Abstract
Purpose
To evaluate the available evidence for the clinical effectiveness of the EOS® 2D/3D X-ray imaging system for the evaluation and monitoring of scoliosis and other relevant orthopaedic conditions.
Methods
A systematic review of studies of EOS®, compared with standard X-ray film, computed radiography or digital radiography, of patients with orthopaedic conditions was undertaken. Ten electronic databases were searched. The quality of the included studies was assessed and a narrative synthesis undertaken.
Results
Three small, limited quality studies, primarily of children with scoliosis, were identified. No patient health outcomes were reported. Spinal image quality was comparable or better overall with EOS®. Radiation dose was considerably lower with EOS® than X-ray film or computed radiography; the mean entrance surface dose was over five times lower with EOS® for the posteroanterior spine radiograph and over six times lower for the lateral spine radiograph.
Conclusions
The available clinical evidence for EOS® is limited to establishing its basic technical ability. The technical advancements associated with EOS® (the ability to generate a full body scan and to construct a three-dimensional model from synchronously acquired lateral and posteroanterior images) have not been evaluated in terms of their ability to improve patient outcomes. Whilst radiation dose is a concern for orthopaedic patients who require repeated imaging, it is difficult to quantify the reductions in radiation dose seen with EOS® in terms of patient health benefits. Clinical studies that investigate the impact of EOS® on patient management are required.
Keywords: Systematic review, EOS®, Scoliosis, X-ray
Introduction
EOS® is a biplane X-ray imaging system manufactured by EOS imaging (formerly Biospace Med, Paris). It uses slot-scanning technology, based on the Nobel prize-winning work of physicist Georges Charpak on multiwire proportional chambers [1], to produce a high-quality image with less radiation than standard imaging techniques [2]. EOS® has been developed for orthopaedic imaging, with the benefit that it can take posteroanterior (PA) and lateral images simultaneously, allowing the reconstruction of a three-dimensional model, a facility that should greatly enhance the imaging of the spine. EOS® allows the acquisition of images whilst the patient is in an upright, weight-bearing (standing, seated or squatting) position, and can image the full length of the body (up to 175 cm), removing the need for digital stitching/manual joining of multiple images. The system takes approximately 20 s for an adult full body scan and 4–6 s to scan the spine, depending on the patient’s height. The quality and nature of the image is similar to computed radiography (CR) and digital radiography (DR), rather than computed tomography (CT). The generation of a three-dimensional model allows analysis of individual vertebral rotation and the rotation of a scoliotic curve to a level of accuracy which was not previously possible.
The indications for which there may be a potential benefit associated with EOS® are in those pathologies which change under load, where rotational deformity is relevant or where radiation exposure is a concern due to the need for repeated X-ray imaging. The principal indication is scoliosis, a three-dimensional deformity of the spine, characterised by a lateral curve (coronal plane deformity) of ten degrees or more [3]. Other relevant indications include sagittal plane deformities such as kyphosis and deformities of the lower limbs.
The evaluation and monitoring of scoliosis has been based on two-dimensional imaging, with the Cobb angle being the prime radiographic parameter of interest. Much of what is known regarding the natural history of this condition is based on the Cobb angle. Over time, it has been recognised that this over-simplifies the deformity [4, 5]. The character and magnitude of the scoliotic curve change according to the plane of radiographic projection; therefore, the deformity cannot be adequately quantified in one plane only [6]. Computed radiography and digital radiography only give a limited indication of axial rotation.
Unless a spine curve is entirely fused, some correction (in all three planes) will occur when the patient lies down. Supine X-rays are only useful when assessing curve flexibility prior to intervention. However, the currently available imaging technologies that can be used in a weight-bearing position, X-ray film, CR and DR, cannot take orthogonal PA and lateral images simultaneously, reducing the potential for three-dimensional reconstruction techniques. In addition, when a full body image is required, these standard imaging technologies require adjustment for distortion or digital stitching/manual joining of multiple images. Imaging in the standing position (or seated position for non-ambulators) enables a clearer understanding of the patient’s global spinal balance [7]. Sagittal spinal balance is inextricably linked to the geometry of the pelvis (and thence to the lower limbs). Unless specifically requested, the pelvis is not imaged on the standard lumbar film, and consequently the spino-pelvic balance may be neglected.
Computed tomography (CT) scanning has been used to quantify vertebral rotation. This may be useful when done in the standing position, but the vertebral rotational information from a supine image may not reflect the situation when the patient is standing. The radiation dose associated with CT has fallen over time, but remains significant [5]. Supine CT is more frequently used for assessing the rotational profile of the lower limbs. CT still has an important role in characterising local anatomy prior to intervention.
Patients with adolescent idiopathic scoliosis undergo repeated X-ray imaging for diagnosis, monitoring, surgical planning and post-operative follow-up. This repeated X-ray exposure is a cause for concern, owing to the harmful effects linked to ionising radiation, particularly in children and adolescents [8]. Children are more sensitive to the harmful effects of radiation than adults and are more likely to manifest radiation-induced changes over their lifetime [9]. Strategies to reduce the number and effective tissue dose of these repeated radiographic examinations include the use of PA rather than AP films (to reduce breast dose) and alternatives to X-ray such as raster stereography (topographic mapping of the posterior body wall).
Whilst the potential benefits of EOS® are promising and attractive, it is unclear how well they are supported by evidence. The objective of this systematic review was to investigate the amount, nature and quality of the evidence on the clinical effectiveness of the EOS® 2D/3D X-ray imaging system, compared with the technologies used in standard practice; X-ray film, CR or DR, for the evaluation and monitoring of scoliosis and other relevant orthopaedic conditions. In diagnostic research, clinical effectiveness indicates that the diagnostic technology provides some real value in terms of influencing the clinician’s diagnostic thinking and therapeutic management, and ultimately improves patient outcomes [10]. Thus, the outcomes of interest in this review are patients’ health outcomes, radiation dose and quality of the image.
Materials and methods
The systematic review was conducted following the general principles recommended in the Centre for Reviews and Dissemination’s (CRD) guidance [11] and the PRISMA statement [12]. Ten electronic databases (MEDLINE, EMBASE, the Cochrane Library, AMED, CINAHL, Biosis Previews, HMIC, INSPEC, ISI Science Citation Index and Pascal), two clinical trial registries (ClinicalTrials.gov and Current Controlled Trials) and the manufacturer’s Web site were searched in November 2010 for potentially relevant studies. Searches were limited by date (1993 onwards) since the prototype of the EOS® system was purchased by Biospace Med in 1994. No language, study design or other limits were applied. Details of the search strategies are published in an HTA monograph [13]. Reference lists of all included studies and relevant editorials were hand searched to identify further relevant studies. EOS imaging were contacted for information regarding any unpublished or ongoing studies.
Two reviewers independently screened all titles and abstracts. Full paper manuscripts of any records that appeared to be about EOS® were obtained and the relevance of each study assessed by two reviewers according to the inclusion and exclusion criteria described below. Any discrepancies were resolved by consensus.
Studies comparing EOS® with X-ray film, CR or DR in patients with any orthopaedic condition were eligible for inclusion. Studies reporting any outcome were eligible for inclusion. The primary outcome of interest was patient health outcomes; secondary outcomes of interest were the surrogate outcomes radiation dose and quality of the image. Studies comparing EOS® with CT were not eligible for inclusion. Studies using healthy volunteers, vertebrae from cadavers or the European Spine Phantom were not eligible for inclusion.
Data from the included studies were extracted by one reviewer using a standardised data extraction form and checked for accuracy by a second reviewer. Disagreements were resolved through consensus. Where data were missing, the authors of the study were contacted.
The quality of the included studies was assessed using the QUADAS quality assessment tool for diagnostic studies [14]. Whilst the included studies were not typical diagnostic cohort studies, they compared two ‘tests’ in a single group of patients, one being standard practice. Therefore, the majority of items on the QUADAS tool were applicable to the studies being assessed. An additional six quality items specific to the review were also assessed, relating to the appropriateness of the methods used for measuring radiation dose and image quality and whether the execution of the technologies matched clinical practice. The quality assessment was performed by one reviewer and checked by a second reviewer. Disagreements were resolved through consensus. A consultant paediatric radiologist assisted in completing the six technical quality questions.
Results
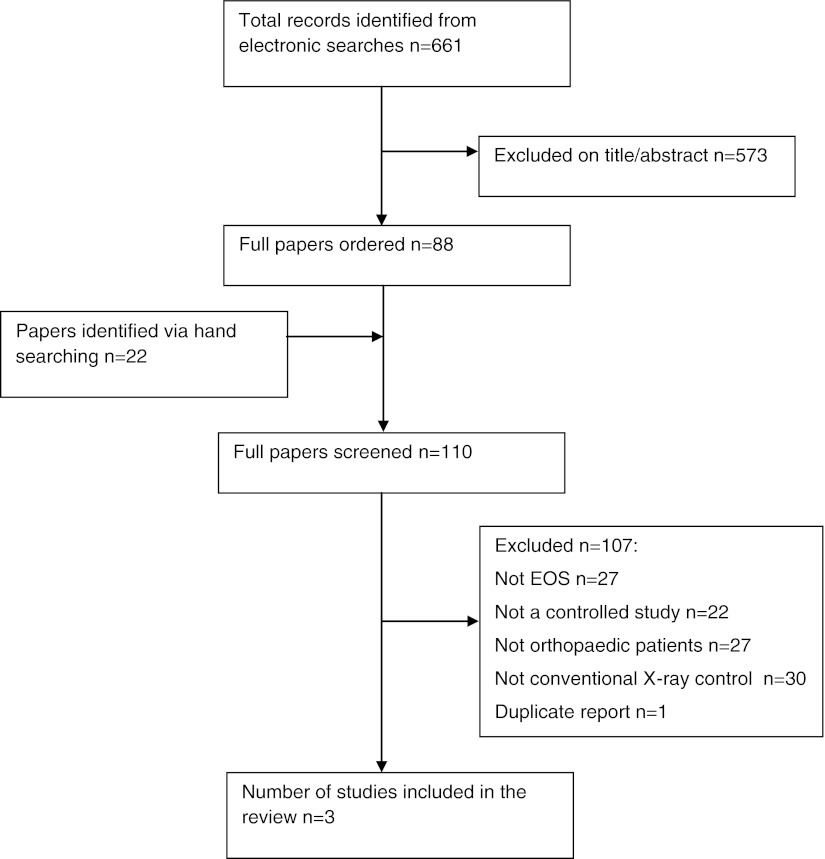
A flowchart of the study selection process is presented in Fig. 1. A full list of publications that did not meet all of the inclusion criteria, along with the reason for their exclusion, is available from the authors on request.
Fig. 1.
Flow diagram of the study selection process
Three studies met the inclusion criteria for the review, comprising a total of 290 patients. The main characteristics of the included studies are presented in Table 1. All three studies included patients with scoliosis, although one study also included patients being followed up for known hip diseases [15]. One set of images was taken using each imaging device. For patients with scoliosis, PA and lateral images of the spine were taken, whilst patients being followed up for known hip diseases underwent imaging of the pelvis. Two studies compared EOS® with film X-ray imaging [15, 16] and one compared EOS® with CR [17].
Table 1.
Summary of study characteristics and results
| Kalifa [15] | Le Bras [16] | Deschênes [17] | |
|---|---|---|---|
| Duration of patient recruitment | December 1994 to January 1996 | Not reported | Not reported |
| Patients recruited | 176 | 64 | 50 |
| Patients analysed | 140 | Not reported | 49 |
| Patient characteristics | Children (>5 years) undergoing follow-up for scoliosis (93) or known hip diseases (47) | Adolescents who required full spine radiographs for scoliosis detection or follow-up | Children undergoing follow-up for scoliosis |
| Mean age | Not reported | 14.7 years (SD 4.8) | 14.8 years (SD 3.6) |
| Proportion male | Not reported | 36 % | 22 % |
| Intervention | EOS® (earlier version, referred to as ‘the Charpak system’) | EOS® | EOS® |
| Comparator | Film | Film | Fuji FCR 7501S |
| Image quality results | Image quality comparable between EOS® and film | Image quality comparable or better with EOS® for the majority of quality criteria | Image quality comparable or better with EOS® for the vast majority of images |
| Radiation dose results | Mean ESD (mGy) | Mean ESD (mGy) | Mean ESD (mGy) |
| Spine PA | EOS® 0.07, film 0.92. Ratio of means: 13.1 | EOS® 0.23, film 1.2. Ratio of means: 5.2 calculated by CRD | |
| Spine lateral | EOS® 0.13, film 1.96. Ratio of means: 15.1 | EOS® 0.37, film 2.3. Ratio of means: 6.2 calculated by CRD | |
| Spine AP | EOS® 0.08, film 0.93. Ratio of means: 11.6 | ||
| Pelvis | EOS® 0.06, film 1.13. Ratio of means: 18.8 | ||
| Centre of back | EOS® 0.18, CR 1.04. Ratio of means: 5.9 | ||
| Proximal lateral point | EOS® 0.27, CR 2.38. Ratio of means: 8.8 | ||
| Outer side of proximal breast | EOS® 0.11, CR 0.83. Ratio of means: 7.6 | ||
| Proximal anterosuperior iliac spine | EOS® 0.16, CR 1.47. Ratio of means: 9.2 | ||
| Proximal iliac crest | EOS® 0.30, CR 2.47. Ratio of means: 8.2 | ||
| Distal iliac crest | EOS® 0.11, CR 0.73. Ratio of means: 6.5 | ||
| Nape of neck | EOS® 0.20, CR 0.59. Ratio of means: 2.9 |
In view of the heterogeneity of the included studies, in terms of participant characteristics and comparator technologies, formal meta-analysis was not appropriate. Therefore, the studies were grouped according to the comparator technology used and a narrative synthesis is presented.
Quality of the included studies
Quality assessment highlighted limitations in each of the included studies. The results of the quality assessment are presented in Table 2, including an assessment of the overall risk of bias across studies. The study by Kalifa [15] was the largest study with 140 participants. However, some methods were not fully reported, for example the execution of the intervention and comparator technologies was not described in sufficient detail to permit their replication, and the authors did not report whether the tube voltage was similar between the two systems. A major limitation of the study by Le Bras [16] was the high proportion of patient withdrawals, which may have biased the results. The study by Deschenes [17] was well reported, with the execution of both technologies described in sufficient detail. In addition, the authors attempted to reduce the potential for bias in the interpretation of image results by using blinded assessment of image quality outcomes. The major limitation of this study was the small sample size of only 50 patients. In addition, standard deviations were not reported for the mean dosimetry results, making it impossible to assess the certainty of the estimates.
Table 2.
Quality assessment results
| Quality assessment criteria | Study | Overall risk of bias | |||
|---|---|---|---|---|---|
| Kalifa [15] | Le Bras [16] | Deschênes [17] | |||
| 1 | Was the spectrum of patients representative of the patients who will receive the test in practice? | Yes | Yes | Yes | Low |
| 2 | Were selection criteria clearly described? | Yes | No | No | Unclear |
| 3 | Is the reference standard likely to correctly classify the target condition? | Not applicable | Not applicable | Not applicable | Not applicable |
| 4a | Is the time period between reference standard and index test short enough to be reasonably sure that the target condition did not change between the two tests? | Yes | Yes | Yes | Low |
| 5a | Did the whole sample or a random selection of the sample receive verification using a reference standard of diagnosis? | Yes | Yes | Yes | Low |
| 6a | Did patients receive the same reference standard regardless of the index test result? | Yes | Yes | Yes | Low |
| 7a | Was the reference standard independent of the index test (i.e., the index test did not form part of the reference standard)? | Yes | Yes | Yes | Low |
| 8a | Was the execution of the index test described in sufficient detail to permit replication of the test? | No | Yes | Yes | Unclear |
| 9a | Was the execution of the reference standard described in sufficient detail to permit its replication? | No | Yes | Yes | Unclear |
| 10a | Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | No | Yes | High |
| 11a | Were the reference standard results interpreted without knowledge of the results of the index test? | Unclear | No | Yes | High |
| 12 | Were the same clinical data available when test results were interpreted as would be available when the test is used in practice? | Unclear | Unclear | Unclear | Unclear |
| 13 | Were uninterpretable/intermediate test results reported? | Not applicable | Not applicable | Not applicable | Not applicable |
| 14 | Were withdrawals from the study explained? | Yes | No | Yes | Unclear |
| 15b | Was a sample size calculation used? | Yes; but no details were reported. The authors intended to recruit 150 participants; only 140 participants were included in the analysis | Not reported | Not reported | Unclear |
| 16b | Was the method for measuring radiation dose appropriate for both the intervention and comparator technologies? | Yes; basic, but appropriate | Yes | Yes; basic, but appropriate | Low |
| 17b | Was the method of measuring image quality appropriate for both the intervention and comparator technologies? | Unclear. Appropriate criteria used; however, it is not clear if results were reported for ‘agreed results’ or if seen by one reader. Not stated how results were categorised as ‘good’ or ‘poor’—cutoff not defined | Yes | Yes | Low |
| 18b | Was the execution of the intervention technology as it would be in practice? | No; the apparatus used for the paper appears to be a ‘bespoke’ unit (the ‘Charpak system’), but appears to be similar in many ways to EOS®. In addition, digital images were viewed on radiographic laser film, rather than on the screen, which is not as it would be in practice | Yes | Yes | Low |
| 19b | Was the execution of the comparator technology as it would be in practice? | Yes | Yes | Yes | Low |
| 20b | Were measures of variability for outcomes reported? | Standard deviations were not reported for dosimetric results | Standard deviations were not reported for ‘percentage decrease’ for dosimetric results | Standard deviations were not reported for dosimetric results | High |
| 21b | Any other comments? | Contradiction in text: ‘all images were analysed separately by two senior radiologists… All discordant results between independent viewers were further reviewed to achieve a consensus verdict’. ‘Comparison between the two systems was made on the frequency with which each radiologist perceived the information as ‘available’ or ‘not available’. There was no attempt to obtain consensus between readers’ | Lots of withdrawals from the analysis: of the 62 PA images obtained, only 44 were assessed for image quality, 59 for radiation dose using ESAK and 46 for radiation dose using ESD; of 57 LAT images obtained, only 41 were assessed for image quality, 52 for radiation dose using ESAK and 36 for radiation dose using ESD | ||
aFor the purposes of quality assessment, EOS® was considered as the ‘index test’ and CR/film the ‘reference standard’
bQuestions 15 to 20 are the project-specific quality items
All three studies measured radiation dose appropriately and image quality was independently assessed by at least two radiologists using appropriate criteria. Radiation dose was measured using ‘entrance surface dose’, in which thermoluminescent dosimeters or optically stimulated luminescence dosimeters are placed on the patient’s skin.
The patients in the included studies were representative of patients who may benefit from EOS® in practice, primarily children (mean age 14 years, where reported) with scoliosis. The execution of EOS® and the comparator imaging systems was generally as it would be in practice, except that the study by Kalifa [15] used an earlier version of EOS® ‘the Charpak system’ and viewed the images on laser film, rather than on screen, so the results may not reflect current EOS® machines. Two of the studies reported that tube voltage was similar between the two radiographic systems [16, 17].
All three studies obtained ethical committee approval. Two of the studies declared that at least one author was employed by Biospace Med [16] or that the evaluation was supported through research funds from Biospace Med [17]. Other sources of funding were the CEDIT (Assistance Publique-Hôpitaux de Paris), the Programme Hospitalier de Recherche Clinique (PHRC) of the French Ministry of Health, Agence Nationale pour la Valorisation de la Recherche (ANVAR), Biocrit, Baxter SA and Cogema [15] and the European Union “GROWTH” programme for research and development [16].
Synthesis of the included studies
None of the studies reported patient health outcomes; there was no evidence that the facilities offered by EOS®, such as the ability to scan a full body image (removing the need for digital stitching/manual joining of multiple images), or the ability to take PA and lateral images simultaneously (so that a three-dimensional image can be produced), translated into patient health benefits. None of the included studies compared the measurement of the Cobb angle between EOS® and CR or DR, despite including patients with scoliosis.
Both studies comparing EOS® (or the earlier ‘Charpak system’) with film X-ray imaging [15, 16] found image quality to be comparable or better with EOS® overall. The study comparing EOS® with CR [17] found image quality to be comparable or better with EOS® for the majority of images (see Table 1).
Radiation dose was significantly lower with EOS® (or the Charpak system) than film X-ray for all images: the mean entrance surface dose with EOS® (or the Charpak system) for the PA spine was 0.23 milligray (mGy) (0.07 mGy for the Charpak system) compared with 1.2 mGy (0.92 mGy) with film; the mean entrance surface dose with EOS® (or the Charpak system) for the lateral spine was 0.37 mGy (0.13 mGy for the Charpak system) compared with 2.3 mGy (1.96 mGy) with film. The ratio of mean doses for PA spine was 5.2 (13.1 for the Charpak system); the ratio of mean doses for the lateral spine was 6.2 (15.1 for the Charpak system). The studies did not report confidence intervals or standard deviations. One study reported ranges [15] which indicated that they did not overlap for the majority of results.
Radiation dose was considerably lower with EOS® than CR for all images: the mean entrance surface dose with EOS® for the centre of the back was 0.18 mGy compared with 1.04 mGy with CR; the mean entrance surface dose with EOS® for the proximal lateral point was 0.27 mGy compared with 2.38 mGy with CR; the mean entrance surface dose with EOS® for the nape of the neck was 0.20 mGy compared with 0.59 mGy with CR. The ratio of mean doses for the centre of the back was 5.9 and for the proximal lateral point 8.8. The lowest ratio of mean doses was at the nape of the neck, which was 2.9. This study did not report confidence intervals or standard deviations.
To put this level of radiation in context, the average entrance surface dose for an adult PA chest X-ray is 0.11 mGy [18].
Discussion
This systematic review identified that only a small amount of limited quality data are available for the assessment of the clinical effectiveness of EOS® in scoliosis. The available data suggest that EOS® can generate comparable or better image quality than standard X-ray film or CR and is associated with a reduced radiation dose. However, no data were identified in relation to patients’ health outcomes, for example there is no evidence from any of the studies that the use of EOS® improves the monitoring or treatment of scoliosis.
Ilharreborde et al. [19] have shown the reproducibility of 2D and 3D measurements in scoliosis cases imaged with EOS®. They have speculated on the potential benefits of improved 3D information, but as yet they have not proved this hypothesis.
Strengths and limitations of the review
This was a rigorous systematic review, which addressed a clear research question using predefined inclusion criteria. Comprehensive literature searches were performed in order to locate all of the relevant published and unpublished studies, without any language restrictions, minimising the potential for publication bias and language bias.
Study selection was undertaken independently by two reviewers and data extraction and quality assessment were checked by a second reviewer to minimise the potential for reviewer bias or error. Validity assessment was undertaken using a validated checklist for diagnostic studies, with additional project-specific quality assessment items.
The main finding of this systematic review was that there was limited data on the clinical effectiveness of EOS®. Only three studies comparing EOS® with conventional X-ray imaging were identified; two of which only included a small number of participants. Importantly, none of the included studies assessed patient health outcomes.
In terms of a framework of diagnostic technology evaluation [10], the available clinical evidence for EOS® is limited to establishing the basic technical ability of the technology. The technical advancements associated with the EOS® generated image (the ability of EOS® to generate a full body scan and the ability to construct a three-dimensional model) have not been investigated for their impact on patient outcomes. Clinical studies that investigate the impact of EOS® on patient management are required. Such studies should compare EOS® with standard imaging (CR or DR) in patients with scoliosis and other relevant indications. The increasing recognition of the importance of spino-pelvic parameters and global spinal balance in all spinal pathologies leads us to suggest that a clinical evaluation of this system across all spinal pathology would be valuable. In the first instance, such studies should investigate whether the specific assessments required (e.g., in scoliosis, the Cobb angle measurement) are improved, or whether the use of EOS® enables a better assessment of disease progression. In addition, it is important that studies assess long-term outcomes, i.e., the proportion of patients for whom the use of EOS® changes diagnosis and/or therapy, and whether any therapeutic changes result in improved patient health outcomes.
Whilst radiation dose is a concern for patients who require repeated imaging, and appears to be a clear benefit of EOS® over standard X-ray technology, it is difficult to quantify the reductions in radiation dose seen with EOS® in terms of patient health benefits. Furthermore, it is unclear whether the radiation doses reported in the EOS® studies are the same as they would be in clinical practice. Whilst two of the studies reported that tube voltage was similar between the two radiographic systems, it is unclear whether the other exposure factors were similar. It is also unclear how these relate to the factors used in a clinical setting, hence the uncertainty regarding dose in practice. Radiographic equipment can be used in such a way as to reduce radiation dose, but this reduction in radiation dose results in a reduction in image quality. Radiation dose should be ‘as low as reasonably achievable’ (ALARA), which means obtaining the best image quality necessary for the lowest possible radiation dose. Monitoring patients with scoliosis does not require high-quality images, because the image is only required to show the geometry of the vertebral column, rather than the bony detail, and therefore a low-dose (high-speed) acquisition is appropriate [9]. It is possible to use the EOS system to take a single view (e.g. just a PA radiograph to monitor the coronal plane deformity). An understanding of the risks and benefits of two views (with computation of a 3D model) versus a single view (for 2D monitoring, with further dose reduction) will not become clear until clinical studies have quantified the benefits of 3D analysis.
The long-term benefit to patients associated with a reduced radiation dose is an important consideration, but it is not something that was or could be investigated in short-term studies of EOS®. A large cohort study of patients with scoliosis and other spinal deformity, in the USA, exposed to repeated X-ray monitoring found that there was evidence of an increased risk of breast cancer mortality amongst spinal deformity patients compared with the general female population of the USA [8]. However, this finding might be confounded by characteristics of patients with spinal deformity which may affect their eligibility for, or response to, cancer treatment. In addition, the relevance of this cohort to current clinical practice may be questionable: the included patients were diagnosed with spinal deformity between 1912 and 1965, since which time radiation doses from X-ray examinations have decreased substantially, due to technological advancements and the use of procedures to reduce radiation dose, such as using the PA view (rather than anteroposterior), appropriate collimation and breast shielding.
Previous research describing the EOS® technology was limited to small comparative studies or non-comparative case series. This systematic review critically appraises and synthesises the available evidence on the clinical effectiveness of EOS®, compared with standard X-ray film, computed radiography or digital radiography, for patients with orthopaedic conditions. The main finding of this systematic review is that there is limited data on the clinical effectiveness of EOS®; the technical advancements associated with EOS® (the ability to generate a full body scan and to construct a three-dimensional model) have not been evaluated in terms of their impact on scoliosis patient management, or longer-term health outcomes.
In conclusion, whilst the technical advancements of EOS® appear promising, much further clinical research is required in order to establish the nature and extent of any benefits in terms of patient management and patient health outcomes associated with the use of EOS®.
Acknowledgments
We would like to thank Lisa Stirk, Information Specialist at the Centre for Reviews and Dissemination for devising the search strategy and carrying out the literature searches. We would like to thank the following for providing clinical advice: Professor Jeremy Fairbank, Consultant Orthopaedic Surgeon, Nuffield Orthopaedic Centre NHS Trust; Dr David Grier, Consultant Paediatric Radiologist, Bristol Royal Hospital for Children; Mr Peter Millner, Consultant Orthopaedic and Spinal Surgeon, Leeds Teaching Hospitals NHS Trust; Dr James Rankine, Consultant Radiologist, Leeds Teaching Hospitals NHS Trust. This report was commissioned by the National Institute for Health Research (NIHR) Health Technology Assessment (HTA) Programme on behalf of the National Institute for Health and Clinical Excellence (NICE) as project number HTA 10/67/01. The views expressed are those of the authors and not necessarily those of the NIHR HTA Programme. Any errors are the responsibility of the authors.
Conflict of interest
Nigel Gummerson has received travel, accommodation and course expenses unrelated to this piece of work from the following spinal implant companies: Biomet, DePuy, Zimmer, K2M, Medtronic and Synthes.
References
- 1.Georges Charpak. The Nobel Foundation “The Nobel prize in physics 1992”. Available from http://www.nobelprize.org/nobel_prizes/physics/laureates/1992/index.html. Accessed 28 June 2012
- 2.Morvan G, Mathieu P, Vuillemin V, Guerini H, Bossard P, Zeitoun F, Wybier M. Standardized way for imaging of the sagittal spinal balance. Eur Spine J. 2011;20:602–608. doi: 10.1007/s00586-011-1927-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gummerson NW, Millner PA. Spinal fusion for scoliosis, clinical decision-making and choice of approach and devices. Skeletal Radiol. 2010;39:939–942. doi: 10.1007/s00256-010-0995-0. [DOI] [PubMed] [Google Scholar]
- 4.Stokes IAF. Three-dimensional terminology of spinal deformity: a report presented to the Scoliosis Research Society by the Scoliosis Research Society working group on 3D terminology of spinal deformity. Spine. 1994;19:236–248. doi: 10.1097/00007632-199401001-00020. [DOI] [PubMed] [Google Scholar]
- 5.Illes T, Tunyogi-Csapo M, Somoskeoy S. Breakthrough in three-dimensional scoliosis diagnosis: significance of horizontal plane view and vertebra vectors. Eur Spine J. 2011;20:135–143. doi: 10.1007/s00586-010-1566-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deacon P, Flood BM, Dickson RA. Idiopathic scoliosis in three dimensions: a radiographic and morphometric analysis. J Bone Joint Surg Br. 1984;66-B:509–512. doi: 10.1302/0301-620X.66B4.6746683. [DOI] [PubMed] [Google Scholar]
- 7.Lazennec JY, Brusson A, Rousseau MA. Hip–spine relations and sagittal balance clinical consequences. Eur Spine J. 2011;20:686–698. doi: 10.1007/s00586-011-1937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ronckers CM, Land CE, Miller JS, Stovall M, Lonstein JE, Doody MM. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res. 2010;174:83–90. doi: 10.1667/RR2022.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seibert JA. Tradeoffs between image quality and dose. Pediatr Radiol. 2004;34:S183–S195. doi: 10.1007/s00247-004-1268-7. [DOI] [PubMed] [Google Scholar]
- 10.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making. 1991;11:88. doi: 10.1177/0272989X9101100203. [DOI] [PubMed] [Google Scholar]
- 11.Centre for Reviews and Dissemination (2009) Systematic reviews of clinical tests. In: Centre for Reviews and Dissemination. Systematic reviews: CRD’s guidance for undertaking reviews in health care. University of York, York
- 12.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McKenna C, Wade R, Faria R, Yang H, Stirk L, Gummerson N, Sculpher N, Woolacott N. EOS 2D/3D X-ray imaging system: a systematic review and economic evaluation. Health Technol Assess. 2012;16:1–181. doi: 10.3310/hta16140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whiting P, Rutjes AWS, Reitsma JB, Bossuyt PMM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25. doi: 10.1186/1471-2288-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalifa G, Charpak Y, Maccia C, Fery-Lemonnier E, Bloch J, Boussard JM, Attal M, Dubousset J, Adamsbaum C. Evaluation of a new low-dose digital X-ray device: first dosimetric and clinical results in children. Pediatr Radiol. 1998;28:557–561. doi: 10.1007/s002470050413. [DOI] [PubMed] [Google Scholar]
- 16.Le Bras A, Dorion I, Ferey S, Maccia C, Parent S, Kalifa G Low dose 2D-3D X-ray scanning imaging for osteoarticular pathologies: initial results on scoliotic children (unpublished study)
- 17.Deschenes S, Charron G, Beaudoin G, Labelle H, Dubois J, Miron M-C, Parent S. Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine. 2010;35:989–994. doi: 10.1097/BRS.0b013e3181bdcaa4. [DOI] [PubMed] [Google Scholar]
- 18.Hart D, Hillier MC, Wall BF. Doses to patients from radiographic and fluoroscopic X-ray imaging procedures in the UK-2005 review. Didcot: Health Protection Agency; 2007. p. 89. [Google Scholar]
- 19.IIlharreborde B, Steffen JS, Nectoux E, Vital JM, Mazda K, Skalli W, Obeid I. Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine. 2011;36:E1306–E1313. doi: 10.1097/BRS.0b013e3182293548. [DOI] [PubMed] [Google Scholar]