Abstract
AIMS
Alveolar nitric oxide (CANO) is a potential biomarker of small airway inflammation. We investigated effects on CANO of the addition of coarse and fine particle inhaled corticosteroids to standard therapy in severe asthma.
METHODS
Severe asthmatics taking ≥1600 µg day−1 budesonide or equivalent performed a randomized open-label crossover study. Subjects with FEV1 < 80%, gas trapping and CANO≥2 ppb entered a 6 week dose-ramp run-in of fluticasone/salmeterol(FPSM) 250/50 µg twice daily for 3 weeks, then 500/50 µg twice daily for 3 weeks. Patients then received additional HFA-beclomethasone diproprionate (BDP) 200 µg twice daily or FP 250 µg twice daily for 3 weeks in a crossover. Participants then received prednisolone(PRED) 25 mg day−1 for 1 week. Nitric oxide, lung function, mannitol challenge, systemic inflammatory markers and urinary cortisol were measured.
RESULTS
Fifteen completed per protocol: mean (SD) age 51 (12) years, FEV1 58 (13)% predicted, residual volume 193 (100)% predicted and mannitolPD10 177 (2.8) µg. There was no significant difference between FPSM and add-on therapy for CANO. FPSM/BDP and FPSM/PRED suppressed broncial flux (JawNO) and FENO compared with FPSM alone, but there was no significant difference between FPSM/BDP and FPSM/FP. ECP, e-selectin and ICAM-1 were suppressed by FPSM/PRED compared with FPSM and FPSM/FP but not FPSM/BDP. Plasma cortisol was significantly suppressed by FPSM/PRED.
CONCLUSION
In severe asthma, CANO is insensitive to changes in dose and delivery of inhaled corticosteroids and is not suppressed by systemic corticosteroids. Additional inhaled HFA-BDP reduced FENO and JawNO without adrenal suppression. There was a trend to reduction in FENO and JawNO with additional FP but this did not reach statistical significance. PRED reduced FENO and JawNO with suppression of systemic inflammatory markers and urinary cortisol.
Keywords: alveolar nitric oxide, asthma
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Extra fine inhaled corticosteroid formulations such as HFA beclomethasone may be used to target the small airways in asthma. However, it is unclear which outcome measures may detect such small airways effects in patients with severe asthma.
WHAT THIS STUDY ADDS
The alveolar fraction of exhaled nitric oxide is not a sensitive outcome measure for following effects of extra fine particle inhaled beclomethasone in severe asthma. However there were significant effects on nitric oxide fractions measured at 50 ml s−1 and bronchial flux with the extra fine formulation, which did not produce significant cortisol suppression.
Introduction
Asthma is characterized by inflammation of the airways associated with smooth muscle hypertrophy, bronchial hyper-reactivity and airway remodelling [1, 2]. Whilst inhaled corticosteroids (ICS) are effective for the treatment for most asthmatics, 5–15% of patients are poorly controlled despite combination therapy, or require high dose therapy to control their disease [3]. Pathology series suggest that in severe asthma, disease may be more distally distributed compared with mild-to-moderate disease [2, 4, 5].
Fractional exhaled nitric oxide (NO) measured at a flow rate of 50 ml s−1 (FENO) is correlated with airway eosinophila and has been used as a surrogate of steroid responsiveness [6]. In recent years extended exhaled NO techniques have been developed which calculate values representative of NO derived from the large conducting airways and the small airways and alveoli, respectively, the so-called ‘two compartment model’ of NO production [7]. The technique involves the measurement of exhaled NO at several flow rates from which alveolar NO (CANO) and bronchial flux (JawNO) can be derived. The majority of traditional FENO is derived from JawNO[8].
Early papers reported that CANO was elevated in severe asthmatics suggesting that it could be a useful biomarker for the monitoring of small airway disease in severe asthma [9, 10]. It is now recognized that the two compartment model was an over-simplification in that it does not account for NO diffusion between compartments. Hence a proportion of NO produced proximally (JawNO) will diffuse back into the alveolar compartment resulting in false elevation of CANO and vice versa. Mathematical adjustments are now used to correct for this [11, 12]. This correction is especially important when JawNO (and hence FENO) are elevated as is often the case in severe asthma. Hence in severe asthma, the response of CANO to different preparations of corticosteroids has not been studied in a controlled trial with correction for back-diffusion.
The aim of the present study was to investigate the effects on CANO of the addition of coarse or fine particle ICS to standard therapy in severe asthma, using oral prednisolone (PRED) as a positive control. Other surrogates of airway and systemic inflammation were assessed for comparison.
Methods
Study design
An open-label randomized crossover study was performed (Figure 1). Participants were never-smokers or ex-smokers with <10 pack years, aged 16–65 years, a respiratory physician diagnosis of asthma, prescribed ≥1000 µg day−1 fluticasone or 1600 µg day−1 budesonide in the previous year. Subjects required evidence of persistent airflow obstruction (post-bronchodilator FEV1 : FVC ratio < 0.7, FEV1 < 80%) and gas trapping (total lung capacity and residual volume > 100%). Exclusion criteria included diagnosis of bronchiectasis or allergic broncho-pulmonary aspergillosis and long term oral corticosteroid use. Subjects were also required to have an elevated uncorrected alveolar NO (≥2 ppb) following a 6 week dose-ramp run-in of fluticasone/salmeterol (FPSM) 500 µg day−1 for 3 weeks, then 1000 µg day−1 for 3 weeks via dry powder inhaler (Seretide Accuhaler, Allen & Hanbury).
Figure 1.
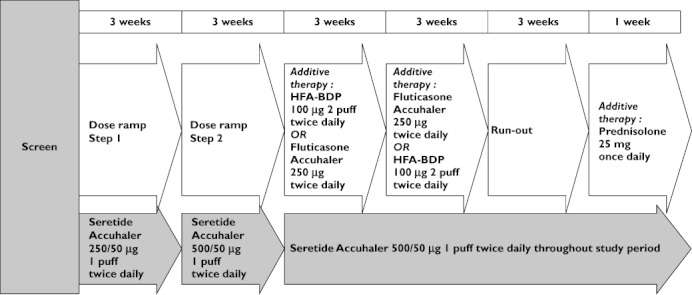
Study diagram
For the treatment periods, participants continued FPSM 1000 µg day−1 and were additionally randomized to extra-fine HFA-beclomethasone diproprionate (BDP) 400 µg day−1 (BDP) (Qvar easibreathe, Teva Pharmaceuticals) or fluticasone propionate 500 µg day−1 (FP) (Flixotide Accuhaler, Allen & Hanbury) for 3 weeks in a crossover fashion. Following a 3 week run-out all participants were allocated PRED 25 mg day−1 (PRED) for 1 week. Inhaler technique was assessed and corrected at every visit using an In-check dial (Clement Clarke International Limited, Essex, UK). Compliance was re-enforced at each visit and dose counters checked for DPI treatments. Computer generated simple randomization was performed to allocate subjects to cross-over sequence.
At baseline and following each treatment the following measurements were performed: extended exhaled NO, spirometry, impulse oscillometry, body plethysmography, asthma quality of life questionnaire (AQLQ), asthma control questionnaire (ACQ), mannitol challenge and blood for ECP, ICAM-1 and E-selectin. Subjects took study medication on the morning of visits, but withheld ‘as required’ medications. Leukotriene receptor antagonists were not permitted during the study. Alveolar NO was the primary outcome and other measurements secondary. All measurements were performed at the Asthma and Allergy Research Group at Ninewells Hospital, Dundee and Perth Royal Infirmary, Perth. The study was approved by the Tayside Committee on Medical Research Ethics and registered on clinicaltrials.gov (NCT00829257).
Measurements
Lung function
Spirometry was performed in accordance with guidelines [13] using a SuperSpiro spirometer (Micro Medical Ltd, Chatham, Kent, UK). A Jaeger Masterscreen (Erich Jaeger, Hoechberg, Germany) was used for impulse oscillometry (IOS) and full body plethysmography. IOS was performed as previously published [14]. If FEV1 > 60% the provocative dose of mannitol required for a 10% fall in FEV1 (mannitol PD10) was performed as previously published [15].
Extended exhaled nitric oxide
An on-line chemiluminescence analyzer (Niox, Aerocrine AB, Solna, Sweden) was used to quantify exhaled NO at multiple flow rates, 50 ml s−1, 100 ml s−1 and 200 ml s−1. Online graphs of NO exhalation manoeuvres were examined to ensure that an adequate plateau had been achieved. Measurements were repeated as necessary to ensure a minimum of two satisfactory readings at each flow rate with <10% variation. CANO and JawNO were derived using the two-compartment models described by Tsoukias & George and Tsoukias et al. [7, 16] with correction for axial diffusion as described by Kerckx et al. [12].
Laboratory analysis
Urine was collected overnight for 10 h prior to study visits. Urinary creatinine was determined using a Roche Cobas analyzer (Roche, Burgess Hill, UK; coefficient of variance (CV) 4.9%) and cortisol by radioimmunoassay (Diasorin, Bracknell, UK; CV 8.6%). ECP was determined using the UNICAP method (Phadia Ltd, Milton Keynes, UK; CV 4.0%). E-selectin and ICAM-1 were measured through use of enzyme immunoassays (Diaclone, Besancon, France; CV 1.5% and 2.8%).
Statistical analysis
Data were assessed for normality using the Shapiro-Wilk test and inspection of boxplots. Non-Gaussian data were log-transformed prior to analysis. Values for baseline (FPSM), treatment limbs (FPSM/FP and FPSM/FP) and positive control limb (FPSM/PRED) were compared using an anova of repeated measures followed by Bonferroni correction for multiple comparisons. A priori power calculations predicted that 14 participants in crossover design ensured 90% power, with an α error of 0.05, to detect a 0.5 ppb change in CANO, assuming a within patient standard deviation of 0.37 ppb based on previous studies in asthmatics [9, 17]. Analyses were performed using SPSS version 17.0 (Chicago, Illinois, USA) or GraphPad PRISM version 5.01 (San Diego, California, USA).
Results
Fifty-two screens were performed of which 26 were suitable to enter the 6 week dose ramp run-in. Following run-in 17 met entry criteria for randomization to treatments. Two subjects were withdrawn post randomization due to exacerbation requiring systemic steroids (one on each treatment) (see figure 2). Demographic data and medication at screen are shown in Table 1. Mean (SD) age and FEV1 were 51 (12) years and 58 (13)% predicted respectively. All were current non-smokers and 13/15 were never smokers.
Figure 2.
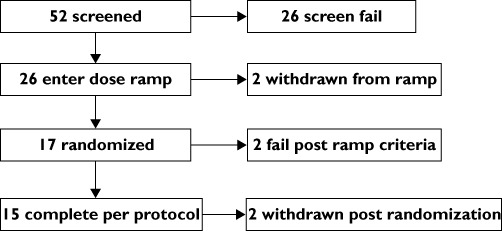
Consort diagram
Table 1.
Demographics at screen
| Screen number | Age(years)/Gender | BDP (µg ) | LABA (L), Nasal steroid (N), LAMA(T), Antihistamine (A) | FEV1 (%) | Residual volume (%) | Resistance at 5 Hz (R5%) | Mannitol PD10 |
|---|---|---|---|---|---|---|---|
| 1 | 50/M | 1600 | L | 77 | 159 | 202 | 95.53 |
| 2 | 52/F | 2000 | L | 66 | 456 | 115 | 30.39 |
| 6 | 52/M | 1000 | LNA | 67 | 83 | 109 | 139.73 |
| 3 | 63/M | 1600 | LN | 54 | 142 | 215 | 170.37 |
| 10 | 37 M | 2000 | LA | 71 | 170 | 129 | 13.28 |
| 23 | 65F | 1000 | L | 49 | 216 | 192 | 337.32 |
| 27 | 48 M | 2000 | L | 67 | 130 | 130 | 192.50 |
| 31 | 40/M | 2000 | LA | 44 | 224 | 213 | NR |
| 32 | 28/M | 1000 | L | 64 | 140 | 214 | 96.94 |
| 36 | 43 M | 2000 | L | 70 | 162 | 286 | 455.89 |
| 37 | 65/M | 1600 | – | 69 | 147 | 151 | 129.27 |
| 38 | 60/M | 2000 | – | 57 | 128 | 153 | 443.57 |
| 39 | 61/F | 2000 | N | 48 | 185 | 142 | NR |
| 40 | 52/M | 2000 | L | 63 | 153 | 200 | 121.69 |
| 41 | 52/M | 2000 | LN | 38 | 188 | 306 | NR |
| Mean (SD) | 51 (10) | 1635 (448) | 58 (13) | 193 (100) | 184 (56) | 177 (2.81) |
Challenge not performed as FEV1 < 50% predicted. BDP, beclomethasone diproprionate equivalent; LABA, long acting beta-agonist; LAMA, long acting anti-muscarinic.
There was no significant difference between FPSM and any add-on therapy for corrected CANO. Mean (95% CI) values were 1.39 ppb (0.48, 2.31) for FPSM, 1.79 ppb (0.58, 3.00) for FPSM/FP, 1.71 ppb (0.69, 2.73) for FPSM/BDP and 1.29 ppb (0.62, 1.96) for FPSM/PRED (Figure 3, Table 2). The FPSM/BDP and FPSM/PRED suppressed JawNO and FENO compared with FPSM alone (Figure 3, Table 2, Table 4). For FENO values were 22.5 ppb (17.0, 27.9) and 21.4 ppb (16.4, 26.4) for FPSM/BDP and FPSM/PRED, respectively compared with 30.7 ppb (21.1, 40.4) for FPSM alone. There was a numerical trend for a reduction in FENO and JawNO with FPSM/FP, but this did not reach statistical significance (P= 0.09 for both). There was no significant difference between FPSM/FP and FPSM/BDP (Figure 3, Table 2, Table 4).
Figure 3.
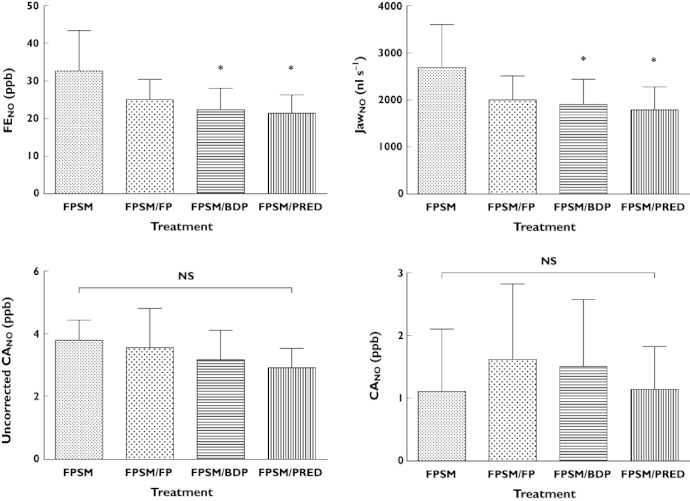
Extended nitric oxide measurements stratified by treatment group. Data displayed as mean with 95% confidence intervals. *P < 0.05 compared with FPSM. FP, fluticasone; FPSM, fluticasone/salmeterol; BDP, beclomethasone diproprionate; PRED, prednisolone
Table 2.
Inflammation and adrenal axis
| Treatment | FPSM | FPSM/FP | FPSM/BDP | FPSM/PRED |
|---|---|---|---|---|
| Exhaled nitric oxide | ||||
| FENO (ppb) | 30.7 (21.1–40.4) | 24.3 (18.9–29.7) | 22.5 (17.0–27.9)* | 21.4 (16.4–26.4)* |
| JawNO (nL.s−1) | 2667 (1744–3590) | 2008 (1517–2500) | 1902 (1370–2434)* | 1795 (1323–2266)* |
| CANO (ppb) | 1.39 (0.48–2.31) | 1.79 (0.58–3.00) | 1.71 (0.69–2.73) | 1.29 (0.62–1.96) |
| Uncorrected CANO (ppb) | 3.74 (3.17–4.31) | 3.59 (2.44–4.74) | 3.37 (2.40–4.34) | 2.90 (2.26–3.54) |
| Plasma ECP | 33.3 (17.6 to 49.0) | 31.2 (21.2 to 41.7) | 23.1 (14.1 to 32.1) | 15.9 (12.0 to 19.7)** |
| Plasma E-selectin | 95.3 (82.2 to 108.3 | 103.7 (87.8 to 119.5) | 94.0 (77.4 to 110.7) | 78.0 (64.3 to 91.7) ** |
| Plasma ICAM-1 | 546 (485 to 607) | 540 (475 to 605) | 513 (456 to 571) | 479 (418 to 540) ** |
| Mannitol PD10 (µg)† | 135 (57–320) | 133 (60–294) | 182 (72–459) | 119 (55–260) |
| Adrenal axis | ||||
| 08.00 h plasma cortisol† | 394 (338 to 459) | 419 (349 to 503) | 407 (356 to 466) | 61 (31 to 121)*** |
P < 0.05 compared with FPSM.
P < 0.05 compared with FPSM and FPSM/FP.
P < 0.05 compared with FPSM, FPSM/FP and FPSM/BDP.
Presented as geometric mean and 95% CI.
FP, fluticasone; FPSM, fluticasone/salmeterol; BDP, beclomethasone diproprionate; PRED, prednisolone.
Table 4.
Difference in means and 95% confidence intervals for extended nitric oxide measurements
| Mean difference | 95% CI | Significance | ||
|---|---|---|---|---|
| FENO (ppb) | ||||
| FPSM | vs. FPSM/FP | 7.85 | (–1.10, 16.80) | 0.094 |
| vs. FPSM/BDP | 10.41 | (1.46, 19.36) | 0.048 | |
| vs. FPSM/PRED | 11.18 | (2.23, 20.13) | 0.041 | |
| FPSM/FP | vs. FPSM/BDP | 2.57 | (–6.38, 11.52) | 0.485 |
| vs. FPSM/PRED | 3.33 | (–5.62, 12.28) | 0.379 | |
| FPSM/BDP | vs. FPSM/PRED | 0.76 | (–8.19, 9.71) | 0.829 |
| JawNO (nl s−1) | ||||
| FPSM | vs. FPSM/FP | 765.1 | (–103.5, 1634) | 0.093 |
| vs. FPSM/BDP | 932.6 | (63.96, 1801) | 0.049 | |
| vs. FPSM/PRED | 1027 | (158.6, 1896) | 0.047 | |
| FPSM/FP | vs. FPSM/BDP | 167.5 | (–701.1, 1036) | 0.630 |
| vs. FPSM/PRED | 262.1 | (–606.5, 1131) | 0.465 | |
| FPSM/BDP | vs. FPSM/PRED | 94.63 | (–774.0, 963.3) | 0.783 |
| CANO (ppb) | ||||
| FPSM | vs. FPSM/FP | –0.56 | (–2.35, 1.24) | 0.459 |
| vs. FPSM/BDP | –0.32 | (–2.12, 1.47) | 0.651 | |
| vs. FPSM/PRED | –0.15 | (–1.94, 1.64) | 0.832 | |
| FPSM/FP | vs. FPSM/BDP | 0.23 | (–1.56, 2.03) | 0.741 |
| vs. FPSM/PRED | 0.41 | (–1.39, 2.20) | 0.631 | |
| FPSM/BDP | vs. FPSM/PRED | 0.17 | (–1.62, 1.97) | 0.806 |
| Uncorrected CANO (ppb) | ||||
| FPSM | vs. FPSM/FP | 0.20 | (–1.33, 1.73) | 0.740 |
| vs. FPSM/BDP | 0.60 | (–0.92, 2.13) | 0.355 | |
| vs. FPSM/PRED | 0.87 | (–0.66, 2.40) | 0.213 | |
| FPSM/FP | vs. FPSM/BDP | 0.40 | (–1.13, 1.93) | 0.520 |
| vs. FPSM/PRED | 0.67 | (–0.86, 2.19) | 0.312 | |
| FPSM/BDP | vs. FPSM/PRED | 0.27 | (–1.26, 1.79) | 0.660 |
FP, fluticasone; FPSM, fluticasone/salmeterol; BDP, beclomethasone diproprionate; PRED, prednisolone.
There was no statistically significant difference between treatments for any measure of pulmonary function including spirometry, IOS, body plethysmography and bronchial challenge, although there was a numerical trend for improvement in body plethysmography with FPSM/PRED (Tables 2 and 3).
Table 3.
Lung function
| Treatment | FPSM | FPSM/FP | FPSM/BDP | FPSM/PRED |
|---|---|---|---|---|
| Spirometry | ||||
| FEV1 (l) | 2.16 (1.81 to 2.51) | 2.18 (1.82 to 2.54) | 2.21 (1.81 to 2.61) | 2.26 (1.89 to 2.63) |
| FEF25–75 (l) | 1.35 (0.98 to 1.71) | 1.29 (0.92 to 1.66) | 1.36 (0.95 to 1.77) | 1.38 (1.00 to 1.76) |
| FVC (l) | 3.42 (3.03 to 3.81) | 3.40 (3.00 to 3.81) | 3.45 (3.03 to 3.87) | 3.49 (3.08 to 3.90) |
| RVC (l) | 3.70 (3.25 to 4.16) | 3.49 (3.03 to 3.94} | 3.51 (3.06 to 3.96) | 3.66 (3.26 to 4.06) |
| FEV1 (%) | 63.4 (57.6 to 69.1) | 64.2 (59.0 to 69.4) | 64.6 (58.5 to 70.7) | 65.5 (59.6 to 71.4) |
| FEF25–75 (%) | 34.8 (26.3 to 43.3) | 34.0 (25.4 to 42.5) | 35.0 (25.7 to 44.3) | 35.6 (26.6 to 44.6) |
| FVC (%) | 83.2 (78.5 to 88.0) | 83.0 (80.4 to 85.6) | 83.9 (81.2 to 86.7) | 83.6 (78.5 to 88.7) |
| RVC (%0 | 88.0 (83.5 to 92.5) | 82.5 (77.9 to 87.0) | 82.6 (79.2 to 86.0) | 84.8 (81.3 to 88.4) |
| Impulse oscillometry | ||||
| R5 (kPa l−1 s) | 0.47 (0.39 to 0.56) | 0.45 (0.40 to 0.59) | 0.44 (0.41 to 0.66) | 0.47 (0.37 to 0.68 |
| R5-R20 | 0.13 (0.23 to 0.13) | 0.11 (0.06 to 0.23) | 0.11 (0.06 to 0.25) | 0.09 (0.03 to 0.21) |
| X5 (kPa l−1 s) | −0.15 (−0.23 to −0.13) | −0.17 (−0.24 to −0.13) | −0.15 (−0.26 to −0.12) | −0.15 (−0.33 to −0.12) |
| Body plethysmography | ||||
| sRaw (kPa s−1) | 1.87 (1.31 to 2.42) | 1.94 (1.43 to 2.45) | 2.02 (1.51 to 2.54) | 1.57 (1.02 to 2.13) |
| sRaw (%) | 166 (114 to 218) | 175 (127 to 222) | 180 (131 to 229) | 142 (93 to 192) |
| RV (l) | 3.28 (2.58 to 3.97) | 3.16 (2.80 to 3.51) | 3.44 (2.60 to 4.28) | 2.76 (2.42 to 3.10) |
| RV (%) | 159 (113 to 205) | 144 (127 to 161) | 170 (113 to 227) | 130 (117 to 143) |
| RV/TLC | 0.44 (0.38 to 0.51) | 0.46 (0.41 to 0.50) | 0.46 (0.41 to 0.52) | 0.41 (0.36 to 0.46) |
Presented as mean and (95% CI) except impulse oscillometry which is median (IQR). % shown as percent predicted for race, age and gender. FP, fluticasone; FPSM, fluticasone/salmeterol; BDP, beclomethasone diproprionate; PRED, prednisolone.
Plasma ECP, e-selectin and ICAM-1 were significantly suppressed by FPSM/PRED compared wit FPSM and FPSM/FP but not FPSM/BDP. However FPSM/BDP was not significantly reduced compared with FPSM/FP or FPSM (Figure 4, Table 2).
Figure 4.
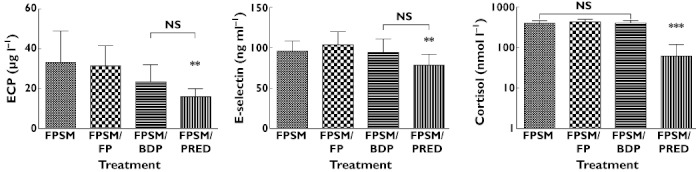
Plasma ECP, E-selectin and cortisol stratified by treatment group. Data displayed as mean and 95% confidence intervals with exception of plasma cortisol, displayed as geometric mean and 95% confidence intervals. **P < 0.05 compared with FPSM and FPSM/FP, ***P < 0.05 compared with FPSM, FPSM/ FP and FPSM/BDP. FP, fluticasone; FPSM, fluticasone/salmeterol; BDP, beclomethasone diproprionate; PRED, prednisolone
Plasma cortisol was significantly suppressed by FPSM/PRED compared with all other limbs (Figure 4, Table 2). There was no difference in overnight urinary cortisol : creatinine ratio (OUCC) for inhaled treatment (FPSM, FPSM/FP or FPSM/BDP). OUCC was not tested in the FPSM/PRED limb due to cross-reactivity of the assay to urinary metabolites.
ACQ and AQLQ values are shown (Figure 5). There was no significant difference in symptoms scores for any treatment.
Figure 5.
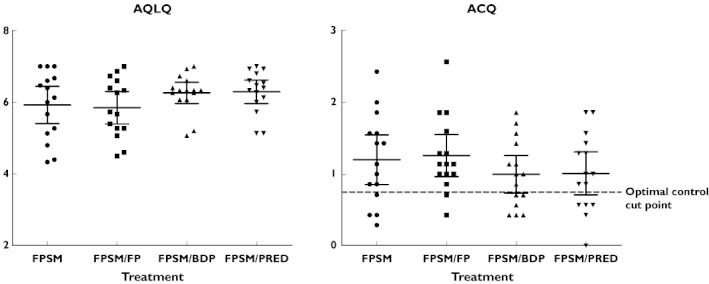
Asthma control questionnaire (ACQ) and asthma quality of life questionnaire (AQLQ) stratified by treatment group. Data displayed as mean and 95% confidence intervals. FP, fluticasone; FPSM, fluticasone/salmeterol; BDP, beclomethasone diproprionate; PRED, prednisolone
Discussion
This is the first study to examine the potential role of CANO for assessing therapies in severe asthma. Whilst early studies suggested CANO could be an attractive biomarker to assess the small airways we have demonstrated it is insufficiently sensitive to detect a dose response to inhaled corticosteroids or a response to systemic therapy.
Secondary outcomes in the present study showed that inhaled HFA-BDP produced significant reductions in FENO and JawNO when added to a maximal dose of FPSM, without causing adrenal suppression. Similar effects on FENO and JawNO were observed with oral PRED, but were associated with significant cortisol suppression. The addition of high dose FP showed a numerical trend for reduction which did not reach statistical significance (Table 2, Table 4). There was no statistically significant difference between FPSM/BDP and FPSM/FP.
‘Severe’ or ‘refractory’ asthma is difficult to characterize for research purposes and recommendations have been reviewed several times in recent years [3, 18–21]. The joint American Thoracic Society statement on refractory asthma suggests that criteria should include measures of airway obstruction and level of therapy a patient requires for stability [3]. We therefore selected participants on the basis of lung function as well as the dose of inhaled corticosteroids. In order to include a positive control limb of systemic steroids and to select a group stable enough to tolerate changes to medication we did not include subjects on long term oral corticosteroid therapy. In this regard our patients may not be considered as severe as cohorts in other studies on refractory asthma [22–24] but nonetheless represent a refractory group as evidenced by a lack of improvement in lung function and symptoms even with systemic therapy. To ensure enrolment of subjects with airflow obstruction due to asthma, we sought evidence of gas trapping with body plethysmography (mean residual volume 193% predicted), excluded current smokers or ex-smokers with >10 pack year history and confirmed bronchial hyper-reactivity in all subjects with sufficient respiratory reserve to tolerate a bronchial challenge (mean mannitol PD10 177 µg).
In order to select participants with evidence of small airways inflammation and room for further suppression of CANO, entry criteria also included a CANO > 2 ppb following the 6 week run-in period. This level was selected on the basis of pilot data, but at the time of protocol design the importance of correction for axial diffusion was not widely recognized and therefore an uncorrected value was used [25].
Whilst several studies have reported elevated levels of CANO in severe asthma, only one other study has assessed its responsiveness to corticosteroids [9, 10, 17, 25]. A number of studies have been performed in milder asthma with regards to suppression of CANO using ICS. However methods and results are varied and results have been conflicting [26]. In an uncontrolled study by Berry et al. CANO was suppressed in severe asthmatics by oral PRED but not by a doubling of inhaled FP [9]. The authors concluded that systemic treatment may be required to target adequately the small airways, in keeping with Bel et al. who have shown benefits of parenteral steroids in refractory asthma [23]. However, in the paper by Berry et al. [9], no correction for axial diffusion was applied and further inspection of the data reveals that FENO was significantly suppressed with PRED (32.4 vs. 17.8 ppb) but not by a doubling of ICS (41.6 vs. 41.3 ppb). Hence the apparent fall in uncorrected CANO may represent a significant reduction in back-diffusion rather than a true reduction in alveolar NO. In the present study there was no significant suppression of uncorrected values, but the respective changes in FENO and JawNO were far more modest (Table 2). Our findings are also consistent with a more recent observational study of 15 asthmatics demonstrating that CANO is not elevated during acute exacerbations and change in FENO output was due to flux rather than CANO[27]. This paper also suggested that after correction for JawNO, CANO was not elevated in asthma compared with age matched controls, in keeping with the lack of response in the present paper and pilot work by our department [25].
There are a number of possible reasons that CANO was not suppressed in the present study. The run-in of FPSM may have maximally suppressed CANO preventing any further suppression. The run-in period included a dose-ramp from FPSM 500 µg day−1 to FPSM 1000 µg day−1 to assess if a dose–response to CANO could be demonstrated. As in the main study, this showed a dose–response in FENO and JawNO but not corrected CANO (data not shown). It has been shown that for FENO there is a level of maximal suppression for an individual which varies dependent on factors such as age, gender, atopy and height [28]. Similarly, it is plausible there is a level of maximal suppression for CANO. If so, inclusion of individuals with a CANO >2 ppb on FPSM 1000 µg day−1 may have inadvertently selected individuals maximally suppressed at a high level, rather than allowing further ‘room for improvement’ as initially hypothesized. Finally it is possible that the steroids simply have no significant effect on CANO in severe asthma, as has been suggested in COPD [29].
It has been suggested that small airway disease may be an important target for asthma therapy. With the development of extra-fine particle ICS it is now possible to achieve greater small airways drug deposition [30]. This is particularly pertinent in individuals with airflow obstruction as this leads to more central distribution of inhaled therapies [31]. We had hypothesized that extra-fine HFA-BDP may achieve additional suppression of CANO compared with a biological equivalent dose of coarse particle ICS. Whilst this was not observed, extra-fine BDP achieved significant suppression of FENO and JawNO compared with FPSM without causing adrenal suppression. Similarly whilst FPSM/PRED significantly suppressed systemic markers of asthmatic inflammation (ECP, e-selectin and ICAM-1) compared with FPSM and FPSM/FP, they were not significantly lower than extra-fine HFA-BDP (Table 2). The consistency of this trend across ECP, e-selectin and ICAM-1 would suggest that a larger study powered for these markers may have demonstrated significant suppression with FPSM/BDP compared with FPSM and FPSM/FP, though this cannot be confirmed with the present data. Alternatively, it is possible that systemic markers of inflammation can only be suppressed with appreciable systemic bioavailability, which was demonstrated for PRED but not inhaled therapies. In this regard only moderate doses of HFA-BDP were used as add-on therapy. Hence suppression of inflammatory markers and cortisol may have been observed at higher doses. Whilst the combined doses of inhaled therapy in the study would be very high for most asthmatics, it should be recognized that severe airflow obstruction reduces the lung bioavailability of inhaled steroid as has been shown previously with FP [32–35].
Although HFA-BDP showed additional suppression of FENO and flux, the clinical significance of such changes in steroid treated asthmatics is not established. Smith et al. have examined ‘personal best FENO’ in 73 non-severe asthmatics comparing FENO at a threshold where control is lost, ‘optimized’ inhaled FP and oral corticosteroid. They also found levels were significantly lower on oral steroid compared with optimized inhaled FP, but had no extra-fine particle comparator [28]. Further adequately powered studies would be required to establish whether extra-fine particle ICS could achieve near ‘personal best’ FENO and whether this would confer greater asthma control with long term therapy.
We were also interested to see that there was a non-significant numerical trend towards improvement in mannitol airway hyperreactivity with FPSM/BDP, though this was less than the biological variability of one doubling dilution. Again, larger studies would be warranted to assess the relative benefits of different particle size over a wider dose range and sufficiently powered to assess effects on mannitol challenge, exacerbations and systemic inflammatory markers.
For lung function, whilst there was a numerical trend for improvement with FPSM/PRED, there were no statistically significant changes. These were secondary outcomes and as such the study was not sufficiently powered to detect small changes. Furthermore, we felt it unethical to use our standard medication withholding time of three half-lives because of our cohorts relative instability. Instead we asked participants to use their study medication on the morning of the visit and as such measurements of lung function, IOS and body plethysmography represent post bronchodilator measurements. Any additional bronchodilator effect from corticosteroids is therefore likely to be small and difficult to detect even with techniques sensitive to changes in airway obstruction undetectable by spirometry alone [36]. Similarly, no significant improvement was seen in symptom scores. We would interpret the lack of improvement in symptoms and lung function, even on oral therapy, as good evidence of the refractory nature of our cohort's asthma. Lung function and symptoms were secondary outcomes and as such the study was not powered for these outcomes. Large long term studies would be required to confirm or refute whether changes in NO would translate to clinically meaningful patient outcomes.
We must acknowledge that our study had no placebo control arm which is always desirable in clinical trial design. The severity of our patients meant that a true placebo arm with no therapy was not possible. Instead a ‘positive’ control arm was used to characterize maximal suppression. We believe this is still a clinically meaningful comparison in individuals who, by definition, have treatment resistant disease. We acknowledge that our cohort was older than a general population of severe asthmatics, perhaps reflecting a population willing and able to engage in active clinical research. We acknowledge several further limitations to our study design which were required to minimize risks of exacerbation in a severe cohort: a baseline with a full washout would have been potentially hazardous, full bronchial challenge in all patients would have been dangerous due to low FEV1, as would inhalation of hypertonic saline for induced sputum. The stringency of the inclusion criteria meant that numbers were necessarily limited, though a cross-over design was employed to maximize statistical power. Finally, some may feel that our study design was contrived as addition of high dose ICS to combination therapy is not a standard approach in refractory disease and is not included in guidelines. Whilst we acknowledge this, we feel there is a paucity of data to inform on a pharmacological approach to refractory asthma and much of the published work focuses on non-pharmacological and co-morbid aspects of disease. We are aware anecdotally of pulmonologists who may indeed add high dose ICS to combination therapy rather than step-up to maintenance dose oral corticosteroid. Therefore whilst the study design is artificial it is nonetheless of interest pharmacologically.
In conclusion, in severe asthma, inhaled HFA-BDP produced additional reductions in FENO and JawNO without adrenal suppression. Oral PRED produced similar effects but with additional suppression of systemic inflammatory markers and cortisol. There was a numerical trend for reduction with FP but this did not reach statistical significance and no significant difference between FPSM/BDP and FPSM/FP. Alveolar NO is insensitive to changes in dose and delivery of ICS and is not suppressed by systemic corticosteroids. This suggests that CANO is either an insensitive test of reversible small airway disease, or that this cohort of patients require non-steroidal immunosuppressive treatments. CANO is therefore unlikely to be a useful tool in measuring response to treatments targeted at small airway disease in refractory asthma.
Competing Interests
BJL has received unrestricted educational grant support from TEVA for the present study and has also received funds for giving post graduate educational talks and attending advisory boards for TEVA. There are no other competing interests to declare.
Source of funding
Investigator led study supported by an unrestricted educational grant from TEVA Pharmaceuticals Inc. USA.
Contributions
Conception and design: PAW, SV, BJL. Analysis and interpretation: PAW, PMS, BJL. Drafting of manuscript for important intellectual content: PAW, PMS, SV, BJL.
REFERENCES
- 1.Brightling CE, Gupta S, Gonem S, Siddiqui S. Lung damage and airway remodelling in severe asthma. Clin Exp Allergy. 2012;42:638–49. doi: 10.1111/j.1365-2222.2011.03917.x. May. [DOI] [PubMed] [Google Scholar]
- 2.Jeffery PK. Remodeling in asthma and chronic obstructive lung disease. Am J Respir Crit Care Med. 2001;164:S28–38. doi: 10.1164/ajrccm.164.supplement_2.2106061. [DOI] [PubMed] [Google Scholar]
- 3.American Thoracic Society. Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. Am J Respir Crit Care Med. 2000;162:2341–51. doi: 10.1164/ajrccm.162.6.ats9-00. [DOI] [PubMed] [Google Scholar]
- 4.Carroll N, Elliot J, Morton A, James A. The structure of large and small airways in nonfatal and fatal asthma. Am Rev Respir Dis. 1993;147:405–10. doi: 10.1164/ajrccm/147.2.405. [DOI] [PubMed] [Google Scholar]
- 5.Chen FH, Chen ZG, Chen H, Ji JZ, Chen YF, Peng BX, Shioda SJ. [Correlation of reticular basement membrane thickness and airway wall remolding in asthma patients] Zhonghua Yi Xue Za Zhi. 2006;86:468–71. [PubMed] [Google Scholar]
- 6.Taylor DR. Nitric oxide as a clinical guide for asthma management. J Allergy Clin Immunol. 2006;117:259–62. doi: 10.1016/j.jaci.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Tsoukias NM, George SC. A two-compartment model of pulmonary nitric oxide exchange dynamics. J Appl Physiol. 1998;85:653–66. doi: 10.1152/jappl.1998.85.2.653. [DOI] [PubMed] [Google Scholar]
- 8.George SC, Hogman M, Permutt S, Silkoff PE. Modeling pulmonary nitric oxide exchange. J Appl Physiol. 2004;96:831–9. doi: 10.1152/japplphysiol.00950.2003. [DOI] [PubMed] [Google Scholar]
- 9.Berry M, Hargadon B, Morgan A, Shelley M, Richter J, Shaw D, Green RH, Brightling C, Wardlaw AJ, Pavord ID. Alveolar nitric oxide in adults with asthma: evidence of distal lung inflammation in refractory asthma. Eur Respir J. 2005;25:986–91. doi: 10.1183/09031936.05.00132404. [DOI] [PubMed] [Google Scholar]
- 10.van Veen IH, Sterk PJ, Schot R, Gauw SA, Rabe KF, Bel EH. Alveolar nitric oxide versus measures of peripheral airway dysfunction in severe asthma. Eur Respir J. 2006;27:951–6. doi: 10.1183/09031936.06.00087905. [DOI] [PubMed] [Google Scholar]
- 11.Condorelli P, Shin HW, Aledia AS, Silkoff PE, George SC. A simple technique to characterize proximal and peripheral nitric oxide exchange using constant flow exhalations and an axial diffusion model. J Appl Physiol. 2007;102:417–25. doi: 10.1152/japplphysiol.00533.2006. [DOI] [PubMed] [Google Scholar]
- 12.Kerckx Y, Michils A, Van Muylem A. Airway contribution to alveolar nitric oxide in healthy subjects and stable asthma patients. J Appl Physiol. 2008;104:918–24. doi: 10.1152/japplphysiol.01032.2007. [DOI] [PubMed] [Google Scholar]
- 13.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, Jensen R, Johnson DC, MacIntyre N, McKay R, Navajas D, Pedersen OF, Pellegrino R, Viegi G, Wanger J. Standardisation of spirometry. Eur Respir J. 2005;26:319–38. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 14.Williamson PA, Short PM, Clearie KL, Vaidyanathan S, Fardon TC, Howaniec LJ, Lipworth BJ. Paradoxical trough effects of triple therapy with budesonide/formoterol and tiotropium bromide on pulmonary function outcomes in COPD. Chest. 2010;138:595–604. doi: 10.1378/chest.10-0247. Sep. [DOI] [PubMed] [Google Scholar]
- 15.Clearie KL, Jackson CM, Fardon TC, Williamson PA, Vaidyanathan S, Burns P, Lipworth BJ. Supervised step-down of inhaled corticosteroids in the community – an observational study. Respir Med. 2011;105:558–65. doi: 10.1016/j.rmed.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Tsoukias NM, Shin HW, Wilson AF, George SC. A single-breath technique with variable flow rate to characterize nitric oxide exchange dynamics in the lungs. J Appl Physiol. 2001;91:477–87. doi: 10.1152/jappl.2001.91.1.477. [DOI] [PubMed] [Google Scholar]
- 17.Brindicci C, Ito K, Barnes PJ, Kharitonov SA. Differential flow analysis of exhaled nitric oxide in patients with asthma of differing severity. Chest. 2007;131:1353–62. doi: 10.1378/chest.06-2531. [DOI] [PubMed] [Google Scholar]
- 18.Bel EH, Sousa A, Fleming L, Bush A, Chung KF, Versnel J, Wagener AH, Wagers SS, Sterk PJ, Compton CH. Diagnosis and definition of severe refractory asthma: an international consensus statement from the Innovative Medicine Initiative (IMI) Thorax. 2011;66:910–7. doi: 10.1136/thx.2010.153643. [DOI] [PubMed] [Google Scholar]
- 19.Chung KF, Godard P, Adelroth E, Ayres J, Barnes N, Barnes P, Bel E, Burney P, Chanez P, Connett G, Corrigan C, de Blic J, Fabbri L, Holgate ST, Ind P, Joos G, Kerstjens H, Leuenberger P, Lofdahl CG, McKenzie S, Magnussen H, Postma D, Saetta M, Salmeron S, Sterk P. Difficult/therapy-resistant asthma: the need for an integrated approach to define clinical phenotypes, evaluate risk factors, understand pathophysiology and find novel therapies. ERS Task Force on Difficult/Therapy-Resistant Asthma. European Respiratory Society. Eur Respir J. 1999;13:1198–208. doi: 10.1034/j.1399-3003.1999.13e43.x. [DOI] [PubMed] [Google Scholar]
- 20.Heaney LG, Robinson DS. Severe asthma treatment: need for characterising patients. Lancet. 2005;365:974–6. doi: 10.1016/S0140-6736(05)71087-4. [DOI] [PubMed] [Google Scholar]
- 21.Holgate ST, Polosa R. The mechanisms, diagnosis, and management of severe asthma in adults. Lancet. 2006;368:780–93. doi: 10.1016/S0140-6736(06)69288-X. [DOI] [PubMed] [Google Scholar]
- 22.Gamble J, Stevenson M, McClean E, Heaney LG. The prevalence of nonadherence in difficult asthma. Am J Respir Crit Care Med. 2009;180:817–22. doi: 10.1164/rccm.200902-0166OC. [DOI] [PubMed] [Google Scholar]
- 23.ten Brinke A, Zwinderman AH, Sterk PJ, Rabe KF, Bel EH. ‘Refractory’ eosinophilic airway inflammation in severe asthma: effect of parenteral corticosteroids. Am J Respir Crit Care Med. 2004;170:601–5. doi: 10.1164/rccm.200404-440OC. [DOI] [PubMed] [Google Scholar]
- 24.Heaney LG, Brightling CE, Menzies-Gow A, Stevenson M, Niven RM. Refractory asthma in the UK: cross-sectional findings from a UK multicentre registry. Thorax. 2010;65:787–94. doi: 10.1136/thx.2010.137414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williamson PA, Clearie K, Menzies D, Vaidyanathan S, Lipworth BJ. Assessment of small-airways disease using alveolar nitric oxide and impulse oscillometry in asthma and COPD. Lung. 2011;189:121–9. doi: 10.1007/s00408-010-9275-y. [DOI] [PubMed] [Google Scholar]
- 26.Barnes PJ, Dweik RA, Gelb AF, Gibson PG, George SC, Grasemann H, Pavord ID, Ratjen F, Silkoff PE, Taylor DR, Zamel N. Exhaled nitric oxide in pulmonary diseases: a comprehensive review. Chest. 2010;138:682–92. doi: 10.1378/chest.09-2090. [DOI] [PubMed] [Google Scholar]
- 27.Gelb AF, George SC, Silkoff PE, Krishnan A, Fraser C, Taylor CF, Shinar CM, Maginot T. Central and peripheral airway/alveolar sites of exhaled nitric oxide in acute asthma. Thorax. 2010;65:619–25. doi: 10.1136/thx.2009.132696. [DOI] [PubMed] [Google Scholar]
- 28.Smith AD, Cowan JO, Taylor DR. Exhaled nitric oxide levels in asthma: personal best versus reference values. J Allergy Clin Immunol. 2009;124:714–8. doi: 10.1016/j.jaci.2009.07.020. e4. [DOI] [PubMed] [Google Scholar]
- 29.Gelb AF, Flynn Taylor C, Krishnan A, Fraser C, Shinar CM, Schein MJ, Osann K. Central and peripheral airway sites of nitric oxide gas exchange in COPD. Chest. 2010;137:575–84. doi: 10.1378/chest.09-1522. [DOI] [PubMed] [Google Scholar]
- 30.Usmani OS, Biddiscombe MF, Barnes PJ. Regional lung deposition and bronchodilator response as a function of beta2-agonist particle size. Am J Respir Crit Care Med. 2005;172:1497–504. doi: 10.1164/rccm.200410-1414OC. [DOI] [PubMed] [Google Scholar]
- 31.Saari SM, Vidgren MT, Koskinen MO, Turjanmaa VM, Waldrep JC, Nieminen MM. Regional lung deposition and clearance of 99mTc-labeled beclomethasone-DLPC liposomes in mild and severe asthma. Chest. 1998;113:1573–9. doi: 10.1378/chest.113.6.1573. [DOI] [PubMed] [Google Scholar]
- 32.Brutsche MH, Brutsche IC, Munawar M, Langley SJ, Masterson CM, Daley-Yates PT, Brown R, Custovic A, Woodcock A. Comparison of pharmacokinetics and systemic effects of inhaled fluticasone propionate in patients with asthma and healthy volunteers: a randomised crossover study. Lancet. 2000;356:556–61. doi: 10.1016/S0140-6736(00)02581-2. [DOI] [PubMed] [Google Scholar]
- 33.Weiner P, Berar-Yanay N, Davidovich A, Magadle R. Nocturnal cortisol secretion in asthmatic patients after inhalation of fluticasone propionate. Chest. 1999;116:931–4. doi: 10.1378/chest.116.4.931. [DOI] [PubMed] [Google Scholar]
- 34.Mortimer KJ, Harrison TW, Tang Y, Wu K, Lewis S, Sahasranaman S, Hochhaus G, Tattersfield AE. Plasma concentrations of inhaled corticosteroids in relation to airflow obstruction in asthma. Br J Clin Pharmacol. 2006;62:412–9. doi: 10.1111/j.1365-2125.2006.02712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee DK, Bates CE, Currie GP, Cowan LM, McFarlane LC, Lipworth BJ. Effects of high-dose inhaled fluticasone propionate on the hypothalamic-pituitary-adrenal axis in asthmatic patients with severely impaired lung function. Ann Allergy Asthma Immunol. 2004;93:253–8. doi: 10.1016/S1081-1206(10)61497-4. [DOI] [PubMed] [Google Scholar]
- 36.Williamson PA, Short PM, Clearie KL, Vaidyanathan S, Fardon TC, Howaniec LJ, Lipworth BJ. Paradoxical trough effects of triple therapy with budesonide/formoterol and tiotropium bromide on pulmonary function outcomes in COPD. Chest. 2010;138:595–604. doi: 10.1378/chest.10-0247. [DOI] [PubMed] [Google Scholar]


