Abstract
Background:
To study the menopause related symptoms affecting the quality of life (QOL) of perimenopausal women in order to understand the prevalence and plan for the interventions.
Materials and Methods:
Two hundred and nine women were evaluated for perimenopausal symptoms using a 29 item MENQOL questionnaire.
Results:
The physical and psychosocial symptoms were found to be more prevalent than the vasomotor and sexual symptoms.
Conclusion:
Perimenopausal symptoms widely vary in women populations, accurate recording and understanding of which is essential to plan effective interventions to improve the QOL.
Keywords: Awareness, Karnataka, MENQOL questionnaire, perimenopausal symptoms, QOL
INTRODUCTION
Menopause is the permanent cessation of menstruation which is retrospectively determined following twelve months of amenorrhea during midlife period and the most identifiable event of the perimenopausal period. The year immediately preceding and the decade afterwards, however, are of far greater clinical significance. The perimenopausal period encompasses the time before; during and after menopause.[1] Symptoms that begin with the menopausal transition usually continue making a compensatory decrease in the postmenopause.[2] The immediate symptoms of menopause are the effects of hormonal changes on many organ system, most extensively the cardiovascular and musculoskeletal system affecting their quality of life.[3] Commonly reported symptoms include hot flushes, night sweats, muscles and joint pains, sleep disturbances, urinary frequency, vaginal dryness, poor memory, anxiety and depression.[4,5] Menopausal symptoms have been widely studied in women from western societies, but less information is available for women of non-western ethnic groups. There is evidence of differences in the prevalence of symptoms in Asian versus Western women.[6–10] Further, wide variations have been observed in the sub population studies,[11] including studies in Indian women from selected regions.[12–15]
There were no studies from this region of subcontinent regarding the quality of life of perimenopausal women. This study evaluates the menopausal symptom of women aged between 40 to 60 years which is important to understand the prevalence and plan for the remedial measures and also to create awareness.
MATERIALS AND METHODS
This cross sectional study was carried out in 209 women (aged 40 to 60 years) who were from the local community belonging to various women organizations, self-help groups in this area. They were included in this study based on their menstrual history (to assess menopausal status) and the experience menopausal symptoms by using the questionnaires. The self-administered questionnaire included socio-demographic factors with menstrual history. Women with surgical menopause, receiving any kind of hormone therapy, presence of medical conditions like diabetes, hypertension and cardiac diseases were excluded. The self-administered questionnaire included socio-demographic information with menstrual history and the Menopausal Specific Quality of Life (MENQOL) questionnaire[16] to document the menopausal symptoms to assess their quality of life. Women with perimenopausal symptoms included in this group were ‘premenopausal’ who reported still having menstrual cycles or with slight change in the length of cycle and ‘postmenopausal’ women whose last menstrual period occurred 12 months or later. The MENQOL questionnaire is a self-administered 29-item survey questionnaire, designed to describe quality of life in menopausal women and which measures the extent to which an individual is affected by menopausal symptoms. All items in the Menqol questionnaire followed the same format. It comprised of menopausal symptoms in four domains: Vasomotor, Psychosocial, Physical and Sexual. Each women was asked whether she experienced the symptoms in the previous six months if answer was no she was asked next item and if answer was yes she was asked to indicate how bothered she had been by the symptoms on a seven point scale ranging from 0 = not at all bothered to 6 extremely bothered. For analysis score becomes 1 for ‘No’, 2 for ‘Yes’ through to 8 for “Yes (Extremely bothered)”. The questionnaire was in English and translated to local language Kannada. The questionnaire was given after obtaining written informed consent. This study has been approved by the institutional ethics committee.
All data gathered was analyzed by using Statistical Package for Social Science (SPSS) Ver. 15. QOL score for each domain are presented as median with quartiles. Demographic features and symptoms are reported as frequency with percentages. Mann-Whitney U test was used to compare QOL score among premenopausal and postmenopausal group. A P value less than 0.05 were considered as statistically significant.
RESULTS
Characteristics of the study population
The mean age of the group was 48.30 ± 5.30 of years. Among 209 women, 33 (15.8%) were obese (BMI ≥ 30), 77 (36.8%) were overweight (BMI 25-30), 88 (42.1%) were normal (BMI 18.5-24.99) and 11 (5.3%) were of below normal weight (BMI ≤18.5). Out of 209, 200 (95.7%) were married and 8 (3.8%) were separated. In all, 9 (4.3%) have no children, 37 (17.7%) have one, 122 (58.4%) have two, 41 (19.6%) have more than two children. All of them were educated with 74 (35.4%) graduate/post graduate, 102 (48.8%) intermediate/high school education and 33 (15.8%) middle/primary school education. 87 (41.6%) of the women were employed and 122 (58.4%) were house wives with domestic duties. With regard to the perimenopause status 129 (61.7%) women were premenopausal, and 80 (38.3%) postmenopausal within 40-55 years and 45-57 years age groups respectively.
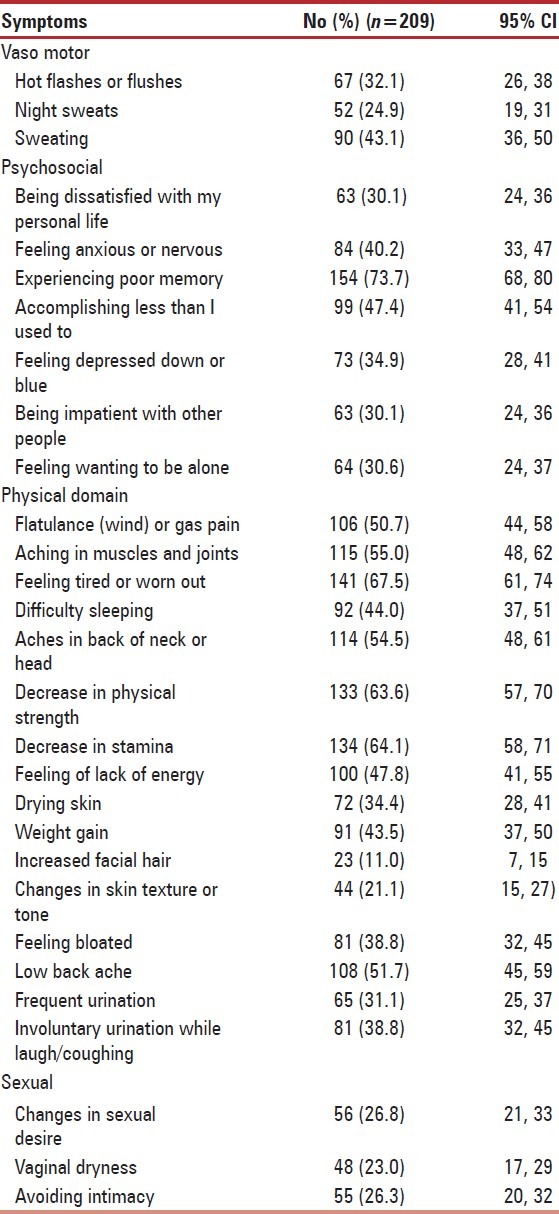
Physical and psychosocial symptoms were more commonly reported among the women [Table 1]. Feeling tired or worn out 141 (67.5%), decrease in physical strength and stamina 134 (64.1%), muscles and joint pain 115 (55.0%), aches in the back of neck or head 114 (54.5%), flatulence or gas pain 106 (50.7%), low back ache 108 (51.7%), lack of energy 100 (47.8%), difficulty in sleeping 92 (44%), feeling bloated 81 (38.8%), involuntary urination while laughing, coughing 81 (38.8%) were reported by over a half of the women in physical domain. The major symptoms in psychosocial domain were poor memory 154 (73.7%), accomplishing less than they used to 99 (47.4%), feeling anxious or nervous 87 (40.2%). Experiences of vasomotor symptoms were relatively less with 67 (32.1%) reporting hot flushes and 57 (24.9%) night sweats.
Table 1.
Menopausal specific quality of life questionnaire
Quality of life
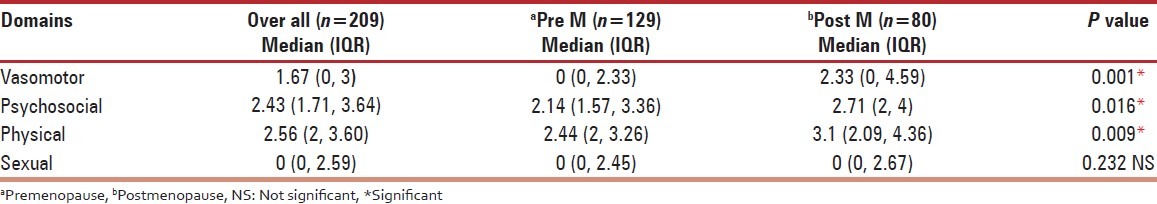
The median of the each domain of MENQOL was used as the overall subscale score. Table 2 lists the scores of four domains by menopausal status. The overall median score of QOL with respect to the physical and psychosocial domains were higher than the vasomotor and sexual domains. Comparatively the scores of vasomotor domain were statistically significantly different in postmenopausal women group P < 0.001 than the premenopausal women group and physical and psychological domain scores were also statistically significantly different in postmenopausal women group with P < 0.02 and P < 0.01 respectively.
Table 2.
Quality of life
DISCUSSION
The present study records the menopausal symptom profile in women from coastal Karnataka, India. Compared to similar studies conducted in India and outside India indicates wide variation in perimenopausal symptoms [Table 3]. The women from the present study reported higher physical and psychosocial symptoms with a high frequency of physical symptoms such as feeling tired, decrease in physical strength and stamina, poor memory, muscles and joint pains, low back ache, and flatulence. Although the overall symptom profile is consistent with other Indian women from Jammu,[12] Mumbai,[13] Chandigarh[14] and Amritsar,[15] the actual percentage, the intensity and the frequency of individual symptom varied in these Indian sub populations. Similarly, some symptoms in women from other countries were comparable with the present study (physical and psychosocial), while others differed (vasomotor and sexual).
Table 3.
Predominant perimenopausal symptom profiles in various studies conducted in India and outside India
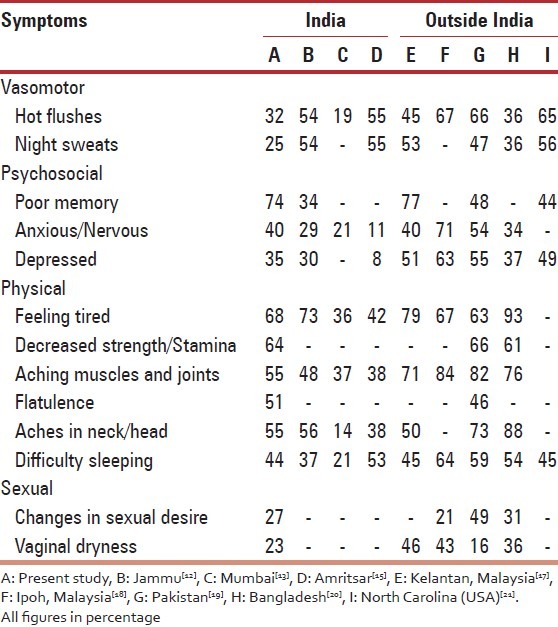
In the present study, 79 (36.6%) reported of hot flushes which were lower as compared to women from Jammu[12] and Mumbai.[13] This kind of national variations was also observed in Malaysian studies. While one study[17] reported (45%) of hot flushes which was lower compared to other Malaysian study,[18] where the subjects were mostly disturbed by joint and muscular discomfort (84%) followed by anxiety (71%) and hot flushes (67%). The variations in symptoms were also observed in menopausal women from Pakistan[19] and Bangladesh.[20] Neslihan from Turkey also reported higher rate of musculoskeletal symptoms compared with vasomotor.[22] Indian women seem to be less affected by hot flushes unlike the Caucasians.[23] In countries such as India, Malaysia and Thailand hot and humid weather may mask similar symptoms associated with the climacteric. Obermeyer[11] has suggested that dietary factors in Asians would contribute to lower frequency of hot flushes, as phytoestrogens have a role in reducing vasomotor symptoms. However, this does not seem to explain the difference of hot flush incidence observed in our study compared to those from North India.[12–15] Fu et al.[24] also compared estrogen levels and found higher levels in Taiwanese women then in Australians and suggested that there might be a relationship between cultural life style factors and the estrogen level. Asian women living in Birmingham had menopausal symptoms similar to that of their Caucasian counterparts[25] suggesting attribution of symptoms varying in women of the same ethnic origin depending on their country of residence. Thus estrogen levels, environmental and socio-cultural factors such as diet, exercise and other life style modifications seems to be determine the menopausal symptom profile.
The prevalence of sexual symptoms showed variations in various women population. Reporting of sexual symptoms was low in the present study as compared to the women of Caucasian origin.[20,21,26] The reporting of sexual symptom was also related to the socioeconomic status, with upper and middle socioeconomic classes reporting higher incidences than the lower socioeconomic class (51 vs. 40%).[27] The sexual symptom seems to be best explained by reduced estrogen levels in perimenopause.[28]
In this study the postmenopausal women had significantly higher scores in vasomotor, psychological and physical domains than the premenopausal group. These findings differ from other earlier studies. A study from Thailand showed hot flushes, upset stomach, insomnia and urinary symptoms to be predominant in menopausal transition while night sweats and joint aches and pains were significantly associated with post menopause.[29] Another study from Pakistan reported higher physical domain scores in post menopause and significant psychological domain symptoms in menopausal transition women.[19]
Other studies reported that vasomotor complaints were more prevalent in menopausal transition whereas psychological complaints were more in post menopause.[30]
However the specific features and rates varied probably because of the individual methodologies used. Moreover, several other factors also seem to influence the physical and psychosocial development of symptoms such as progressive aging, growing family responsibilities, possible mid-life crisis and other non-menopausal factors during this phase of their lives. Moreover, understanding, belief, values, attitudes, education, cultural factors seems to indirectly influence the symptom profile.
These kind of community surveys helps to serve several purposes. First and most importantly, they educate the participating women and create awareness that the perimenopausal symptoms are natural consequences of progressive life events. Many women mistake these symptoms as a part of serious systemic disease and waste lots of time, energy, effort and money on pursuing ineffective medical remedies. Understanding the physiology of perimenopause and its symptoms helps to cope more effectively. Identifying the predominant symptoms in a local community also helps to plan suitable intervention to reduce the symptom burden and thereby improve the quality of life. For populations with high incidence of vasomotor and sexual symptoms hormonal therapy may be more beneficial while for predominant physical and psychosocial symptoms other alternative therapies may work better. For instance, in our women population, as a preliminary study we implemented 12 weeks yoga therapy protocol which included selective asana-s (postures), pranayama (breathing exercise) and meditation. The initial results were very encouraging with highly significant improvement in perimenopausal symptoms.
Thus, as noted above a large number of women all over the world suffer from perimenopausal symptoms and the problem cannot be ignored. Education, creating awareness and providing suitable intervention to improve the quality of life are important social and medical issues which are to be addressed.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hurd WW, Amesse LS, Randolph JF., Jr . Menopause. In: Jonathan SB, editor. Novak's gynecology. 13th ed. Philadelphia: Lippincott Williams and Wilkins; 2002. pp. 1109–42. [Google Scholar]
- 2.McKinley SM, Brambilla DJ, Posner JG. The normal menopause transition. Maturitas. 2008;61:4–16. doi: 10.1016/j.maturitas.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 3.WHO technical report series 866. Geneva: WHO; 1996. World Health Organization (WHO). Report of WHO scientific group on the menopause in the 1990s; pp. 12–3. [PubMed] [Google Scholar]
- 4.Greendale GA, Lee NP, Arriola ER. The menopause. Lancet. 1999;353:571–80. doi: 10.1016/S0140-6736(98)05352-5. [DOI] [PubMed] [Google Scholar]
- 5.Nachtigall LE. The symptoms of perimenopause. Clin Obstet Gynaecol. 1998;41:921–7. doi: 10.1097/00003081-199812000-00018. [DOI] [PubMed] [Google Scholar]
- 6.McCarthy T. The prevalence of symptoms in menopausal women in the Far East: Singapore segment. Maturitas. 1994;19:199–204. doi: 10.1016/0378-5122(94)90072-8. [DOI] [PubMed] [Google Scholar]
- 7.Ho SC, Chan SG, Yip YB, Cheng A, Yi Q, Chan C. Menopausal symptoms clustering in Chinese women. Maturitas. 1999;33:219–27. doi: 10.1016/s0378-5122(99)00056-0. [DOI] [PubMed] [Google Scholar]
- 8.Pan HA, WuM H, Hsu CC, Yao BL, Huong KE. The perception of menopause among women in Taiwan. Maturitas. 2002;41:269–74. doi: 10.1016/s0378-5122(01)00279-1. [DOI] [PubMed] [Google Scholar]
- 9.Wasti S, Robinson SC, Aktar Y, Khan S, Badaruddin N. Characteristics of menopause in three socioeconomic urban groups in Karachi Pakistan. Maturitas. 1993;16:61–9. doi: 10.1016/0378-5122(93)90134-4. [DOI] [PubMed] [Google Scholar]
- 10.Singh M, Singh S. A comparison of mental health status during menopause and post menopause middle aged working women. Int J World Health Soc Polit. 2007:4. [Google Scholar]
- 11.Obermeyer CM. Menopause across cultures: A review of evidence. Menopause. 2000;7:184–92. doi: 10.1097/00042192-200007030-00009. [DOI] [PubMed] [Google Scholar]
- 12.Sharma S, Tandon VR, Mahajan A. Menopausal symptoms in urban women. JK Sci. 2007;9:13–7. [Google Scholar]
- 13.Shah R, Kalgutkar S, Sarvardekar L, Chitlang S, Iddya U, Balaiah D. Menopausal symptoms in urban Indian women. Obstet Gynecol Today. 2004;11:667–70. [Google Scholar]
- 14.Kaur S, Wlia I, Singh A. How menopause affects the lives of women in suburban Chandigarh, India. Climacteric. 2004;7:175–80. doi: 10.1080/13697130410001713779. [DOI] [PubMed] [Google Scholar]
- 15.Sidhu S, Kaur A, Sidhu M. Age at menopause in educated women Amritsar (Punjab) J Hum Ecol. 2005;18:49–51. [Google Scholar]
- 16.Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, et al. A menopause specific quality of life questionnaire: Development and psychometric properties. Maturitas. 1996;24:161–75. doi: 10.1016/s0378-5122(96)82006-8. [DOI] [PubMed] [Google Scholar]
- 17.Dhillon HK, Singh HJ, Shuib R, Hamid AM, Mahmood NM. Prevalence of menopausal symptoms in women in Kelantan, Malaysia. Maturitas. 2006;54:213–21. doi: 10.1016/j.maturitas.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 18.Jahanfar SH, Abdul Rahim BA, Shah Reza BK, Nor Azura BT, Sharifah Nora BT, Siti Asma BT, et al. Age of menopause and menopausal symptoms among Malaysian Women Who referred to health clinic in Malaysia. Shiraz E-Med J. 2006;7:1–9. [Google Scholar]
- 19.Nisar N, Sahoo NA. Frequency of menopausal symptoms and their impact on the quality of life of women: A hospital based survey. J Pak Med Assoc. 2009;59:752–6. [PubMed] [Google Scholar]
- 20.Rahman S, Salehin F, Iqbal A. Menopausal symptoms assessment among middle age women in Kushtia, Bangladesh. BMC Res Notes. 2011;4:188. doi: 10.1186/1756-0500-4-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bosworth HB, Bastian LA, Kuchibhatla MN, Steffens DC, McBride CM, Skinner CS, et al. Depressive symptoms, menopausal status and climacteric symptoms in women at midlife. Psychosom Med. 2001;63:603–8. doi: 10.1097/00006842-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Neslihan Carda S, Bilge SA, Ozturk TN, Oya G, Ece O, Hamiyet B. The menopausal age, related factors and climacteric symptoms in Turkish women. Maturitas. 1998;30:37–40. doi: 10.1016/s0378-5122(98)00041-3. [DOI] [PubMed] [Google Scholar]
- 23.Avis NE, Stellato R, Crawford S, Bromberger J, Ganz P, Cain V, et al. Is there a menopause syndrome? Menopausal status and symptoms across racial/ethnic groups. Soc Sci Med. 2001;52:345–56. doi: 10.1016/s0277-9536(00)00147-7. [DOI] [PubMed] [Google Scholar]
- 24.Fu SY, Anderson D, Courtney M. Cross cultural menopausal experience : Comparison of Australian and Taiwanese Women. Nurs Health Sci. 2003;5:77–84. doi: 10.1046/j.1442-2018.2003.00139.x. [DOI] [PubMed] [Google Scholar]
- 25.Gupta P, Sturdee DW, Hunter MS. Mid-age health in women from the Indian subcontinent (MAHWIS): General health and the experience of menopause in women. Climacteric. 2006;9:13–22. doi: 10.1080/13697130500515776. [DOI] [PubMed] [Google Scholar]
- 26.Brsyski RJ, Medrano MA, Hyatt-Santos JM, Ross JS. Quality of life in low-income menopausal women attending primary care clinics. Fertil Steril. 2001;76:44–50. doi: 10.1016/s0015-0282(01)01852-0. [DOI] [PubMed] [Google Scholar]
- 27.Taechakraichana N, Nakornpanom PN, Limpaphayom K. Climacteric complaints of paramedical personnel. J Med Assoc Thai. 1997;80:297–302. [PubMed] [Google Scholar]
- 28.Dennerstein L, Dudley EC, Hopper JL, Burger H. Sexuality, hormones and the menopausal transition. Maturitas. 1997;26:83–93. doi: 10.1016/s0378-5122(96)01093-6. [DOI] [PubMed] [Google Scholar]
- 29.Punyahotra S, Dennerstein L, Lehert P. Menopausal experience of Thai women. Part 1: Symptom and their correlates. Maturitas. 1997;26:1–7. doi: 10.1016/s0378-5122(96)01058-4. [DOI] [PubMed] [Google Scholar]
- 30.Boulet MJ, Oddens BJ, Lehert P, Vemer HM, Visser A. Climacteric and menopause in seven South-East Asian countries. Maturitas. 1994;19:157–76. doi: 10.1016/0378-5122(94)90068-x. [DOI] [PubMed] [Google Scholar]


