Thoracic Surgery is a continuous evolving specialty. In the past, thoracic surgeons had to make large incisions in order to operate any pathology inside the chest. This often meant big, painful and ugly scars and long recovery times after surgery. But he history of thoracic surgery changed since the begining of video-assisted thoracoscopic surgery (VATS).
Hans Christian Jacobaeus provided the first description of a thoracoscopy in 1910 (1). During decades the role of thoracocopy was only related to diagnostic and minor therapeutic procedures. Since the past two decades, thoracoscopic procedures have increasingly gained acceptance specially with the introduction of VATS major pulmonary resections (2).
Although there is no standardised technique for the thoracoscopic approach used in this type of procedure, most groups use a utility incision of about 4-6 cm, and add between 1-3 ancillary incisions, i.e., there is variability in the number of incisions used, depending on the centre in question. The most common approach comprises a utility incision plus two supporting incisions, i.e., three ports, and a very important consideration is the obviation of rib-spreading (3).
The use of multiple ports seems to entail more facilities for performing VATS lung resection and provides different angles for hilar dissection and lymphadenectomy. However, the performance of a lobectomy can be accomplished by only one incision with similar results (4). With increased experience in VATS lobectomy, we have gradually improved less invasive techniques and thanks to the advances in the field of thoracoscopic surgery the indications and contraindications for lung cancer treatment have been changed overtime.
We evolved from the conventional VATS to a single incision approach after gained experience via three ports. The first step was to avoid the posterior incision to perform cases by the double port technique (5), and the second step was avoid the inferior incision and insert the camera and the instruments through the utility incision (Figure 1).
Figure 1.
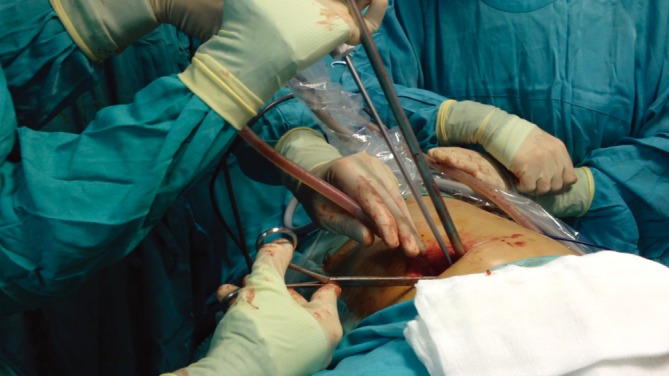
Surgical instrumentation (camera placed in the posterior part of the incision)
We started to perform major pulmonary resections by uniportal approach in 2010 in our department (6). No other reports were described in the literature before. Actually we apply the single-port technique for most major resections including advanced and complex cases (7). To date we have performed 430 single-port VATS pulmonary resections (140 were lobectomies) through a single-incision (Figure 2) with excellent postoperative results.
Figure 2.

Postoperative result with chest tube placed through the incision
The advantage of using the camera in coordination with the instruments is that the vision is directed to the target tissue, bringing the instruments to address the target lesion from a straight perspective, thus we can obtain similar angle of view as for open surgery (Figure 3). Coventional three-port triangulation creates a new optical plane with genesis of dihedral or torsional angle that is not favorable with standard two-dimension monitors. Instruments inserted parallel to the videothoracoscope also mimic inside the chest maneuvers performed during open surgery. There is a physical and mathematical demonstration about better view and instrumentation obtained in the uniportal VATS over conventional approach. Other potential advantage could be less postoperative pain: only one intercostal space is involved and avoiding the use of a trocar could minimize the risk of intercostal nerve injury. Further studies will be required to demonstrate other geometric aspects like ergonomy and that there is less pain with single incision techniques, compared to conventional VATS for lobectomy.
Figure 3.

Surgeons position (anterior location)
On the other hand technology improves and there is no question that robotic surgery has an important role in the future of thoracic minimally invasive surgery. Over the past 10 years, robotics have revolutionized surgery, and new innovations are continuing to push the boundaries of surgery (8). We are currently in a phase of rapid growth and dissemination of the applications for robotic surgical technology within thoracic surgery (9).
The first generation of robotic technology appeared twenty years ago (10). The robot lets surgeons carry out keyhole surgery remotely, allowing them to control robot arms from a console that also provides a three-dimensional image of the proceedings. The idea to develop robotic surgery platforms evolved from the need to improve the precision of surgical techniques. There is no doubt that robotics will be always more precise than even the most skilled surgeon with the steadiest hand. This development is growing and probably will allow surgeons to perform extremely complex surgical procedures using a minimally invasive approach through a small single hole in a near future.
Anyway nowadays, in my opinion, there are several disadvantages with robotic pulmonary resection: still is a hybrid procedure (robot makes the dissection and VATS is used for staplers) high cost, the need of 3-4 incisions, time-consuming procedure, difficulties to detect nodule lesions and to solve a major bleeding event. However, several advantages of the robot over VATS are clear: instrumentation with more degree of motion and perfect 3D view, specially to achieve a radical lymph node dissection and teaching residents (robotic lobectomy can be performed with no previous VATS experience) (11).
Therefore the adoption of new emergent robotic technology and the minimization of surgical aggression is a recommendable way to follow (12,13). We truly believe on the use of the single port technique for major pulmonary resections because we understand that the future goes in that direction, i.e., robotics and single-port. The instruments that would be necessary develop in the next future for single port robotic surgery should be vessel and bronchus sealer devices, snake-like arms inside the chest for instrumentation, wireless cameras and feedback robotic tactile Systems. We have to be open to the new therapies and the next robotic era because the future of lung cancer treatment probably will be related to genetic, selective molecular chemotherapy and microrobotic technology.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- 1.Jacobaeus H.Über die Möglichkeit die Zystoskopie bei Untersuchung seröser Höhlungen anzuwenden. Munch Med Wochenschr 1910;57:2 [Google Scholar]
- 2.Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7 [PubMed] [Google Scholar]
- 3.McKenna RJ, Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6 [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5 [DOI] [PubMed] [Google Scholar]
- 5.Burfeind WR, D’Amico TA. Thoracoscopic lobectomy- Operative Techniques. Thoracic and Cardiovascular Surgery 2004;9:98-114 [Google Scholar]
- 6.Gonzalez-Rivas D, Fernandez R, De la Torre M, et al. Thoracoscopic lobectomy through a single incision. MMCTS 2012. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7 [DOI] [PubMed] [Google Scholar]
- 8.Swanson SJ. Robotic pulmonary lobectomy--the future and probably should remain so. J Thorac Cardiovasc Surg 2010;140:954. [DOI] [PubMed] [Google Scholar]
- 9.Cerfolio RJ, Bryant AS. Perspectives on robotic pulmonary resection: It’s current and future status. Ann Cardiothorac Surg 2012;1:59-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park BJ. Robotic lobectomy for non-small cell lung cancer (NSCLC): Multi-registry study of long-term oncologic results. Ann Cardiothorac Surg 2012;1:24-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cerfolio RJ, Bryant AS, Minnich DJ. Starting a robotic program in general thoracic surgery: why, how, and lessons learned. Ann Thorac Surg 2011;91:1729-36; discussion 1736-7. [DOI] [PubMed]
- 12.Park BJ. Cost concerns for robotic thoracic surgery. Ann Cardiothorac Surg 2012;1:56-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cao C, Manganas C, Ang SC, et al. A systematic review and meta-analysis on pulmonary resections by robotic video-assisted thoracic surgery. Ann Cardiothorac Surg 2012;1:3-10 [DOI] [PMC free article] [PubMed] [Google Scholar]


