Abstract
Introduction
Direct apical vertebral rotation represents an important goal of posterior surgery for thoracic adolescent idiopathic scoliosis (AIS), so as to obtain a better cosmetic effect and to avoid posterior thoracoplasty. However, the real effectiveness in correction of vertebral rotation, using posterior only procedures, is still open to debate. The aim of the present study is to compare the correction of axial apical rotation obtained with direct rotation procedure versus simple concave rod rotation, in patients treated by posterior fusion for thoracic AIS using pedicle screw-only construct.
Materials and methods
A retrospective review was performed on a total of 62 consecutive patients (one single institution, three different surgeons) affected by AIS, who had undergone a posterior spinal fusion with pedicle screw-only instrumentation between January 2005 and April 2008 at the reference center. All cases presented a main thoracic curve (Lenke type 1 and 2). The angle of rotation (RAsag) of the apical vertebra was measured from the preoperative and last follow-up axial CT. According to the derotation procedure, two groups were identified: a direct vertebral rotation group (DR group; n = 32 patients) and a simple concave rod rotation group (No-DR group; n = 30 patients). There were no statistical differences between the two groups, in terms of age, Risser’s sign, curve patterns, Cobb main thoracic (MT) curve magnitude and flexibility, extension of fusion, offset measurements on the coronal plane and sagittal preoperative contour.
Results
All 62 patients were reviewed at an average follow-up of 3.7 years (range 2.5–4.2 years). The DR group compared to the No-DR group showed a significantly better final correction of apical vertebral rotation (DR 63.4 % vs. No-DR 14.8 %; p < 0.05) and a greater final correction (61.3 vs. 52.4 %; p < 0.05) with better maintenance of the initial correction (−1.7° vs. −1.9°; ns) of the main thoracic curve. Concerning the coronal balance, there was the same aforementioned trend of better results in the DR group, with less final apical MT vertebra translation (DR 2.2 cm vs. No-DR 4.1 cm), greater overall change (preop-final) of lower instrumented vertebra (LIV) coronal tilt (−14.9° vs. −11.1°; p < 0.05); the final global coronal balance (C7–S1) resulted quite better in DR group, but without a significant difference. The T5–T12 kyphosis angle was quite similar in both group before surgery (DR 16.8° vs. No-DR 17.5°) and was little lower at final follow-up evaluation in direct vertebral rotation group (14.5° vs. 16.5°). The T10–L2 sagittal alignment angle was similar in each group before surgery (12.5° in DR vs. 11.8° in No-DR), and at the latest follow-up averaged 5.3° versus 8.2°, respectively. Lumbar lordosis was similar in each group before surgery (DR −42° vs. No-DR −44.1°) and at the final follow-up evaluation (−45.9° vs. −43.2°). At the latest follow-up, SRS-30 and SF-36 findings were similar between the two groups. The complication rate was higher in the simple concave rod rotation group (13.3 vs. 9.3 %), related in two cases to thoracoplasty, which was never utilized in direct rotation patients.
Conclusions
The direct vertebral rotation obtained significantly better final results, when compared to simple concave rod rotation, both concerning correction of apical vertebral rotation and magnitude of MT curve. On the other hand, the DR group presented a little reduction in T5–T12 kyphosis at follow-up, in comparison with concave rod rotation procedure. Both procedures were found to be satisfying from patients’ perspective. Nevertheless overall complication rate was higher in the simple concave rod rotation group, related mainly to thoracoplasty (2 cases), which was never necessary in direct rotation patients.
Keywords: Adolescent idiopathic scoliosis, Posterior instrumented fusion only, Direct rotation procedure
Introduction
Adolescent idiopathic scoliosis (AIS) represents a complex three-dimensional deformity. The rotation of the apical vertebrae is primarily responsible for the rib hump that represents the main cosmetic problem for adolescent patients. Thoracoplasty is often necessary to enhance the cosmetic result of a posterior instrumented fusion [16]. However, rib resections presented adverse pulmonary effects, with a 27 % decrease of pulmonary function at 3 months and a 16 % reduction at 1 year [24, 26], even if at a long-term follow-up such deterioration was not confirmed [15]. The possibility to obtain a direct apical vertebral derotation represents an important goal of posterior surgery for thoracic AIS, so as to realize a better cosmetic effect and to avoid the use of posterior thoracoplasty.
About 30 years ago, Cotrel and Dubousset [10] introduced the concept of the concave rod rotation to obtain a three-dimensional correction in scoliosis surgery. Regardless better results obtained both in coronal and sagittal planes in comparison with previous posterior procedures, many papers reported on only a limited effect to the apical rotational correction, using C-D instrumentation. Lenke et al. [25] assessed a 11° of rotation improvement. A little or a limited amount of rotational correction has been reported by Krismer et al. [20] and Bridwell et al. [6]. At last, Lee et al. [22] highlighted that the C-D rod rotation has a powerful postero-medialization effect on the curve, but a doubtful effect on rotational correction.
The idea of derotating the apical vertebra has been described more than 10 years ago by Pratt et al. [31] using sticks attached to pedicle screws. Successively, Lee et al. [22] used direct vertebral rotation by application of a posterior force in the direction opposite to that of the deformity: the results were significantly better for rotational correction (42.5 vs. 2.4 %) and coronal correction too (79.6 vs. 68.9 %) than simple rod rotation procedure. Other techniques of posterior derotation have been proposed later on, such as the vertebral coplanar alignment by Vallespir et al. [36] with slotted tubes attached to convex side screws, or the vertebral column manipulation (VCM) by Lenke [7] with a direct vertebral rotation device. Recently, a better thoracic derotation using uniplanar apical screws and direct derotation maneuvers has been reported [11, 21].
The aim of our study is to compare the correction of axial apical rotation, obtained with a direct vertebral rotation procedure in comparison with a simple concave rod rotation, in patients treated by posterior fusion for thoracic AIS using pedicle screws construct.
Materials and methods
Patient evaluation
A retrospective review, based on a database search, was performed to identify all AIS patients who had undergone posterior spinal fusion with pedicle screw-only instrumentation between January 2005 and April 2008 at the reference center. The inclusion criteria were: (1) diagnosis of adolescent idiopathic scoliosis; (2) main thoracic curve (Lenke type 1 and 2); (3) posterior fusion using pedicle screw-only construct; (4) a minimum clinical and radiographic follow-up of 2.5 years.
An independent spine surgeon reviewed all the medical records and X-rays of the patients considered. Inpatient and outpatient charts were used for collecting demographic data, peri-operative treatment, and annotation of any medical and surgical-related complications, including revision surgeries. Radiographic evaluation included standing posterior-anterior and lateral films on long-cassettes (90 × 30 cm), before and after surgery and at the latest follow-up. The Lenke et al. [26] surgical classification of AIS was used to describe curve patterns. Cobb measurements [9] of the major thoracic (MT) curves were obtained, and the lateral films were evaluated for thoracic kyphosis (T5–T12), lumbar lordosis (superior endplate of L1 to inferior endplate of L5), and thoracolumbar sagittal alignment (T10–L2). Supine preoperative bending films of the major and compensatory curves were also used to determine flexibility. Offset on the coronal plane was determined by measuring (in centimeters) the global coronal balance, as the distance between the C7 plumb line and the perpendicular line drawn through the center of the S1 vertebral body (center sacral vertical line), and the translation of the apical thoracic vertebra (AVT), as the distance between C7 plumb line and the center of the apical thoracic vertebral body or disc. The lowest instrumented vertebra tilt angle (LIV tilt) on the coronal plane (angle between an horizontal line and the lower endplate of LIV) was also assessed in degrees [30, 35]. MRI of the spine, including cervical, thoracic and lumbar segments, was performed preoperatively to exclude congenital intramedullary anomalies.
The vertebral rotation was measured from the preoperative and last follow-up axial CT using the methods described by Aaro and Dahlborn [1]. Image slices at each apical vertebra were selected by using either the scout, sagittal, and/or coronal reconstructions to ensure that the axial images were taken parallel to the end plates. The selected image of the apical vertebra included both pedicles and junction of the inner surface of the laminae. The angle of rotation (RAsag) of the vertebra was measured by using the angle between the junction of the laminae, the dorsal central aspect of the vertebral foramen and the middle of the vertebral body, and the sagittal plane. Preoperative and follow-up RAsag were measured in all cases.
A total of 62 consecutive patients (one single institution, three different surgeons) fulfilled our inclusion criteria. According to the derotation procedure, two groups were identified: a direct vertebral rotation group (DR group; n = 32 patients), and a simple concave rod rotation group (No-DR group; n = 30 patients).
Operative procedures
Intraoperative monitoring of spinal cord function was provided in all patients of both groups by recording somatosensory evoked potentials (SEPs) and transcranial electric stimulation-motor evoked potentials (TES-MEPs) [30, 34]. A neurophysiological change was defined relevant when it consisted of a persistent unilateral or bilateral reduction in amplitude ≥50 % for SEPs and ≥65 % for TES-MEPs compared with baseline. The wake-up test was performed intraoperatively only in 2 cases (1 patients of DR group, and 1 of No-Dr group) due to particular technical difficulties in acquiring the evoked responses.
The same operating table was used in all patients. All cases underwent posterior instrumented fusion after a meticulous exposure of the posterior elements of the spine to the tips of the transverse processes bilaterally. For thoracic screw placement we used the spatula technique [12] that allowed for inspection with a spatula inside the canal of the borders of the pedicle, after excision of spinous process, ligamentum flavum and superior part of lamina. A radical posterior release was performed in every patient at each level to be fused, obtaining a Smith-Pethersen osteotomy at 3–4 levels for apical vertebrae. In all cases the instrumentation alloy implanted was in titanium, using monoaxial reduction screws at each level; polyaxial reduction screws were occasionally used in more severe scoliosis in periapical sites to reduce the difficulties of rod capture. For the concave rod a Cobalt–Crome alloy was preferred as its inherent stiffness permits a better correction of scoliosis curve and thoracic hypokyphosis. Arthrodesis was carried out using banked bone (obtained from femoral epiphyses) and autologous chips obtained from resected ribs, when thoracoplasty was done. Posterior thoracoplasty was performed using the same midline incision, removing 4 ribs on average (range 3–5): it happened in 25 patients of No-DR group (83.3 %) (Fig. 1), whereas no patient in the DR group has been treated by means of rib resections.
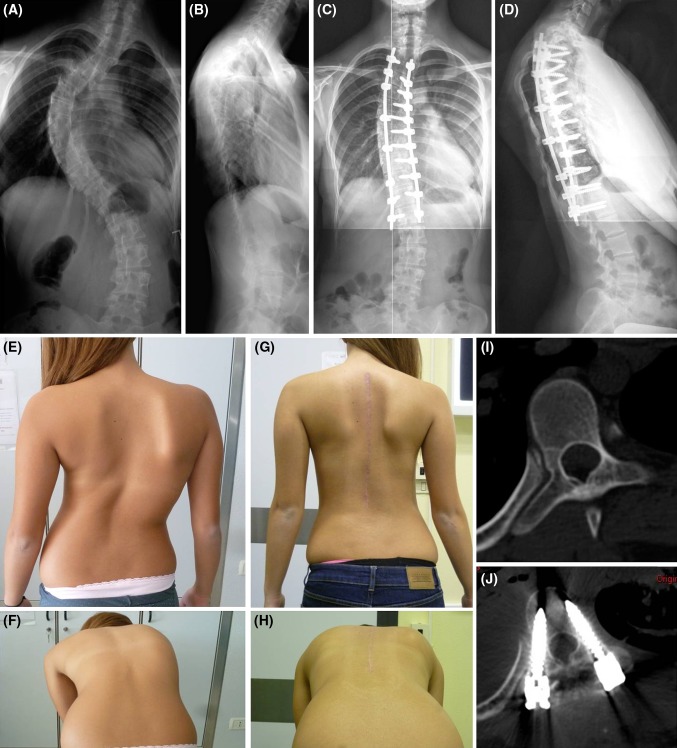
Fig. 1.
PM, 16-year-old female. AIS: MT right (88°) and left lumbar curve (46°), Lenke’s type 2BN (a, b). X-rays control 3.2 years after T3–L1 posterior fusion (simple concave rod maneuver) and thoracoplasty (c, d): MT curve was corrected to 30° (correction of 65.9 %). T5–T12 kyphosis remained unchanged at follow-up (18°) (c, d). The clinical aspect before surgery (e, f) and at last control (g, h). Apical RAsag had a negligible correction, from 21° before surgery (i) to 17° at last follow-up (j) (19 % of correction)
In the DR group (Fig. 2), instrumentation consisted of an average of 16.5 pedicle screws (range 10–19); instrumentation extended from T1 in 2 cases, T2 in 1, T3 in 19 and T4 in 10 cases, to T12 in 6 patients, L1 in 16 and L2 in 8 cases. In the No-Dr group, instrumentation included an average of 15.5 screws (range 10–18), and extended from T1 in 2 cases, T2 in 2, T3 in 14 cases and T4 in 12, to T12 in 7 cases, L1 in 14 and L2 in 9.
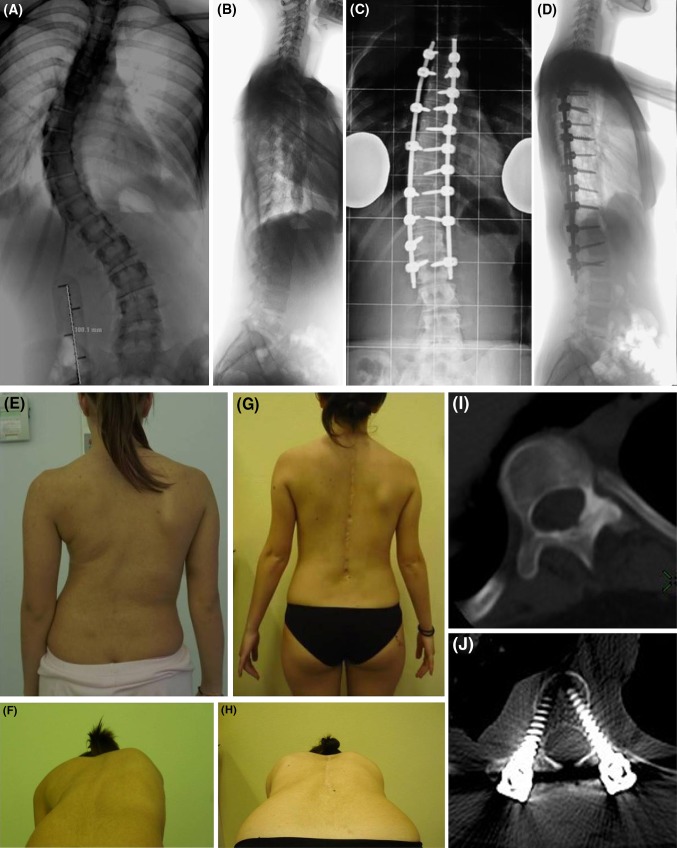
Fig. 2.
DAA, 14-year-old female. AIS: right thoracic (65°) and left lumbar curve (35°), Lenke’s type 1A-curve (a, b). X-rays control 2.8 years after T4–L2 posterior fusion (direct vertebral rotation): the thoracic curve was corrected to 18° (correction of 72.3 %) (c, d). T5–T12 kyphosis remained unchanged at follow-up (8°) (c, d). The clinical aspect before surgery (e, f) and at last control (g, h). Apical RAsag decreased from 29° before surgery (i) to 8° at last follow-up (j) (72 % of correction)
In all cases the first step of deformity correction was the concave rod rotation maneuver according to C-D procedure [10]. In DR group patients, the second step was carried out using a direct rotation maneuver, according to the Lenke’s procedure [7] using a vertebral column manipulator (VCM, Medtronic, Minneapolis, MN). The derotation initially was done with an en bloc maneuver [3] applied to apical screws (on concave and convex sides): the screws were not tightened, while the concave rod was firmly maintained in the final correct rotated position. Concurrently, an assistant applied a force on the rib prominence. Once the maneuver was completed, the sets screws were tightened. At the end, once the convex rod was placed, for increasing the rotation correction a supplementary segmentary derotation was done, starting from the distal instrumented vertebra and the next 2 proximal segments, that were rotated towards the prominence: the segmentary derotation continued to the upper level instrumented. The entire derotation procedure required about 30 min.
The operation time averaged a mean of 320 min in the DR group (range 250–370 min) and 270 min in the No-DR group (range 230–350 min). Mean intraoperative bleeding was 860 ml (range 600–1,200 ml) in the DR group, and 800 ml (range 550–1,100 ml) in the No-DR group, with a mean estimated blood loss of 14.4 and 12.7 cc/kg, respectively. No postoperative brace or a cast was used in any of the patients.
Questionnaires
Two self-reported, patient-based outcome tools, the Italian version of the SF-36 Questionnaire [2] and of the SRS-30 [4, 5] were obtained by all patients during the last follow-up visit. Statistical analysis was performed using the Mann–Whitney U test for non-parametric unpaired analysis. Results are expressed as the mean (range), with a p value of <0.05 considered as being statistically significant.
Results
The entire series of 62 cases were reviewed at an average follow-up of 3.7 years (range 2.5–4.2 years). There were no statistical differences between the direct rotation group (DR group) and the simple rod rotation one (No-DR group), in terms of age, Risser’s sign, curve patterns according to Lenke’s classification, Cobb preoperative main thoracic (MT) curve magnitude and flexibility on supine side bending, extension of fusion (Table 1), offset measurements on the coronal plane (Table 2) and sagittal preoperative contour (Table 3).
Table 1.
Posterior fusion: direct rotation (DR) versus no-direct rotation (No-DR)
| DR | No-DR | Significance | |
|---|---|---|---|
| Age | 13.1 (11 to 16) | 13.8 (12 to 14) | ns |
| Risser’s sign | 1.4 (0 to 3) | 1.8 (0 to 3) | ns |
| Lenke’s type | 25 (type 1); 7 (type 2) | 26 (type 1); 4 (type 2) | ns |
| MT curve preop | 68° (52 to 88) | 64° (50 to 84) | ns |
| Flexibility MT curve | 41 % (22 to 59) | 40 % (15 to 57) | ns |
| MT curve follow-up | 28° (20 to 50) | 35° (25 to 60) | p < 0.05 |
| Final MT curve correction | 61.3 % (39 to 72) | 52.4 % (23 to 66) | p < 0.05 |
| MT curve post surgical loss (final-postoperative) | −1.7° (−4 to 0) | −1.9° (−5 to 0) | ns |
| Fusion levels | 10.3 (8 to 11) | 10.8 (9 to 12) | ns |
| Apical RAsag preop | 27.5° (22 to 31) | 26.9° (21 to 32) | ns |
| Apical RAsag follow-up | 10.2° (8 to 13) | 22.7° (19 to 26) | p < 0.05 |
| Final Apical RAsag correction (%) | 63.4 % (54 to 68) | 14.8 % (8 to 19) | p < 0.05 |
Inside brackets (Range, minimum to maximum)
MT main thoracic, RAsag rotation angle, ns not statistically significant
Table 2.
Posterior fusion: direct rotation (DR) versus no-direct rotation (No-DR)
| Coronal measurements | DR | No-DR | Significance |
|---|---|---|---|
| AVT translation preop (cm) | 7.0 (2.6 to 9) | 7.1 (2.8 to 11) | ns |
| AVT translation postop (cm) | 2.1 (0 to 6) | 3.6 (0 to 8) | p < 0.05 |
| AVT translation follow-up (cm) | 2.2 (0.2 to 6.4) | 4.1 (0.5 to 8.8) | p < 0.05 |
| Overall change (preop-final) AVT translation | −4.8 (−2.6 to −6.5) | −3.0 (−2.2 to −5.5) | p < 0.05 |
| LIV tilt preop (°) | 21.4° (0 to 28) | 19.8° (4 to 25) | ns |
| LIV tilt postop (°) | 6.2° (0 to 11) | 8.4° (0 to 13) | ns |
| LIV tilt follow-up (°) | 4.8° (0 to 11) | 8.7° (0 to 15) | ns |
| Overall change (preop-final) LIV tilt (°) | −14.9° (0 to −22) | −11.1° (−4 to −16) | p < 0.05 |
| Global coronal balance (C7–S1) preop (cm) | 1.2 (0 to 3.8) | 1.3 (0 to 4) | ns |
| Global coronal balance (C7–S1) postop (cm) | 0.9 (0 to 4) | 1.2 (0 to 3.5) | ns |
| Global coronal balance (C7–S1) follow-up (cm) | 0.5 (0 to 2) | 0.7 (0 to 3) | ns |
Inside brackets (Range, minimum to maximum)
AVT apical thoracic vertebra, LIV lowest instrumented vertebra, ns not statistically significant
Table 3.
Posterior fusion: direct rotation (DR) versus no-direct rotation (No-DR)
| Sagittal measurements | DR | No-DR | Significance |
|---|---|---|---|
| T5–T12 kyphosis preop (°) | 16.8° (0 to 28) | 17.5° (2 to 29) | ns |
| T5–T12 kyphosis postop (°) | 14.1° (0 to 21) | 16.0° (2 to 25) | ns |
| T5–T12 kyphosis follow-up (°) | 14.5° (3 to 22) | 16.5° (4 to 26) | ns |
| T10–L2 alignment preop (°) | 12.5° (−10 to −55) | 11.8° (−18 to −58) | ns |
| T10–L2 postop (°) | 4.5° (−15 to −57) | 6.8° (−10 to −21) | ns |
| T10–L2 follow-up (°) | 5.3° (−10 to −65) | 8.2° (−10 to −22) | ns |
| L1–L5 lordosis preop (°) | −42.0° (−60 to −15) | −44.1° (−65 to −20) | ns |
| L1–L5 lordosis postop (°) | −40.8° (−55 to −15) | −41.2° (−60 to −15) | ns |
| L1–L5 lordosis follow-up (°) | −45.9° (−58 to −20) | −43.2° (−65 to −20) | ns |
Inside brackets (Range, minimum to maximum)
ns not statistically significant
The Direct Rotation (DR) group (n = 32 patients) consisted of 27 female and 5 male patients, with a mean age at surgery of 13.1 years (11–16), and a mean Risser sign of 1.4 (0–3). The curve patterns according to the Lenke’s classification were: 25 (78 %) type 1 and 7 (22 %) type 2. The preoperative MT Cobb was of 68° (52–88), which presented on spine bending test a flexibility of 41 % (22–59), and achieved a follow-up correction down to 28° (20–50), for a final correction of 61.3 % (39–72), with a mean loss of −1.7° (−4 to 0) at follow-up (Table 1). Preoperatively, in this group the angle of rotation (RAsag) of the apical vertebra was on average of 27.5° (range 22–31) and at follow-up was corrected to 10.2° (range 8–13) with a mean correction of 63.4 % (range 54–68).
The Simple concave rod rotation (No-DR) group (n = 30 patients) had 26 female and 4 male patients, with a mean age at surgery of 13.8 years (12–14), and a mean Risser sign of 1.8 (0–3). The curve patterns according to the Lenke’s classification were: 26 (86.7 %) type 1 and 4 (13.3 %) type 2. The No-DR group showed a preoperative Cobb of 64° (50–84), with a flexibility on bending test of 40 % (15–57), final correction down to 35° (25–60); an overall correction of 52.4 % (23–66), and an average loss of −1.9° (−5 to 0) at follow-up (Table 1). In these patients the angle of rotation (RAsag) of the apical vertebra was on average of 26.9° (range 21–32) before surgery and 22.7° (range 19–26) at follow-up with a mean correction of 14.8 % (range 8–19). In conclusion, the DR group compared to the No-DR group showed a significantly greater final correction (p < 0.05) and a better maintenance of the initial correction (ns) of the MT curve (Table 1). There was a significant difference between the two groups concerning the correction obtained of apical vertebral rotation at follow-up (DR 63.4 % vs. CD-R 14.8 %) (p < 0.05) (Table 1).
Concerning the coronal balance radiographic measurements (Table 2), we observed the same aforementioned trend of better results in the DR group, with less final apical MT vertebra translation (DR 2.2 cm vs. No-DR 4.1 cm), and greater overall change (preop-final) of LIV coronal tilt (DR −14.9° vs. No-DR −11.1°; p < 0.05). The final global coronal balance (C7–S1) resulted quite better in DR group, but without a significant difference (ns). The thoracic kyphosis T5–T12 angle (Table 3) was quite similar in each group before surgery (DR 16.8° vs. No-DR 17.5°), but resulted a little lower in DR group in immediate postoperative (14.1° vs. 16.0°) and at final follow-up evaluation (14.5° vs. 16.5°; ns). The thoracolumbar T10–L2 angle was similar in each group before surgery (12.5° in DR group vs. 11.8° in No-DR group); the immediate postoperative thoracolumbar contour averaged 4.5° versus 6.8° and at the latest follow-up was 5.3° versus 8.2°, respectively. Lumbar lordosis was similar in each group before surgery (DR −42.0° vs. No-DR −44.1°), in the immediate postoperative (−40.8° vs. −41.2°), and at the final follow-up evaluation (−45.9° vs. −43.2°) (Table 3). In conclusion, we found no statistically significant differences between the two groups in terms both of sagittal contour and global coronal alignment, with no patient decompensated in the final follow-up (Tables 2, 3).
The extension of fusion levels were found to be equal when the two groups were compared: DR 10.3 versus No-DR 10.8 (Table 1). The extension of unfused area was on average 4.48 (range 4–5) in the DR group versus 4.71 (range 4–5)(ns) in the No-DR group.
Questionnaires
Questionnaires scores were available in all patients, at the last follow-up. Preoperative to postoperative comparison of SRS scores could not be performed since the majority of patients in both groups had undergone surgery before an Italian version of the SRS-30 questionnaire was available. The SRS pain domain has been found to correlate well with the SF-36 bodily pain domain, correlation found also for the function domain with the SF 36 physical role domain. At the latest follow-up, SRS-30 and SF-36 findings were similar between the two groups, with mean scores shown in Table 4.
Table 4.
Posterior fusion: direct rotation (DR) versus no-direct rotation (No-DR)
| Patient-based outcome tools (F-U) | DR | No-DR | Significance |
|---|---|---|---|
| SRS pain | 4.17 | 4.24 | ns |
| SRS self-image | 3.85 | 3.46 | ns |
| SRS function | 3.54 | 3.25 | ns |
| SRS mental health | 4.02 | 3.64 | ns |
| SRS satisfaction | 4.1 | 4.36 | ns |
| SRS total score | 3.90 | 3.71 | ns |
| SF-36 physical function | 85 | 78.57 | ns |
| SF-36 role physical | 67.5 | 57.14 | ns |
| SF-36 bodily pain | 70.25 | 66.7 | ns |
| SF-36 general health | 71.6 | 72.57 | ns |
| SF-36 vitality | 70 | 69.29 | ns |
| SF-36 role emotional | 73.27 | 66.6 | ns |
| SF-36 social function | 70 | 75 | ns |
ns not statistically significant
Complications
At the latest follow-up, we found no fatal or neurologic complications, either acute or delayed deep wound infection or pseudoarthrosis in this case series.
Direct rotation group
In the DR group there were three surgery-related complications in three patients (9.3 %) that required one revision surgery (3.1 %).
One of them presented a temporary neurological complication: immediately after direct rotation, a 16-year-old girl presented the sudden drop of the amplitude of motor evoked responses at lower limbs with minor changes of SEPs recordings. The immediate removal of the rods was followed by rapid recovery of SEPs and TES-MEPs. A new attempt of direct rotation procedure presented again with a drop of the amplitude of motor evoked responses at lower limbs. The removal of the rods permitted a new recovery of SEPs and TES-MEPs responses: the surgery was concluded without attempting a DVR and finished with normal neurophysiological responses. At the end of surgery and at follow-up the girl remained neurologically intact.
A revision surgery was performed 1.9 years after the index procedure: a 16-year-old girl presented a pedicle screw pull-out at upper convex site with subcutaneous prominence, which required the pedicle screw replacement.
In another patient, a 15-year-old girl, an adding-on phenomenon was observed after a T4–L1 arthrodesis; revision surgery was refused by parents, and at the latest follow-up of 3 years, she was free of pain and the fractional curve was found stabilized.
Simple concave rod rotation group
In the Simple concave rod rotation group there were four surgery-related complications in four patients (13.3 %) that required one revision surgery (3.3 %).
Two patients (6.6 %) presented complications related to the rib resections (hemothorax in one case and pleural effusion in the other one) in the postoperative period, which required a chest tube insertion, removed 6 days later without consequences.
In a 16-year-old girl, who complained 3.6 years postoperatively of late operative site pain and persistent rib hump deformity; implant removal and posterior thoracoplasty were performed, as a solid fusion mass was detected intraoperatively.
An adding-on phenomenon was observed in a 15-year-old boy with an increase of the fractional curve below the arthrodesis, performed down to L1. The proposed revision procedure extending the arthrodesis was refused by the parents; at 3.7 years’ follow-up, he was doing well and his fractional curve was stabilized.
Discussion
The concave rod rotation maneuver proposed by Cotrel and Dubousset [10] introduced a completely new and revolutionary concept in surgical correction of AIS. This maneuver requires stable anchors at apical vertebrae on the concave side of the curve. Posterior instrumentation using apical fixation with hooks or sublaminar wires resulted inferior to periapical concave screws in the correction of rotation of AIS in the study of Fu et al. [14]: however, the correction obtained by pedicle screw construct was very small at 2 years follow-up (RAsag from 25.5° ± 4.6 to 22.6° ± 5.3), resulting more effective in flexible scoliosis curves. Similarly, pedicle screws obtained a limited effect on vertebral rotation in the study of Lee et al. [22]: the correction was negligible from 16.1° before surgery to 15.7° after simple concave rod maneuver. Recently, the concave rod rotation maneuver has been found to pronounce the rib hump prominence [3]. Kadoury et al. [19] suggested that in order to really derotate the vertebrae, moments in the opposite direction should also be applied to the spine. Recent studies confirmed the possibility to obtain a real derotation effect in AIS [3, 21, 22, 36].
However, many aspects are still open to debate. The first aspect is related to accuracy of radiographic measurements of vertebral rotation adopted in different studies. Standard methods were in the past the Perdriolle and Nash-Moe techniques, because of their simplicity [18], but resulted difficult to be evaluated after spinal instrumentation, that covers osseous landmarks on standard X-rays [33]. Other conventional measures of thoracic torsion on X-rays, particularly apical rib hump prominence (RH) and apical vertebral body-rib ratio (AVB-R), demonstrated moderate to good overall correlation with apical CT rotation measurements [21]. However, CT has been largely accepted as the most accurate method to evaluate the vertebral rotation: the criteria introduced by Aaro and Dahlborn [1] were used in some studies [3, 14, 22] and in our series, despite the higher radiation exposure for patients and underestimated derotation effect related to supine position [38].
The second aspect, the most important, is related to the choice between different procedures proposed for obtaining direct vertebral rotation. In the DVR introduced by Lee et al. [22], during or after the rod concave rotation, screw derotators, that are inserted into the juxta-apical screws on the concave and the convex sides, are rotated to the opposite direction of rod rotation. On the contrary, the vertebral coplanar alignment (VCA) proposed by Vallespir et al. [36] used slotted tubes attached to monoaxial screws at every level on the convex side. The vertebral column manipulation (VCM) introduced by Lenke [7] has been widely used and adopted in present authors center, with a derotation through either the convex or the concave side: in this procedure the derotator device is used to initially “triangulate” periapical pedicle screws, then to link the triangulated screw constructs together into a “quadrilateral” frame. We preferred this procedure for its inherent advantage of applying the derotation forces bilaterally (on concave and convex screws) so as to prevent failures with body wall cut out of screws, as documented in a recent biomechanical study [8].
Different procedures have been employed for direct vertebral rotation and it’s difficult to affirm which is the most effective technique. In our series, the derotation procedure was an en bloc maneuver in the first part, followed by, after the positioning of the convex rod, a supplementary segmentary derotation. The instrumentation alloy used was in titanium and we routinely used a Cobalt-Chrome concave rod in combination with monoaxial reduction screws. Monoaxial screws can improve significantly the vertebral derotation effect, as other authors have sustained [11, 21]. However, the direct rotation procedure required a longer operative time (320 vs. 270 min) and a higher intraoperative bleeding (860 vs. 800 ml) in comparison with simple concave rod procedure, in our series. The direct rotation can expose to neurological risks, as occurred in a patient: the use of SEPs and TES-MEPs, strongly recommended, avoided neurological deficit. The advantages are represented by the possibility to avoid the posterior thoracoplasty and its related complications, such as hemothorax or pleural effusion, that required in two of our cases a chest tube positioning in the postoperative period.
The third questionable aspect is represented by the real effect on vertebral rotation. In literature very favorable results have been reported. Lee et al. [22] with DVR obtained 42.5 % of correction. Vallespir et al. [36] with VCA concluded for 56 % rate of correction. Other authors reported higher rate of correction: Kuklo et al. [21] obtained with monoaxial screws up to 77.9 %, Asghar et al. [3] a rate of 60 % and Kadoury et al. [19] of 74 %. A study [3] compared the effect on apical rotation correction, with rods and hooks versus direct derotation with screws, obtaining a significant improvement with screws (60 vs. 22 %). Only a single report [22] considered pedicle screw-only construct and compared direct vertebral rotation versus simple concave rod rotation procedure, obtaining significantly better results with derotation. The present review focused on a similar comparison, with a substantial difference on the technique used for derotation. Our series confirm that there is a significant difference between the two groups concerning the correction of apical vertebral rotation (DR 63.4 % vs. No-DR 14.8 %; p < 0.05). Also, the DR group showed a significantly greater final correction (p < 0.05) of the MT curve, as reported by Lee et al. [22]. Considering the coronal balance, we observed the same trend of better results in the DR group, with less final apical MT vertebra translation (DR 2.2 cm vs. No-D-R 4.1 cm) and a greater overall change (preop-final) of LIV coronal tilt (DR −14.9° vs. No-DR −11.1°; p < 0.05). It must be stressed that at the latest follow-up, SRS-30 and SF-36 findings were similar between the two groups (Table 4), demonstrating a similar trend in the patients’ satisfaction. However, the complications rate was found to be superior in the No-DR group (13.3 vs. 9.3 %), that presented two cases with pulmonary adverse effects related to thoracoplasty, and quite similar for the revision rate (3.3 vs. 3.1).
Another questionable aspect is the effect of derotation procedure on thoracic sagittal profile. Thoracic pedicle screws instrumentation, without a direct vertebral derotation, has been found to enhance a loss of sagittal profile (from 8.4° to 12°) by several studies investigating the treatment of AIS [13, 23, 27, 28, 32]. In the study of Fu et al. [14], at 2-years follow-up, thoracic kyphosis resulted less of the preoperative value (14.5 ± 6.5 vs. 15.8 ± 10.7) in patients treated with screws, in contrast with increased kyphosis obtained at follow-up with hooks construct. The impression is that direct derotation with screws construct could increase this lordosing trend on thoracic kyphosis in AIS patients. This risk has been stressed [36]: the derotation may have a lordogenic effect due to the translation of the overgrown vertebral body from the lateral to an anterior position. With the exception of Lee et al. [22] that obtained a moderate increase of kyphosis with DVR, and Vallespir et al. [36] that maintained the preoperative kyphosis, other studies and our results confirmed this hypokyphotic effect from derotation procedure. Kuklo et al. [21] presented T5–T12 kyphosis reduced after surgery from 28.2° to 24.5° and from 30.8° to 27.4°, respectively, using monoaxial versus polyaxial screws with direct derotation. Vora et al. [37] compared three different posterior instrumentations for AIS patients (hooks plus intraspinous wires vs. hooks plus screws vs. direct rotation with screws): derotation with screws determined a significant loss of the preoperative kyphosis, while hybrid construct gained few degrees in kyphosis after surgery. Moreover, Mladenov et al. [29] obtained a significant decrease of thoracic kyphosis in cases treated with direct vertebral derotation, while kyphosis remained unchanged in patients with simple rod rotation. Recently, Hwang et al. [17] observed a decreased mean thoracic kyphosis postoperatively in both groups of patients (whether or not a derotation maneuver was performed during surgery); however, authors concluded that application of direct derotation in the correction of scoliosis did not additionally worsen the sagittal profile. In our patients the T5–T12 kyphosis resulted quite similar in both groups before surgery with a little decline after direct rotation procedure at follow-up, in comparison with simple rod rotation (even if such difference was not statistically significant between the two procedures).
Conclusions
The present series must be interpreted in the context of its limitations (i.e., retrospective nature of the review and patients not randomized). However, the series is a consecutive one, with no statistical differences between the two groups in terms of age, Risser’s sign, curve patterns according to Lenke’s classification, Cobb preoperative MT curve magnitude and flexibility, extension of fusion, offset measurements on the coronal plane and sagittal preoperative contour. These findings may serve to reduce some of the potential selection bias associated with nonrandomized studies.
The direct vertebral rotation obtained significantly better correction of apical vertebral rotation at follow-up (63.4 vs. 14.8 %; p < 0.05) in comparison with simple concave rod rotation. Furthermore, the DR group showed a significantly greater final correction of the MT curve (DR 61.3 % vs. No-DR 52.4 %; p < 0.05) and a better maintenance of its initial correction (−1.7 vs. −1.9°; ns). On the other hand, the thoracic T5–T12 kyphosis presented in DR group a little reduction at follow-up in comparison with simple concave rod rotation procedure (14.5° vs. 16.5°), even if such difference was not statistically significant between the two groups.
It must be stressed that at the latest follow-up, SRS-30 and SF-36 findings were similar between the two groups, with a similar trend in the patients’ satisfaction. The complication rate however was higher in the simple concave rod rotation group, related in two cases to thoracoplasty, whereas no patient in the DR group has been treated by means of rib resections.
Conflict of interest
None.
References
- 1.Aaro S, Dahlborn M. Estimation of vertebral rotation and the spinal and ribcage deformity in scoliosis by computer tomography. Spine. 1981;6:460–467. doi: 10.1097/00007632-198109000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Apolone G, Mosconi P, Ware JE (1997) Questionario sullo stato di salute SF-36. Guerini e Associati Milano
- 3.Asghar J, Samdani AF, Pahys JM, et al. Computed tomography evaluation of rotation correction in adolescent idiopathic scoliosis. A comparison of an all pedicle screw construct versus a hook-rod system. Spine. 2009;34:804–807. doi: 10.1097/BRS.0b013e3181996c1b. [DOI] [PubMed] [Google Scholar]
- 4.Asher MA, Min Lai S, Burton DC. Further development and validation of the Scoliosis Research Society (SRS) outcomes instrument. Spine. 2000;25:2381–2386. doi: 10.1097/00007632-200009150-00018. [DOI] [PubMed] [Google Scholar]
- 5.Asher M, Min Lai S, Burton D, et al. The reliability and concurrent validity of the Scoliosis Research Society-22 patient questionnaire for idiopathic scoliosis. Spine. 2003;28:63–69. doi: 10.1097/00007632-200301010-00015. [DOI] [PubMed] [Google Scholar]
- 6.Bridwell KH. Surgical treatment of adolescent idiopathic scoliosis: the basics and the controversies. Spine. 1994;19:1095–1100. doi: 10.1097/00007632-199405000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Chang MS, Lenke GL. Vertebral derotation in adolescent idiopathic scoliosis. Oper Tech Orthop. 2009;19:19–23. doi: 10.1053/j.oto.2009.04.001. [DOI] [Google Scholar]
- 8.Cheng I, Hay D, Iezza A, et al. Biomechanical analysis of derotation of the thoracic spine using pedicle screws. Spine. 2010;35:1039–1043. doi: 10.1097/BRS.0b013e3181d833d4. [DOI] [PubMed] [Google Scholar]
- 9.Cobb JR. Outline for the study of scoliosis. AAOS Instr Course Lect. 1948;5:261–275. [Google Scholar]
- 10.Cotrel Y, Dubousset J, Guillamat M. New universal instrumentation in spinal surgery. Clin Orthop. 1988;227:10–23. [PubMed] [Google Scholar]
- 11.Dalal A, Upasani VV, Bastrom TP, et al. Apical vertebral rotation in adolescent idiopathic scoliosis: comparison of uniplanar and polyaxial pedicle screws. J Spinal Disord Tech. 2011;24(4):151–257. doi: 10.1097/BSD.0b013e3181edebc4. [DOI] [PubMed] [Google Scholar]
- 12.Di Silvestre M, Parisini P, Lolli F, Bakaloudis G. Complications of thoracic pedicle screws in scoliosis treatment. Spine. 2007;32:1655–1661. doi: 10.1097/BRS.0b013e318074d604. [DOI] [PubMed] [Google Scholar]
- 13.Dobbs MB, Lenke LG, Kim YL, et al. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus pedicle screws. Spine. 2006;31:2400–2404. doi: 10.1097/01.brs.0000240212.31241.8e. [DOI] [PubMed] [Google Scholar]
- 14.Fu G, Kawakami N, Goto M, et al. Comparison of vertebral rotation corrected by different techniques and anchors in surgical treatment of adolescent thoracic idiopathic scoliosis. J Spinal Disord Tech. 2009;22:182–189. doi: 10.1097/BSD.0b013e318177028b. [DOI] [PubMed] [Google Scholar]
- 15.Greggi T, Bakaloudis G, Fusaro I, et al. Pulmonary function after thoracoplasty in the surgical treatment of adolescent idiopathic scoliosis. J Spinal Disord Tech. 2010;23:e63–e69. doi: 10.1097/BSD.0b013e3181d268b9. [DOI] [PubMed] [Google Scholar]
- 16.Harvey CJ, Jr, Betz RR, Clements DH, et al. Are there indications for partial rib resection in patients with adolescent idiopathic scoliosis treated with Cotrel-Dubousset instrumentation? Spine. 1993;18:1593–1598. doi: 10.1097/00007632-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Hwang SW, Samdani AF, Gressot LV, Hubler K, Marks MC, Bastrom TP, Betz RR, Cahill PJ. Effect of direct vertebral body derotation on the sagittal profile in adolescent idiopathic scoliosis. Eur Spine J. 2012;21(1):31–39. doi: 10.1007/s00586-011-1991-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jhaveri SN, Zeller R, Miller S, Lewis SJ (2009) The effect of intra-operative skeletal (skull femoral) traction on apical vertebral rotation. Eur Spine J 18(3):352–356 [DOI] [PMC free article] [PubMed]
- 19.Kadoury S, Cheriet F, Beausejour M, et al. A three-dimensional retrospective analysis of the evolution of spinal instrumentation for the correction of adolescent idiopathic scoliosis. Eur Spine J. 2009;18:23–37. doi: 10.1007/s00586-008-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krismer M, Bauer R, Sterzinger W. Scoliosis correction by Cotrel-Dubousset instrumentation. The effect of derotation and three-dimensional correction. Spine. 1992;17:S263–S269. doi: 10.1097/00007632-199208001-00009. [DOI] [PubMed] [Google Scholar]
- 21.Kuklo TR, Potter BK, Polly DW, Jr, et al. Monaxial versus multiaxial thoracic pedicle screws in the correction of adolescent idiopathic scoliosis. Spine. 2005;30:2113–2120. doi: 10.1097/01.brs.0000179260.73267.f4. [DOI] [PubMed] [Google Scholar]
- 22.Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine. 2004;29:343–349. doi: 10.1097/01.BRS.0000109991.88149.19. [DOI] [PubMed] [Google Scholar]
- 23.Lehman RA, Lenke LG, Keeler KA, et al. Operative treatment of adolescent scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine. 2008;33:1598–1604. doi: 10.1097/BRS.0b013e318178872a. [DOI] [PubMed] [Google Scholar]
- 24.Lenke LG, Bridwell KH, Baldus C, et al. Analysis of pulmonary function and axis rotation in adolescent and young adult idiopathic scoliosis patients treated with Cotrel-Dubousset instrumentation. J Spinal Disord. 1992;5:16–25. doi: 10.1097/00002517-199203000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Lenke LG, Bridwell KH, Baldus C, et al. Cotrel Dubousset instrumentation for adolescent idiopathic scoliosis. J Bone Jt Surg Am. 1992;74:1056–1067. [PubMed] [Google Scholar]
- 26.Lenke L, Betz R, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Jt Surg Am. 2001;83:1169–1181. [PubMed] [Google Scholar]
- 27.Lowenstein JE, Matsumoto H, Vitale MG, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw construct. Spine. 2007;32:448–452. doi: 10.1097/01.brs.0000255030.78293.fd. [DOI] [PubMed] [Google Scholar]
- 28.Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70° and 100°. Is anterior release necessary? Spine. 2005;30:2061–2067. doi: 10.1097/01.brs.0000179299.78791.96. [DOI] [PubMed] [Google Scholar]
- 29.Mladenov KV, Vaeterlein C, Stuecker R (2011) Selective posterior thoracic fusion by means of direct vertebral derotation in adolescent idiopathic scoliosis: effects on the sagittal alignment. Eur Spine J 20(7):1114–1117 [DOI] [PMC free article] [PubMed]
- 30.O’Brein M, Kuklo T, Blanke K et al (2004) Spinal Deformity Study Group. Radiographic measurement manual Ed. Medtronic Sofamor Danek, USA, pp 59–61
- 31.Pratt RK, Webb JK, Burwell RG, Cole AA (2001) Changes in surface and radiographic deformity after Universal Spine System for right thoracic adolescent idiopathic scoliosis: is rib-hump reassertion a mechanical problem of the thoracic cage rather than an effect of relative anterior spinal overgrowth? Spine 26(16):1778–1787 [DOI] [PubMed]
- 32.Quan GM, Gibson MJ. Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation. Does higher implant density improve correction? Spine. 2010;35(5):562–567. doi: 10.1097/BRS.0b013e3181b4af34. [DOI] [PubMed] [Google Scholar]
- 33.Richards BS. Measurement error in assessment of vertebral rotation using the Perdriolle torsion meter. Spine. 1992;17:513–517. doi: 10.1097/00007632-199205000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Schwartz DM, Auerbach JD, Dormans JP, et al. Neurophysiological detection of impending spinal cord injury during scoliosis surgery. J Bone Joint Surg Am. 2007;89:2440–2449. doi: 10.2106/JBJS.F.01476. [DOI] [PubMed] [Google Scholar]
- 35.Stokes IAF. Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine. 1994;19:236–248. doi: 10.1097/00007632-199401001-00020. [DOI] [PubMed] [Google Scholar]
- 36.Vallespir GP, Flores JB, Trigueros IS, et al. Vertebral coplanar alignment. A standardized technique for three dimensional correction in scoliosis surgery: technical description and preliminary results in Lenke type 1 curves. Spine. 2008;33:1588–1597. doi: 10.1097/BRS.0b013e3181788704. [DOI] [PubMed] [Google Scholar]
- 37.Vora V, Crawford A, Babekhir N, et al. A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: myth or reality. Spine. 2007;32:1869–1874. doi: 10.1097/BRS.0b013e318108b912. [DOI] [PubMed] [Google Scholar]
- 38.Yazici M, Acaroglu ER, Alanay A, et al. Measurement of vertebral rotation in standing versus supine position in adolescent idiopathic scoliosis. J Pediatr Orthop. 2001;21:252–256. [PubMed] [Google Scholar]