Summary
There is a debate in the literature about the need for Computed Tomagraphy (CT) before removing third molars, even if positive radiographic signs are present. In few cases, the third molar is so close to the inferior alveolar nerve that its extraction might expose patients to the risk of post-operative neuro-sensitive alterations of the skin and the mucosa of the homolateral lower lip and chin. Thus, the injury of the inferior alveolar nerve may represent a serious, though infrequent, neurologic complication in the surgery of the third molars rendering necessary a careful pre-operative evaluation of their anatomical relationship with the inferior alveolar nerve by means of radiographic imaging techniques. This contribution presents two case reports showing positive radiographic signs, which are the hallmarks of a possible close relationship between the inferior alveolar nerve and the third molars. We aim at better defining the relationship between third molars and the mandibular canal using Dental CT Scan, DICOM image acquisition and 3D reconstruction with a dedicated software. By our study we deduce that 3D images are not indispensable, but they can provide a very agreeable assistance in the most complicated cases.
Keywords: IAN Inferior Alveolar Nerve, 3M third molar, CBCT Cone-Beam Computed Tomography, Dental CT Scan, DICOM image, 3D reconstruction
Introduction
Extraction of lower third molars, both impacted and not, has become a standard procedure in the clinical dental practice. In most cases, this surgical treatment implies little or no risk for the adjacent anatomic structures that comprise first of all the inferior alveolar nerve (IAN), and the lingual nerve. However, in very few cases, the third molar is so close to the IAN that its extraction might expose patients to the risk, more or less relevant, of post-operative neuro sensitive alterations of the skin and the mucosa of the homolateral lower lip and chin.
Moreover, extraction of the third molar is the primary cause of the permanent neurologic deficit of the inferior alveolar nerve, being even more important than implant and orthognathic surgery (1,2). Other less frequent causes of IAN injury reported in literature are: loco-regional injection of anaesthetic for IAN block, endodontic treatment of lower premolar and molar after overfilling, malignant expansive lesions, metastases, mandibular fractures, local infections(osteomyelitis) and pre-prosthetic surgery (3,4). The incidence of temporary (reversible) injuries ranges from 3,3% to 13.0% and represents the third most common complication after alveolitis and post-operative infections; the incidence of permanent (irreversible) lesions of the IAN ranges from 0,2% to 9% (Tab.1) (5). Thus, the injury of the inferior alveolar nerve represents a serious but infrequent neurologic complication in the surgery of the third molars, which is usually due to the close anatomic relationship between IAN and third molars. Therefore, this anatomical relationship must be investigated pre-operatively by means of the radiographic imaging techniques currently available (1). In this study clinical cases are presented where the Orthopanoramic radiography shows positive radiographic signs, which are the hallmarks of a possible close relationship between the IAN and the third molars. This paper aims at better defining the relationship between third molars and the mandibular canal using Dental CT Scan, DICOM image acquisition and 3D reconstruction with a dedicated software Simplant (Materialise, Ann Arbor, MI 1997).
Table 1.
Incidence of IAN injury after extraction of the third molar (5).
| Temporary IAN Injury | Permanent IAN Injury | |
|---|---|---|
| Brann CR et al., 1999 | 13.0% | 1.0% |
| Carmichael FA, McGowan DA, 1992 | 3.9% | 9.0% |
| Gülicher D, Gerlach KL, 2000 | 3.6% | 9.0% |
| Kipp DP et al., 1980 | 4.5% | 1.0% |
| Smith AC et al., 1997 | 5.2% | 0.2% |
| Strietzel FP, Reichart PA, 2002 | 3.6% | 0.9% |
| Wofford DT, Miller RI, 1987 | 3.3% |
Cases reports
Case 1
A patient (female, age 35) was referred for the removal of both lower third molars. The panoramic radiography showed a darkening of the roots of the right third molar and a deviation of the canal of the left third molar. These are telltale signs of a close relationship with the mandibular canal. In order to confidently proceed to surgery, the patient underwent a Dental CT Scan to better evaluate the relationship between the canal and the roots of the third molar as this was not sufficiently clear on the first-level bi-dimensional examination (orthopanoramic radiography). After an accurate analysis of the CT, axial, paraxial and panoramic slices, given the close relationship between the roots and the IAN and the complex anatomic morphology of the examined third molars, we decided to proceed to the 3-D reconstruction of the surgical area by means of a dedicated software (Simplant).
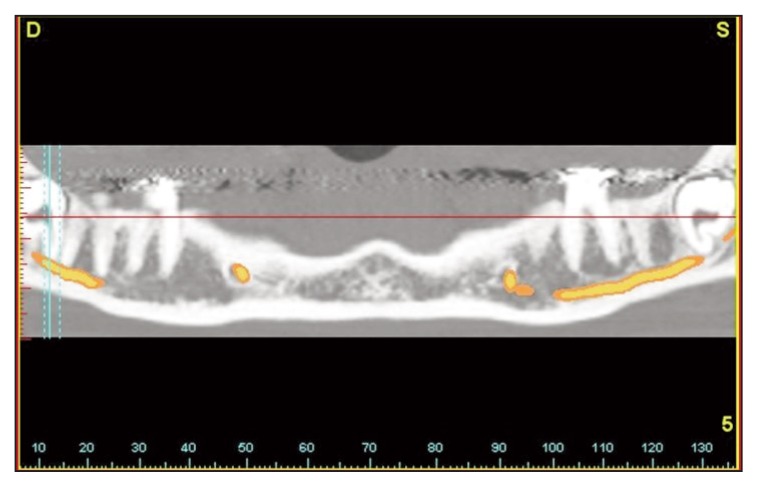
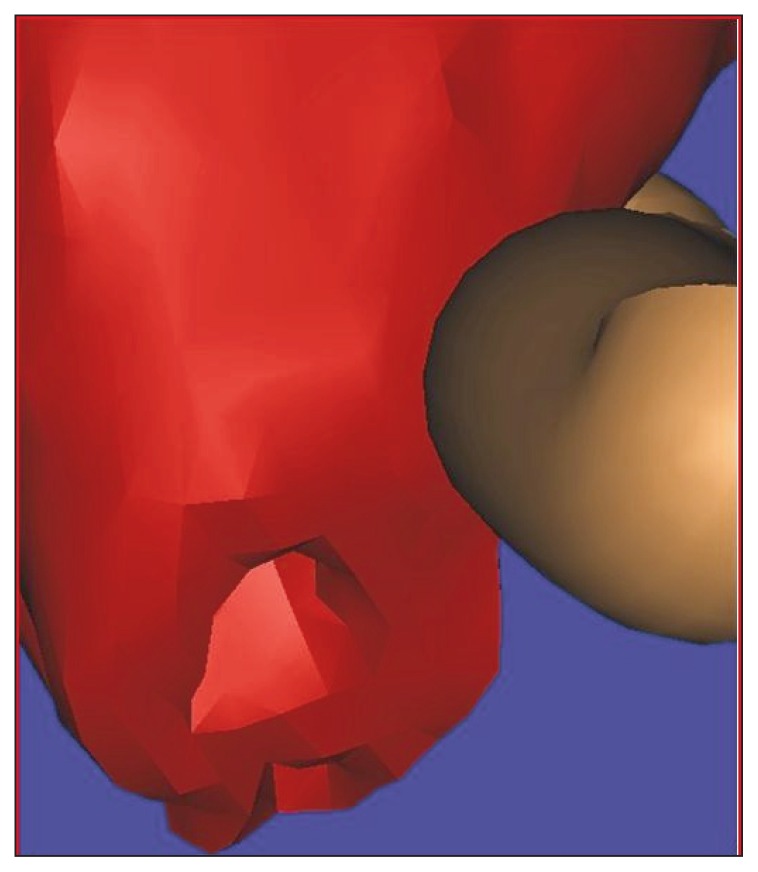
First step was to obtain the panoramic reconstruction carried out on the basis of the CT data (Fig. 1). On this image we traced the right and left mandibular canal by means of a dedicated tool (“nerve tool”) and the software automatically traced it also on the axial and paraxial sections. Then we have studied the right and left mandibular canal, highlighted by the software, on the paraxial sections (Figs. 3, 10). In both cases, we can appreciate IAN’s lingual position to the roots as well as the area of contact (interruption of the cortical wall of the canal) between the IAN and the mesiolingual and distolingual roots of the right third molar, and between the IAN and the mesial root of the left third molar. Moreover we can evaluate the mandibular canal on its axial view (Figs. 2, 9). Using the three scholding tools of the software we are able to obtain a 3D recostraction of the 3M teeth. We can decide to visualize only the tooth, the mandibular canal or all the anatomical structures (also in transparency modality). 3D reconstructions help the surgeon in analysing the relationship between the canal and the roots of the third molar from different perspectives (Figs. 4, 5, 6, 11, 12). For the right molar the buccal and mesiobuccal views providing information on both the morphology and crown-root angulation with respect to the canal pathway. Notice the apical hook-like shape of mesiolingual root, which was not clearly detectable on the CTs (Figs. 4, 5). The bottom view providing accurate information on the number and diameter of the tooth roots, 2 mesial and 2 distal roots- all separated, and on which root is in contact with the canal (Fig. 6). After the extraction we take some photos of the tooth: notice the correspondence between real anatomical details and 3D reconstruction (Figs. 7, 8).
Figure 1.
CT image of a panoramic reconstruction showing the impacted third molars and the right and left mandibular canal partially traced in Simplant (Case 1 - Right third molar).
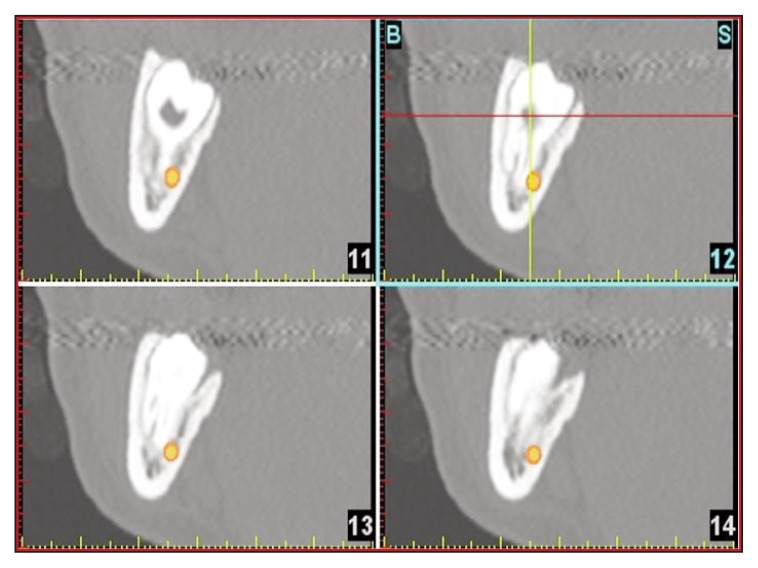
Figure 3.
Paraxial (coronal) views of the area of the right third molar highlighting the canal (Case 1 - Right third molar).
Figure 10.
CT image of paraxial (coronal) views of the area of the left third molar showing the mandibular canal, in Simplant, passing lingually to the roots and in close contact with the mesial root (Case 1 - Left third molar).
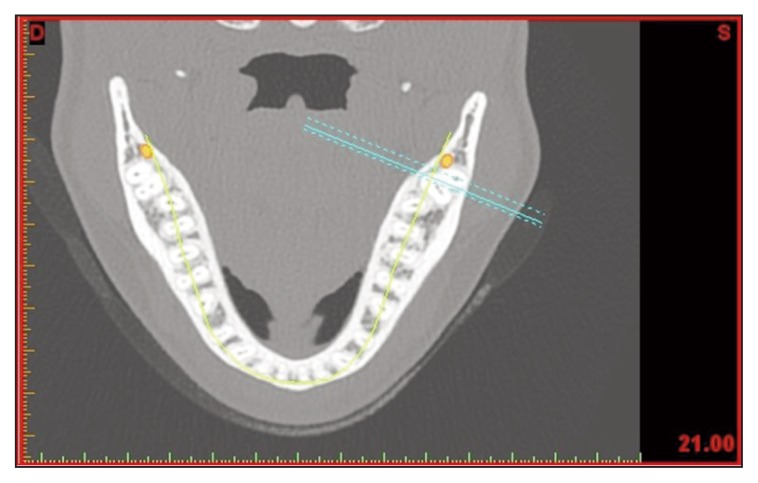
Figure 2.
Axial view passing through the tooth roots and showing the canal traced at the level of the left and right third molars (Case 1 - Right third molar).
Figure 9.
Axial view left molar (Case 1 - Left third molar).
Figure 4.
3D reconstruction buccal views showing the anteroposterior pathway of the IAN. The other teeth are not shown (Case 1 - Right third molar).
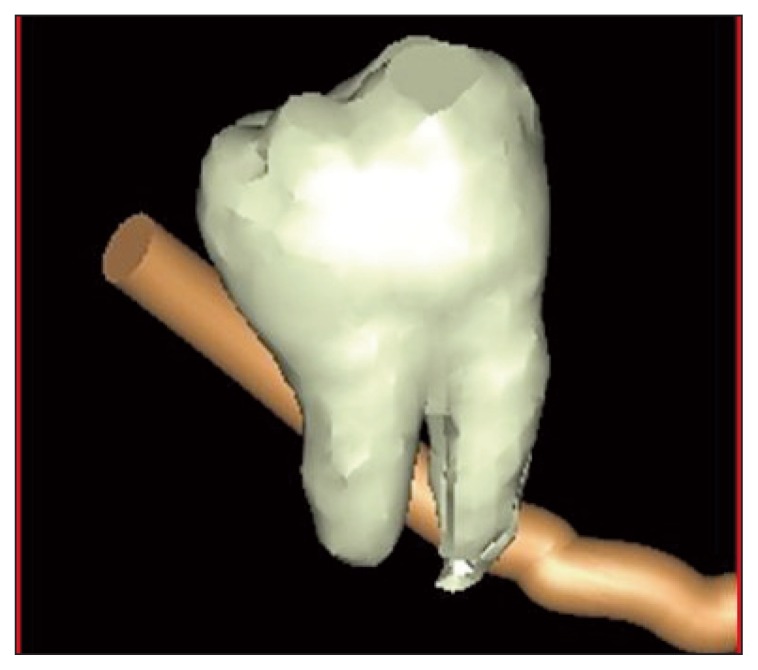
Figure 5.
3D reconstruction mesiobuccal views showing the anteroposterior pathway of the IAN. The other teeth are not shown (Case 1 - Right third molar).
Figure 6.
3D reconstruction bottom view showing the contact between the IAN and the mesiolingual and distolingual roots (Case 1 - Right third molar).
Figure 11.
3D reconstructions from different perspectives confirming what was already highlighted on the paraxial views, i.e. the IAN’s lingual position and its contact with the third upper portion of the mesial root (Case 1 - Left third molar).
Figure 12.
3D reconstructions from different perspectives confirming what was already highlighted on the paraxial views, i.e. the IAN’s lingual position and its contact with the third upper portion of the mesial root (Case 1 - Left third molar).
Figure 7.
Buccal View - extracted right molar (Case 1 - Right third molar).
Figure 8.
Bottom view - extracted right molar (Case 1 - Right third molar).
For the left molar, lingual and distal views indicate the presence of two separate roots, a distal and a mesial one respectively; the mesial root is in contact with the IAN while the distal root has no relationship with the canal (Figs. 11, 12).
Also for the left 3M molar a photo-analysis of the extracted tooth confirm the quality of 3D reconstruction (Fig. 13).
Figure 13.
The extracted Tooth (Case 1 - Left third molar).
Case 2
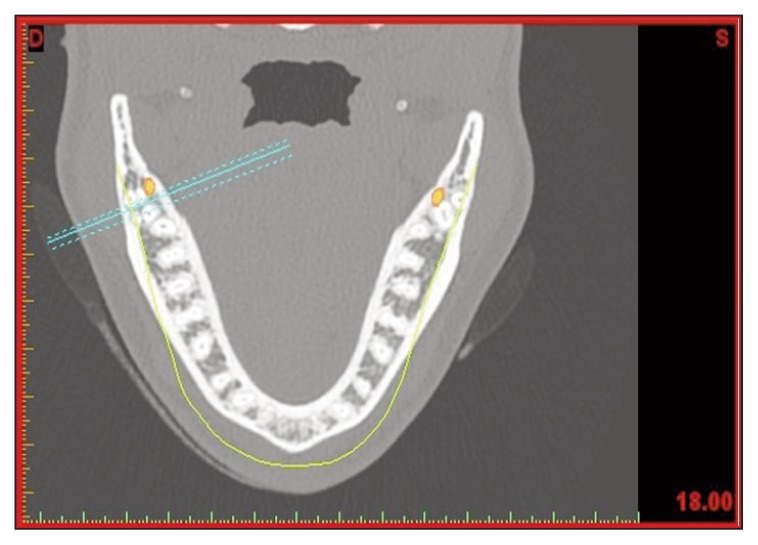
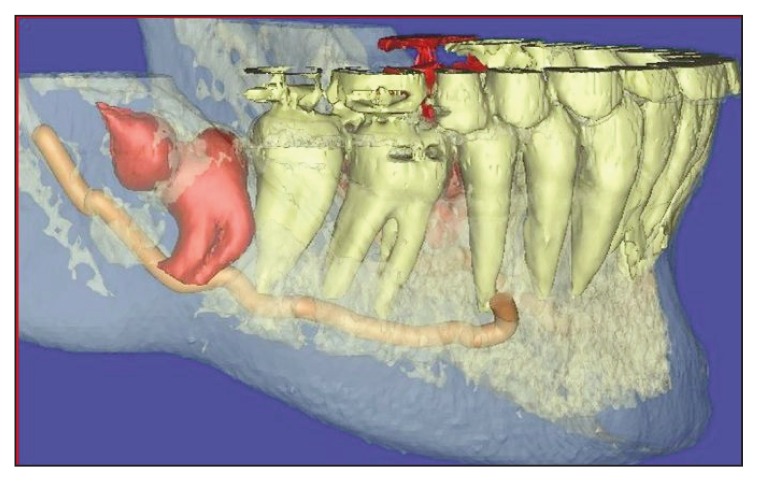
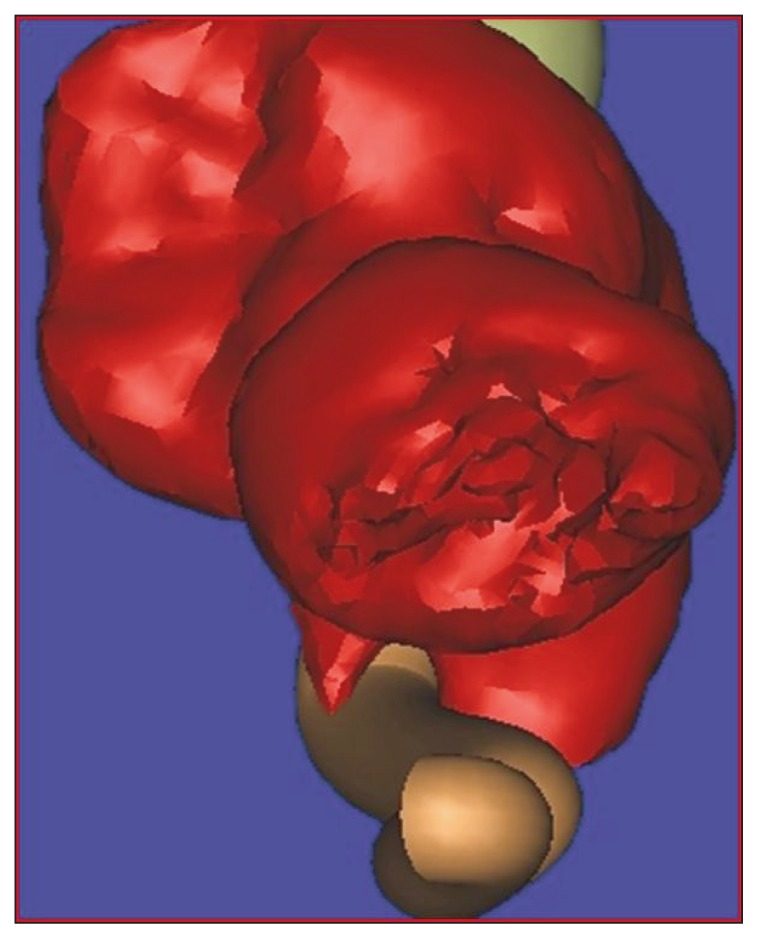
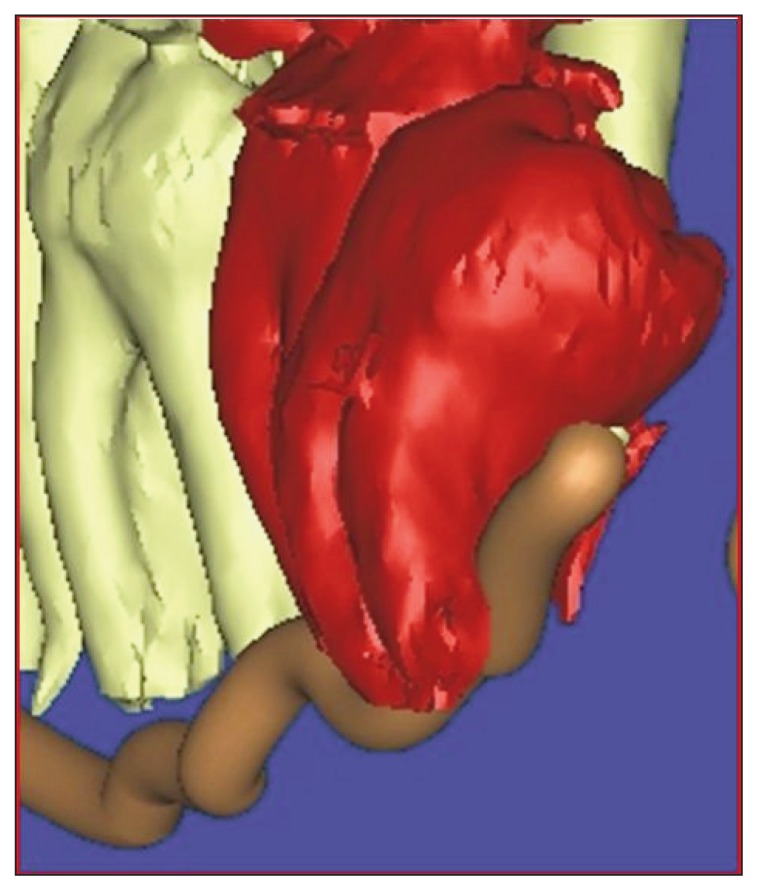
The patient (female, 30 years) had to remove both lower third molars and a supernumerary tooth in the right molar region. The first-level panoramic X-ray showed positive radiographic signs, including interruption of the cortical bone of the roof of the canal and darkening of the roots of the left lower third molar; darkening of the roots and deviation of the canal when passing nearby the left lower third molar. These signs indicated the presence of a close relationship between the IAN and the roots of the third molars. This was an indication to proceed to the second- level examination, i.e. Dental CT Scan and 3D analysis using the dedicated Simplant software. We started with a panoramic reconstruction (Fig. 14) tracing the mandibular canal that is also traced on the paraxial and sagittal sections (Figs. 15, 16, 19). Furthermore, in both cases the IAN is lingual to the roots and seems to be in contact with them. The 3-D reconstrucions confirmed the information provided by CT images, and in particular gave us the possibility to appreciate an array of anatomical details that were not easily detectable on the CTs: the presence of a mesio-lingual root, with a 90° curvature in the distal direction, lying on the canal roof (Figs. 17, 18); the IAN partially entrapped between the buccal and lingual roots (Fig. 18); the direct contact between the distal root and the IAN and the IAN’s close relationship with the mesial root (Fig. 20); the contact between the IAN and the disto-buccal root of the left third molar that showed a depression on the lingual surface due to the direct contact with the IAN (Fig. 21) and an intimate relationship (but no direct contact) with the mesio-buccal root. The software can zoom-in the relevant area highlighting anatomic details that help the surgeon both in assessing the risk of damaging the IAN and in planning the operation (Figs. 20, 21).
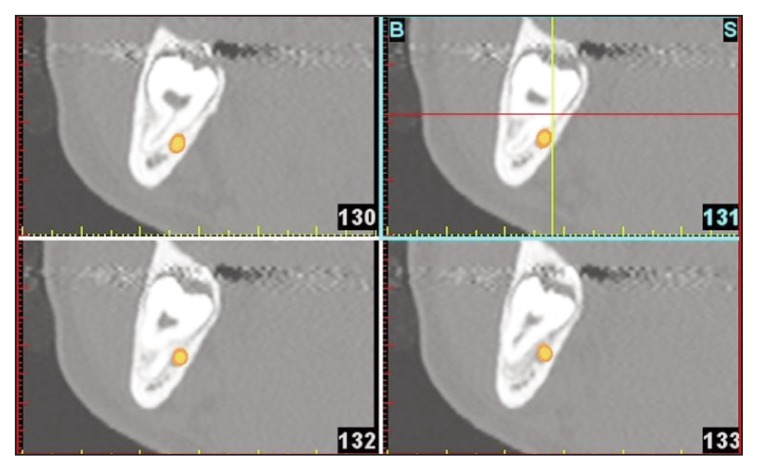
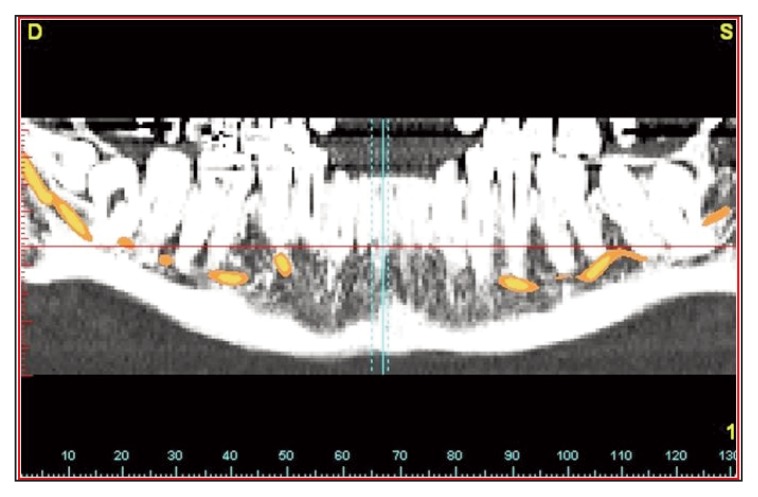
Figure 14.
CT image of panoramic reconstruction showing impacted third molars and the right and left mandibular canal traced in Simplant (Case 2 - Right third molar).
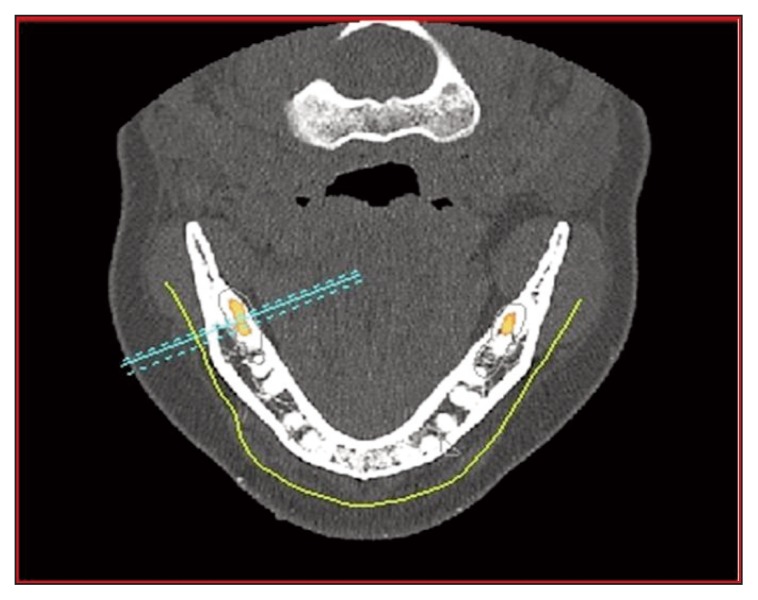
Figure 15.
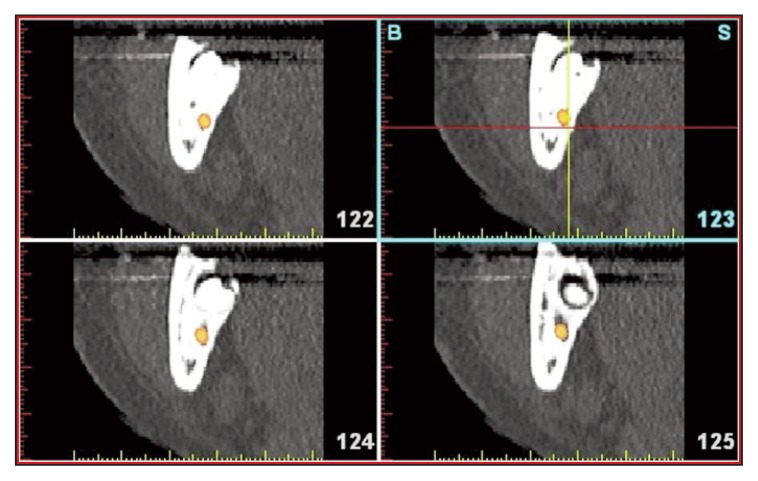
Axial slice showing the canal traced at the level of the third molars (Case 2 - Right third molar).
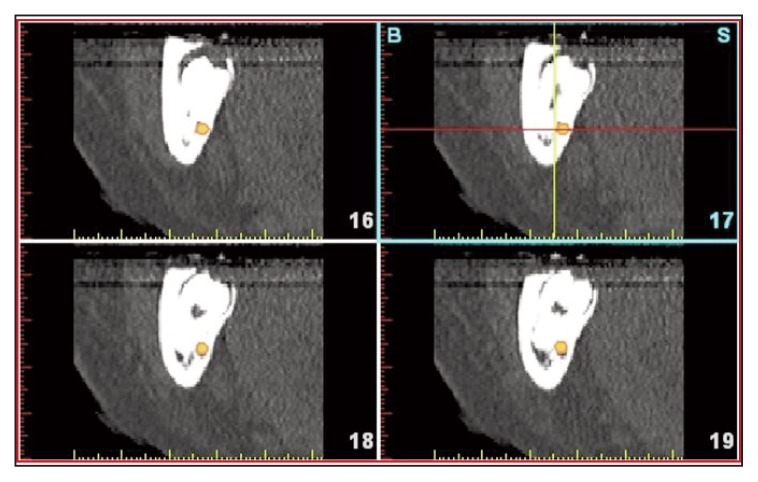
Figure 16.
Paraxial slices (coronal) of the region of the right third molar with highlighted canal (Case 2 - Right third molar).
Figure 19.
Images of paraxial (coronal) slices showing the mandibular canal, traced in Simplant, lingual to and in contact with the roots of the third molar (Case 2 - Left third molar).
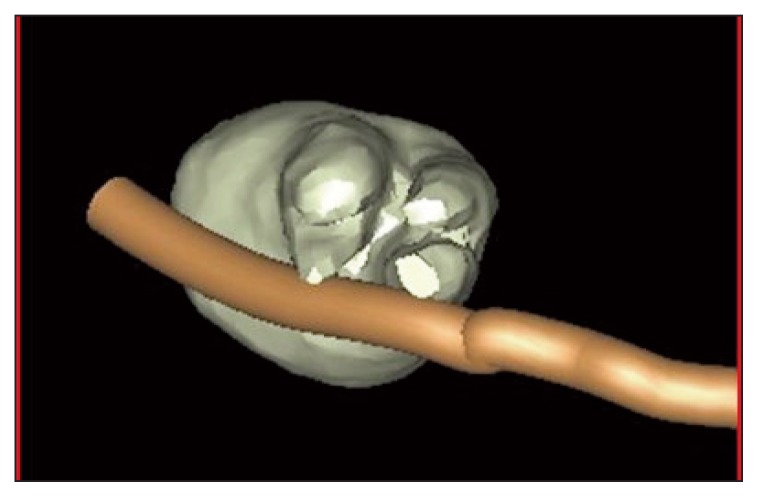
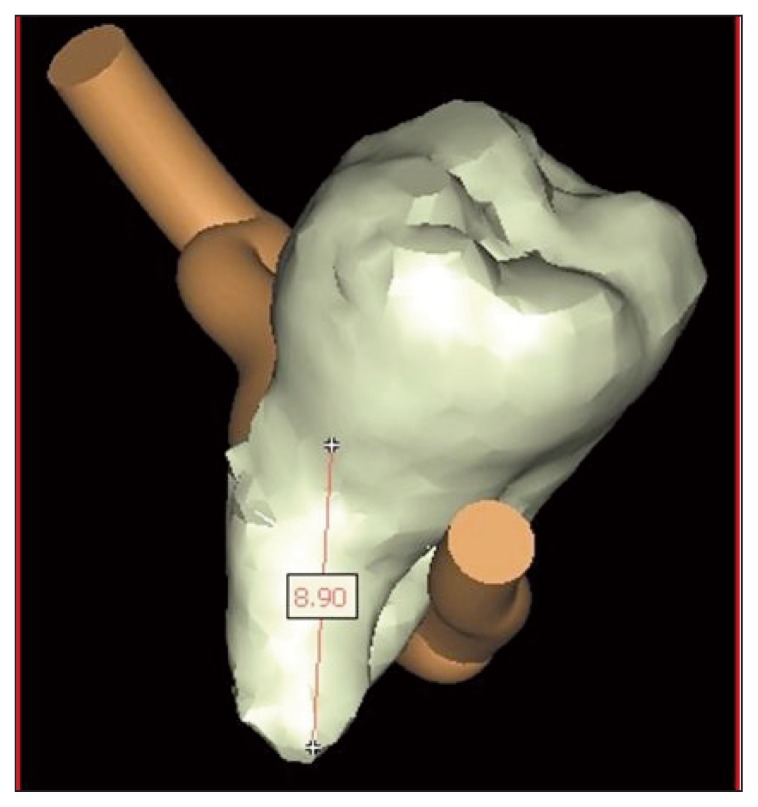
Figure 17.
3D reconstruction with the mandible in transparent mode: we can appreciate the tooth roots and the pathway of the mandibular canal (Case 2 - Right third molar).
Figure 18.
3D reconstruction with different views showing the relationship between the third molar and the IAN which is partially entrapped between the buccal and lingual roots (Case 2 - Right third molar).
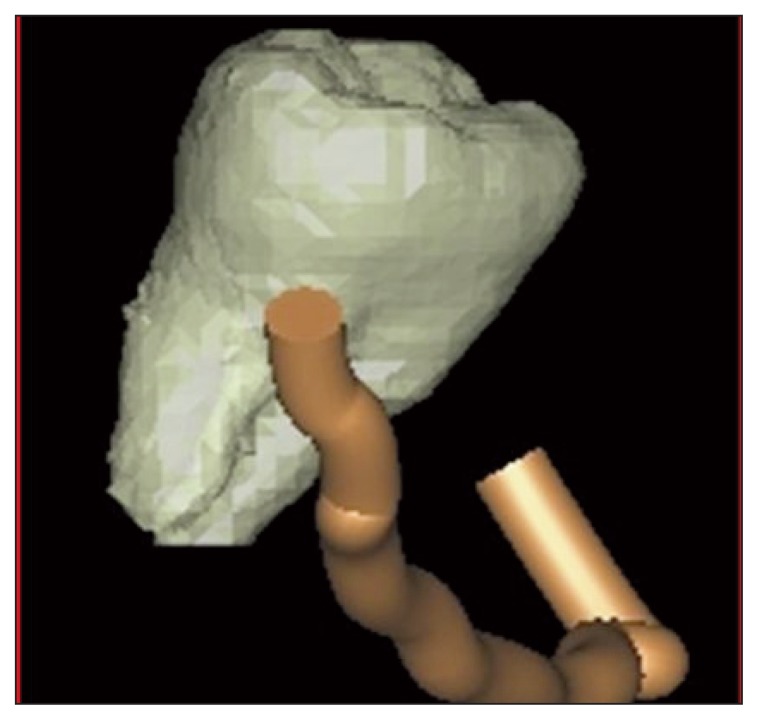
Figure 20.
3D reconstruction, disto-buccal view, showing both the buccal roots fused, with distal curvature extending apically beyond the IAN and partially enveloping it (Case 2 - Left third molar).
Figure 21.
3D reconstructions, distal views, respectively, confirming the contact between roots and mandibular canal that creates a depression on the lingual surface of the distal root (Case 2 - Left third molar).
Discussion
Despite its wide use in the dental clinical practice, periapical endoral radiography is not the ideal imaging technique to study impacted and non impacted third molars. In fact, it has many major limitations linked to superimposition, and thus to improper visualization of all anatomical structures, as well as to the operator’s difficulty in appropriately positioning the film without causing major discomfort to the patient (2). Currently in oral surgery, panoramic radiography is the first-level imaging of choice in the pre-operative evaluation of the third molar (6). Rood e Shehab (1990) described a series of radiographic signs, detectable on the OPT, that indicate the presence of a close relationship between the IAN and the lower third molar (Tab. 2) (7,8). There is no consensus in the literature about which of these 9 signs, detected on the panoramic radiography, is the most useful one in order to predict exposure of the IAN or clinical complications, such as paraesthesia, after the removal of a third molar (10). Some studies report that darkening of the roots, interruption of the cortex of the roof of the canal, and canal deviation are the radiographic signs, detected pre-operatively, that are most often associated with IAN’s exposure and injury (1,6,8,10). Sedaghatfar et al. found an association even between root narrowing and increased possibility of visualizing the IAN after removal of the third molars (10). Instead, Bell reported, a close relationship between the third molar and the inferior alveolar nerve in 51% of cases where the panoramic radiography showed a darkening of the roots, and only in 11% of cases where the OPT detected an interruption of the cortical bone of the roof of the canal (8). De Melo Albert et al. report that root darkening, detected on the OPT, coincides in 92% of cases with a direct relationship between the IAN and the roots of the third molar, detected on the CT (13). A review of literature indicates that most authors agree that root deviation, bifid apex and canal narrowing may have a lower predictive value in terms of IAN’s exposure and injury.
Table 2.
Radiographic signs, detectable on the OPT, that indicate the presence of a close relationship between the IAN and the lower third molar (7,9).
|
We can thus deduce that for pre-operative diagnostic purposes, the absence of positive radiographic signs on the panoramic radiography is preferable to their presence. Without positive radiographic signs the risk of IAN injury is considered very low, while the presence of one or more signs is not a good predictor of IAN injury, although it indicates a high probability of intra-operative exposure of the vascular nervous bundle. This probability, in turn, increases with an increase in the number of positive radiographic signs detected on the OPT (9,10,15). In a study by Susarla and Dodson, the authors conclude that the specificity of orthopanoramic radiography to predict IAN injury ranges between 96% and 98% (ability to exclude a direct IAN/M3 relationship); while its sensitivity ranges between 24% and 38% (6,16) (ability to identify a direct IAN/M3 relationship). This means that, in the absence of positive radiographic signs, the OPT enables us to detect with almost 100% accuracy- the cases of third molars that are not in direct relationship with the IAN (high negative predictive value), whose extraction is thus not associated with the risk of damaging the IAN. However, given its low sensitivity, in the presence of positive radiographic signs, OPT does not allow to detect- with equal accuracy- the cases where third molars are in direct relationship with the IAN (low positive predictive value), and whose extraction entails the risk of injuring the IAN (6,17). In fact, it has been shown that relying only on the positive radiographic signs to make a pre-operatory diagnosis, can lead to an overestimate of the actual possibility of contact between the IAN and third molars, thus erroneously classifying a situation as a high risk one (false positive) (18). Therefore, the presence of positive radiographic signs on the OPT should be regarded just an indication to proceed to second-level instrumental investigations with CT Dental Scan or Cone-Beam Computed Tomography (CBCT). These methods will provide a better way to evaluate the relationship between the third molar’s roots and the IAN (2,9,10,16). As OPT is a bi-dimensional examination, it does not provide information on the depth of the anatomical structures studied. Indeed, it locates the mandibular canal only in the vertical and not in the horizontal plane (2,6). Furthermore, the evaluation of the position of the mandibular canal in the vertical plane is not always reliable due to magnification variables- 20–30% difference. Moreover, there may be other confounding sources of variation, e.g. the position of patient’s head on the pantograph, and also the area of interest given that the amplification might not be homogeneous across the whole image (5,19). Other challenges with OPT are the superimposition of air shadows and soft tissues as well as phantom images (20). Furthermore, the OPT does not detect either the buccolingual width or the atrophy of the alveolar crest (20). A positive feature of bi-dimensional images, in standard radiological techniques, is the high resolution and contrast of anatomical details which is not provided by CT images (8). It is important to notice that the anatomical structures that are out of the centre of rotation of the source/detector are blurred and distorted. Impacted or ectopic third molars are frequently out of the centre of rotation and thus cannot be properly visualized. Hence it is often difficult to make a diagnosis based only on OPT. Neugebauer et al. (5) compared the diagnostic accuracy of OPT vs CBCT in detecting the position of the root apex of third molars with respect to the IAN. There were no significant differences in diagnostic information between the two radiographic techniques with respect to the vertical plane. In fact, both provide the clinician with the same type of information. Conversely, there was a significant difference between the two techniques with respect to the horizontal plane, and the diagnostic information provided by CBCT was clearly preferable (5). The latter is a 3-D exam, which enables us to:
- evaluate the buccolingual relationship between the IAN and the roots of the third molar, so as to avoid impacting the tooth with movements that can cause a impingement of the nerve’s root; plan the appropriate interradicular section if it is evident that the IAN crosses the roots (21);
- identify the presence or the partial/total absence of cortical bone around the IAN (21);
- visualize the number of roots and the exact root anatomy of the third molar; define the inclination of the tooth and the position of the crown with respect to the buccal or lingual surface of the mandible (21).
To conclude, most authors in the literature agree that Dental CT Scan and CBCT are the most effective imaging techniques to detect both the localization of the canal in relation to its superior/inferior and bucco/lingual dimensions, and the exact crown-root morphology of third molars (5). In the last decade, 3-D reconstruction softwares- designed for the study of the jaws have been introduced to help clinicians both in the diagnosis and in the treatment plan.
These softwares, initially introduced in implantology, represent an excellent tool for the study of the relationship between mandibular canal and third molars. They are useful especially in challenging diagnostic cases, where the 3-D visualization of the IAN/M3 relationship enables clinicians both to decide the appropriate planning of the surgical step, and to avoid jeopardising the integrity of the mandibular canal (9). One of the first softwares to be marketed is SimPlant (Materialise, Ann Arbor, MI 1997). This software accepts images in DICOM format (Digital Imaging and Communications in Medicine), i.e. the first standard format for the distribution and viewing of any type of medical image. Simplant is able to recognize DICOM images from many different types of CTs and CBCTs.
So to pass from a Digital CT or CBCT to a 3D reconstruction we have to import DICOM files in Simplant. A 3d reconstruction doesn’t need an higher dose of radiation to patient; it allows to optimize the information contained in CT or CBCT files.
Once imported in SimPlant, the images show maxillary sections on the axial, paraxial (coronal) and sagittal planes (panoramic reconstructions). These images are realistic representations of the maxilla (1:1 scale), allowing accurate measurements of anatomical structures. Importantly, SimPlant enables surgeons to trace the path of the mandibular canal. It can be traced either on the paraxial sections (coronal) or on the sagittal sections (panorex); usually it is easier to use than the panoramic images as the IAN can be more easily identified and the software automatically detects it also on the paraxial views. The buccolingual position of the IAN (in the horizontal plane) is detected on the paraxial views, while the position in the vertical plane can be assessed both in the panoramic and on the paraxial images. The great advantage of SimPlant, and similar softwares, is the possibility to have virtual 3-D reconstructions of the bones, of the teeth, of the mandibular canal as well as of other structure of the face.
The most interesting feature of the software is its capability to rotate images, thus providing clinicians with a 360° view of the anatomic structures. Moreover it can hide or highlight the single components (bone, teeth, canal, implants, etc.) in different combinations (9).
Conclusions
There is currently debate in literature about the need for CTs before removing third molars, even if one or more positive radiographic signs, as mentioned before, are present on the panoramic radiography. Indeed, there are oral and maxillofacial surgeons who disagree about the need to resort to CTs, as they consider the panoramic radiography as the first choice examination for the pre-operative evaluation of impacted and non impacted third molars. These surgeons infact underline both the high cost of CT and the high dose of radiation patients are exposed to. So, unlike OPT, CTs are not seen by these surgeons as a routine examination for the evaluation of third molars. However, CT evaluation should not be excluded a priori as a potential diagnostic tool for clinicians (9). Indeed, it should be used only for those patients whose first-level OPT shows one or more of the nine radiographic signs indicating a close relationship between the IAN and the tooth root, and when this relationship cannot be defined sufficiently using conventional radiology (2,9,10,16). In particular, Jhamb et al. (18) deem that a CT examination is absolutely necessary when the OPT detects one or more of the following radiographic signs: darkening of the roots; interruption of the white line with narrowing of the canal and superimposition of the roots and the mandibular canal. Moreover, CT examination is recommendable in all those instances in which it may have a direct impact on the planning of the surgical steps, and on the evaluation of sequelae, outcome and morbidity.
It should also be stressed that the advent of CBCT in the early 2000s has reduced the cost for patients, and mostly it has improved the risk-benefit profile by reducing the dose of radiations for patients if compared to conventional CT scans (10). Moreover, in those cases where the root of the third molars shows a complex morphology, and it is located in contact with the mandibular canal, the new 3D reconstruction softwares supporting CTs provide surgeons with an additional planning tool that offers:
immediate and neat visualization of the noble structures that have to be respected and their localization in the three spatial planes;
the exact morphology of the relevant root apex;
a 360° view of the relationship between the IAN and the third molar;
the exact point in which the root is in relationship with the canal.
The complete anatomical image’s details and the friendly and dynamic approach to them can influence the surgical approach: single or multiple odontotomy, depth of osteotomy or direct of luxation can be programmed more accurately.
To conclude, we can state that although 3D images are not essential for the pre-operative evaluation of third molars, they definitely enhance the information provided by CT scans, and thus represent an added value in the choice of the therapy to adopt in order to minimize possible injuries of the IAN.
References
- 1.Dodson TB. Role of computerized tomography in management of impacted mandibular third molars. N Y State Dent J. 2005 Nov; [PubMed] [Google Scholar]
- 2.Flygare L, Ohman A. Preoperative imaging procedures for lower wisdom teeth removal. Review. Clin Oral Invest. 2008;12:291–302. doi: 10.1007/s00784-008-0200-1. [DOI] [PubMed] [Google Scholar]
- 3.Jerjes W, Upile T, Shah P, Nhembe F, et al. Risk factors associated with injury to the inferior alveolar and lingual nerves following third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:335–345. doi: 10.1016/j.tripleo.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Tolstunov L, Pogrel MA. Delayed paresthesia of inferior alveolar nerve after extraction of mandibular third molar: case report and possible etiology. J Oral Maxillofac Surg. 2009;67:1764–1766. doi: 10.1016/j.joms.2009.03.057. [DOI] [PubMed] [Google Scholar]
- 5.Neugebauer J, Shirani R, Mischkowski RA, Ritter L, Scheer M, Keeve E, Zoller JE. Comparison of cone beam volumetric imaging and combined plain radiographs for localization of the mandibular canal before removal of impacted lower third molars. Oral Surg Oral Med Oral Pathol Oral Radiol End. 2008;105:633–42. doi: 10.1016/j.tripleo.2007.08.041. [DOI] [PubMed] [Google Scholar]
- 6.Atieh MA. Diagnostic accuracy of panoramic radiography in determining relationship between inferior alveolar nerve and mandibular third molar. J Oral Maxillofac Surg. 2010;68:74–82. doi: 10.1016/j.joms.2009.04.074. [DOI] [PubMed] [Google Scholar]
- 7.Koong B, Pharoah MJ, Bulsara M, Tennant M. Methods of determining the relationship of the mandibular canal and third molars: a survey of Australian oral maxillofacial surgeons. Aust Dent J. 2006;51:64–68. doi: 10.1111/j.1834-7819.2006.tb00403.x. [DOI] [PubMed] [Google Scholar]
- 8.Bell GW. Use of dental panoramic tomographs to predict the relation between mandibular third molar teeth and the inferior alveolar nerve. Radiological and surgical findings, and clinical outcome. Brit J Oral Maxillofac Surg. 2004;42:21–27. doi: 10.1016/s0266-4356(03)00186-4. [DOI] [PubMed] [Google Scholar]
- 9.Friedland B, Donoff B, Dodson TB. The use of 3-dimensional reconstruction to evaluate the anatomic relationship of the mandibular canal and impacted mandibular third molars. J Oral Maxillofac Surg. 2008;66:1678–1685. doi: 10.1016/j.joms.2007.08.032. [DOI] [PubMed] [Google Scholar]
- 10.Sedaghatfar M, August MA, Dodson TB. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg. 2005;63:3–7. doi: 10.1016/j.joms.2004.05.217. [DOI] [PubMed] [Google Scholar]
- 11.Hillerup S. Iatrogenic injury to the inferior alveolar nerve: etiology, signs and symptoms, and observations on recovery. J Oral Maxillofac Surg. 2008;37:704–709. doi: 10.1016/j.ijom.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Savi A, Manfredi M, Pizzi S, Vescovi P, Ferrari S. Inferior alveolar nerve injury related to surgery for an erupted third molar. Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e7–e9. doi: 10.1016/j.tripleo.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 13.Guimaraes D, de Melo ADG, Gomes ACA, do Egito Vasconcelos BC, de Oliveira e Silva ED, Holanda GZ. Comparison of ortho-pantomographs and conventional tomography images for assessing the relationship between impacted lower third molars and the mandibular canal. J Oral Maxillofac Surg. 2006;64:1030–1037. doi: 10.1016/j.joms.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 14.Tantanapornkul W, Okouchi K, Fujiwara Y, Yamashiro M, Maruoka Y, Ohbayashi N, Kurabayashi T. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Edod. 2007;103:253–9. doi: 10.1016/j.tripleo.2006.06.060. [DOI] [PubMed] [Google Scholar]
- 15.Jozsef S, Lempel E, Jeges S, Szabò G, Olasz L. The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:294–302. doi: 10.1016/j.tripleo.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 16.Susarla SM, Dodson TB. Preoperative computed tomography imaging in the management of impacted mandibular third molars. J Oral Maxillofac Surg. 2007;65:83–88. doi: 10.1016/j.joms.2005.10.052. [DOI] [PubMed] [Google Scholar]
- 17.Susarla SM, Sidhu HK, Avery LL, Dodson TB. Does computed tomographic assessment of inferior alveolar canal cortical integrity predict nerve exposure during third molar surgery? J Oral Maxillofac Surg. 2010;68:1296–1303. doi: 10.1016/j.joms.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 18.Jhamb A, Dolas R, Pandiwar PK, Mohanty S. Comparative efficacy of spiral computed tomography and orthopantomography in preoperative detection of relation of inferior alveolar neurovascolar bundle to the impacted mandibular third molar. J Oral Maxillofac Surg. 2009;67:58–66. doi: 10.1016/j.joms.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 19.Angelopoulos C, Thomas S, Hechler S, Parissis N, Hlavacek M. Comparison Between Digital Panoramic Radiography and Cone-Beam Computed Tomography for the Identification of the Mandibular Canal as Part of Presurgical Dental Implant Assessment. J Oral Maxillofac Surg. 2008;66:2130–2135. doi: 10.1016/j.joms.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 20.Liu T, Xia B, Gu Z. Inferior alveolar canal course: a radiographic study. Clin Oral Implants Res. 2009;20:1212–1218. doi: 10.1111/j.1600-0501.2009.01736.x. [DOI] [PubMed] [Google Scholar]
- 21.Pippi R. A case of inferior alveolar entrapment in the roots of a partially erupted mandibular third molar. J Oral Maxillofac Surg. 2010;68:1170–1173. doi: 10.1016/j.joms.2009.10.007. [DOI] [PubMed] [Google Scholar]