Abstract
Purpose
Predictors of marked improvement versus failure to improve following surgery for adult scoliosis have not been identified. Our objective was to identify factors that distinguish between patients with the best and worst outcomes following surgery for adult scoliosis.
Methods
This is a secondary analysis of a prospective, multicenter spinal deformity database. Inclusion criteria included: age 18–85, scoliosis (Cobb ≥ 30°), and 2-year follow-up. Based on the Oswestry Disability Index (ODI) and the SRS-22 at 2-year follow-up, patients with the best and worst outcomes were identified for younger (18–45) and older (46–85) adults with scoliosis. Clinical and radiographic factors were compared between patients with the best and worst outcomes.
Results
276 patients met inclusion criteria (89 younger and 187 older patients). Among younger patients, predictors of poor outcome included: depression/anxiety, smoking, narcotic medication use, older age, greater body mass index (BMI) and greater severity of pain prior to surgery. Among older patients, predictors of poor outcome included: depression/anxiety, narcotic medication use, greater BMI and greater severity of pain prior to surgery. None of the other baseline or peri-operative factors assessed distinguished the best and worst outcomes for younger or older patients, including severity of deformity, operative parameters, or the occurrence of complications.
Conclusions
Not all patients achieve favorable outcomes following surgery for adult scoliosis. Baseline and peri-operative factors distinguishing between patients with the best and worst outcomes were predominantly patient factors, including BMI, depression/anxiety, smoking, and pain severity; not comorbidities, severity of deformity, operative parameters, or complications.
Keywords: Adult scoliosis, Outcomes, Surgery, Disability, Age, Depression, Obesity, Smoking
Introduction
The prevalence of scoliosis among adults has been reported to be as high as 68 % in elderly volunteers [1]. Although the majority of those affected are asymptomatic, others may present with pain, functional limitations, neural dysfunction, and disability. Management of symptomatic adult scoliosis typically involves an initial attempt at non-operative measures. However, non-operative measures have not demonstrated a reliably durable improvement in patients with symptomatic scoliosis, and pain and disability may progress to a point warranting consideration of surgical treatment [2–7].
Most reported studies suggest that operative treatment results in significant improvement of pain, disability, and health-related quality of life [3, 4, 8–10]. However, these assessments are based on averages across large groups of patients and often inadequately emphasize the range of outcomes [3, 4, 8–10]. Certainly not all surgically treated patients achieve average or above average outcomes, and for each patient that reaches an incrementally better than average outcome, mathematics would suggest that another is achieving a commensurately poorer than average outcome. Assessing and comparing patients at the extremes of outcome measures can provide helpful insight into factors that may be predictive of outcome.
Our hypothesis was that specific clinical, radiographic, and/or surgical parameters can distinguish between adult scoliosis patients with the best and worst outcomes following surgical treatment. The purposes of this study were to assess the ranges of clinical outcomes in patients treated with surgery for adult scoliosis and to identify factors that distinguish between patients with the best and worst outcomes.
Materials and methods
Patient population and imaging
This is a secondary analysis of prospectively, consecutively collected patients from the Spinal Deformity Study Group multi-institutional database for adult spinal deformity. At enrollment and follow-up, patients complete health-related quality of life (HRQL) measures, including the Modified Oswestry Low Back Pain Disability Questionnaire v.1.2 [11] (ODI), the Scoliosis Research Society-22 (SRS-22) questionnaire [12], and back and leg pain numeric rating scale scores [12], in which extreme scores of 0 and 10 reflect no pain and “unbearable” pain, respectively. This study was approved by the institutional review boards of all participating institutions.
Inclusion criteria for the present study were: operatively treated adult idiopathic or degenerative scoliosis (Cobb > 30°) enrolled between January 2002 and June 2007, age of 18–85 years, ODI and SRS-22 at baseline and 2-years following surgery. Patients with prior spine instrumentation were excluded.
Clinical and operative data were extracted from standardized study forms. Presence of medical conditions, including anxiety/depression, was based on a patient-completed questionnaire at enrollment. A physician-completed questionnaire that details co-morbidity factors was used to calculate co-morbidity scores [13]. Short-term complications were classified as minor or major [14].
Imaging parameters
Full-length scoliosis radiographs were obtained at the time of enrollment and at follow-up. Curves were classified based on the largest coronal Cobb angle as thoracic, thoracolumbar/lumbar, or lumbosacral. Maximum Cobb angle, sagittal vertical axis (SVA), and coronal alignment (CA) were assessed using standard techniques [15]. SVA was classified into one of two groups, ≤+6 or >+6 cm, and CA magnitude was classified into one of two groups, ≤4 or >4 cm, based on previous reports that suggest these values as thresholds for disability [16, 17].
Statistical analyses
Patients were classified into one of two age groups, 18–45 or 46–85 years old. The top and bottom 15–20 % were identified for each age group, based separately on ODI and SRS-22 scores, through assessment of distribution plots. For each age group and for each outcomes measure, patients with the best and worst outcomes were compared based on clinical, radiographic, and surgical parameters.
Frequency distributions and summary statistics were calculated for all clinical, operative, and radiographic variables. For categorical variables, cross-tabulations were generated and Fisher’s exact or Pearson Chi-square tests were used to compare distributions. For continuous variables, unpaired t-tests were used to investigate differences in the distributions between subsets of patients classified by categorical data. Binary logistic regression analysis was used to adjust for the effects of multiple covariates predictive of best versus worst clinical outcomes. Statistical analyses were two-sided, and p < 0.05 was considered statistically significant.
Results
Patient population
276 patients met inclusion criteria, including 89 who were 18–45 years of age and 187 who were 46–85 years of age. Demographic and radiographic parameters are summarized in Table 1. Compared with the younger patient group, older patients had greater body mass index (BMI), higher co-morbidity score, lower prevalence of smoking, greater use of narcotics, greater severity of pain, greater disability (ODI), and poorer health status (SRS-22). Older patients were more likely to have degenerative versus idiopathic scoliosis and to be more sagittally and coronally malaligned.
Table 1.
Pre-operative demographic and radiologic parameters for operatively treated adults with scoliosis stratified based on patient age group
| Patient age group (years) | p value | ||
|---|---|---|---|
| 18–45 | 46–85 | ||
| n | 89 | 187 | |
| Female:male | 80:9 | 169:18 | 1.0 |
| Mean age (SD, range) | 32 (9, 18–45) | 59 (7, 46–83) | <0.001 |
| Mean body mass index (SD, range) | 24 (4, 16–39) | 26 (5, 16–46) | <0.001 |
| Mean comorbidity score (SD, range) | 0.7 (1.1, 0–5) | 2.7 (2.7, 0–16) | <0.001 |
| Depression/anxiety (%) | 26 | 26 | 1.0 |
| Smoker (%) | 13 | 3 | 0.006 |
| Narcotic use (%) | 12 | 38 | <0.001 |
| Mean back pain score (SD, range) | 6.0 (2.3, 2–10) | 6.6 (2.0, 2–10) | 0.049 |
| Mean leg pain score (SD, range) | 1.9 (3.0, 0–10) | 4.9 (2.8, 0–10) | <0.001 |
| Mean ODI (SD, range) | 23 (18, 0–72) | 38 (16, 0–82) | <0.001 |
| Mean SRS-22 score (SD, range) | 3.3 (0.6, 2–5) | 3.0 (0.6, 1–4) | <0.001 |
| Scoliosis etiology (%) | <0.001 | ||
| Idiopathic | 89 (100) | 147 (79) | |
| Degenerative | 0 (0) | 40 (21) | |
| Curve type (%) | <0.001 | ||
| Thoracic | 50 (56) | 39 (21) | |
| Thoracolumbar | 39 (44) | 145 (77) | |
| Lumbar/lumbosacral | 0 (0) | 3 (2) | |
| Mean maximum Cobb angle (SD, range) | 59 (15, 30–110) | 54 (18, 20–103) | 0.059 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 2 | 17 | <0.001 |
| Coronal alignment, percent with CA magnitude >4 cm | 6 | 16 | 0.042 |
ODI Oswestry Disability Index, SD standard deviation, SRS Scoliosis Research Society, SVA sagittal vertical axis, CA coronal alignment
All operative parameters assessed differed significantly between the younger and older age groups (Table 2). The vast majority of patients in each group underwent a posterior instrumented procedure, but older patients were significantly more likely to undergo both anterior and posterior procedures. The surgical procedures for older patients involved greater operative time and estimated blood loss (EBL) and had higher complication rates. A significantly greater proportion of older patients had fusion to the sacro-pelvis, compared with younger patients.
Table 2.
Operative procedures and parameters for surgically treated adults with scoliosis stratified based on patient age group
| Patient age group (years) | p value | ||
|---|---|---|---|
| 18–45 | 46–85 | ||
| n | 89 | 187 | |
| Operative data available (%) | 84 (94) | 186 (99) | |
| Anterior procedure (%) | 18 (21) | 89 (48) | <0.001 |
| Mean levels (SD, range) | 4 (2, 2–7) | 4 (2, 2–11) | |
| Posterior procedure (%) | 76 (90) | 184 (99) | 0.002 |
| Mean levels (SD, range) | 11 (3, 3–18) | 11 (4, 2–18) | |
| Fusion to the sacro-pelvis (%) | 15 (17) | 88 (47) | <0.001 |
| Mean operating room time, h (SD, range) | 7.3 (3.0, 2.0–17.5) | 8.6 (3.3, 1.0–19.0) | 0.002 |
| Mean estimated blood loss, L (SD, range) | 1.0 (0.8, 0.1–4.5) | 1.8 (1.4, 0.2–6.5) | <0.001 |
| Minor complication (%) | 11 (13) | 65 (35) | <0.001 |
| Major complication (%) | 4 (5) | 47 (25) | <0.001 |
SD standard deviation
At follow-up, there continued to be significant differences between the younger and older patient groups (Table 3). The disability, SRS-22, and leg pain scores were modestly, but significantly, poorer in the older patient group, compared with the younger patient group. The percentage of patients remaining on narcotic medications was significantly higher for the older patients. At follow-up, younger patients had greater residual Cobb angle, and older patients had greater sagittal malalignment.
Table 3.
Radiographic and clinical outcomes at follow-up for operatively treated adults with scoliosis stratified based on patient age group
| Patient age group (years) | p value | ||
|---|---|---|---|
| 18–45 | 46–85 | ||
| n | 89 | 187 | |
| Mean ODI (SD, range) | 17 (17, 0–84) | 24 (18, 0–84) | 0.001 |
| Mean SRS-22 score (SD, range) | 3.9 (0.7, 1.2–4.9) | 3.7 (0.7, 2.0–5.0) | 0.036 |
| Mean back pain score (SD, range) | 2.4 (2.4, 0–10) | 3.0 (2.5, 0–9) | 0.12 |
| Mean leg pain score (SD, range) | 0.9 (2.1, 0–10) | 2.1 (2.6, 0–10) | <0.001 |
| Narcotic use (%) | 4 (4) | 33 (18) | <0.001 |
| Mean maximum Cobb angle (SD, range) | 28 (14, 7–84) | 22 (15, 4–72) | 0.002 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 5 | 19 | 0.009 |
| Coronal alignment, percent with CA magnitude >4 cm | 6 | 8 | 0.8 |
ODI Oswestry Disability Index, SD standard deviation, SRS Scoliosis Research Society, SVA sagittal vertical axis, CA coronal alignment
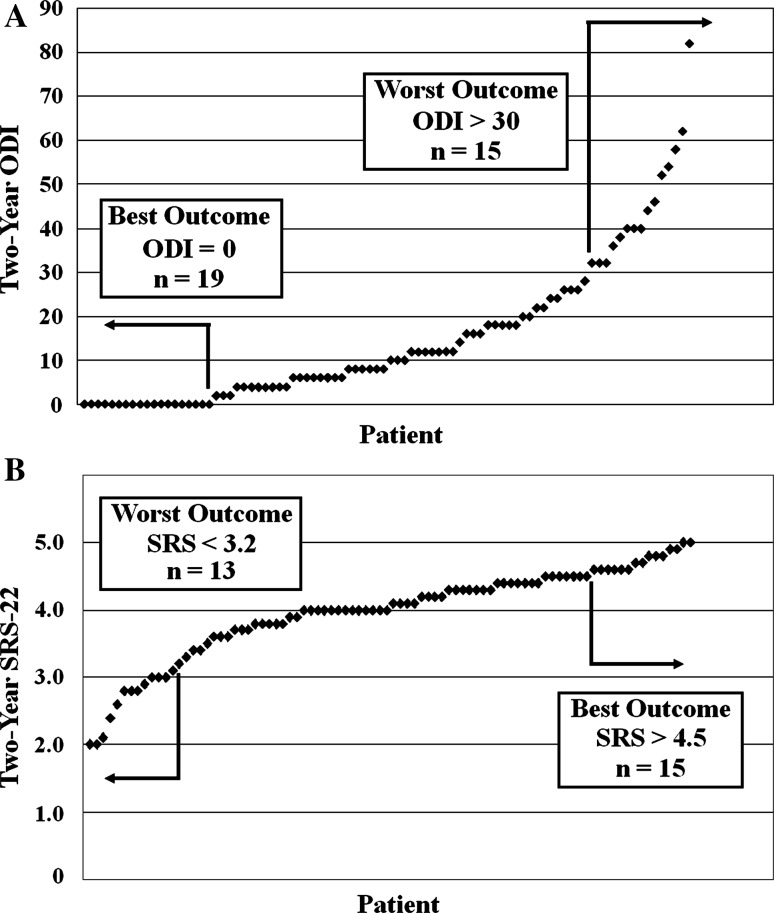
Best and worst outcomes for younger patients based on ODI
Based on the ODI, the best and worst outcome groups for younger patients (18–45 years old) consisted of 19 (22 %) with an ODI = 0 and 15 (17 %) with an ODI >30 (mean = 46, range = 32–82) at follow-up, respectively (Fig. 1a). Compared with patients with the best outcomes, those with the worst outcomes were older, had a higher BMI, had a higher prevalence of smoking, and had more leg and back pain (Table 4). The remaining baseline parameters and the operative parameters did not differ significantly between the groups, including severity of deformity, operative time, EBL, and occurrence of complications (Table 4). Although the percentage of patients treated with fusion to include the sacro-pelvis was higher in the worst outcome group compared with the best outcome group, this did not reach statistical significance. In addition, of the total 34 patients in the combined worst and best outcomes groups, only 5 had fusion that included the sacro-pelvis, and these patients were significantly older than those who did not have fusion to the sacro-pelvis (mean of 43.2 vs. 30.8 years, p = 0.003). At follow-up, compared with the best outcome group, the worst outcome group had greater back pain and modestly higher Cobb angle (Table 4).
Fig. 1.
Best and worst outcomes based on the Oswestry Disability Index (ODI, a) and the Scoliosis Research Society-22 (SRS-22, b) for adults 18–45 years old at 2 years following surgery for adult scoliosis
Table 4.
Comparison of baseline, operative, and follow-up parameters between patients with the best and worst outcomes, based on the Oswestry Disability Index, following surgery for scoliosis among adults 18–45 years old
| Worst (n = 15) | Best (n = 19) | p value | |
|---|---|---|---|
| Baseline parameters | |||
| Gender (M/F) | 1/14 | 2/17 | 1.000 |
| Mean age, years (SD) | 37 (5) | 29 (10) | 0.002 |
| Mean body mass index (SD) | 27 (5) | 22 (3) | 0.001 |
| Smoker (%) | 33 % | 0 % | 0.011 |
| Depression/anxiety (%) | 33 % | 11 % | 0.199 |
| Narcotic use (%) | 33 % | 5 % | 0.066 |
| Mean comorbidity index (SD) | 1.4 (2.1) | 0.3 (0.7) | 0.306 |
| Mean leg pain score (SD) | 3.2 (3.7) | 0.0 (0.0) | 0.010 |
| Mean back pain score (SD) | 7.2 (1.9) | 5.3 (2.8) | 0.044 |
| Diagnosis (de novo/AIS) | 0/15 | 0/19 | – |
| Curve type (thoracic/thoracolumbar) | 8/7 | 11/8 | 1.000 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 7 % | 0 % | 0.452 |
| Coronal malalignment, percent with CA magnitude >4 cm | 8 % | 6 % | 1.000 |
| Mean max coronal Cobb angle, ° (SD) | 62 (10) | 59 (14) | 0.429 |
| Operative parameters | |||
| Operative time, h (SD) | 7.3 (2.5) | 6.6 (2.6) | 0.490 |
| Estimated blood loss, L (SD) | 0.9 (0.5) | 1.1 (0.7) | 0.558 |
| Fusion to the sacro-pelvis (%) | 27 % | 5 % | 0.146 |
| Major complication (%) | 7 % | 5 % | 1.000 |
| Minor or major complication (%) | 20 % | 21 % | 1.000 |
| 2-year follow-up parameters | |||
| Mean leg pain score (SD) | 2.9 (4.1) | 0.3 (0.6) | 0.060 |
| Mean back pain score (SD) | 6.5 (1.9) | 0.6 (0.7) | <0.001 |
| Narcotic use (%) | 10 % | 0 % | 0.357 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 13 % | 0 % | 0.187 |
| Coronal malalignment, percent with CA magnitude > 4 cm | 7 % | 6 % | 1.000 |
| Mean max coronal Cobb angle, ° (SD) | 30 (9) | 22 (9) | 0.038 |
SD standard deviation, AIS adult idiopathic scoliosis, SVA sagittal vertical axis, CA coronal alignment
Significant p values are shown in bold
Best and worst outcomes for younger patients based on SRS-22
Based on the SRS-22, the best and worst outcome groups for younger patients consisted of 15 (17 %) with an SRS-22 >4.5 (mean = 4.7, range = 4.6–5.0) and 13 (15 %) with an SRS-22 <3.2 (mean = 2.7, range = 2.0–3.1) at follow-up, respectively (Fig. 1b). Of the total 24 patients with the best outcome based on either ODI or SRS-22, 10 were defined by both the ODI and SRS-22, 5 were defined based only on the SRS-22, and 9 were defined based only on the ODI. Of the total 16 patients that were categorized as having the worst outcome based on either ODI or SRS-22, 12 were defined by both the ODI and SRS-22, 3 were defined based only on the SRS-22, and 1 was defined based only on the ODI.
Compared with patients with the best outcomes, those with the worst outcomes were older, had a higher BMI, had a higher prevalence of depression/anxiety, had a higher prevalence of narcotic use, and had more leg and back pain (Table 5). The remaining baseline parameters and the operative parameters did not differ significantly between the groups, including severity of deformity, operative time, EBL, and occurrence of complications (Table 5). At follow-up, compared with the best outcome group, the worst outcome group had greater back pain (Table 5).
Table 5.
Comparison of baseline, operative, and follow-up parameters between patients with the best and worst outcomes, based on the SRS-22, following surgery for scoliosis among adults 18–45 years old
| Worst (n = 13) | Best (n = 15) | p value | |
|---|---|---|---|
| Baseline parameters | |||
| Gender (M/F) | 1/12 | 2/13 | 1.000 |
| Mean age, years (SD) | 37 (6) | 27 (7) | <0.001 |
| Mean body mass index (SD) | 28 (5) | 22 (3) | 0.002 |
| Smoker (%) | 31 % | 7 % | 0.153 |
| Depression/anxiety (%) | 38 % | 0 % | 0.013 |
| Narcotic use (%) | 38 % | 0 % | 0.030 |
| Mean comorbidity index (SD) | 1.4 (2.1) | 0.4 (0.8) | 0.278 |
| Mean leg pain score (SD) | 3.3 (3.7) | 0.2 (0.7) | 0.027 |
| Mean back pain score (SD) | 7.4 (1.9) | 5.2 (2.7) | 0.038 |
| Diagnosis (de novo/AIS) | 0/13 | 0/15 | – |
| Curve type (thoracic/thoracolumbar) | 7/6 | 6/9 | 0.705 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 8 % | 0 % | 0.480 |
| Coronal malalignment, percent with CA magnitude >4 cm | 9 % | 0 % | 0.423 |
| Mean max coronal Cobb angle, ° (SD) | 62 (11) | 55 (16) | 0.267 |
| Operative parameters | |||
| Operative time, h (SD) | 7.3 (2.8) | 6.2 (2.0) | 0.220 |
| Estimated blood loss, L (SD) | 1.0 (0.5) | 0.8 (0.5) | 0.201 |
| Fusion to the sacro-pelvis (%) | 17 % | 11 % | 1.000 |
| Major complication (%) | 8 % | 0 % | 0.464 |
| Minor or major complication (%) | 15 % | 20 % | 1.000 |
| 2-year follow-up parameters | |||
| Mean leg pain score (SD) | 2.8 (4.2) | 0.1 (0.3) | 0.092 |
| Mean back pain score (SD) | 6.6 (2.3) | 0.6 (0.9) | <0.001 |
| Narcotic use (%) | 13 % | 0 % | 0.364 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 15 % | 0 % | 0.206 |
| Coronal malalignment, percent with CA magnitude >4 cm | 0 % | 7 % | 1.000 |
| Mean max coronal Cobb angle, ° (SD) | 27 (10) | 18 (11) | 0.090 |
SRS Scoliosis Research Society, SD standard deviation, AIS adult idiopathic scoliosis, SVA sagittal vertical axis, CA coronal alignment
Significant p values are shown in bold
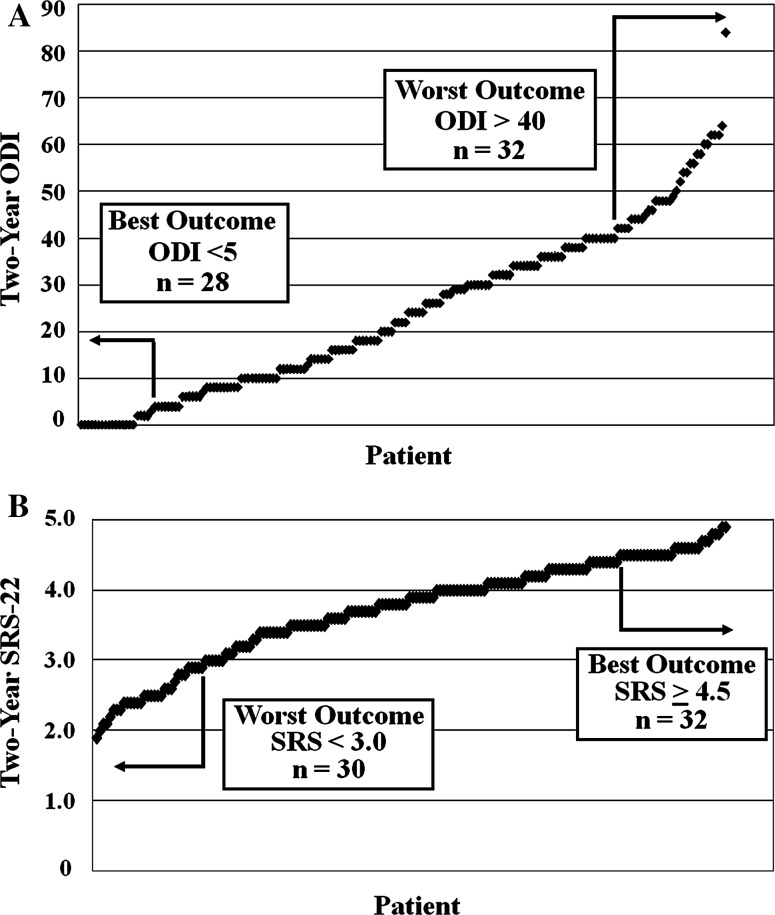
Best and worst outcomes for older patients based on ODI
Based on the ODI, the best and worst outcome groups for older patients consisted of 28 (15 %) with an ODI <5 (mean = 2, range = 0–4) and 32 (17 %) with an ODI >40 (mean = 52, range = 42–84) at follow-up, respectively (Fig. 2a). Compared with patients with the best outcomes, those with the worst outcomes had a higher BMI, had a higher prevalence of anxiety/depression, had a higher prevalence of narcotic use, and had more back pain (Table 6). The remaining baseline parameters and the operative parameters did not differ significantly between the groups, including severity of deformity, operative time, EBL, and occurrence of complications (Table 6). At follow-up, compared with the best outcome group, the worst outcome group had greater back and leg pain and higher prevalence of narcotic use (Table 6).
Fig. 2.
Best and worst outcomes based on the Oswestry Disability Index (ODI, a) and the Scoliosis Research Society-22 (SRS-22, b) for adults 46–85 years old at 2 years following surgery for adult scoliosis
Table 6.
Comparison of baseline, operative, and follow-up parameters between patients with the best and worst outcomes, based on the Oswestry Disability Index, following surgery for scoliosis among adults 46–85 years old
| Worst (n = 32) | Best (n = 28) | p value | |
|---|---|---|---|
| Baseline parameters | |||
| Gender (M/F) | 3/29 | 2/26 | 1.000 |
| Mean age, years (SD) | 58 (7) | 58 (7) | 0.749 |
| Mean body mass index (SD) | 27 (6) | 24 (4) | 0.042 |
| Smoker (%) | 9 % | 0 % | 0.241 |
| Depression/anxiety (%) | 63 % | 14 % | <0.001 |
| Narcotic use (%) | 66 % | 18 % | 0.001 |
| Mean comorbidity index (SD) | 3.1 (2.6) | 2.2 (2.0) | 0.284 |
| Mean leg pain score (SD) | 5.9 (2.1) | 5.7 (2.3) | 0.801 |
| Mean back pain score (SD) | 7.4 (1.5) | 5.5 (2.2) | 0.001 |
| Diagnosis (de novo/AIS) | 5/27 | 7/21 | 0.520 |
| Curve type (thoracic/thoracolumbar)a | 6/25 | 4/24 | 0.560 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 30 % | 20 % | 0.528 |
| Coronal malalignment, percent with CA magnitude >4 cm | 19 % | 15 % | 0.737 |
| Mean max coronal Cobb angle, ° (SD) | 54 (16) | 53 (20) | 0.336 |
| Operative parameters | |||
| Operative time, h (SD) | 8.4 (3.6) | 8.5 (3.2) | 0.911 |
| Estimated blood loss, L (SD) | 1.9 (1.5) | 1.3 (1.0) | 0.188 |
| Fusion to the sacro-pelvis (%) | 45 % | 58 % | 0.536 |
| Major complication (%) | 34 % | 18 % | 0.242 |
| Minor or major complication (%) | 50 % | 36 % | 0.305 |
| 2-year follow-up parameters | |||
| Mean leg pain score (SD) | 4.3 (3.0) | 0.9 (1.2) | <0.001 |
| Mean back pain score (SD) | 5.4 (2.1) | 0.8 (1.1) | <0.001 |
| Narcotic use (%) | 59 % | 0 % | <0.001 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 30 % | 11 % | 0.117 |
| Coronal malalignment, percent with CA magnitude >4 cm | 13 % | 0 % | 0.239 |
| Mean max coronal Cobb angle, ° (SD) | 31 (13) | 24 (14) | 0.116 |
SD standard deviation, AIS adult idiopathic scoliosis, SVA sagittal vertical axis, CA coronal alignment
aOne patient had a lumbosacral
Significant p values are shown in bold
Best and worst outcomes for older patients based on SRS-22
Based on the SRS-22, the best and worst outcome groups for older patients consisted of 32 (17 %) with an SRS-22 ≥4.5 (mean = 4.6, range = 4.5–5.0) and 30 (16 %) with an SRS-22 <3.0 (mean = 2.5, range = 1.9–2.9) at follow-up, respectively (Fig. 2b). Of the total 42 patients having the best outcome based on either ODI or SRS-22, 18 were defined by both the ODI and SRS-22, 14 were defined based only on the SRS-22, and 10 were defined based only on the ODI. Of the total 42 patients that were categorized as having the worst outcome based on either ODI or SRS-22, 20 were defined by both the ODI and SRS-22, 10 were defined based only on the SRS-22, and 12 were defined based only on the ODI.
Compared with patients with the best outcomes, those with the worst outcomes had a higher prevalence of depression/anxiety, had a higher prevalence of narcotic use, and had more back pain (Table 7). The remaining baseline parameters and the operative parameters did not differ significantly between the groups, including severity of deformity, operative time, EBL, and occurrence of complications (Table 7). At follow-up, compared with the best outcome group, the worst outcome group had greater back and leg pain, a higher prevalence of narcotic use, and a higher prevalence of sagittal malalignment (Table 7). After adjusting for the effects of 2-year follow-up sagittal malignment (SVA >6 cm) using logistic regression analysis, baseline depression/anxiety remained a significant factor in distinguishing between the best and worst outcomes (p = 0.025), baseline narcotics use demonstrated a non-significant predictive trend (p = 0.055), and baseline back pain was no longer predictive of the best and worst outcomes (p = 0.142).
Table 7.
Comparison of baseline, operative, and follow-up parameters between patients with the best and worst outcomes, based on the SRS-22, following surgery for scoliosis among adults 46–85 years old
| Worst (n = 30) | Best (n = 32) | p value | |
|---|---|---|---|
| Baseline parameters | |||
| Gender (M/F) | 3/27 | 5/27 | 0.709 |
| Mean age, years (SD) | 58 (7) | 58 (8) | 0.974 |
| Mean body mass index (SD) | 27 (6) | 25 (3) | 0.058 |
| Smoker (%) | 10 % | 0 % | 0.102 |
| Depression/anxiety (%) | 57 % | 13 % | <0.001 |
| Narcotic use (%) | 60 % | 33 % | 0.043 |
| Mean comorbidity index (SD) | 3.5 (2.6) | 2.2 (1.7) | 0.079 |
| Mean leg pain score (SD) | 5.8 (1.8) | 6.2 (2.1) | 0.530 |
| Mean back pain score (SD) | 7.2 (1.4) | 5.9 (2.3) | 0.010 |
| Diagnosis (de novo/AIS) | 8/22 | 9/23 | 1.000 |
| Curve type (thoracic/thoracolumbar)a | 5/24 | 5/26 | 0.992 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 24 % | 14 % | 0.485 |
| Coronal malalignment, percent with CA magnitude >4 cm | 14 % | 21 % | 0.730 |
| Mean max coronal Cobb angle, ° (SD) | 52 (18) | 52 (21) | 0.948 |
| Operative parameters | |||
| Operative time, h (SD) | 7.9 (3.2) | 9.3 (3.8) | 0.128 |
| Estimated blood loss, L (SD) | 2.0 (1.6) | 1.8 (1.5) | 0.545 |
| Fusion to the sacro-pelvis (%) | 33 % | 50 % | 0.142 |
| Major complication (%) | 30 % | 16 % | 0.230 |
| Minor or major complication (%) | 50 % | 28 % | 0.117 |
| 2-year follow-up parameters | |||
| Mean leg pain score (SD) | 4.5 (3.0) | 0.6 (1.0) | <0.001 |
| Mean back pain score (SD) | 5.3 (2.4) | 0.8 (1.7) | <0.001 |
| Narcotic use (%) | 56 % | 0 % | <0.001 |
| Positive sagittal malalignment, percent with SVA >+6 cm | 33 % | 3 % | 0.004 |
| Coronal malalignment, percent with CA magnitude >4 cm | 10 % | 6 % | 0.671 |
| Mean max coronal Cobb angle, ° (SD) | 27 (13) | 26 (16) | 0.972 |
SRS Scoliosis Research Society, SD standard deviation, AIS adult idiopathic scoliosis, SVA sagittal vertical axis, CA coronal alignment
aTwo patients had lumbosacral curves
Significant p values are shown in bold
Discussion
This paper provides age-stratified comparisons of patients with the best and worst outcomes following surgical treatment of adult scoliosis, based on two standardized outcome measures. Patients were stratified based on age into two groups, 18–45 and 46–85 years old. These groups differed significantly with regard to almost all demographics, pre- and post-operative clinical assessments, pre- and post-operative radiographic measures, and operative parameters assessed. In general, patients in the older age group had greater BMI, more pain, greater severity of deformity, required more operative time with greater EBL, and had substantially more complications compared with patients in the younger age group. Collectively, these data not only summarize the patient populations from which the best and worst outcomes were drawn, but also demonstrate the degree to which these groups represent different populations.
Two standardized measures were used to assess outcomes for determination of the best and worst outcomes. The ODI focuses on pain and disability, while the SRS-22 is a scoliosis-specific measure and incorporates assessment of pain, function, self-image, mental health, and satisfaction [12]. Reflective of these differences, less than one-half (48 %) of patients defined to have had the best or worst outcomes based on either the ODI or SRS-22 were defined to be so by both measures. The difference in the identification of health status by each instrument may be related to the specificity of the SRS-22 instrument for concerns of patients with scoliosis.
Among younger and older adults surgically treated for scoliosis, the present study identifies baseline and operative factors that significantly distinguish between patients with the best and worst outcomes. It is interesting that despite the substantial differences between the younger and older populations in this study, there is considerable overlap in the distinguishing factors for the two age groups. It is also interesting that despite the differences in the composition of the best and worst outcome populations defined by the ODI and SRS-22, many of the predictive factors are the same for the two outcome measures.
Poorer post-surgical outcomes for patients with depression/anxiety have been previously reported in patients with lumbar stenosis [18], adolescent idiopathic scoliosis [19], and a diverse group of lumbar pathologies [20]. Pre-operative smoking has been previously linked to poorer surgical outcomes for cervical procedures [21] and for lumbar spinal procedures [20, 22–24], including both instrumented and non-instrumented procedures. Several prior reports suggest that obese patients surgically treated for degenerative lumbar disease do not have poorer outcomes compared with non-obese patients [25–27]. In contrast to these reports, in the present study, greater BMI was significantly associated with the poorest outcomes. It is possible that greater BMI may reflect a greater degree of pre-operative deconditioning and could have negatively impacted postoperative rehabilitation.
In the present study, poor outcome in either age group, based on either the ODI or SRS-22, was not predicted by the pre-operative severity of deformity. Poor outcome was also not predicted by pre-operative co-morbidities, complexity of surgery (using operative time and EBL as surrogates), or the occurrence of minor or major complications. Other reports have also documented limited impact of complications on clinical outcome for adult scoliosis surgery [10, 28].
Not unexpectedly, at follow-up, patients in the worst outcome group had more pain and among older patients were more likely to be taking narcotic medications. Older patients in the worst outcome group based on the SRS-22 had a higher prevalence of positive sagittal malalignment on 2-year follow-up, consistent with prior reports documenting the relationship between sagittal alignment and outcome [29]. However, after accounting for the effects of 2-year follow-up sagittal malalignment using regression analysis, the association between baseline anxiety/depression and poor outcome remained significant.
Collectively, the data in the present study suggest that the factors predictive of which patients will have the best and worst outcomes following surgery for adult scoliosis are predominantly related to patient factors, not radiographic measures or surgical parameters. Although our data suggest that patients who are obese, have depression/anxiety, use narcotic medication, or have more severe pain have a greater likelihood of having a poor outcome with surgery, these factors alone should not necessarily preclude such patients from being offered surgery. When considering surgical treatment, several other factors should also be considered, including the overall severity of symptoms, impact of the symptoms on functionality and quality of life, overall health of the patient, and willingness of the patient to accept the risks of surgery [4].
The strengths of the present study include the prospective multicenter database from which data were extracted, the use of validated measures, and the relatively large patient population. In addition, patients were drawn from the practices of multiple surgeons at multiple institutions, offering representation of a broader range of patient populations and surgeon approaches. Although the data were prospectively collected, the primary limitation of this study remains the retrospective design. In addition, since this study focused on the limited subsets of patients with the best and worst outcomes, the numbers of patients were not adequate to perform extensive multivariate analyses.
Conclusions
Collectively, this study demonstrates substantial differences between younger and older adults with scoliosis treated surgically, with regard to clinical, radiographic, surgical, and outcomes parameters. Despite the differences between these populations, the baseline factors predictive of the best and worst outcomes were remarkably similar. Factors distinguishing between the best and worst outcomes were predominantly patient-related factors, such as obesity, depression/anxiety, smoking, and severity of pain, and not factors related to severity of deformity, operative parameters, or the occurrence of complications.
Acknowledgments
Funding for the Spinal Deformity Study Group provided by Medtronic.
Conflict of interest
The present study was performed through the Spinal Deformity Study Group, which received funding from Medtronic. Dr. Smith is a consultant for Medtronic, DePuy, and Biomet; has received honoraria for teaching from Medtronic, DePuy, Biomet, and Globus; and has received research study group support from Medtronic and DePuy. Dr. Shaffrey is a consultant for Biomet; receives royalties from Medtronic and Biomet; has received honoraria from DePuy; has received research support from NIH, US Department of Defense, AO, and NACTN; and has received fellowship support from AO. Dr. Glassman is a consultant for Medtronic; has received royalties from Medtronic; has received research funding from Medtronic and Norton Healthcare; is an employee of Norton Healthcare; and has received travel expenses from Stryker. Dr. Schwab is a shareholder in Nemaris, Inc; is a consultant for DePuy; is a consultant for Medtronic; has received research grant support from DePuy; and has received research grant support from Medtronic. Dr. Lafage is a shareholder in Nemaris, Inc. Dr. Bridwell is a consultant for DePuy.
References
- 1.Schwab F, Dubey A, Gamez L, El Fegoun AB, Hwang K, Pagala M, Farcy JP. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine. 2005;30:1082–1085. doi: 10.1097/01.brs.0000160842.43482.cd. [DOI] [PubMed] [Google Scholar]
- 2.Glassman SD, Schwab FJ, Bridwell KH, Ondra SL, Berven S, Lenke LG. The selection of operative versus nonoperative treatment in patients with adult scoliosis. Spine. 2007;32:93–97. doi: 10.1097/01.brs.0000251022.18847.77. [DOI] [PubMed] [Google Scholar]
- 3.Smith JS, Shaffrey CI, Berven S, Glassman S, Hamill C, Horton WC, Ondra S, Schwab F, Shainline M, Fu KG, Bridwell KH. Operative versus nonoperative treatment of leg pain in adults with scoliosis. A retrospective review of a prospective multicenter database with two-year follow-up. Spine. 2009;34:1693–1698. doi: 10.1097/BRS.0b013e3181ac5fcd. [DOI] [PubMed] [Google Scholar]
- 4.Smith JS, Shaffrey CI, Berven S, Glassman S, Hamill C, Horton WC, Ondra S, Schwab F, Shainline M, Fu KG, Bridwell KH. Improvement of back pain with operative and nonoperative treatment in adults with scoliosis. Neurosurgery. 2009;65:86–94. doi: 10.1227/01.NEU.0000347005.35282.6C. [DOI] [PubMed] [Google Scholar]
- 5.Smith JS, Fu KM, Urban P, Shaffrey CI. Neurological symptoms and deficits in adults with scoliosis who present to a surgical clinic: incidence and association with the choice of operative versus nonoperative management. J Neurosurg Spine. 2008;9:326–331. doi: 10.3171/SPI.2008.9.10.326. [DOI] [PubMed] [Google Scholar]
- 6.Glassman SD, Carreon LY, Shaffrey CI, Polly DW, Ondra SL, Berven SH, Bridwell KH. The costs and benefits of nonoperative management for adult scoliosis. Spine (Phila Pa 1976) 2010;35:578–582. doi: 10.1097/BRS.0b013e3181b0f2f8. [DOI] [PubMed] [Google Scholar]
- 7.Fu KM, Smith JS, Sansur CA, Shaffrey CI. Standardized measures of health status and disability and the decision to pursue operative treatment in elderly patients with degenerative scoliosis. Neurosurgery. 2010;66:42–47. doi: 10.1227/01.NEU.0000361999.29279.E6. [DOI] [PubMed] [Google Scholar]
- 8.Bridwell KH, Glassman S, Horton W, Shaffrey C, Schwab F, Zebala LP, Lenke LG, Hilton JF, Shainline M, Baldus C, Wootten D. Does treatment (nonoperative and operative) improve the two-year quality of life in patients with adult symptomatic lumbar scoliosis: a prospective multicenter evidence-based medicine study. Spine (Phila Pa 1976) 2009;34:2171–2178. doi: 10.1097/BRS.0b013e3181a8fdc8. [DOI] [PubMed] [Google Scholar]
- 9.Li G, Passias P, Kozanek M, Fu E, Wang S, Xia Q, Li G, Rand FE, Wood KB. Adult scoliosis in patients over sixty-five years of age: outcomes of operative versus nonoperative treatment at a minimum two-year follow-up. Spine (Phila Pa 1976) 2009;34:2165–2170. doi: 10.1097/BRS.0b013e3181b3ff0c. [DOI] [PubMed] [Google Scholar]
- 10.Smith JS, Shaffrey CI, Glassman SD, Berven SH, Schwab FJ, Hamill CL, Horton WC, Ondra SL, Sansur CA, Bridwell KH. Risk-benefit assessment of surgery for adult scoliosis: an analysis based on patient age. Spine. 2010;36:817–824. doi: 10.1097/BRS.0b013e3181e21783. [DOI] [PubMed] [Google Scholar]
- 11.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81:776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 12.Berven S, Deviren V, Demir-Deviren S, Hu SS, Bradford DS. Studies in the modified Scoliosis Research Society Outcomes Instrument in adults: validation, reliability, and discriminatory capacity. Spine. 2003;28:2164–2169. doi: 10.1097/01.BRS.0000084666.53553.D6. [DOI] [PubMed] [Google Scholar]
- 13.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 14.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Jt Surg Am. 2003;85-A:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 15.O’Brien MF, Kuklo TR, Blanke KM, Lenke LG. Spinal deformity study group radiographic measurement manual. Memphis: Medtronic; 2005. [Google Scholar]
- 16.Mac-Thiong JM, Transfeldt EE, Mehbod AA, Perra JH, Denis F, Garvey TA, Lonstein JE, Wu C, Dorman CW, Winter RB. Can c7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine (Phila Pa 1976) 2009;34:E519–E527. doi: 10.1097/BRS.0b013e3181a9c7ad. [DOI] [PubMed] [Google Scholar]
- 17.Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30:682–688. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 18.Aalto TJ, Malmivaara A, Kovacs F, Herno A, Alen M, Salmi L, Kroger H, Andrade J, Jimenez R, Tapaninaho A, Turunen V, Savolainen S, Airaksinen O. Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine (Phila Pa 1976) 2006;31:E648–E663. doi: 10.1097/01.brs.0000231727.88477.da. [DOI] [PubMed] [Google Scholar]
- 19.Clayson D, Mahon B, Levine DB. Preoperative personality characteristics as predictors of postoperative physical and psychological patterns in scoliosis. Spine (Phila Pa 1976) 1981;6:9–12. doi: 10.1097/00007632-198101000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Slover J, Abdu WA, Hanscom B, Weinstein JN. The impact of comorbidities on the change in short-form 36 and oswestry scores following lumbar spine surgery. Spine (Phila Pa 1976) 2006;31:1974–1980. doi: 10.1097/01.brs.0000229252.30903.b9. [DOI] [PubMed] [Google Scholar]
- 21.Peolsson A, Peolsson M. Predictive factors for long-term outcome of anterior cervical decompression and fusion: a multivariate data analysis. Eur Spine J. 2008;17:406–414. doi: 10.1007/s00586-007-0560-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trief PM, Ploutz-Snyder R, Fredrickson BE. Emotional health predicts pain and function after fusion: a prospective multicenter study. Spine (Phila Pa 1976) 2006;31:823–830. doi: 10.1097/01.brs.0000206362.03950.5b. [DOI] [PubMed] [Google Scholar]
- 23.Krebs EE, Lurie JD, Fanciullo G, Tosteson TD, Blood EA, Carey TS, Weinstein JN. Predictors of long-term opioid use among patients with painful lumbar spine conditions. J Pain. 2010;11:44–52. doi: 10.1016/j.jpain.2009.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dewing CB, Provencher MT, Riffenburgh RH, Kerr S, Manos RE. The outcomes of lumbar microdiscectomy in a young, active population: correlation by herniation type and level. Spine (Phila Pa 1976) 2008;33:33–38. doi: 10.1097/BRS.0b013e31815e3a42. [DOI] [PubMed] [Google Scholar]
- 25.Djurasovic M, Bratcher KR, Glassman SD, Dimar JR, Carreon LY. The effect of obesity on clinical outcomes after lumbar fusion. Spine (Phila Pa 1976) 2008;33:1789–1792. doi: 10.1097/BRS.0b013e31817b8f6f. [DOI] [PubMed] [Google Scholar]
- 26.Gepstein R, Shabat S, Arinzon ZH, Berner Y, Catz A, Folman Y (2004) Does obesity affect the results of lumbar decompressive spinal surgery in the elderly? Clin Orthop Relat Res 426:138–144 [DOI] [PubMed]
- 27.Andreshak TG, An HS, Hall J, Stein B. Lumbar spine surgery in the obese patient. J Spinal Disord. 1997;10:376–379. doi: 10.1097/00002517-199710000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Glassman SD, Hamill CL, Bridwell KH, Schwab FJ, Dimar JR, Lowe TG. The impact of perioperative complications on clinical outcome in adult deformity surgery. Spine (Phila Pa 1976) 2007;32:2764–2770. doi: 10.1097/BRS.0b013e31815a7644. [DOI] [PubMed] [Google Scholar]
- 29.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30:2024–2029. doi: 10.1097/01.brs.0000179086.30449.96. [DOI] [PubMed] [Google Scholar]