Summary
Aims
the aim of this study was to analyse the awareness of oral cancer among young adults in the city of Rome.
Materials and methods
during the orientation period for new graduates students, or “Porte aperte”, organised by the Sapienza University of Rome in July 2009 and 2010, a survey among young people regarding their knowledge on the risk factors, the importance of early diagnosis, and the methods for primary and secondary prevention of oral cancer was conducted. A total of 1125 questionnaires were administered to subjects who agreed to respond to assess the level of knowledge of the disease.
Results
only 45.3% of the sample population was aware of the existence of oral cancer; among these individuals, 36.9% did not perceive seriousness of the malignancy. High school students who attended a scientific high school knew the risk factors better than the students who attended classical and technical high school.
Conclusions
rigorous educational programs along with diagnostic strategies promise to reduce the burden of oral cancer. The data obtained from this study highlight the need to increase health education, especially among young people in humanistic or technical high schools and universities (Classical High School, Technical Institutes, Faculty of Letters, Faculty of Law) where there is a lack of knowledge concerning oral cancer prevention.
Keywords: oral cancer, prevention, late diagnosis
Introduction
Oral cancer is one of the most common cancers worldwide and is highly invasive and debilitating. With approximately 6000 new cases per year in Italy, oral cancer represents a public health problem. Squamous cell carcinoma of the oral cavity represents about 2% of all malignant neoplasms and 47% of those developing in the head and neck area, with survival rates that are among the lowest of all major cancers. More deadly than breast cancer, cervical cancer and prostate cancer, oral cancer was estimated to kill one person every hour, every day (1,2). The tongue is the most common site involved, and this incidence is increasing mainly in young people, possibly related to human papilloma virus infections. Prognosis depends on the stage: the 5-year survival rate of tongue squamous cell carcinoma, whatever the T stage, is 73% in pN0 cases, 40% in patients with positive nodes without extracapsular spread (pN1 ECS−), and 29% when nodes are metastatic with extracapsular spread (pN1 ECS+: p ≥ 0.0001) (3–6).
These statistics are dramatic, especially if we consider that the disease arises in the foreground on the oral mucosa, which is easily accessible to endoral objective examination. Thus, the lesions are ignored or not observed by patients or healthcare professionals. In part, the late diagnosis may result from an incomplete understanding or a lack of awareness that small asymptomatic lesions have a significant malignant potential.
Furthermore, a delay in diagnosis or monitoring of the disease in advanced stages may be caused by the patient or health personnel (7). Health education with programs designed to motivate patients to undergo periodic checks are the best way to promote prevention (8).
Dental health care providers play a key role in the prevention of oral cancer; these health workers, with the detection of neoplastic disease and the proper health education, contribute to the reduction of poor outcomes from this serious disease. Recent research conducted in a group of Italian cancer centres demonstrated that an average of 6 months elapses between the diagnosis of cancer and the start of an appropriate therapy, a period that irreversibly influences the therapeutic approach to this disease. It is reasonable that all patients who present symptoms of suspected neoplastic nature have access to a specialist visit no later than 2 weeks from the first contact with services and to have a definitive diagnosis no later than one month (objective set by the British National Health Service in relation to time considered desirable in cancer diagnos) (9). Currently, early diagnosis is, for many neoplastic diseases, essential to achieve good therapeutic results, with a positive impact in terms of not only prolonged survival but also improved quality of life (10,11). An early cancer diagnosis made when the disease is not at an advanced stage allows the possibility to offer the patient surgical techniques that are less invasive and destructive.
Thus, early diagnosis represents an important chapter of cancer care that must be solved by services through two different points of view:
- the view of a single patient who presents as a “suspect case” with the target of rapid diagnosis, obtained through a careful clinical examination by operators able to identify the symptoms that qualify the patient as the bearer of a possible tumour;
- the view of the whole population whose goal is early diagnosis when the disease has not yet clinically manifested itself by offering participation in screening programs.
This project, was set-up as a campaign to raise awareness of such a disease that, despite being serious, is only little known to the general public.
Materials and methods
In the orientation period for high school graduates students, organised by the Sapienza University of Rome in July 2009 and 2010, a survey among young people was conducted. The survey concerned the knowledge of risk factors, importance of early diagnosis, and the methods of primary and secondary prevention of oral cancer (12). During the three days of the “Porte aperte alla Sapienza”, a team of students enrolled to the degree course of Dentistry has been working at the stand dedicated to the Faculty of Medicine and Odontology. This group administered 1125 questionnaires to subjects who agreed to participate (661 subjects in 2009 and 464 subjects in 2010) to assess the knowledge of oral disease within this population. Data were collected regarding the type of work or study activities, the age of population, the presence of doctors in the family context and the possibility to made preventive specialist check-ups (Tabs.1-4).
Table 1.
Sample composition.
| Category | Frequency | Percentage |
|---|---|---|
| High School students | 402 | 35.7 |
|
| ||
| Classical High School | 130 | 11.6 |
| Scientific High School | 167 | 14.8 |
| Technical High School | 105 | 9.3 |
|
| ||
| University students | 475 | 42.2 |
|
| ||
| Law | 122 | 10.8 |
| Letters and Philosophy | 118 | 10.5 |
| Medicine and Surgery | 112 | 10.0 |
| SMFN* | 123 | 10.9 |
|
| ||
| Other | 248 | 22.1 |
|
| ||
| Total | 1125 | 100 |
Faculty of Mathematical, Physical and Natural Sciences
Table 2.
Sample age.
| Type Activities | Mean | N | SD | Median | Minimum | Maximum |
|---|---|---|---|---|---|---|
| Workers | 37.35 | 248 | 7.786 | 37.00 | 24 | 61 |
| High School students | 18.75 | 402 | 1.097 | 19.00 | 16 | 25 |
| University students | 21.79 | 475 | 2.462 | 21.00 | 18 | 29 |
| Total | 24.13 | 1125 | 8.219 | 21.00 | 16 | 61 |
Table 3.
Questionnaire administered.
| Question | Frequency | Percentage | |
|---|---|---|---|
| 1. Have you ever heard about the oral cancer? | No | 615 | 54.7 |
| Yes | 510 | 45.3 | |
| Tot. | 1125 | 100.0 | |
|
| |||
| 2. Oral cancer is a benign or malignant tumour? | Malignant | 493 | 43.8 |
| Benign | 83 | 7.4 | |
| Do not know | 549 | 48.8 | |
| Tot. | 1125 | 100.0 | |
|
| |||
| 3. Smoking may increase the risk of developing oral cancer? | No | 24 | 2.1 |
| Yes | 903 | 80.3 | |
| Do not know | 198 | 17.6 | |
| Tot. | 1125 | 100.0 | |
|
| |||
| 4. Alcohol may increase the risk of developing oral cancer? | No | 194 | 17.2 |
| Yes | 474 | 42.2 | |
| Do not know | 457 | 40.6 | |
| Tot. | 1125 | 100.0 | |
|
| |||
| 5. A long exposure to sunlight may contribute to the onset of oral cancer? | No | 317 | 28.2 |
| Yes | 230 | 20.4 | |
| Do not know | 578 | 51.4 | |
| Tot. | 1125 | 100.0 | |
|
| |||
| 6. Early diagnosis of oral cancer may help? | No | 8 0.7 | |
| Yes | 893 | 79.4 | |
| Do not know | 224 | 19.9 | |
| Tot. | 1125 | 100.0 | |
|
| |||
| 7. Do you know that you can make a visit for prevention of oral cancer? | No | 638 | 56.7 |
| Yes | 487 | 43.3 | |
| Tot. | 1125 | 100.0 | |
|
| |||
| 8. Have you ever made a dentist’s visit for prevention of oral cancer? | No | 1093 | 97.2 |
| Yes | 32 | 2.8 | |
| Tot. | 1125 | 100.0 | |
|
| |||
| 9. Has your dentist ever proposed a prevention visit to you? | No | 1102 | 98.0 |
| Yes | 23 | 2.0 | |
| Tot. | 1125 | 100.0 | |
|
| |||
| 10. Do you think that it is helpful to make a prevention visit even if there are no symptoms? | No | 30 | 2.7 |
| Yes | 908 | 80.7 | |
| Do not know | 187 | 16.6 | |
| Tot. | 1125 | 100.0 | |
Table 4.
Knowledge of oral cancer in the sample.
| Question 1: Have you ever heard about oral cancer? | ||||
|---|---|---|---|---|
|
|
||||
| No | Yes | |||
|
| ||||
| Frequency | Percentage | Frequency | Percentage | |
|
|
||||
| Question 2: Oral cancer is a benign or malignant tumour? | ||||
| Malignant | 171 | 27.8 | 322 | 63.1 |
| Benign | 56 | 9.1 | 27 | 5.3 |
| Do not know | 388 | 63.1 | 161 | 31.6 |
| Tot. | 615 | 100.0 | 510 | 100.0 |
|
| ||||
| Presence of family members who practice medical disciplines | ||||
| No | 478 | 77.7 | 347 | 68.0 |
| Yes | 137 | 22.3 | 163 | 32.0 |
| Tot. | 615 | 100.0 | 510 | 100.0 |
Afterwards informational brochures (13) were distributed to the students illustrating the incidence of various risk factors, the general characteristics of the disease, the signs and symptoms and what to do when they are present. Our work has focused on risk factors that the international scientific literature indicates as being the most involved in the aetiopathogenesis of oral cancer, i.e., smoking, alcohol and sunlight (14–23).
Statistical analysis
The data are reported using frequency counts and percentages. To evaluate the possible associations between variables the chi-squared test or the Fisher’s exact test were used, where appropriate. Tests are adjusted for all pairwise comparisons within a row of each innermost subtable using the Bonferroni correction. The statistical significance was set at 5%, and the analysis was conducted with SPSS v13.
Results
A total of 1125 questionnaires were completed, which could be divided into the following populations: 248 workers (22.1%), 402 High School students (35.7%), and 475 University students (42.2%).
The High School students were further subdivided into the following groups: 130 from Classical High School (11.6%), 167 from Scientific High School (14.8%), and 105 from Technical High School (9.3%). The university students were further subdivided into the following groups: 122 frequented the Faculty of Law (10.8%), 118 the Faculty of Letters and Philosophy (10.5%), 112 the Faculty of Medicine and Surgery (10.0%), and 123 the Faculty of Mathematical, Physical and Natural Sciences – SMFN (10.9%).
Of the entire study population, 45.3% (510 subjects) knew of the existence of oral cancer; among these, 36.9% (444 subjects) do not perceive the seriousness of the malignancy. There is a statistically significant difference in the perception of malignancy between those ones who have heard about oral cancer and those who have not (p<0.0001). Importantly, having a family member who practices a medical discipline significantly improved knowledge of the disease (54.3%) (p<0.0001) (Tab.4).
The highest results were obtained among the University students of scientific faculties, which largely knew about oral cancer (74% Faculty of Medicine and Surgery; 65% Faculty of Mathematical, Physical and Natural Sciences). A university education increases knowledge of oral cancer in a statistically significant way in comparison with the high school students (p<0.0001) (Tabs. 3,5).
Table 5.
Knowledge of oral cancer per category.
| Question 1: Have you ever heard about oral cancer? | ||||
|---|---|---|---|---|
|
|
||||
| No | Yes | |||
|
| ||||
| Category | Frequency | Percentage | Frequency | Percentage |
| High School students | 256 | 41.6 | 146 | 28.6 |
| Classical High School | 68 | 11.1 | 62 | 12.2 |
| Scientific High School | 123 | 20.0 | 44 | 8.6 |
| Technical High School | 65 | 10.5 | 40 | 7.8 |
|
| ||||
| University stundents | 221 | 35.9 | 254 | 49.8 |
| Law | 79 | 12.8 | 43 | 8.4 |
| Letters and Philosophy | 70 | 11.4 | 48 | 9.4 |
| Medicine and Surgery | 29 | 4.7 | 83 | 16.3 |
| SMFN * | 43 | 7 | 80 | 15.7 |
|
| ||||
| Other | 138 | 22.5 | 110 | 21.6 |
|
| ||||
| Total | 615 | 100.0 | 510 | 100.0 |
Faculty of Mathematical, Physical and Natural Sciences
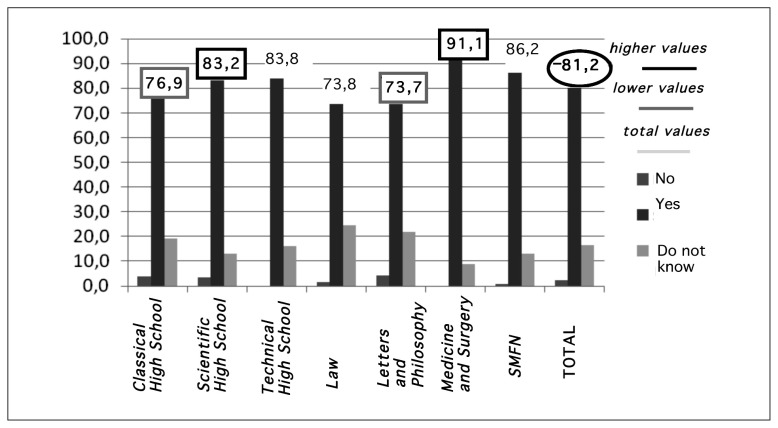
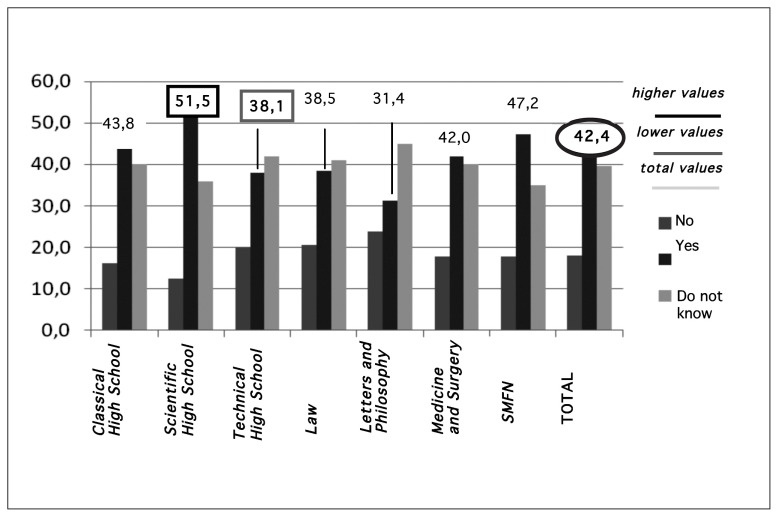
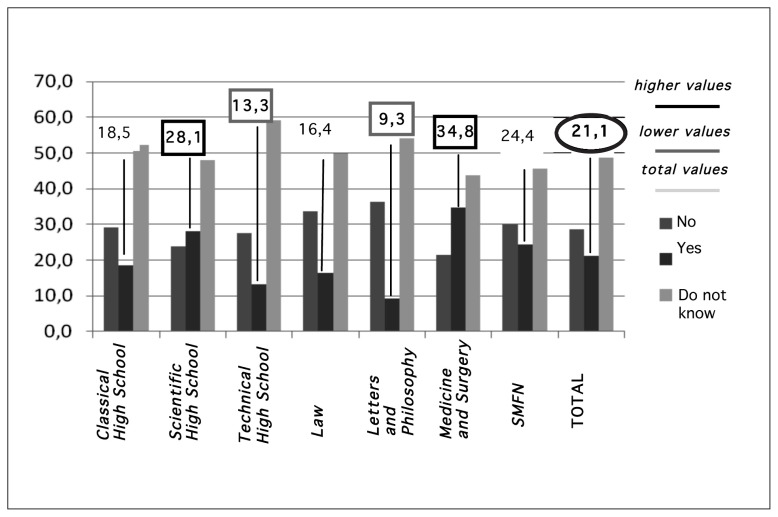
Of those interviewed, 81.2% identified smoking as a risk factor, with the highest values found in areas of scientific study (91.1% Faculty of Medicine and Surgery; 86.2% Faculty of Mathematical, Physical and Natural Sciences). Knowledge of oral cancer was found to be lower in subjects with humanistic preparation (73.8% Faculty of Law; 73.7% Faculty of Letters and Philosophy). Although smoking was perceived by the population as a clear risk factor in the aetiopathogenesis of oral cancer, it should be emphasised that alcohol and sunlight were less known factors. Of those interviewed, 42.4% (for alcohol) and 21.1% (for sunlight) considered these factors as possible causes of oral cancer.
Among the High School students, those who attended a scientific high school had a greater knowledge of the risk factors than those who attended a Classical High School or Technical High School. More specifically, with regard to smoking, 83.2% of scientific high school students identified smoking as a clear risk factor compared with 76.9% of those who attended classical high school. There is a statistically significant difference of knowledge of the risk factor “smoke“ between the humanistic studies (Classical High School, Faculty of Letters) and scientific studies (Scientific High School, Faculty of Medicine and Surgery) (p = 0.0399).
Importantly, even among high school students, there is a lower perception of the importance of alcohol and sunlight as possible aetiologic factors. Thus, alcohol is recognised as a risk factor by 51.5% of Scientific High School students compared with 38.1% of the students attending Technical High School and 43.8% of the students attending Classical High School. There is a statistically significant difference of knowledge of the risk factor “alcohol” between Scientific and Technical High School (p = 0.0331).
Finally, sun exposure is known as a risk factor by 28.1% of students in Scientific High School compared with 18.5% of the students in Classical High School and 13.3% of the students in Technical High School. There is a statistically significant difference of knowledge of the risk factor “sunlight“ between the humanistic studies (Technical High School, Faculty of Letters) and scientific studies (Scientific High School, Faculty of Medicine and Surgery). (p = 0.0057) (Graphs 1,2,3).
Graphic 1.
Perception of smoking as a risk factor among the subjects who reported being aware of oral cancer.
(QUESTION 3 = Smoking may increase the risk of developing oral cancer?)
Graphic 2.
Perception of alcohol as a risk factor among the subjects who reported being aware of oral cancer.
(QUESTION 4 = Alcohol may increase the risk of developing oral cancer?)
Graphic 3.
Perception of sunlight as a risk factor among the subjects who reported being aware of oral cancer.
(QUESTION 5 = A long exposure to sunlight may contribute to the onset of oral cancer?)
Additionally, having a doctor in the family can improve the knowledge of the risk factors involved in oral cancer. In fact, 88.3% of the interviewed students who have a doctor in their family recognised smoking as a risk factor, 50.3% recognised alcohol and 24.3% identified exposure to sunlight as a risk factor.
Regarding the prevention of oral cancer, only 43.3% (487 of 1125 interviewed subjects) were aware of the possibility of preventive health screenings, whereas 80.7% (908 of total) recognised this as a useful event even in the absence of symptoms; however, only 2.8% (32 subjects of 1125) had received a specialist check, with 12.5% (4 subjects of 32) of these interviewed students having received a specialist check due to suggestions from their dentist. In our population, only 2% (23 subjects out of 1125) were asked by their own dentist to make a visit for the prevention of oral cancer.
Discussion and conclusions
In general, knowledge of oral cancer is poor among the interviewed people, and the majority of the population was not aware of the existence of oral cancer. Importantly, it should be noted that high school or university courses that specialise in scientific branches provide significantly better awareness of the disease and its risk factors to students enrolled in these courses. In addition, individuals with doctors in the family have a better perception of the disease than the rest of the sample.
Recently in Italy, knowledge of cancer prevention has spread widely, especially regarding lung or breast cancer, for which check-ups and preventive instrumental tests are regularly performed in the population. This culture of prevention is absent for oral cancer, as evident from the results of the study. Therefore, it is crucial to inform and educate the public regarding this serious disease: if this tumour is known and monitored with regular check-ups, it can be prevented or treated effectively.
The prevention of oral cancer has a major role in dental practice. Due to the identification of malignant disease and a proper health education, health care professionals can contribute to decreasing the prevalence of this serious disease.
The data obtained from this study highlight the need to increase health education, especially among younger people in high schools and university faculties, with humanistic or technical programs, in which the knowledge regarding prevention is more limited. A delay in the diagnosis and a long waiting period prior to a confirmed diagnosis favour the progression of the tumour to a more advanced stage, placing the life of the patient at serious risk.
Currently, early diagnosis for many neoplastic diseases is a prerequisite to achieve good therapeutic results, with a positive impact in terms of prolonged survival and improved quality of life.
References
- 1.Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics. CA Cancer J Clin. 2007;57(1):43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 3.Mashberg A, Samit AM. Early detection, diagnosis, and management of oral and oropharyngeal cancer. CA Cancer J Clin. 1989;39:67–88. doi: 10.3322/canjclin.39.2.67. [DOI] [PubMed] [Google Scholar]
- 4.Calabrese L, Bruschini R, Ansarin M, Giugliano G, De Cicco C, Ionna F, et al. Role of sentinel lymph node biopsy in oral cancer. Acta Otorhinolaryngol Ital. 2006 Dec;26(6):345–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Silverman S, Gorsky M. Epidemiologic and demographic update in oral cancer: California and national data, 1973–1985. J Am Dent Assoc. 1990;120:495–9. doi: 10.14219/jada.archive.1990.0082. [DOI] [PubMed] [Google Scholar]
- 6.http://www.registri-tumori.it
- 7.Bilancetti M. La responsabilità penale e civile del medico. CEDAM; Padova: 2000. [Google Scholar]
- 8.Messadi DV, Wilder-Smith P, Wolinsky L. Improving oral cancer survival: the role of dental providers. J Calif Dent Assoc. 2009 Nov;37(11):789–98. [PMC free article] [PubMed] [Google Scholar]
- 9.SNLG-ISS (Sistema Nazionale Linee Guida - Istituto Superiore di Sanità) Rapido accesso alla diagnosi per il paziente con sospetta patologia oncologica. http://www.snlg-iss.it/PNLG/LG/001onco/aintrod.htm. [Google Scholar]
- 10.Yellowitz JA, Horowitz AM, Drury TF, Goodman HS. Survey of US dentists’ knowledge and opinions about oral pharyngeal cancer. J Am Dent Assoc. 2000;131:653–661. doi: 10.14219/jada.archive.2000.0239. [DOI] [PubMed] [Google Scholar]
- 11.Sciubba JJ. Improving detection of precancerous and cancerous oral lesions. Computer-assisted analysis of the oral brush biopsy. US Collaborative OralCDx Study Group. J Am Dent Assoc. 1999;130:1445–1457. doi: 10.14219/jada.archive.1999.0055. [DOI] [PubMed] [Google Scholar]
- 12.www.nidcr.nih.gov/OralHealth/Topics/OralCancer/DetectingOralCancer.htm
- 13.www.nidcr.nih.gov/OralHealth/Topics/OralCancer/Oral-Cancer.htm
- 14.Nagler R, Ben-Izhak O, Savulescu D, Krayzler E, Akrish S, Leschiner S, et al. Oral cancer, cigarette smoke and mitochondrial 18kDa translocator protein (TSPO) - In vitro, in vivo, salivary analysis. Biochim Biophys Acta. 2010 1802 May;(5):454–61. doi: 10.1016/j.bbadis.2010.01.008. Epub 2010 Jan 18. [DOI] [PubMed] [Google Scholar]
- 15.Tsai KY, Su CC, Lin YY, Chung JA, Lian IeB. Quantification of betel quid chewing and cigarette smoking in oral cancer patients. Community Dent Oral Epidemiol. 2009;37:555–561. doi: 10.1111/j.1600-0528.2009.00504.x. [DOI] [PubMed] [Google Scholar]
- 16.Sasco AJ, Secretan MB, Straif K. Tobacco smoking and cancer: a brief review of recent epidemiological evidence. Lung Cancer. 2004;45(Suppl 2):S3–9. doi: 10.1016/j.lungcan.2004.07.998. [DOI] [PubMed] [Google Scholar]
- 17.Petti S, Scully C. Polyphenols, oral health and disease: A review. J Dent. 2009 Jun;37(6):413–23. doi: 10.1016/j.jdent.2009.02.003. Epub 2009 Mar 19. [DOI] [PubMed] [Google Scholar]
- 18.Ogden GR, Wight AJ. Aetiology of oral cancer: alcohol. Br J Oral Maxillofac Surg. 1998;36:247–51. doi: 10.1016/s0266-4356(98)90707-0. [DOI] [PubMed] [Google Scholar]
- 19.Wight AJ, Ogden GR. Possible mechanisms by which alcohol may influence the development of oral cancer. A review. Oral Oncol. 1998;34:441–7. doi: 10.1016/s1368-8375(98)00022-0. [DOI] [PubMed] [Google Scholar]
- 20.Petti S, Scully C. Oral cancer: The association between nation- based alcohol-drinking profiles and oral cancer mortality. Oral Oncol. 2005 Sep;41(8):828–34. doi: 10.1016/j.oraloncology.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Markopoulos A, Albanidou-Farmaki E, Kayavis I. Actinic cheilitis: clinical and pathologic characteristics in 65 cases. Oral Diseases. 2004;10:212–216. doi: 10.1111/j.1601-0825.2004.01004.x. [DOI] [PubMed] [Google Scholar]
- 22.Schwartz RA. Therapeutic perspectives in actinic and other keratoses. Int J Dermatol. 1996;35:533–538. doi: 10.1111/j.1365-4362.1996.tb03649.x. [DOI] [PubMed] [Google Scholar]
- 23.Barnaby JWJ, Styles AR, Cockerell CJ. Actinic keratoses: differential diagnosis and treatment. Drugs Aging. 1997;11:186–205. doi: 10.2165/00002512-199711030-00004. [DOI] [PubMed] [Google Scholar]