Summary Statement
Symptomatic knee osteoarthritis (OA) is a prevalent chronic degenerative disease that is associated with impaired quality of life and physical functioning. Although there is no cure for knee OA, regular exercise participation consistently results in improvements in quality of life, physical function, and knee OA symptoms. Findings from contemporary randomized controlled trials also demonstrate that lifestyle interventions involving modification of exercise and dietary behaviors yield superior improvements in relevant quality of life outcomes relative to either intervention alone.
Keywords: Physical activity, arthritis, lifestyle intervention, well-being, obesity
Knee osteoarthritis (OA) is a chronic, progressive degenerative disease that increases in prevalence with advancing age (6). The joint damage and symptoms (i.e., pain, stiffness, and fatigue) accompanying symptomatic knee OA result in activity restriction, muscle atrophy, reduced quality of life, and difficulty in performance of functional tasks involving ambulation and transfer. Inactivity, secondary to the symptoms of knee OA, results in muscular weakness and physical deconditioning that exacerbates pain symptoms and accelerates the progression towards physical disability. Thus, knee OA is a prevalent chronic condition that acts as one of the primary causes of activity restriction and functional limitations among older adults (4, 14).
There is no cure for knee OA and traditional treatments (e.g., pharmacologic and surgical interventions) have mixed efficacy and are linked with adverse long-term side effects. Consequently, current approaches to treatment have increasingly focused upon lifestyle modification designed to help manage OA symptoms. There is considerable evidence that exercise is an efficacious lifestyle intervention for knee OA patients (8, 16). Specifically, exercise consistently results in modest, yet meaningful improvements in pain symptoms, physical function, and quality of life in knee OA patients. Consistent with these findings, exercise is now advocated as an essential portion of the medical management of knee OA in contemporary treatment guidelines (1).
Being overweight or obese can exacerbate the pain symptoms and functional limitations accompanying OA (19). Thus, although increased physical activity participation is central to improving quality of life, emerging evidence suggests that the combination of exercise and dietary weight loss approaches produces superior improvements in several key quality of life outcomes among OA patients who are overweight or obese relative to exercise alone (17, 18). Many knee OA patients also experience considerable obstacles to successfully adopting and maintaining physical activity/exercise participation as part of behavioral disease management efforts. Consequently, the purpose of the present article is to provide an overview of role of physical activity and weight loss for enhancing quality of life in knee OA patients. Behavioral and programmatic considerations that are integral to optimizing the beneficial effects of exercise upon quality of life outcomes in knee OA are also highlighted.
Body Weight in the Development of Knee OA
Although the etiology of knee OA is multifactorial, being overweight or obese is recognized as being a primary independent risk factor for developing knee OA. Significant relationships between even small increases in body mass index and prevalence of knee OA have been consistently documented (15). Findings from the Framingham Heart study and the first National Health and Nutrition Examination Survey (NHANES I) demonstrated that individuals with the highest body weights had the greatest risk of developing knee OA (3, 7). Prospective studies also revealed that individuals who become overweight or obese have significantly greater risk of developing knee OA and that successful weight loss substantially reduces the risk of knee OA (7, 20). It is important to note, that while being overweight or obese is consistently related to increased risk of developing knee OA, the role of body weight in the progression of diagnosed OA is less clear (8, 9). However, recent findings suggest the link between body weight and OA severity may be related to the type and degree of joint malalignment (25). The link between body weight and the risk and severity of knee OA highlights the importance of changes in lifestyle, including increased physical activity and modified dietary intake, as key components of successful knee OA management approaches.
Importance of Exercise and Weight Management
In the absence of a cure for OA, current treatment approaches are increasingly focusing upon lifestyle interventions that enhance individual’s functional health and quality of life. Findings from several randomized controlled trials of patients with knee OA demonstrate that exercise results in modest, yet significant improvements in quality of life (8, 16). Recent evidence also supports the utility of combining exercise with dietary modification in the treatment of overweight or obese knee OA patients. For example, findings from the Arthritis, Diet, and Activity Promotion Trial (ADAPT), a single blind randomized controlled trial of 316 older, overweight or obese knee OA patients, revealed that in those receiving a combined exercise and dietary weight loss intervention experienced greater weight loss and superior improvements in physical function and pain symptoms compared to patients receiving exercise alone, dietary weight loss alone, or healthy lifestyle education (18). The combined intervention resulted in a weight loss of approximately 6% at 18 month follow-up suggesting that achieving even a modest amount of weight loss through the concomitant modification of exercise and dietary behavior results in a synergistic effect that is superior to implementation of either intervention alone. Miller et al (17) subsequently demonstrated that a more intensive weight loss (10% of body weight) intervention resulted in significantly greater improvements in quality of life when compared to a weight stable control group.
Although it is possible that promoting greater amounts of weight loss (>10% of body weight) through appropriate modification of exercise and dietary behaviors could be of even greater benefit to quality of life for OA patients, neither the optimal amount of weight loss nor the dose-response relationship between weight loss and improvements in quality of life outcomes have been clearly defined for overweight or obese knee OA patients. It is also important to recognize that behavioral weight loss interventions primarily addressing modification of exercise and dietary behavior typically result in the modest amounts (e.g., 5–10%) of weight loss (8, 17, 18). Consequently, the feasibility and efficacy of promoting or sustaining greater amounts of weight loss for OA patients is also presently unknown.
Physical Activity Considerations
Exercise consistently yields meaningful improvements in pain, physical function, and other relevant aspects of quality of life for knee OA patients (8, 16). It is also well established that elevating energy expenditure through increased exercise and/or physical activity levels is an integral component of successful behavioral weight management approaches (8, 12, 22). Therefore, increasing physical activity levels by engaging in structured exercise, purposeful activity, and mobility-related activities of daily living is an essential aspect of the successful behavioral management of OA symptoms.
Despite the strong support for the beneficence of exercise for OA patients, knowledge of the most appropriate types or amounts of physical activity/exercise for knee OA patients remains relatively limited. Muscle atrophy and weakness contribute to the functional limitations and pain commonly observed in patients with knee OA and findings from several randomized controlled trials reveal the benefits of lower extremity strength training for offsetting these impairments and enhancing quality of life (7, 15, 17, 20). Impairments in aerobic endurance and cardiorespiratory fitness are also important determinants of functional capacity and one’s ability to successfully engage in mobility-related activities of daily living. Thus, with regard to the most effective type of exercise, exercise programs designed to enhance quality of life in OA patients should target impairments in muscular and cardiorespiratory fitness through the inclusion of both aerobic and strength training components.
In addition to encouraging OA patients to engage in both aerobic and strength training exercises, the amount of activity patients should be prescribed also warrants careful consideration. Given that increased energy expenditure aids in weight management efforts and promotes increased fitness gains, titrating the exercise prescription towards higher volumes of physical activity participation could be viewed as sensible approach that could yield the most favorable changes in quality of life outcomes. Nonetheless, evidence from the Fitness and Arthritis in Seniors Trials (FAST) demonstrating that higher volumes of exercise were not the most efficacious approach for individuals with OA suggests a more cautious prescription approach is warranted (21). Specifically, the most physically active FAST participants, who were accruing over 40 minutes of moderate intensity walking per day, reported pain and functional limitations that did not differ significantly from non-exercising control participants. Conversely, participants engaging in approximately 30 min per day of moderate intensity walking exhibited the most favorable improvements in pain and physical function. These results suggest that prescribing generally modest volumes (e.g., 30 min) of daily moderate intensity physical activity, essentially levels of physical activity comparable to those recommended in national physical activity guidelines for general health promotion and disease prevention, may be preferable for enhancing quality of life in OA patients.
Sedentary and inactive knee OA patients are characterized by marked variability in exercise tolerances and preferences. Thus, from a programming perspective, no single exercise prescription will result in optimal improvements in fitness and quality of life outcomes for all patients. Flexibility in programming and personalization of the exercise prescription is essential to successfully promoting physical activity and improving quality of life. Nonetheless, general physical activity guidelines, based on national guidelines (2) and approaches implemented in prior exercise interventions targeting OA patients, have been developed and warrant consideration (8, 13, 16). Central aspects of this prescription approach are to encourage patients to begin moderate intensity walking four to five times per week. Intensity is not as critical as total energy expenditure when promoting exercise in weight management efforts. Additionally, many of the patients that progressed to reaching 30 or more minutes of moderate intensity walking in our prior exercise interventions achieved this volume of activity through participation in multiple, intermittent bouts of walking lasting anywhere from 5 to 20 min in duration. Accordingly, one reasonable approach is to encourage patient to accrue 10–15 minutes of moderate intensity walking four to five times a week initially and gradually introduce additional multiple intermittent sessions that progress towards an overall volume of 30–40 min per day.
Strength training exercises focusing on the muscles of the lower body should be performed two to three times per week using a weight that allows participants to complete 8–12 repetitions without experiencing excessive knee pain or fatigue. Performing strength training using traditional resistance exercise machines, dynabands, dumbbells, or ankle weights have all been found to be feasible and effective ways to implement this training component (7, 8, 12, 17).
Behavioral Considerations in Lifestyle Changes for Knee OA Patients
Being overweight or obese can exacerbate the pain and functional limitations that commonly accompany symptomatic OA. As noted previously, even modest weight loss results in meaningful improvements in various OA outcomes and provides strong support for the utility of implementing lifestyle exercise and dietary interventions in the treatment of knee OA patients (8, 17, 18). Despite the potential benefits of weight loss through exercise and dietary interventions, many OA patients experience considerable behavioral challenges when attempting to change lifestyle physical activity and dietary behaviors. The knee pain, fatigue, and a lack of mobility and physical activity-related self efficacy are meaningful barriers to patients’ motivation for adopting and maintaining recommended lifestyle changes. Evidence from several recent studies suggests attention to some key behavioral considerations may enhance the efficacy of lifestyle intervention approaches for knee OA patients (8–12, 21, 22).
Shaping realistic expectations about the process and outcomes accompanying the adoption of exercise and dietary weight management strategies is a key behavioral concern. Many overweight individuals adopt lifestyle interventions expecting to lose three or four times the amount of weight commonly observed with behavioral weight management programs. Failure to achieve unrealistic expectations can undermine confidence and motivation to continue lifestyle behavior change efforts (9, 13). Modifying diet and exercise habits requires considerable effort and vigilance to maintain. Counseling individuals about the amount of weight loss typically achieved through exercise and dietary modification, the amount of weight loss associated with improved quality of life, and time and effort required to achieve these outcomes may assist individuals in setting realistic process and outcome goals. Additionally, moderate intensity walking and strength training sessions can be accompanied by modest, transient increases in knee pain and fatigue in knee OA patients (9, 10). Individuals should be informed of this possibility to set appropriate expectations regarding normal exertional and symptom responses to acute exercise participation. Patients should also be encouraged to pace themselves to prevent excessive physical discomfort, rest when experiencing pain or fatigue, and integrate sensible, gradual progression when increasing intensity or duration. As noted previously, many knee OA patients reach targeted volumes of physical activity by accruing activity through multiple, intermittent bouts of activity. Teaching participants to actively monitor multiple factors during exercise such as perceived exertion, pain, and fatigue levels can foster appropriate activity pacing and, in turn, facilitate physical activity maintenance and weight loss efforts.
Emerging findings also reveal that changes in OA patients’ pain intensity and satisfaction with their physical function are integral determinants of the quality of life benefits of lifestyle interventions (see Figure 1). That is, individuals reporting the greatest improvement in their pain symptoms, satisfaction with physical functioning, and mobility-related self-efficacy experience the most favorable quality of life changes (24). Systematically monitoring changes in these outcomes during the course of exercise and weight loss programs can provide both participants and health and fitness professionals with important feedback about intervention efficacy and patient responsivity to the behavior change effort.
Figure 1.
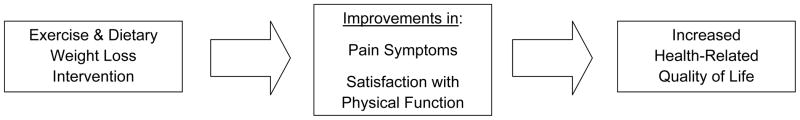
Pain and Satisfaction with Function as Mediators of the Effects of Lifestyle Exercise and Dietary Interventions on Quality of Life
In addition to the challenges posed by disease symptoms, many sedentary OA patients also struggle to cope with more common barriers to physical activity and dietary behavior change. Maintaining regular exercise participation is a critical determinant of long term quality of life benefits for OA patients. Indeed, poor post-intervention exercise adherence rates have been implicated in the deterioration of pain and physical function benefits frequently observed following the end of structured exercise interventions (8, 21). Providing participants with training in basic behavioral skills necessary to overcome barriers to physical activity and independently self-regulate physical activity and dietary behaviors can promote better long-term maintenance of lifestyle behavior change. A new approach, the group-mediated cognitive behavioral (GMCB) physical activity intervention, has recently yielded significant improvements in physical activity, physical function, and quality of life in large randomized controlled trials targeting older adults with chronic disease or mobility disability (22, 23). We applied this approach with knee OA patients in a recently completed pilot study and observed that the GMCB approach resulted in superior physical activity participation and more favorable changes in quality of life relative to a traditional center-based exercise therapy intervention (11, 12). Consequently, integrating group-based self-regulatory skills counseling with lifestyle exercise and dietary interventions is one intervention approach that shows considerable promise for facilitating behavior change maintenance among knee OA patients. Examples of the basic behavioral skills addressed in the GMCB intervention we implemented in our recent randomized controlled trial in sedentary, knee OA patients are provided in Table 1.
Table 1.
Recommended Basic Behavioral Strategies to Promote Physical Activity in Knee OA Patients
| Provide patients counseling, instruction, and practice in: |
| Self-Monitoring: monitoring/tracking of physical activity and the intensity, effort sense, and pain experienced during activity |
| Goal-Setting: setting realistic, yet challenging, short term and long-term behavioral and outcome-related goals |
| Barrier Problem-Solving: using the group setting to identify, evaluate, and implement peer-initiated solutions to overcome common and disease-related barriers that impede regular physical activity participation |
| Independent Activity Planning: gradually phased increased in responsibility for planning and carrying out independent exercise/physical activity sessions |
In summary, inactivity compounds the adverse effects of knee OA on quality of life and functional health. Exercise results in modest, yet clinically meaningful improvements in pain symptoms, physical function, and quality of life. Exercise is a beneficial lifestyle intervention for OA patients that is now advocated as an important aspect of the medical management of knee OA. However, for overweight or obese individuals with OA, combining exercise and dietary modification that results weight loss is associated with superior improvements in quality of life relative to either intervention alone. Individuals with knee OA face numerous behavioral challenges in adopting and maintaining physical activity. However, recent evidence indicates that attention to key behavior considerations can aid in fostering physical activity maintenance and augment the beneficial effect of lifestyle interventions on quality of life
Condensed Version and Bottom Line
Exercise consistently results in improvements in quality of life for knee OA patients. Although exercise represents a promising lifestyle intervention, recent findings demonstrate that combining exercise and dietary weight loss is superior to implementing either intervention alone for overweight or obese individuals with knee OA. Many OA patients struggle with the challenge of adopting and maintaining exercise and dietary behavior change. Integrating key behavioral strategies with exercise and weight management programming can aid in facilitating successful behavior change and augmenting the effects of these approaches on quality of life outcomes.
Learning Objectives.
To develop a more comprehensive understanding of the quality of life benefits of exercise and key behavioral considerations for improving physical activity participation and weight management efforts in knee osteoarthritis patients.
Biography

Brian C. Focht, Ph.D., FACSM, CSCS is an Associate Professor in Kinesiology at The Ohio State University. His research focuses upon the role of exercise in enhancing quality of life across the lifespan and the design and implementation of lifestyle interventions for health promotion and disease prevention.
Footnotes
The author declares no conflict of interest and does not have any financial disclosures.
References
- 1.American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Recommendations for the medical management of osteoarthritis of the hip or knee: 2000 update. Arthritis Rheum. 2000;43:1905–15. doi: 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 2.American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. Lippincott, Williams, and Wilkins; 2009. [DOI] [PubMed] [Google Scholar]
- 3.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first national Health and Nutrition Examination Survey (HANES I). Evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol. 1998;128:179–89. doi: 10.1093/oxfordjournals.aje.a114939. [DOI] [PubMed] [Google Scholar]
- 4.Davis MA, Ettinger WH, Neuhas JM. Obesity and osteoarthritis of the knee; evidence from the National Health and Nutrition Examination Survey (NHANES I) Semin Arthritis Rheumatol. 1990;20:34–41. doi: 10.1016/0049-0172(90)90045-h. [DOI] [PubMed] [Google Scholar]
- 5.Felson DT, Anderson JJ, Naimark A, et al. Obesity and knee osteoarthritis. The Framingham Study. Ann Intern Med. 1988;109:18–24. doi: 10.7326/0003-4819-109-1-18. [DOI] [PubMed] [Google Scholar]
- 6.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham osteoarthritis study. Arthritis Rheum. 1987;30:914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 7.Felson DT, Zhang Y, Anthony JM, et al. Weight loss reduces the risk for symptomatic knee osteoarthritis in women. The Framingham Study. Ann Intern Med. 1992;116:535–9. doi: 10.7326/0003-4819-116-7-535. [DOI] [PubMed] [Google Scholar]
- 8.Focht BC. Effectiveness of exercise interventions in reducing pain symptoms among older adults with knee osteoarthritis: a review. J Aging Phys Act. 2006;14:212–35. doi: 10.1123/japa.14.2.212. [DOI] [PubMed] [Google Scholar]
- 9.Focht BC. Obesity and knee osteoarthritis: Behavioral considerations in weight management. Int J Adv Rheumatol. 2007;4:128–132. [Google Scholar]
- 10.Focht BC, Ewing V, Gauvin L, et al. The unique and transient impact of acute exercise on pain perception in older obese or overweight older adults with knee osteoarthritis. Ann Behav Med. 2002;24:201–10. doi: 10.1207/S15324796ABM2403_05. [DOI] [PubMed] [Google Scholar]
- 11.Focht BC, Garver M, Devor ST, et al. Short-term changes in pedometer-determined physical activity in knee osteoarthritis patients: Evidence from the IMPACT-P trial. Med Sci Sports Exerc. 2011;43:S53. [Google Scholar]
- 12.Focht BC, Garver M, Devor ST, et al. Group-Mediated Activity Counseling and Self-Reported Physical Activity in Older, Knee Osteoarthritis Patients: Evidence from the IMPACT-P Trial. Ann Behav Med. 2012;43:S80. [Google Scholar]
- 13.Focht BC, Rejeski WJ, Rejeski AF. Treating obesity in patients with knee osteoarthritis. J Musculoskel Med. 2005;22:491–502. [Google Scholar]
- 14.Leville SG, Fried LP, McMullen W, Guralnik JM. Advancing the taxonomy of disability in older adults. J Gerontol Bio Sci Med Sci. 2004;59:86–93. doi: 10.1093/gerona/59.1.m86. [DOI] [PubMed] [Google Scholar]
- 15.Mehrotra C, Naimi TS, Serdula M, et al. Arthritis, body mass index, and professional advice to lose weight: implications for clinical medicine and public health. Am J Prev Med. 2004;27:16–21. doi: 10.1016/j.amepre.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Minor MA. Impact of exercise on osteoarthritis outcomes. J Rheumatol Suppl. 2004;31:81–86. [PubMed] [Google Scholar]
- 17.Miller GD, Nicklas BJ, Davis C, et al. Intensive weight loss program improves physical function in older obese adults with knee osteoarthritis. Obesity. 2006;14:1219–30. doi: 10.1038/oby.2006.139. [DOI] [PubMed] [Google Scholar]
- 18.Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum. 2004;50:1501–10. doi: 10.1002/art.20256. [DOI] [PubMed] [Google Scholar]
- 19.Nevitt MC. Obesity outcomes in disease management: clinical outcomes for osteoarthritis. Obesity Res. 2002;10:33S–37S. doi: 10.1038/oby.2002.187. [DOI] [PubMed] [Google Scholar]
- 20.Oliveria SA, Felson DT, Cirillo PA, et al. Body weight, body mass index, and incident symptomatic osteoarthritis of the hand, hip, and knee. Epidemiology. 1999;10:161–6. [PubMed] [Google Scholar]
- 21.Rejeski WJ, Brawley LR, Ettinger W, et al. Compliance to exercise therapy in older participants with knee osteoarthritis: implications for treating disability. Med Sci Sports Exer. 1997;29:977–985. doi: 10.1097/00005768-199708000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Rejeski WJ, Brawley LR, Ambrosius WT, Brubaker PH, Focht BC, Foy CG, Fox LD. Older adults with chronic disease: Benefits of group-mediated counseling in the promotion of physically active lifestyles. Hlth Psychol. 2003;22:414–432. doi: 10.1037/0278-6133.22.4.414. [DOI] [PubMed] [Google Scholar]
- 23.Rejeski WJ, Brubaker PH, Goff DC, Bearon LB, McClelland JW, Perri MG, Ambrosius WT. Translating weight loss and physical activity programs into the community to preserve mobility in older, obese adults in poor cardiovascular health. Arch Intern Med. 2011;171:880–886. doi: 10.1001/archinternmed.2010.522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rejeski WJ, Focht BC, Messier SP, Morgan T, Pahor M, Penninx B. Obese older adults with knee osteoarthritis: Weight loss, exercise, and quality of life. Hlth Psychol. 2002;21:419–426. doi: 10.1037//0278-6133.21.5.419. [DOI] [PubMed] [Google Scholar]
- 25.Sharma L, Lou C, Cahue S, et al. The mechanism of effect of obesity in knee osteoarthritis: the mediating role of malalignment. Arthritis Rheum. 2000;43:568–75. doi: 10.1002/1529-0131(200003)43:3<568::AID-ANR13>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]


