLISTIC APPROACH TO DELIVERY OF CARE
Patient centered care
The term patient centered care (PCC) has found acceptance in family medicine as well as chronic disease, including diabetes and hypothyroidism. For menopause, too, PCC is an integral part of management.
PCC is defined as “as care that is respectful of and responsive to individual patient preferences, needs and values” and that “ensures that patient values guide all clinical decisions”.[8] Holistic management of menopause should understand the values attitudes, needs and wishes of patients while making all decisions.
Shared decision making
Holistic approach to management of menopause overlaps with the concept of shared decision making (SDM) as well. SDM is a process by which patients and providers consider outcome probabilities and patient preferences in order to reach a health care decision based upon mutual agreement.[8] As menopause impacts the life of a patient in many ways, she has the prerogative to choose her treatment. This is best done in consultation with the health care provider, in a shared manner (SDM), after adequate information has been gained about the condition (TPE).[9] What may be appropriate for one patient may be harmful to another.
Patient empowerment
Patients must be empowered to take decisions concerning their health. Empowerment is a patient's right, along with which comes the responsibility of seeking education and support, utilizing available health care resources, and practicing active self-care of oneself.[10] Holistic health includes the provision of all these rights and responsibilities to the patient.
Minimizing the discomfort of change
Any and every, change is associated with discomfort. The onset of menopause necessitates changes in a person's lifestyle, and leads to discomfort. The discomfort of change adds to the discomfort caused by the illness and its complications per se.[11] Minimizing the discomfort of change is an essential part of holistic management of menopause. Health care professionals should be sensitized to the need to internalize discomfort-reducing strategies in their management plans.
HOLISTIC ECOSENSITIVITY
Physical and social ecosensitivity
Menopauseis an ‘ecosensitive’disease. This means that the morbidity and impact of menopause are related to the nature of the environment that the patient lives in. Both physical (natural and man made), and social (human), environment influence the natural history or clinical course of menopause. Adequate provision of facilities for safe outdoor physical activity, and availability of disability friendly measures such as adequate lighting, as ramps, stair case railings and lifts, are examples of ways in which the physical environment can be modified to improve health of elderly postmenopausal women. Access to group based physical activity is known to help improve physical fitness, as compared to being asked to exercise alone: This is an example of social ecosensitivity.
The family
The concept of ecosensitivity leads us to the realization that menopause can not be managed in isolation by patient and physician. The family must be involved in management of menopause, to minimize morbidity and optimize quality of life.
Family members should be encouraged to support the person with menopause, by providing a physical and emotional environment in which she contributes as much as possible to the family, without compromising her health.
The notion of a ‘family with menopausal member’ instead of an ‘individual with menopause’ should be engrained into the minds of both healthcare providers and patient's relatives.
The community
Holistic management of menopause includes the community, so as to optimize both social and physical environment. Spreading public awareness about menopause, its implications, and its management strategies, is essential for reducing the burden of this condition. A supportive community can help minimize the negative impact of menopause on the patients.
Policy makers
Holistic management of menopause also includes patient advocacy. Policy makers and health care system administrators should be petitioned to increase the facilities available for diagnosis and management of menopause. There are just about 250 DEXA machines available in India, to serve a population of over one billion people.[12]
Financial issues
Mangement of menopause may lead to economic hardship for the patient as well as her family, especially in a pay from pocket market such as India where medical insurance coverage is negligible.
The financial burden due to menopause is multifold. Patients find their economic value dropping, as they are unable to contribute in cash or kind to the family income. Expenses incurred on their medical care rise, while indirect costs linked to the need to modify the physical domestic environment creep in.
Holistic management implies that financial consideration must be kept in mind while planning investigations and therapy. Doctors should have a practical, pragmatic and realistic approach to this aspect of menopause care.
CONCLUSION
Holistic care of menopause implies a patient centered approach which utilizes available health care resources to meet all medical, surgical and psychological needs of the patient, using a variety of non pharmacological and drug therapies, while involving all concerned stakeholders to optimize the patient's macroenvironment. This review provides a unified framework which can be followed by practitioners of menopause medicine, as well as health care professionals dealing with other chronic diseases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Berkowitz LR. Focused teaching in menopause: The time is now. Menopause. 2012;19:1072–3. doi: 10.1097/gme.0b013e31826cd9a3. [DOI] [PubMed] [Google Scholar]
- 2.Asokan TV. Towards an ideal paradigm. Indian J Psychol Med. 2009;31:58–61. doi: 10.4103/0253-7176.63574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff (Millwood) 2009;28:75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. [Last accessed on 2012 Oct 1]. Available from: http://www.iofbonehealth.org/osteoporosismusculoskeletal.disorders .
- 5.Kalra S, Kalra B, Saluja S. Dietary management in geriatric patients of diabetes mellitus: Special considerations. Internet J Geriatr Gerontol. 2009;5:1. [Google Scholar]
- 6.Nielsen D, Ryg J, Nielsen W, Knold B, Nissen N, Brixen K. Patient education in groups increases knowledge of osteoporosis and adherence to treatment: A two-year randomized controlled trial. Patient Educ Couns. 2010;81:155–60. doi: 10.1016/j.pec.2010.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Sabo BM. Adverse psychosocial consequences: Compassion fatigue, burnout and vicarious traumatization: Are nurses who provide palliative and hematological cancer care vulnerable? Indian J Palliat Care. 2008;14:23–9. [Google Scholar]
- 8.Washington, DC: The National Academies Press; 2001. Committee on quality of health care in America crossing the quality chasm: Institute of Medicine (U.S.) A new health system for the 21st century. [PubMed] [Google Scholar]
- 9.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango) Soc Sci Med. 1997;44:681–92. doi: 10.1016/s0277-9536(96)00221-3. [DOI] [PubMed] [Google Scholar]
- 10.Kalra S, Unnikrishnan AG, Skovlund SE. Patient empowerment in endocrinology. Indian J Endocr Metab. 2012;16:1–3. doi: 10.4103/2230-8210.91173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalra S, Kumar S, Kalra B, Unnikrishnan A, Agrawal N, Sahay R. Patient-provider interaction in diabetes: Minimizing the discomfort of change. Internet J Fam Pract. 2010;8:1. [Google Scholar]
- 12.Kalra S, Kalra B, Baruah MP. Diagnosing osteoporosis made easier: The FRAX tool gets better. J Med Nutr Nutraceut. 2012;1:61–2. [Google Scholar]


