Abstract
Purpose
The aim of the present research is to evaluate the relationship between an X-ray-based method (i.e. the Raimondi method) and rasterstereography in the evaluation of vertebral rotation (VR) in a sample of adolescent idiopathic scoliosis (AIS) patients.
Methods
A total of 25 patients (9 males; mean age 14 ± 3 years; mean height 160.7 ± 11.9 cm; mean weight 52.4 ± 10.7 kg) were considered for the present analysis. The mean Cobb angle was 30° ± 9°. The evaluation of VR on radiographs was made using the Raimondi method regolo (Marrapese Editore—Demi S.r.1., Rome). Rasterstereography was performed by means of Formetric 4D® (Diers International GmbH, Schlangenbad, Germany). Correlations between rasterstereographic and radiographic measurement of VR were calculated, both for the whole sample and for thoracic and lumbar spinal segments considered separately, as well as for subgroups of patients with a Cobb angle <30° and ≥30° using Spearman’s correlation coefficient by rank (rs).
Results
When applied to the entire spine, measurement of VR by means of the two methods highlighted a significant correlation in the whole group (r = 0.52; p < 0.0001), as well as in the <30° Cobb (r = 0.47; p = 0.0001) and ≥30° Cobb (r = 0.42; p < 0.0001) subgroups. A significant correlation was found also when lumbar and thoracic VR were considered as separated groups (r = 0.30, p = 0.024 and r = 0.47, p = 0.002, respectively).
Conclusions
Rasterstereographic evaluation of VR shows a good correlation with the Raimondi method, thereby confirming the possibility to use this non-invasive method for deformity assessment in AIS patients.
Keywords: Rasterstereography, Vertebral rotation, Adolescent idiopathic scoliosis, Raimondi method
Introduction
Adolescent idiopathic scoliosis (AIS) is a three-dimensional deformity of the spine characterized by a deformation in the sagittal, frontal and transverse plane [1]. The gold standard for diagnosis and monitoring of changes over time in AIS is represented by measurement of the Cobb angle on the standing posteroanterior full length spine radiograph [2], which provides a measure of the curvature of the spine in the frontal plane. A key factor to be evaluated in the assessment of the gravity of AIS [3], as well as for the planning and the analysis of orthopedic and surgical procedures [4] is represented by axial vertebral rotation (VR), defined as the rotation of a vertebra around its own longitudinal axis when projected onto the transverse image plane. Several methods for assessing VR using X-rays have been developed [5–8]; among these, one of the most simple and reliable is represented by the Raimondi method [9] that uses a template (known as regolo Raimondi) to determine the degree of VR. One obvious side-effect of such instrumental assessment methods is that young AIS patients might need a great number of radiographs during their growth period [10], with a consequent exposure to relatively high doses of ionizing radiation, potentially harmful to their health [11, 12]. Alternatively, computerized methods based on MR images can be used to provide repeatable and reliable VR measurements [13]. Clinical evaluation in AIS patients assesses deformities in bending, by means of the Adams test, otherwise known as the “bend test” [14], as well as posture and asymmetries. Despite some correlations have been found between trunk deformities and radiographic measurements of VR [6, 15], the relationship between X-ray measurements and the clinical evaluation is yet under study [16].
With the need of performing an objective, reliable and safe instrumental assessment for follow-ups over time, video, photographic, and computerized imaging methods have been developed that attempted to evaluate AIS deformity using back shape evaluation, without using ionizing radiations [17, 18]. Among these techniques, rasterstereography provides a reliable method for three-dimensional back shape analysis and reconstruction of spinal deformities without radiation exposure [19]. Rasterstereography is a method for stereophotogrammetric surface measuring of the back, originally developed by Drerup and Hierholzer [19]. It has been demonstrated that rasterstereography produces reliable data in patients with conservatively and surgically treated AIS, up to a Cobb angle of 80° [20, 21], so that some authors have proposed to space out radiographs with rasterstereography in AIS long-term follow-up [22]. Since the importance of VR evaluation in AIS assessment, however, whether rasterstereography could give an accurate estimation of VR when compared with radiographs is an issue that remains to be addressed.
The aim of the present research is therefore to evaluate the relationship, if any, between an X-ray-based method (i.e. the Raimondi method) and rasterstereography in the evaluation of VR in a sample of AIS patients.
Materials and methods
Subjects of both sexes with a diagnosis of AIS who referred to our Physical Medicine and Rehabilitation department for routine clinical and radiological follow-up were considered eligible for the present research. Inclusion criteria were age between 11 and 19 years, Cobb degrees between 15° and 50° at plane radiographs, and body mass index <30 kg/m². Subjects were excluded if they had a history of previous spinal surgery, back pain at the moment of evaluation or if they were unable to ensure complete adherence to the protocol requests for the entire duration of the study. The procedure followed was in accordance with the ethical standards of our committee for human experimentations, and all patients or parents gave their signed informed consent to participation.
In order to avoid postural changes that might arise as a result of a significant lapse of time between the two exams, each patient underwent X-ray examination and evaluation by rasterstereography at the same day.
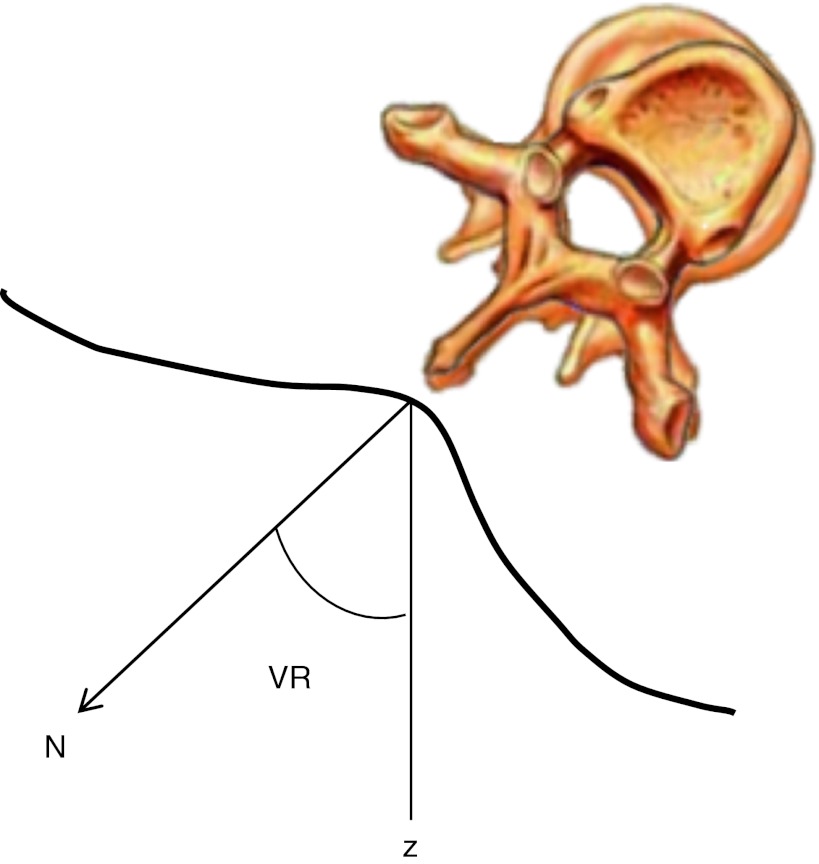
The evaluation of VR on radiographs was made using the Raimondi method regolo (Marrapese Editore—Demi S.r.1., Rome). Through the offset shadow, the widths of the vertebral body are measured in millimeters (Fig. 1). The width of each vertebra is determined on the anterior–posterior X-ray at the most narrow spot, the so-called vertebral waist. The convex-sided pedicle is marked and bisected longitudinally by a line. In order to determine the pedicle offset, the distance of this bisecting line to the convex-sided waist of the vertebral body is evaluated. The value of VR is obtained by inserting the width and the pedicle offset in the Raimondi method regolo [9]. Six physicians independently applied the Raimondi method to the posteroanterior radiographs of each patient in order to assess the VR, the mean value being used for the analysis.
Fig. 1.

Determination of vertebral rotation on plain radiographs using the Raimondi method. The vertebral waist is represented by the A–B segment and the pedicle offset by the C–B segment (see text)
Rasterstereography was performed by means of Formetric 4D® (Diers International GmbH, Schlangenbad, Germany) in which parallel white light lines are projected on the back surface of the patient by a slide projector. The three-dimensional back shape leads to a deformation of the parallel light lines, which can be detected by a camera positioned at a different angle from the projector. Anatomical landmarks are hereby automatically captured by assigning concave and convex areas to the curved light pattern [23]. With these anatomical fix points, the system is able to calculate a three-dimensional model of the human spine. The spinous process line is approximated by the so-called symmetry line of the back, and the angle of VR is estimated from the surface orientation on that line (at the same level) (Fig. 2). The symmetry line is established point by point for every transverse profile so as to minimize lateral asymmetry [18]. The patients was asked to maintain an upright posture at a fixed distance from the camera for 6 s, during which a total number of 12 scanning were performed, the mean value being used for calculations. For the purposes of the present research, we analyzed the VR obtained by Raimondi method and rasterstereography in all those vertebrae of both in thoracic and lumbar spine, in which the Raimondi methods confirmed the presence of VR.
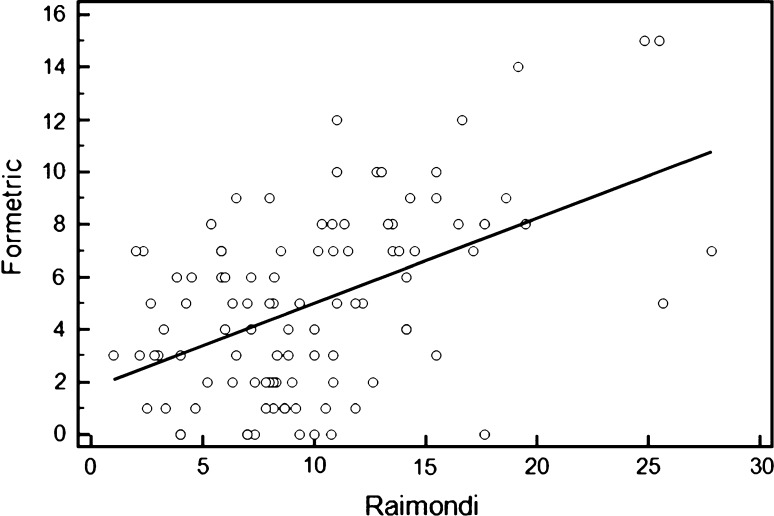
Fig. 2.
The vertebral rotation (VR) is calculated by rasterstereography as the angle between the surface orientation (N) on spinous process line (the so-called symmetry line) and the normal (z) to the frontal plane of the reference system
Statistical analysis
Statistical analysis was performed using the software Graph Pad Instat (Graph Pad Software Inc). The normal distribution was tested by Kolmogorov–Smirnov test. A one-way ANOVA was used to determine differences between VR as measured through Raimondi methods by the six evaluators, and the intra-class correlation coefficient (ICC) with 95 % confidence interval was calculated to evaluate the degree of consistency among measurements. A paired t test was used to determine differences between VR as calculated by Raimondi method and rasterstereography. Correlations between rasterstereographic and radiographic measurement of VR were calculated, both for the whole sample and for thoracic and lumbar spinal segments considered separately, using Spearman’s correlation coefficient by rank (rs). Correlations between rasterstereographic and radiographic measurement of VR were also calculated differentiating data according to two subgroups (patients <30° Cobb and patients >30° Cobb). A correlation coefficient with an absolute value of at least 0.25 and a p value <0.05 were considered statistically significant.
Results
A total of 27 patients were included. Of them, two were excluded because X-rays quality did not allow to exactly detect the parameters needed for Raimondi method calculations. A total of 25 patients (9 males; mean age 14 ± 3 years; mean height 160.7 ± 11.9 cm; mean weight 52.4 ± 10.7 kg) were therefore considered for the present analysis. The mean Cobb angle was 30° ± 9°. The mean ± SD (95 % CI) of VR as calculated by Raimondi method and rasterstereography were, respectively, 9.93 ± 5.38 (8.87–10.99) and 4.99 ± 3.50 (4.30–5.68). The paired t test revealed that the difference was statistically significant (t = 10.48; p < 0.0001). The mean ± SD (95 % CI) of thoracic and lumbar VR were, respectively, 9.18 ± 3.33 (7.80–10.55) and 10.18 ± 5.90 (8.83–11.53) with Raimondi method and 5.52 ± 3.01 (4.27–6.76) and 4.82 ± 3.65 (3.98–5.65) with rasterstereography. The mean ± SD (95 % CI) of VR for patients with a Cobb angle <30° and ≥30° were, respectively, 8.11 ± 3.38 (7.26–8.95) and 15.61 ± 7.05 (13.23–17.99) with Raimondi method and 5.5 ± 4.27 (4.43–6.57) and 8.31 ± 5.13 (6.57–10.04) with rasterstereography. An excellent consistency among the measurements obtained by the Raimondi method was found (ICC = 0.967) in line with the results presented by Weiss [9]. When applied to the entire spine, measurement of VR by means of the two methods highlighted a significant correlation in whole group (r = 0.52; p < 0.0001) (Fig. 3) as well as in the sub group of patients with a Cobb angle <30° (r = 0.47, p = 0.0001) and in the sub group of patients with a Cobb angle ≥30° (r = 0.42, p < 0.0001). A significant correlation was found also when lumbar and thoracic VR were considered as separated groups (r = 0.30; p = 0.024 and r = 0.47; p = 0.002, respectively).
Fig. 3.
Diagram plot showing the correlation of vertebral rotation values as calculated by both methods for each patient
Discussion
Monitoring VR in the follow-up of AIS patients represents a major issue, because the need to periodically evaluate this parameter should be counterbalanced by a safety profile of the technique used for such assessment. Quantitative evaluation of VR is essential to determine reference values in normal and pathological conditions and to understand the mechanisms of the progression of spinal deformities. However, quantitative evaluation of VR is difficult because of the anatomical characteristics of the observed vertebral body, and depends upon inter- and intra-operator variability.
According to our results, a good correlation exists between VR as calculated by a method based on two-dimensional detection on X-rays, the Raimondi method, and rasterstereography, a three-dimensional, radiation-free, detection technique based on back shape evaluation.
The VR values obtained by the two methods displayed a significant difference, with rasterstereographic measurements which are generally lower than radiographic ones. This could derive from the different way in VR calculation, probably because the internal structure of the deformity is mitigated by the ribs and soft tissue before being translated into surface topography changes [24], and should be considered in a clinical setting. Radiographic-based measurements represent in fact the gold standard for diagnosis and for precisely quantify the amount of VR in AIS patients [5]. Rasterstereographic measurements, however, because of their safety profile, may be effectively used for monitoring over time of clinical changes [25], thereby confirming the possibility of their use for AIS follow-ups [22]. Interestingly, two patients were excluded from the present analysis, because the low quality of X-ray images did not allow to estimate anatomical landmarks needed for VR assessment through Raimondi method. One may speculate that this could represent a limitation for X-ray-based measurements of VR.
Worthy of note, the correlation between the two methods was similar in patients with a Cobb angle <30° and ≥30°, confirming that in our group of patients presenting a Cobb angle <50° [19], the rasterstereography is a reliable method for VR evaluation.
When examined as separate groups, according to the anatomical localization of the vertebrae, the correlation between the two methods was lower for lumbar than for thoracic VR, despite being significant for both groups. The different values found in the individual segments can be referred in part to the difference of the sample: the VR of the thoracic vertebrae was measured for 14 subjects, while measurement of the lumbar vertebrae involved all 25 patients. Moreover, the different anatomy of thoracic and lumbar segments has a role in differentiating the internal VR to back shape deformation in the two groups.
Furthermore, in AIS, the lateral bending moment that increases the same VR has to be considered as well as the VR itself. Rasterstereography is based on external measurements and evaluates the VR only on the transverse plane as the angle between the direction of the spinous process and the normal to the frontal plane. Furthermore, it is influenced by supra-vertebral tissue thickness that may affect the evaluation of parameters related to the internal morphology. Instead, the Raimondi method is based on internal measurements and considers the morphological variability of the scoliotic vertebra.
Rasterstereographic measurements also provide an overall analysis of the aesthetic appearance of the body surface. For the AIS patients and their parents, the cosmetic trunk imbalance and deformity is often a major concern rather than the radiologic appearance alone [6]. From this point of view, it could be of interest for further studies to address this specific point in a population of AIS patients.
Conclusions
Rasterstereographic evaluation of VR shows a good correlation with the Raimondi method, thereby confirming the possibility to use this non-invasive method for deformity assessment in AIS patients. Rasterstereography offers the advantage of needlessly exposing the subject to ionize radiation and therefore can be performed much more frequently during both screening and follow-up. Future studies with larger samples are needed to determine if this kind of correlation also exists for VR changes over time.
Conflict of interest
None.
References
- 1.Hattori T, Sakaura H, Iwasaki M, Nagamoto Y, Yoshikawa H, Sugamoto K. In vivo three-dimensional segmental analysis of adolescent idiopathic scoliosis. Eur Spine J. 2011;20:1745–1750. doi: 10.1007/s00586-011-1869-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuklo TR, Potter BK, Schroeder TM, O’Brien MF. Comparison of manual and digital measurements in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:1240–1246. doi: 10.1097/01.brs.0000217774.13433.a7. [DOI] [PubMed] [Google Scholar]
- 3.Stokes IA. Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine (Phila Pa 1976) 1994;19:236–248. doi: 10.1097/00007632-199401001-00020. [DOI] [PubMed] [Google Scholar]
- 4.Qiao J, Zhu F, Xu L, Zhu Z, Qian B, Liu Z, Qiu Y (2012) Comparison of the aorta impingement risks between thoracolumbar/lumbar curves with different convexities in adolescent idiopathic scoliosis: a computed tomography study. Eur Spine J (epub ahead of print) [DOI] [PMC free article] [PubMed]
- 5.Vrtovec T, Pernus F, Likar B. A review of methods for quantitative evaluation of axial vertebral rotation. Eur Spine J. 2009;18:1079–1090. doi: 10.1007/s00586-009-0914-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cimić M, Kovac V, Smiljanić I, Kovac I, Cimić A, Smoljanović T. Relationship between clinical contourometric measurements and vertebral rotation in adolescent idiopathic scoliosis. Coll Antropol. 2009;33:127–133. [PubMed] [Google Scholar]
- 7.Kadoury S, Cheriet F, Beausejour M, Stokes IA, Parent S, Labelle H. A three-dimensional retrospective analysis of the evolution of spinal instrumentation for the correction of adolescent idiopathic scoliosis. Eur Spine J. 2009;18:23–37. doi: 10.1007/s00586-008-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinheiro AP, Tanure MC, Oliveira AS. Validity and reliability of a computer method to estimate vertebral axial rotation from digital radiographs. Eur Spine J. 2010;19:415–420. doi: 10.1007/s00586-009-1186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss HR. Measurement of vertebral rotation: Perdriolle versus Raimondi. Eur Spine J. 1995;4:34–38. doi: 10.1007/BF00298416. [DOI] [PubMed] [Google Scholar]
- 10.Doody MM, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE. Breast cancer mortality after diagnostic radiography: findings from the US Scoliosis Cohort Study. Spine (Phila Pa1976) 2000;25:2052–2056. doi: 10.1097/00007632-200008150-00009. [DOI] [PubMed] [Google Scholar]
- 11.Bone CM, Hsieh GH. The risk of carcinogenesis from radiographs to pediatric orthopedic patients. J Pediatr Orthop. 2000;20:251–254. [PubMed] [Google Scholar]
- 12.Berrington de Gonzales A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet. 2004;363:345–351. doi: 10.1016/S0140-6736(04)15433-0. [DOI] [PubMed] [Google Scholar]
- 13.Vrtovec T, Pernus F, Likar B. Determination of axial vertebral rotation in MR images: comparison of four manual and a computerized method. Eur Spine J. 2010;19:774–781. doi: 10.1007/s00586-010-1340-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Côté P, Kreitz BG, Cassidy JD, Dzus AK, Martel J. A study of the diagnostic accuracy and reliability of the Scoliometer and Adam’s forward bend test. Spine (Phila Pa 1976) 1998;23:796–802. doi: 10.1097/00007632-199804010-00011. [DOI] [PubMed] [Google Scholar]
- 15.Easwar TR, Hong JY, Yang JH, Suh SW, Modi HN. Does lateral vertebral translation correspond to Cobb angle and relate in the same way to axial vertebral rotation and rib hump index? A radiographic analysis on idiopathic scoliosis. Eur Spine J. 2011;20:1095–1105. doi: 10.1007/s00586-011-1702-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stokes IA, Bigalow LC, Moreland MS. Measurement of axial rotation of vertebrae in scoliosis. Spine. 1986;11:213–218. doi: 10.1097/00007632-198604000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Drerup B, Hierholzer E. Automatic localization of anatomical landmarks on the back surface and construction of a body-fixed coordinate system. J Biomech. 1987;20:961–970. doi: 10.1016/0021-9290(87)90325-3. [DOI] [PubMed] [Google Scholar]
- 18.Drerup B, Hierholzer E. Evaluation of frontal radiographs of scoliotic spines—Part I. Measurement of position and orientation of vertebrae and assessment of clinical shape parameters. J Biomech. 1992;25:1357–1362. doi: 10.1016/0021-9290(92)90291-8. [DOI] [PubMed] [Google Scholar]
- 19.Drerup B, Hierholzer E. Assessment of scoliotic deformity from back shape asymmetry using an improved mathematical model. Clin Biomech. 1996;11:376–383. doi: 10.1016/0268-0033(96)00025-3. [DOI] [PubMed] [Google Scholar]
- 20.Hackenberg L, Hierholzer E, Pötzl W, Götze C, Liljenqvist U. Rasterstereographic back shape analysis in idiopathic scoliosis after anterior correction and fusion. Clin Biomech. 2003;18:1–8. doi: 10.1016/S0268-0033(02)00165-1. [DOI] [PubMed] [Google Scholar]
- 21.Hackenberg L, Hierholzer E, Pötzl W, Götze C, Liljenqvist U. Rasterstereographic back shape analysis in idiopathic scoliosis after posterior correction and fusion. Clin Biomech. 2003;18:883–889. doi: 10.1016/S0268-0033(03)00169-4. [DOI] [PubMed] [Google Scholar]
- 22.Schulte TL, Hierholzer E, Boerke A, Lerner T, Liljenqvist U, Bullmann V, Hackenberg L. Raster stereography versus radiography in the long-term follow-up of idiopathic scoliosis. J Spinal Disord Tech. 2008;21:23–28. doi: 10.1097/BSD.0b013e318057529b. [DOI] [PubMed] [Google Scholar]
- 23.Huysmans T, Van Audekercke R, Vander Sloten J, Bruyninckx H, Van der Perre G. A three-dimensional active shape model for the detection of anatomical landmarks on the back surface. Proc Inst Mech Eng H. 2005;219:129–142. doi: 10.1243/095441105X9309. [DOI] [PubMed] [Google Scholar]
- 24.Gorton GE, 3rd, Young ML, Masso PD. Accuracy, reliability and validity of a 3d scanner for assessing torso shape in idiopathic scoliosis. Spine (Phila Pa1976) 2012;37:957–965. doi: 10.1097/BRS.0b013e31823a012e. [DOI] [PubMed] [Google Scholar]
- 25.Hackenberg L, Hierholzer E, Bullmann V, Liljenqvist U, Götze C. Rasterstereographic analysis of axial back surface rotation in standing versus forward bending posture in idiopathic scoliosis. Eur Spine J. 2006;15:1144–1149. doi: 10.1007/s00586-005-0057-9. [DOI] [PMC free article] [PubMed] [Google Scholar]