Abstract
Introduction
There is controversy regarding the appropriate proximal fusion level for adult degenerative scoliosis. Ideally, the horizontal vertebra is chosen for the upper instrumented vertebra to create a balanced spine. Fusion to T10 is recommended to prevent junctional problems at the proximal adjacent segment. The purpose of this retrospective study was to determine the optimal proximal fusion level for adult degenerative lumbar scoliosis.
Materials and Methods
Fifty-one patients with adult degenerative lumbar scoliosis (mean age 64.6 years) who underwent posterior instrumentation were analyzed after a minimum 2-year follow-up. The average number of levels fused was 5.9 segments (range 3–9) with distal fusion at L5 in 30 patients and S1 in 21 patients. The upper instrumented vertebra (UIV) ranged from T9 to L2. According to the relationship between UIV, horizontal vertebra (HV) and upper end vertebra (UEV), the patients were divided into three groups in the coronal plane: Group HV (UIV = HV or above); Group HV–UEV (UIV = between HV and UEV); and Group UEV (UIV = UEV or below). In the sagittal plane; the patients were divided into Group T9–10 (UIV = T9–10), Group T11–12 and Group L1–2.
Results
Proximal adjacent segment disease (ASD) was identified in 13 (25 %) out of 51 patients, including junctional kyphosis (n = 5), compression fractures (n = 4), progression of disc wedging (n = 2) and spinal stenosis (n = 2). Group UEV had more ASD (9 of 16 patients) compared to Group HV (2 of 21 patients) and Group HV–UEV (2 of 14 patients). It appeared that neutral vertebra could be a criterion for the selection of UIV in the coronal plane. Among the groups divided in the sagittal plane, proximal ASD was found in 47 % of 19 patients in Group L1–2, which was notably higher than 9 % in Group T9–10 and 20 % in Group T11–12.
Conclusions
Proximal adjacent segment disease developed more commonly when the proximal fusion stopped at the UEV or below in adult degenerative lumbar scoliosis. UIV must be above UEV in the coronal plane. Fusion to T11 or T12 was acceptable when UIV was above UEV, since there was no significant difference in the rate of proximal adjacent segment between fusion to T10 and fusion to T11 or T12.
Keywords: Adult spinal deformity, Adult degenerative lumbar scoliosis, Fusion level, Adjacent segment disease, Proximal junctional kyphosis
Introduction
Adult degenerative lumbar scoliosis usually has two curves at the lumbar spine, a major curve at the mid-lumbar spine and a compensatory curve at the lower lumbar spine. A thoracic curve is not commonly seen. The proximal lumbar curve has the apex at L2 or L3, and ends proximally at the thoracolumbar (TL) junction.
The TL junction is likely to be susceptible to injury or degenerative changes. In the article [1] about upper instrumented vertebra (UIV) in adult degenerative scoliosis, Suk advocated that fusion to T10 or more cephalad might be beneficial for preventing adjacent segment disease, because T10 has a true rib that can help reinforce a susceptible TL junction. On the other hand, Madjetko stated that adjacent segment problems were not prevented even if the fusion was extended to T10 because adjacent segment disease might be associated with an age-related degenerative process.
When determining the extent of fusion in the adult scoliosis, spinal alignment should be evaluated in both planes: the coronal and sagittal planes. Ideally, the fusion includes all the segments within the deformity in the coronal plane. For that reason, horizontal vertebra can be chosen for proximal fusion level [2]. Lateral bending views with the opening of the disc on the right and on the left judge the reducibility of the curves, and are helpful to decide the proximal fusion level. In the sagittal plane, fusion should improve lumbar lordosis and correct thoracolumbar kyphosis. If there is kyphosis at the thoracolumbar junction, fusion crosses this area above to the proximal thoracic level [3, 4].
There are many options regarding determination of the UIV even though horizontal vertebra is ideal in adult degenerative scoliosis. For example, when a patient has the horizontal vertebra at T9 and the end vertebra at L1, the UIV can be one of the segments between T9 and L1, assuming that surgeons try to fuse all the segments within the curve. T9 is chosen as the UIV if fusion needs to be up to the horizontal vertebra. T10 may be chosen if the UIV is thought to be above the TL transitional zone. T11 or T12 may be acceptable if the extent of fusion in scoliosis is sufficient to include the measured curve.
To our knowledge, there are no guidelines regarding the proximal fusion level for adult degenerative lumbar scoliosis. This study was done to determine the optimal proximal fusion level, as well as to evaluate the proximal adjacent segment disease after long fusion for adult degenerative lumbar scoliosis.
Methods
Fifty-one patients with adult degenerative lumbar scoliosis were reviewed retrospectively with a minimum follow-up of 2 years. The mean follow-up period was 3.4 ± 1.9 years. The mean age of the patients was 64.6 years (range 54–84). There were seven men and 44 women. The inclusion criteria were as follows: (1) age >50 years at the time of surgery, (2) no definite evidence of idiopathic adult scoliosis, and (3) long instrumentation from TL to L5 or the sacrum with a minimum of three segments of fusion.
All patients had severe spinal stenosis, and underwent laminectomy at the stenotic levels. Surgical indications in this series were radiating pain and intermittent claudication. Low back pain was rarely indicated for surgery in this study. The mean number of levels fused was 5.9 segments (range 3–9). Inter-transverse fusion with pedicle screw instrumentation was performed in all patients. Supplemental posterior lumbar interbody fusion (PLIF) was performed in 23 patients, which was done mostly at L4–5 and/or L5–S1. Initially, only posterior instrumentation without interbody fusion was performed, but gradually PLIF was added since the addition of PLIF showed better results regarding correction of lumbar lordosis and fusion rate. The distal fusion level was L5 in 30 patients and S1 in 21 patients. Nine patients had S2 screws or iliac screws inserted to reinforce the sacral screws. Patients who underwent spinal osteotomy were excluded.
The Cobb angle of the major lumbar curve, lumbar lordosis (L1–S1 angle), thoracic kyphosis (T5–12 angle), TL kyphosis (T10–L2 angle), junctional kyphotic angle, disc wedging above UIV, sagittal C7 plumb, coronal C7 plumb, pelvic tilt and pelvic incidence was measured. The junctional kyphotic angle was measured from the lower endplate of the UIV to the upper endplate of one vertebra above on the lateral radiograph. The disc wedging above UIV was measured between the line along the cephalad endplate of the UIV and the caudal endplate of the vertebra above the UIV on the AP radiograph.
The patients were evaluated concerning proximal adjacent segment diseases, including junctional kyphosis, compression fracture, spinal stenosis, and disc wedging above the UIV. Proximal junctional kyphosis was defined when the junctional kyphotic angle worsened by more than 10° compared to the preoperative value. Progression of disc wedging above the UIV was defined when the disc wedging increased by more than 10° compared to preoperative measurement on the AP radiograph.
Statistical analysis was performed using the SPSS version 11.5. Pearson Chi-square tests and Kruskal–Wallis test were used. A p value <0.05 was considered significant.
Surgical procedures
The primary indication of surgery was claudication and/or radiating leg pain in degenerative adult scoliosis. The deformity itself was not a major indication of surgery, because the Cobb angle was not severe in these series (Fig. 1). The biggest Cobb angle was 40.8° and the average Cobb angle was 21.7°. According to Grubb’s research [5], degenerative scoliosis has 28° on average compared to 52° in adult idiopathic scoliosis.
Fig. 1.
a This 72-year-old man had degenerative lumbar scoliosis, which showed larger Cobb angle and loss of lumbar lordosis. The UEV was L1, and horizontal vertebra was T10. b Fusion from T11 to the sacrum achieved greater correction of scoliosis and restoration of lumbar lordosis. T11 as upper instrumented vertebra was acceptable with the absence of proximal adjacent segment disease
Among several surgical methods, decompression alone surgery without fusion was not done due to further collapse or instability. Limited short fusion is carried out on decompressed area, and the fusion does not include entire curve. When scoliosis is not severe and a subluxation of apical vertebra is mild, limited short fusion can be selected. For a severe lateral subluxation with large Cobb angle, long fusion including entire curve was preferentially considered [6].
Both the coronal and sagittal planes were evaluated thoroughly when deciding fusion level. In the coronal plane, we preferred to include following these vertebrae in the fusion: the severe rotatory vertebra or severe tilted vertebra. The fusion was extended proximally if the junctional kyphotic angle in the sagittal plane was >10° in the sagittal plane.
With regard to the distal fusion level, fusion stopped at L5 when the L5–S1 disc looked healthy on MRI. The fusion was extended to the sacrum in the case of a pre-existing pathology at the L5–S1, such as spondylolisthesis and spinal stenosis. In the patients with significant sagittal imbalance, the fusion was also extended to the sacrum even if L5–S1 was healthy because sagittal imbalance was more likely to cause subsequent disc degeneration at the L5–S1 [7].
As for reduction of scoliosis, rod-rotation maneuver was first tried and compression of the rod was added when more correction was required. Before inserting rod, the rod was prebent to fit the desired lumbar lordosis. In situ bending technique was not usually performed, because repeated bending might cause weakening of the rod.
The interbody fusion was performed at the lower lumbar level to enhance fusion. At the level of severe disc collapse, the interbody fusion helps to achieve decompression by enlarging foramen. Furthermore, it could restore lumbar lordosis when cages with greater lordotic angle were used. Iliac screws or additional sacro-pelvic fixation were indicated in the long fusion from TL level and in the patients with sagittal imbalance. But in the beginning period of these series, the iliac screws were not available in our hospital.
Result
Relationship of UIV, UEV, HV and NV
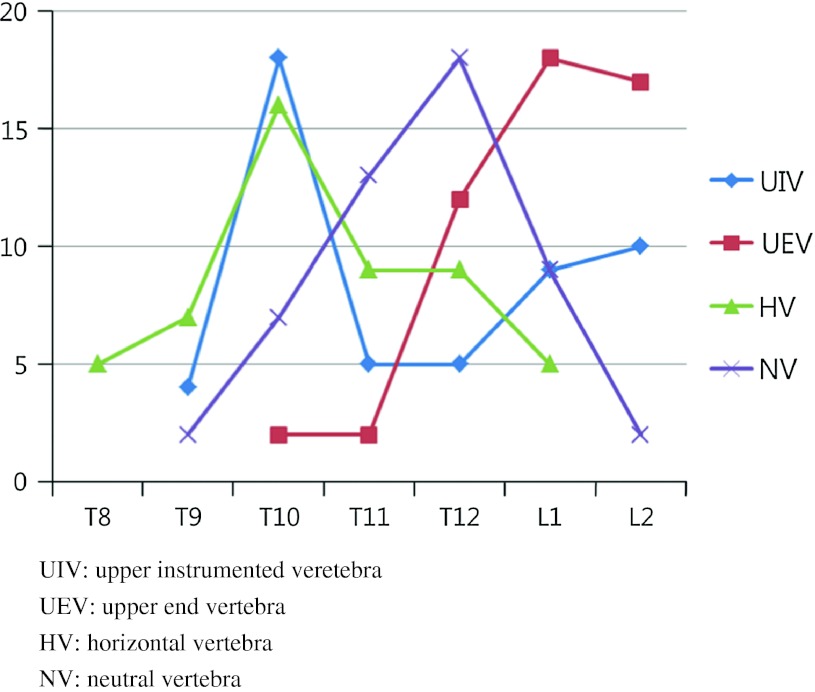
The UIV ranged from T9 to L2. The most common UIV was T10 in 18 patients and the second most common UIV was L1 in 10 patients. As degenerative adult scoliosis curve was confined to the lumbar spine in most patients, the common upper end vertebra (UEV) was L1 in 18 patients and L2 in 17 patients. The horizontal vertebra (HV) was identified from T8 to L1, which was more cephalad than UEV or NV. The neutral vertebra (NV) ranged from T10 to L2, mostly at T11 and T12 (Fig. 2).
Fig. 2.
The number of patients who had UIV, UEV, HV and NV at each level
The radiographs were evaluated in the coronal and sagittal planes. In the coronal plane, the patients were divided into three groups according to the level of UIV: Group HV when the UIV was the HV or above, Group HV–UEV when the UIV was between the HV and the UEV, and Group UEV when the UIV was the UEV or below. In the sagittal plane, the patients were also divided into three groups: Group T9–10 when the UIV was between T9 and T10, Group T11–12 when the UIV was between T11 and T12, and Group L1–2 when the UIV was between L1 and L2.
Proximal adjacent segment disease
Proximal adjacent segment diseases (ASD) developed in 13 of the 51 patients (25 %), including proximal junctional kyphosis (n = 5), compression fracture (n = 4), progression of disc wedging above UIV (n = 2), and spinal stenosis (n = 2). Other minimal radiographic changes, such as disc space narrowing or retrolisthesis, were not included in the definition of adjacent segment disease.
Patients who had proximal ASD were compared with those without ASD. Proximal ASD developed more frequently in the older patients with a statistical significance (p = 0.03). The mean age was 67.8 ± 5.7 in the ASD group and 63.5 ± 6.3 in the control group. The TL kyphosis changed more kyphotic in the ASD group at the last follow-up; 21.7° ± 10.7° compared to 5.4° ± 4.9° in the control group (p < 0.01), although it was similar before surgery in both groups. The progression of kyphosis was associated with the development of proximal junctional kyphosis (Table 1).
Table 1.
Comparisons between patients with proximal ASD and patients without ASD
| Proximal ASD group (n = 13) | Control group (n = 38) | p value | |
|---|---|---|---|
| Age (years) | 67.8 ± 5.7 | 63.5 ± 6.3 | 0.03 |
| No. of fused vertebra | 4.6 ± 1.6 | 6.3 ± 1.6 | 0.01 |
| Cobb angle (°) | |||
| Preop | 20.3 ± 7.7 | 22.8 ± 7.9 | 0.33 |
| Final | 10.3 ± 8.1 | 6.2 ± 4.8 | 0.10 |
| Change | −10.0 ± 6.9 | −16.9 ± 8.1 | <0.01 |
| Thoracolumbar kyphosis (°) | |||
| Preop | 5.9 ± 4.1 | 7.2 ± 5.5 | 0.48 |
| Final | 21.7 ± 10.7 | 5.4 ± 4.9 | <0.01 |
| Change | 15.1 ± 11.9 | −1.4 ± 6.8 | <0.01 |
| Junctional kyphotic angle (°) | |||
| Preop | 3.9 ± 4.6 | 2.8 ± 4.1 | 0.43 |
| Final | 17.9 ± 10.2 | 3.6 ± 4.5 | <0.01 |
| Change | 14.6 ± 8.6 | 1.5 ± 4.2 | <0.01 |
| Lumbar lordosis (°) | |||
| Preop | 25.9 ± 12.2 | 25.6 ± 14.8 | 0.95 |
| Final | 19.5 ± 11.8 | 23.2 ± 11.0 | 0.38 |
| Change | −6.3 ± 11.3 | −2.4 ± 11.5 | 0.28 |
| Sagittal C7 plumb (mm) | |||
| Preop | 52.5 ± 34.0 | 40.3 ± 29.4 | 0.26 |
| Final | 83.5 ± 44.3 | 63.4 ± 24.8 | 0.07 |
| Change | 27.8 ± 34.3 | 23.6 ± 35.5 | 0.98 |
| Pelvic incidence (°) | 60.6° + 9.2° | 57.5° + 9.4° | 0.18 |
| Pelvic tilt (°) | |||
| Preop | 34.2 ± 16.5 | 32.7 ± 12.4 | 0.87 |
| Final | 37.4 ± 19.2 | 35.3 ± 17.8 | 0.75 |
| Change | 2.9 ± 12.5 | 3.3 ± 11.8 | 0.95 |
| Oswesty score | |||
| Preop | 49.1 ± 19.1 | 48.4 ± 17.6 | 0.48 |
| Final | 39.8 ± 22.4 | 32.1 ± 16.5 | 0.23 |
| Change | 9.5 ± 7.8 | 15.9 ± 9.3 | 0.17 |
No significant difference was found in lumbar lordosis, C7 plumb line and pelvic tilt between ASD group and control groups. Compensatory mechanism might be associated with this finding contrary to TL kyphosis that showed significant difference between those two groups. In the sagittal imbalanced position, the body voluntarily takes action to compensate for the imbalance. At first, compensatory mechanism occurs in the un-fused mobile segments. The next step is spino-pelvic balance mechanism; posterior rotation of pelvis can make the balanced spine in the sagittal plane.
The average pelvic incidence was 57.5° + 9.4° in the control group, and 60.6° + 9.2° in the ASD group, demonstrating there was no significant difference between the two groups. The clinical outcome measured by the Oswesty disability index was less improved in the ASD group than in the control group, but there was no significant difference (p = 0.17).
Comparison of three groups in the coronal plane
In the coronal plane, 58 patients were divided into Group HV (n = 21), Group HV–UEV (n = 14), and Group UEV (n = 16). Since the HV was placed more cephalad than UEV, Group HV had a much longer fusion level than the other two groups (p < 0.01). The number of fusion level was 7.4 segments in the Group HV, 5.7 segments in the Group HV–UEV, and 4.0 segments in the Group UEV. The average age at the time of surgery was identical in the groups (p = 0.87; Table 2).
Table 2.
Comparisons of three groups in the coronal plane
| Group 1 (n = 21) (UIV = HV or above) | Group 2 (n = 14) (UIV = HV–UEV) | Group 3 (n = 16) (UIV = UEV or below) | p value | |
|---|---|---|---|---|
| Age (years) | 64.5 ± 7.9 | 64.1 ± 6.2 | 64.6 ± 6.4 | 0.87 |
| No. of fused vertebra | 7.4 ± 0.7 | 5.7 ± 1.3 | 4.0 ± 0.9 | 0.00 |
| Cobb angle (°) | ||||
| Preop | 23.8 ± 7.3 | 22.4 ± 9.3 | 19.7 ± 6.7 | 0.29 |
| Final | 4.3 ± 2.8 | 9.2 ± 6.2 | 9.3 ± 7.6 | 0.01 |
| Change | −19.9 ± 6.8 | −13.2 ± 9.0 | −10.4 ± 6.1 | 0.01 |
| Thoracic kyphosis (°) | ||||
| Preop | 13.5 ± 16.1 | 10.0 ± 14.9 | 13.8 ± 8.8 | 0.73 |
| Final | 14.6 ± 10.6 | 12.7 ± 9.5 | 13.3 ± 9.8 | 0.86 |
| Change | 1.4 ± 8.1 | 1.7 ± 14.7 | 1.0 ± 9.9 | 0.98 |
| Thoracolumbar kyphosis (°) | ||||
| Preop | 7.3 ± 5.7 | 4.0 ± 3.1 | 7.9 ± 4.9 | 0.31 |
| Final | 5.7 ± 6.9 | 6.5 ± 7.4 | 17.0 ± 11.2 | 0.01 |
| Change | −1.9 ± 8.9 | 5.4 ± 9.4 | 7.8 ± 11.7 | 0.04 |
| Junctional kyphotic angle (°) | ||||
| Preop | 3.4 ± 2.7 | 3.5 ± 3.1 | 2.6 ± 6.2 | 0.86 |
| Final | 5.6 ± 6.1 | 6.9 ± 6.9 | 10.4 ± 12.8 | 0.29 |
| Change | 2.7 ± 6.0 | 5.0 ± 5.5 | 8.0 ± 11.0 | 0.14 |
| Lumbar lordosis (°) | ||||
| Preop | 23.8 ± 14.8 | 26.9 ± 16.6 | 27.3 ± 11.2 | 0.72 |
| Final | 21.1 ± 10.2 | 20.0 ± 10.5 | 24.9 ± 13.2 | 0.53 |
| Change | −2.7 ± 12.4 | −5.9 ± 10.4 | −2.4 ± 11.6 | 0.67 |
| Disc wedging (°) | ||||
| Preop | 3.8 ± 3.2 | 6.3 ± 7.6 | 6.6 ± 4.8 | 0.19 |
| Final | 2.9 ± 2.4 | 3.5 ± 3.4 | 5.4 ± 4.1 | 0.35 |
| Change | −1.1 ± 4.2 | −2.7 ± 4.7 | −1.2 ± 3.6 | 0.62 |
Longer fusion in Group HV accomplished the greater correction of the Cobb angle than short fusion in the other groups. The correction of the Cobb angle in Group HV was 19.9° ± 6.8° compared to 13.2° ± 9.0° in Group HV–UEV and 10.4° ± 6.1° in Group UEV (p = 0.01).
Group UEV became more kyphotic at the TL junction after surgery than Groups HV and HV–UEV (p = 0.01). The TL kyphosis changed from 7.9° ± 4.9° preoperatively to 17.0° ± 11.2° at the last visit in Group UEV. In the other two groups, it was similar between pre and postsurgery. The junctional kyphotic angle also had a similar finding that Group UEV showed more kyphotic, but there was no statistical difference (p = 0.29).
The incidence of proximal ASD was much higher in Group UEV, which was 56 %, compared to Group HV (9 %) and Group HV–UEV (14 %). Group UEV identified 9 patients of proximal ASD in 16 patients. Of the five patients with proximal junctional kyphosis, two patients underwent an extension of fusion to T10. Compression fracture was seen in two patients. One of them required extension of fusion for the compression fracture at T12. The progression of disc wedging above UIV >10° was observed in one patient, who was managed conservatively. A patient with spinal stenosis improved with conservative treatment.
Group HV had two complications, compression fracture and spinal stenosis. These two patients were managed conservatively. Group HV–UEV also had two complications, compression fracture and progression of the disc wedging. For the compression fracture at T12 in Group HV-UEV, extension of instrumentation to T10 was performed. The compression fracture can be managed with kyphoplasty if collapse of vertebral body worsens without the evidence of union before extension of instrumentation is considered.
We evaluated the incidence of proximal ASD by the criterion of neutral vertebra. Based on neutral vertebra, the patients were divided into two groups: patients who had fusion to NV or above (37 patients) and patients who had fusion below NV (14 patients). The incidence of proximal ASD was higher in the patients with the fusion below NV compared to the fusion to NV or above, which was 64 % (9 of 14 patients) and 8 % (3 of 37 patients), respectively. This finding indicated that the fusion to NV or above could achieve less development of proximal ASD.
Comparison of three groups in the sagittal plane
When the proximal fusion level is determined, junctional kyphosis and thoracolumbar kyphosis were evaluated in the sagittal plane. Junctional kyphosis was included in the fusion and extended fusion proximally. If thoracolumbar kyphosis was greater than 10°, the fusion was appropriate to be T10, because it is more likely to develop junctional kyphosis at the transitional thoracolumbar spine.
In the sagittal plane, the patients were divided into Group T9–T10 (n = 22), Group T11–T12 (n = 10), and Group L1–L2 (n = 19). The TL kyphosis changed more kyphotic at the last visit in Group L1–2 than in the other two groups (p = 0.02). In Group L1–2, the TL kyphosis changed from 7.4° ± 4.8° before surgery to 14.2° ± 11° at the last visit. Unlike Group L1–2, Group T9–10 and Group T11–12 showed 5.9° ± 6.1° and 8.4° ± 10.4° at the last visit, respectively. This finding indicated that stopping fusion at L1 or L2 worsened kyphosis at the TL junction (Table 3).
Table 3.
Comparisons of three groups in the sagittal plane
| Group T9–10 (n = 22) (UIV = T9 or 10) | Group T11–12 (n = 10) (UIV = T11 or 12) | Group L1–2 (n = 19) (UIV = L1 or 2) | p value | |
|---|---|---|---|---|
| Age (years) | 64.6 ± 7.9 | 63.3 ± 6.0 | 65.3 ± 4.5 | 0.73 |
| No. of fused vertebra | 7.5 ± 0.6 | 5.9 ± 0.7 | 3.9 ± 0.6 | 0.00 |
| Thoracic kyphosis (°) | ||||
| Preop | 11.6 ± 16.9 | 11.8 ± 13.7 | 15.0 ± 8.7 | 0.67 |
| Final | 14.6 ± 10.7 | 12.4 ± 10.1 | 13.2 ± 9.0 | 0.83 |
| Change | 3.3 ± 10.9 | 1.7 ± 11.7 | −1.8 ± 9.2 | 0.39 |
| Thoracolumbar kyphosis (°) | ||||
| Preop | 6.7 ± 5.8 | 6.0 ± 3.9 | 7.4 ± 4.8 | 0.87 |
| Final | 5.9 ± 6.1 | 8.4 ± 10.4 | 14.2 ± 11.1 | 0.02 |
| Change | −1.0 ± 9.2 | 3.5 ± 10.9 | 6.8 ± 11.5 | 0.12 |
| Junctional kyphotic angle (°) | ||||
| Preop | 3.3 ± 2.7 | 5.0 ± 3.9 | 2.2 ± 5.7 | 0.44 |
| Final | 5.9 ± 6.1 | 9.7 ± 8.4 | 7.8 ± 10.6 | 0.34 |
| Change | 3.1 ± 6.1 | 5.6 ± 8.2 | 6.0 ± 9.6 | 0.29 |
| Lumbar lordosis (°) | ||||
| Preop | 22.0 ± 15.3 | 27.2 ± 12.7 | 29.4 ± 12.7 | 0.24 |
| Final | 20.4 ± 10.2 | 25.3 ± 9.7 | 23.2 ± 13.1 | 0.51 |
| Change | −1.6 ± 12.5 | −2.0 ± 11.2 | −6.2 ± 10.5 | 0.42 |
| Sagittal C7 plumb (mm) | ||||
| Preop | 59.6 ± 33.2 | 46.5 ± 34.5 | 38.9 ± 30.2 | 0.15 |
| Final | 99.1 ± 43.8 | 58.7 ± 29.6 | 58.5 ± 26.0 | 0.01 |
| Change | 39.5 ± 31.9 | 12.2 ± 36.2 | 19.3 ± 9.2 | 0.06 |
| Pelvic incidence (°) | 60.7° + 9.6° | 59.4° + 9.1° | 57.2° + 8.9° | 0.25 |
Proximal ASD was identified in 9 patients in Group L1–L2. The incidence was 47 %, which was much higher compared to 9 % in Group T9–10 and 20 % in Group T11–12. Both Group T9–10 and Group T11–12 had 2 ASD.
The sagittal C7 plumb deteriorated into positive decompensation after surgery in all three groups. It was 59.6 ± 33.2 mm before surgery and worsened to 99.1 ± 43.8 mm at the last visit in Group T9–10, even though the least incidence of proximal ASD was found in this group. The sagittal decompensation resulted from multiple causes, such as insufficient correction of lumbar lordosis and loosening of fixation. Pseudarthrosis or fixation failure at the distal segment might be the most significant risk factor of sagittal decompensation, because the moment arm is longer at the distal level than at the proximal level. The long instrumentation applies biomechanical stress at the distal fixation, which leads to loosening of screws. Proximal ASD was less likely to cause the sagittal decompensation.
Pelvic incidence should be considered prior to the correction of spinal deformity [8]. Some authors reported that sagittal decompensation developed more frequently in those patients with higher pelvic incidence as opposed to those patients with lower pelvic incidence [9]. Patients with high pelvic incidence need more correction of lumbar lordosis to achieve sagittal balance. Restoration of lumbar lordosis was crucial to make and maintain balanced spine. In this series, sagittal C7 plumb was relatively balanced before surgery, but after surgery it was worsened. Sagittal decompensation was closely related to insufficient correction of lumbar lordosis. It resulted from implant failure or pseudarthrosis as well. The average pelvic incidence was 60.7° + 9.6° in Group T9–10, 59.4° + 9.1° in Group T10–11, and 57.2° + 8.9° in Group L1–2, which was not statistically different among the three groups.
Discussion
Inappropriate fusion level or insufficient correction of coronal and sagittal curve in the scoliosis results in progression of curve or decompensation. If the fusion stops within the deformity, which does not include the entire curve, degenerative changes are more likely to progress in the remaining curve, ultimately leading to adjacent segment diseases.
The primary indication of surgery for adult degenerative scoliosis is to improve radiculopathy or claudication caused by spinal stenosis, requiring decompressive surgery. Correction of deformity is to obtain sagittal balance and to avoid adjacent segment disease, which is also beneficial to improve back pain and to decompress nerve root at the concave side [10]. Degenerative lumbar scoliosis develops in older patients, accompanied by multiple medical co-morbidities. Old age and medical co-morbidity make surgeons choose shorter fusion if possible. Longer fusion causes more blood loss, which is associated with perioperative complications. Cho et al. [11] reported that risk factors of complications in posterior lumbar fusion for degenerative lumbar scoliosis were excessive perioperative bleeding and longer fusion level.
There are several surgical options regarding the extent of fusion in adult degenerative lumbar scoliosis [12–14]. Short fusion in limited segments within the deformity might be used for scoliosis with a smaller Cobb angle and well-balanced spine. Long fusion, which fuses all the measured scoliotic curves, is performed for severe rotatory subluxation or sagittal imbalance [6].
One of horizontal, neutral or stable vertebra may be a criterion for determining proximal fusion level in the coronal plane. If the fusion goes up to the horizontal vertebra, adjacent segment disease is less likely to occur. In this series, the most common horizontal vertebra was T10 in 16 patients, and the most common neutral vertebra was T12 in 13 patients. Horizontal vertebra is more cephalad than neutral vertebra.
Kim et al. [15] stated that proximal fusion level at the stable and neutral vertebrae may be satisfactory in long adult spinal fusion. The stable vertebra, however, was not an appropriate criterion in patients who have coronal decompensation. The coronal vertical axis was easily deviated by more than 2 cm from the midline when the lateral subluxation was severe at the mid-lumbar spine. In this series, 13 of 51 patients were seen coronal decompensation, having stable vertebra at the mid-lumbar level (Fig. 3).
Fig. 3.
The relationship of HV, NV, and EV. Stable vertebra was not identified in the patient with severe lateral subluxation. In this patient, the proximal fusion level was chosen at T11, which was neutral vertebra. HV horizontal vertebra, NV neutral vertebra, EV end vertebra
Instead of stable vertebrae, neutral vertebra was found to be a useful criterion. Neutral vertebra was mostly found at T11 or T12. Thirty-seven patients had fusion to NV or above, and 14 patients had fusion below NV. Proximal ASD developed in 8 % in the patients with the fusion was NV or above, comparing 64 % incidence of ASD in the patients with fusion below NV. This finding suggested that neutral vertebra might be a criterion to choose UIV in the adult degenerative lumbar scoliosis.
In the coronal plane, the proximal ASD occurred in 10 % of patients with the proximal fusion to HV, and in 14 % of patients with the fusion between HV and UEV. Conversely, proximal ASD was found in 56 % of patients who had fusion to UEV or below. Considering the incidence of proximal ASD, the proximal fusion level should be above UEV.
Fusion to T10 has been known to be more reliable compared to fusion to T11 or L1 since the rib stabilizes the thoracolumbar junction. This study also showed similar results with previous studies. The incidence of proximal ASD was highest in Group L1–2. It was 47 %, compared to fusion to T9–10 (9 %) and T11 or T12 (20 %). However, fusion to T10 was likely to develop perioperative complications. The longer level of fusion and blood loss were proven to be risk factors of perioperative complications. Therefore, fusion to T11 or 12 can be selected instead of T10 when considering risk and benefit of long instrumentation. Fusion to T11 or T12 in the sagittal plane was suggested as an alternative selection when the UIV is above the UEV in the coronal plane.
Several studies have focused on proximal junctional kyphosis after fusion in a scoliotic deformity [16, 17]. Lee et al. [18] reported 46 % of proximal junctional kyphosis after posterior instrumentation and fusion for adolescent idiopathic scoliosis. Yang et al. [4] performed short posterior fusion for TL idiopathic scoliosis in 14 patients, of whom proximal junctional kyphosis occurred in 43 %. They recommended short posterior spinal fusion only if the focal kyphotic angle at the lower thoracic region was <10°. It is important that the absence of junctional kyphosis should be verified before surgery. The segments with a junctional kyphosis should be included in the fusion, especially at the TL level.
Proximal junctional kyphosis was not related directly to the clinical significance in the short-term despite being a major complication. This study showed that patients with ASD were likely to have poor Oswesty scores at the last follow-up, but there was no statistical significance.
The correction of lumbar lordosis was not satisfactory in this series, since only posterior instrumentation was performed in 28 of 51 patients. It appeared that posterior instrumentation was not appropriate to maintain the restored lordosis without anterior column support even though rod bending was done to the desired lordosis. Loss of correction commonly occurred in the elderly and osteoporotic patients. Anterior column support using wedge shaped cage with great lordotic angle can be a tool of restoration of lumbar lordosis. Spinal osteotomy is another solution to make more lordosis in adult deformity.
Conclusions
Adjacent segment disease is one of the major complications after long instrumentation in adult degenerative lumbar scoliosis patients. This study demonstrated proximal adjacent segment disease occurred more common when the fusion stopped at the UEV or below in the coronal plane. Therefore, fusion should be above the UEV. Neutral vertebra was found to be a criterion for the selection of upper instrumented vertebra.
Stopping fusion at L1 or L2 showed the highest incidence of proximal adjacent segment, whereas fusion to T10 or above showed the least incidence of it. Fusion to T11 or T12 was found to be acceptable as upper instrumented vertebra for adult degenerative scoliosis since there was no significant difference in the rate of proximal adjacent segment between fusion to T10 and fusion to T11 or T12.
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Shufflebarger H, Suk SI, Mardjetko S. Debate: determining the upper instrumented vertebra in the management of adult degenerative scoliosis: stopping at T10 versus L1. Spine. 2006;31((19S)):S185–S194. doi: 10.1097/01.brs.0000232811.08673.03. [DOI] [PubMed] [Google Scholar]
- 2.Simmons ED. Surgical treatment of patients with lumbar spinal stenosis with associated scoliosis. Clin Orthop Relat Res. 2001;384:45–53. doi: 10.1097/00003086-200103000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Mok JM, Hu SS. Surgical strategies and choosing levels for spinal deformity: how high, how low, front and back. Neurosurg Clin N Am. 2007;18(2):329–337. doi: 10.1016/j.nec.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Yang SH, Chen PQ. Proximal kyphosis after short posterior fusion for thoracolumbar scoliosis. Clin Orthop Relat Res. 2003;411:152–158. doi: 10.1097/01.blo.0000069885.72909.bb. [DOI] [PubMed] [Google Scholar]
- 5.Grubb SA, Lipscomb HJ, Suh PB. Results of surgical treatment of painful adult scoliosis. Spine. 1994;19(14):1619–1627. doi: 10.1097/00007632-199407001-00011. [DOI] [PubMed] [Google Scholar]
- 6.Cho KJ, Suk SI, Park SR, et al. Short fusion versus long fusion for degenerative lumbar scoliosis. Eur Spine J. 2008;17(5):650–656. doi: 10.1007/s00586-008-0615-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cho KJ, Suk SI, Park SR, et al. Arthrodesis to L5 versus S1 in long instrumentation and fusion for degenerative lumbar scoliosis. Eur Spine J. 2009;18(4):531–537. doi: 10.1007/s00586-009-0883-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le Huec JC, Aunoble S, Philippe L, Nicolas P. Pelvic parameters: origin and significance. Eur Spine J. 2011;20(Supp 5):S564–S571. doi: 10.1007/s00586-011-1940-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cho KJ, Suk SI, Park SR, et al. Risk factors of sagittal decompensation after long posterior instrumentation and fusion for degenerative lumbar scoliosis. Spine. 2010;35(17):1595–1601. doi: 10.1097/BRS.0b013e3181bdad89. [DOI] [PubMed] [Google Scholar]
- 10.de Vries AA, Mullender MG, Pluymakers WJ, et al. Spinal decompensation in degenerative lumbar scoliosis. Eur Spine J. 2010;19(9):1540–1544. doi: 10.1007/s00586-010-1368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cho KJ, Suk SI, Park SR, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine. 2007;32(20):2232–2237. doi: 10.1097/BRS.0b013e31814b2d3c. [DOI] [PubMed] [Google Scholar]
- 12.Aebi M. The adult scoliosis. Eur Spine J. 2005;14(10):925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 13.Transfeldt EE, Topp M, Mehbod AA, Winter RB. Surgical outcomes of decompression, decompression with limited fusion, and decompression with full curve fusion for degenerative scoliosis with radiculopathy. Spine. 2010;35(20):1872–1875. doi: 10.1097/BRS.0b013e3181ce63a2. [DOI] [PubMed] [Google Scholar]
- 14.Gupta MC. Degenerative scoliosis. Options for surgical management. Orthop Clin North Am. 2003;34(2):269–279. doi: 10.1016/S0030-5898(03)00029-4. [DOI] [PubMed] [Google Scholar]
- 15.Kim YJ, Bridwell KH, Lenke LG, Rhim SC, Kim YW, et al. Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine. 2007;32(24):2653–2661. doi: 10.1097/BRS.0b013e31815a5a9d. [DOI] [PubMed] [Google Scholar]
- 16.Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine. 2005;30(14):1643–1649. doi: 10.1097/01.brs.0000169451.76359.49. [DOI] [PubMed] [Google Scholar]
- 17.Kim YJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine. 2008;33(20):2179–2184. doi: 10.1097/BRS.0b013e31817c0428. [DOI] [PubMed] [Google Scholar]
- 18.Lee GA, Betz RR, Clements DH, Huss GK. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine. 1999;24(8):795–799. doi: 10.1097/00007632-199904150-00011. [DOI] [PubMed] [Google Scholar]