Abstract
This study assessed the time to initiation of marijuana abstinence in an adolescent treatment-seeking sample, and identified variables that were predictive of abstinence. Adolescents (n= 69), ages 14 to 18 were randomly assigned to one of two 14-week behavioral treatments. Abstinence was measured with twice-weekly urine toxicology plus teen and parent reports. Discrete-time survival and hazard functions were conducted. The majority of adolescents achieved at least one week of abstinence, and 51% achieved six weeks of abstinence. Initiation of abstinence occurred by the sixth treatment week for 94% of teens with any abstinence suggesting that alternative, clinical approaches should be considered for those not responding by Week 6. Teens with a drug negative urinalysis at intake, and teens that had 2 parents participating in treatment were more likely to achieve at least 6 weeks of abstinence. These findings, if replicated, can be used to inform clinical and research strategies that might lead to enhanced treatment efficacy and cost effectiveness for substance abuse treatment programming.
1. Introduction
Among adolescents admitted for substance abuse treatment in the United States, the proportion of adolescents that were admitted for marijuana treatment was 72% (SAMHSA, 2011). As more adolescents seek treatment for marijuana use disorders, researchers are working to develop more efficacious treatment programs for youth. Multicomponent family treatments, combined evidence-based treatments, group treatments, and behavioral treatments utilizing environmental contingencies have shown success in reducing adolescent substance use although the majority of these treatments produce only moderate effect sizes (Waldron & Turner, 2008).
Unfortunately, a significant number of youth do not achieve short term or sustained abstinence from marijuana during treatment even with the most potent interventions. For example, end of treatment results of the multi-site Cannabis Youth Treatment (CYT) study showed that across 5 treatment sites and types, over 75% of adolescents reported past month substance use (Dennis et al., 2004; Diamond et al., 2002). In a trial conducted by our group examining a multicomponent, contingency management based approach, 42% did not achieve 4 weeks of sustained abstinence while in treatment, and many did not achieve abstinence at all (Stanger, Budney, Kamon, & Thostensen, 2009)
Extant studies with adults have shown that early abstinence and duration of abstinence during treatment is predictive of post treatment abstinence for alcohol, cocaine, marijuana, and tobacco (Carroll et al., 2009; Charney, Zikos, & Gill, 2010; Higgins, Badger, & Budney, 2000; Hildebrandt, McCrady, Epstein, Cook, & Jensen, 2010; Kenford et al., 1994; Moore & Budney, 2002; Petry & Simic, 2002). The time point when abstinence is initiated has also been investigated. For example, one marijuana treatment study showed that of the 54% of participants who achieved 2 or more weeks of abstinence, 90% initiated abstinence within the first 6 weeks of treatment (Moore & Budney, 2003). Similarly, a study of treatment for cocaine dependence observed that most participants who achieved sustained abstinence did so within the initial weeks of the intervention (Weinstock, Rash, & Petry, 2010). Weeks 1 and 2 of the intervention period showed the greatest likelihood for the initiation of abstinence, and few participants initiated any period of abstinence after week 4.
Determining which youth respond to specific interventions, as well as when they respond during the treatment process, would provide important information related to how treatment strategies might be adapted or tailored to improve outcomes. Early identification of treatment non-responders (e.g., those who do not initiate abstinence) can permit those youth to receive alternative treatment strategies such as, more intensive outpatient services, greater magnitude contingencies, or a brief stay in a more restrictive environment so that time and resources are not used to deliver treatments that are ineffective for certain individuals (Borsari, Capone, Mastroleo, & Monti, 2011; Kidorf, Neufeld, King, Clark, & Brooner, 2007; King et al., 2006). Such information would inform stepped care approaches that involve delivering more intensive services only when there is a clear indication of continuing problems despite receiving a lower intensity level of care (Kidorf, et al., 2007; King, et al., 2006). In addition, identification of variables that predict treatment response, such as the initiation of abstinence, can provide guidance in decisions related to assignment to initial treatment modalities (Moore & Budney, 2002).
Although systematic use of toxicology testing to assess treatment response raises some concerns about feasibility in community settings, less costly methods of detecting abstinence through biological specimen testing and more informed understanding and interpretation of test results has made the detection of abstinence a more viable and practical indicator of treatment progress in community treatment settings (Cary, 2006; Gaalema, Higgins, Bradsreet, Heil, & Bernstein, 2011; Huestis et al., 2011). Given the robust findings showing that abstinence during treatment is a robust predictor of later outcomes, initial abstinence would appear to be an optimal indicator of treatment response.
In summary, identifying a time point by which the initiation of abstinence can be expected and finding predictor variables of this response can provide important insight into directing and tailoring adolescent treatments to improve outcomes and optimize costs. To that end, the objective of the present study was to systematically assess the time point at which treatment response (initiation of abstinence) occurs in an adolescent treatment-seeking sample to determine how early in the treatment process we could identify non-responders. Two operational definitions of initiation of abstinence were examined: achieving 1 or more weeks of abstinence and achieving 6 or more sustained weeks of abstinence. One week or more of abstinence was selected to discriminate participants who achieved any versus no abstinence during treatment, and the 6-week duration of abstinence was selected as the indicator of sustained treatment response, which also corresponded to the mean duration of abstinence achieved by the entire sample. The mean duration of abstinence has been used in a similar study conducted with adults as a marker of treatment response (Weinstock et al, 2010). We also explored factors that predict initiation of abstinence such as parent treatment involvement, intake urine toxicology screen result (UA), tobacco use, legal involvement, socioeconomic status, and substance use diagnosis.
2. Materials and Method
2.1. Participant Recruitment
Families from the greater Burlington Vermont area presented for adolescent substance abuse treatment at a University-based treatment research clinic. The families were referred for treatment by schools, the juvenile justice system, community therapists and physicians, or were self-referred. The research treatment services were advertised in local newspapers, through posted flyers, and mailings to local healthcare professionals in the community. Inclusion criteria for treatment were adolescents between 12 and 18 years of age, lived with a parent/guardian who agreed to participate, lived within a 30 minute drive from the clinic, and self-reported use of marijuana during the prior 30 days or a marijuana-positive urine test. Adolescents were ineligible if they displayed active psychosis or current suicidal behavior or had a severe medical illness limiting participation; or if they had other substance dependence requiring more intensive treatment. No adolescents were excluded based on these criteria. A total of 95 youth were assessed, 12 did not meet inclusion criteria, 14 refused treatment or did not complete the intake assessment or did not enroll for another reason.
2.2. Procedures
Detailed description of study procedures can be found in Stanger et al., 2009. All adolescents participated in 14-week treatment program which included twice weekly urine testing, and once weekly 90 minute motivational enhancement and cognitive behavioral therapy (Sampl & Kadden, 2001; Webb, Scudder, Kaminer, & Kadden, 2001). All parent(s) were informed of drug toxicology results. At the end of the 14 weeks, all families were offered an additional 12 weeks of once weekly substance testing to facilitate parental monitoring and were referred, when appropriate, to other community resources. Adolescents were randomized to either one of two conditions. The abstinence-based contingency management (CM) condition included individual counseling plus abstinence-based CM (Stanger, et al., 2009) and family management (Dishion, Nelson, & Kavanagh, 2003). The Comparison condition included individual counseling plus attendance-based vouchers and parent psychoeducation (McCallum, 1994).
Adolescents in the CM condition (n=36) received a contingency management treatment that included monetary vouchers that were awarded on an escalating reinforcement schedule for abstinence. If either the adolescent or parents reported substance use, or a positive breath test or urine specimen was obtained the adolescent was considered positive for substance use. Urinalysis was not performed if the teen or parent reported use to reduce costs, effort and to avoid conflict over potential discrepancies between self report and test results.
Parents received weekly family management sessions that included a parent-delivered, abstinence-based CM program involving rewards for abstinence and negative consequences for substance use. Because Δ-9-THC remains detectable at 50ng/ml for up to two weeks and sometimes longer in heavy marijuana users (Cary, 2006), the abstinence contingency did not start until Week 3. During Weeks 1–2, participants in both conditions received $5 vouchers for each specimen provided to encourage compliance with the program. The adolescent could accrue a maximum of $570 worth of vouchers for abstinence from week 3 to 14 of treatment. Voucher earnings could be redeemed for retail goods selected by the teen (e.g., movie pass, sports/hobby equipment, clothing). Adolescents in the CM condition earned a mean of $312 or $22.28 per week.
Adolescents in the Comparison condition (n=33) earned vouchers for attendance and providing urine specimens for drug testing and their parents attended weekly psychoeducation sessions. Adolescents in the Comparison condition could accrue earnings of $140; average mean earnings were $113 or $8.07 per week.
2.3. Measures
2.3.1. Assessment of substance use
2.3.1.1. Vermont Structured Diagnostic Interview
The Vermont Structured Diagnostic Interview (VSDI) (Hudziak, Copeland, Stanger, & Wadsworth, 2004) was administered by a trained research assistant to assess DSM-IV marijuana abuse and dependence. The interview has demonstrated good psychometric properties (Hudziak et al., 2004). Marijuana use was assessed at intake and twice weekly throughout treatment using the Time-Line Follow-Back method (Sobell & Sobell, 1992), parent report, urinalysis testing, and breathalyzers. At intake, the Time-Line Follow Back assessed frequency of marijuana use three months prior to treatment, and was administered at all visits during treatment.
2.3.1.2. Urine Toxicology Monitoring
Abstinence from marijuana was measured through urine toxicology twice weekly (e.g., Monday/Thursday or Tuesday/Friday). Urine specimens were collected under staff observation and were tested for 11-nor-delta-9-THC-9-carboxylic acid (THCCOOH), the primary marijuana metabolite. A cutoff level of 50 ng/ml for THCCOOH was used to determine marijuana abstinence (Cary, 2006; Huestis, et al., 2011). Creatinine level (<30 ng/ml) was assessed as a proxy for specimens too dilute for valid testing, and an invalid specimen prompted requests to provide another specimen within 4–24 hours. Failure to submit a scheduled specimen was also treated as a positive result. Note that a positive test was always counted as positive, without consideration of whether or not it may have been a function of earlier use detected with the prior test. These procedures were carefully explained to all participants by clinical and research staff.
2.4 Data Analyses
Demographic and baseline substance use variables were compared between participants who achieved ≥ 1 week and ≥ 6 weeks of abstinence from marijuana versus those who did not. Chi-square tests were used for categorical variables and logrank tests for continuous variables. This is a secondary analysis of previously collected data, and thus the original study was not planned and powered for this project specifically. However, assessment of power showed adequate power (78%) to detect a medium effect size at n = 69 and alpha level set at .05 for chi-square tests on baseline demographic characteristics.
Discrete-time survival analysis (Willett & Singer, 1993) using SAS software version 9.3 examined the time to initiation of ≥ 1 week and ≥ 6 weeks marijuana abstinence. Survival analysis provides group detail, week-by-week, about the onset of abstinence for each duration period (≥ 1 week and ≥ 6 weeks) of marijuana abstinence across the intervention. The assessment of power for the discrete-time survival analyses showed adequate power to detect a medium effect size at n = 69 and alpha level set at .05 for ≥ 1 week abstinence and ≥ 6 week abstinence (78% and to 88%, respectively). Initiation (onset) of abstinence was defined as the treatment week during which the first two consecutive marijuana-negative urine specimens were provided (or the first of 12 consecutive marijuana-negative urine specimens for the 6 week period).
A hazard function analysis (Cox, 1972) was also conducted which tested the probability of new initiation of abstinence only among those who had not achieved abstinence in the previous weeks. Often used along with survival analysis, the hazard model has the advantage of allowing the use of continuous factors and covariates and to compare differences in “survival” between groups while adjusting for covariates that affect outcome (Stevens & Hollis, 1989; Weinstock, et al., 2010).
3. Results
3.1. Participant Characteristics
Participants were 69 adolescents (M age = 16 years, SD = 1.05; 57 male; 63 Caucasian) and their parent(s) enrolled in a behavioral treatment trial for marijuana use disorders (Stanger, et al., 2009). Of these adolescents, 68% had 2 parents participating in treatment, 43% met criteria for marijuana dependence, 58% were tobacco users, and 32% were involved with the legal system. Approximately one third of the adolescents (35%) submitted a negative urine specimen at intake indicating that some had initiated a period of abstinence prior to treatment, which is often due to increased parental oversight and pressure to abstain from marijuana use subsequent to school or legal consequences. Of the adolescents that submitted negative urine specimens at intake, 20% resumed marijuana use prior to or during treatment (Tables 1 and 2).
Table 1.
Demographic Characteristics by Abstinence
| Abstinence 0 weeks (n=16) |
Abstinence ≥ 1 week (n=53) |
|||||
|---|---|---|---|---|---|---|
| Variable | n | % | n | % | Statistic (df) | p |
| Gender | ||||||
| male | 13 | 81.2 | 44 | 83.0 | χ2 (1) = 0.03 | .87 |
| female | 3 | 18.8 | 9 | 17.0 | ||
| Treatment | ||||||
| CM† | 6 | 37.5 | 30 | 56.6 | χ2 (1) = 1.80 | .18 |
| Comparison | 10 | 62.5 | 23 | 43.4 | ||
| Intake Urinalysis | ||||||
| Negative | 2 | 12.5 | 22 | 41.5 | χ2 (1) = 4.56 | .03 |
| Positive | 14 | 87.5 | 31 | 58.5 | ||
| # Parent Participants | ||||||
| 1 Parent | 12 | 75.0 | 10 | 18.9 | χ2 (1) = 17.83 | <.001 |
| 2 Parents | 4 | 25.0 | 43 | 81.1 | ||
| Legal Involvement | ||||||
| Yes | 4 | 25.0 | 18 | 33.9 | χ2 (1) = 0.45 | .50 |
| No | 12 | 75.0 | 35 | 66.1 | ||
| Tobacco User | ||||||
| Yes | 9 | 56.3 | 31 | 58.5 | χ2 (1) = 0.30 | .87 |
| No | 7 | 43.7 | 22 | 41.5 | ||
| Cannabis Dependence | ||||||
| Yes | 11 | 68.8 | 19 | 35.8 | χ2 (1) = 5.41 | .02 |
| No | 5 | 31.2 | 34 | 64.2 | ||
CM is Contingency Management
Table 2.
Demographic Characteristics by 6-week Abstinence Status
| Abstinence < 6 weeks (n=34) |
Abstinence ≥ 6 weeks (n=35) |
|||||
|---|---|---|---|---|---|---|
| Variable | n | % | n | % | Statistic (df) | p |
| Gender | ||||||
| male | 28 | 82.4 | 29 | 82.9 | χ2 (1) = .00 | .96 |
| female | 6 | 17.6 | 6 | 17.1 | ||
| Treatment | ||||||
| CM† | 16 | 47.0 | 20 | 57.1 | χ2 (1) = .70 | .40 |
| Comparison | 18 | 53.0 | 15 | 42.9 | ||
| Intake Urinalysis | ||||||
| Negative | 5 | 14.7 | 19 | 54.3 | χ2 (1) = 11.91 | <.001 |
| Positive | 29 | 85.3 | 16 | 45.7 | ||
| # Parent Participants | ||||||
| 1 Parent | 17 | 50.0 | 5 | 14.3 | χ2 (1) = 10.13 | <.01 |
| 2 Parents | 17 | 50.0 | 30 | 85.7 | ||
| Legal Involvement | ||||||
| Yes | 11 | 32.4 | 11 | 31.4 | χ2 (1) = .01 | .93 |
| No | 23 | 67.6 | 24 | 68.6 | ||
| Tobacco User | ||||||
| Yes | 23 | 67.6 | 17 | 48.6 | χ2 (1) = 2.58 | .11 |
| No | 11 | 32.4 | 18 | 51.4 | ||
| Cannabis Dependence | ||||||
| Yes | 16 | 47.0 | 14 | 40.0 | χ2 (1) = .35 | .55 |
| No | 18 | 53.0 | 21 | 60.0 | ||
CM is Contingency Management
3.2. Initiation of 1 or More Week of Abstinence
Overall, 77% percent of the adolescents achieved at least 1 week of marijuana abstinence by the end of treatment. Table 1 presents baseline demographic and substance use variables of the sample by 1 week of abstinence status. Chi-square comparisons of demographic and baseline substance use variables revealed significant differences between participants who achieved ≥ 1 weeks marijuana abstinence versus those who did not. Of seven variables tested, urinalysis at intake, the number of parents participating in treatment, and marijuana dependence were identified as predictor variables (see Table 1). Those who attained abstinence were significantly more likely to: have 2 parents participating in the treatment (81% vs. 25%), meet criteria for marijuana abuse rather than dependence (64% vs. 31%), and have a negative urine toxicology screen result at intake (42% vs. 13%). These 3 significant predictors are included in the hazard model (see below). Other variables (i.e. treatment condition, legal involvement, tobacco use) did not differ significantly between conditions.
Estimated sample survivor probabilities by treatment week (i.e., week 1 through 14) were calculated to indicate the proportion that obtained at least 1 week of abstinence by the end of each treatment week. As shown in Figure 1, the sample survivor probabilities of the two treatment conditions were not significantly different; although they diverged somewhat at week 6 with a higher probability of individuals in the CM treatment achieving at least one week of abstinence after week 6 (although this amounted to only 2 additional teens). The median survival time for the onset of a week or more of marijuana abstinence was 1 week in both the comparison and the CM condition. Overall, the survival probabilities show that 77% of adolescents achieved at least one week of abstinence, and 94% of those did so by week 6.
Figure 1.
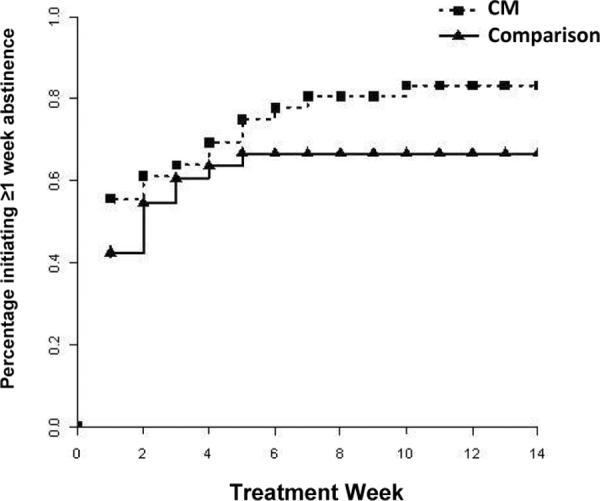
Survival function for initiation of 1 week of abstinence by treatment condition
Figure 2 shows the hazard probabilities by treatment week illustrating the proportion of participants who were not abstinent in prior weeks that initiated 1 or more weeks of marijuana abstinence during that week. The hazard function showed that 78% of participants in the CM condition and 53% of the comparison condition who ever initiated 1 week of abstinence did so by the first week. Only a small number (n = 3) of the remaining teens in the CM condition achieved 1 or more weeks of abstinence beyond week 6.
Figure 2.
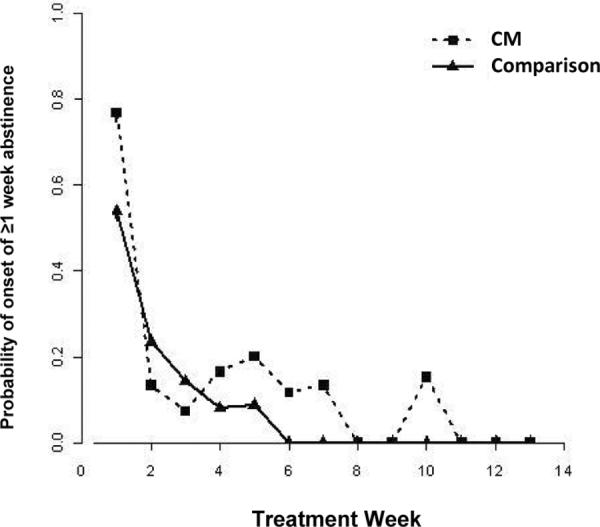
Hazard function for initiation of 1 week of abstinence by treatment condition
Maximum likelihood binary logistic regression was used to fit the discrete-time hazard model for onset of 1 or more weeks of marijuana abstinence (Table 3). A time-only model was first examined using onset of abstinence in weeks 1 through 6 as predictors as weeks 7 through 13 initiation of new abstinence was too infrequent to include in the models. Three time variables were shown to be associated with the initiation of ≥ 1 week of abstinence: onset of abstinence in week 1 (OR = 44.33, p < .001), onset of abstinence in week 2 (OR = 9.46, p < .05), and onset of abstinence in week 5 (OR = 6.89, p < .05). A second model entered additional significant bivariate predictors of achieving ≥1 week of abstinence in a second step: number of parents participating, urinalysis toxicology result at intake, and dependence status. The variables significantly associated with the initiation of ≥ 1 week of abstinence were onset of abstinence in week 1 (p < .001), onset of abstinence in week 2 (p < .05), onset of abstinence in week 5 (p < .05), two parents participating, and negative urinalysis THC result at intake. Using decrement-to-chi-square testing (i.e., −2 LL test) (Willett & Singer, 1993), the difference between the 2 models showed this model fit better than the time-only model (χ2 (3) =219.57–188.02= 31.55, p <.001).
Table 3.
Discrete-time Hazard Model for Onset of≥ 1 or more and ≥ 6 or More Weeks Marijuana Abstinence
| ≥ 1 weeks abstinence | ≥ 6 weeks abstinence | |||||||
|---|---|---|---|---|---|---|---|---|
| Time Only | Time + Predictors | Time Only | Time + Predictors | |||||
|
|
||||||||
| Predictor | Log-Odds | OR + | Log-Odds | OR | Log-Odds | OR | Log-Odds | OR |
| Week 1 | 3.79 | 44.33** | 3.04 | 20.84** | 3.08 | 44.86** | 3.43 | 30.80** |
| Week 2 | 2.25 | 9.46* | 1.80 | 6.08* | 1.58 | 4.88 | 1.32 | 3.73 |
| Week 3 | 1.66 | 5.28 | 1.45 | 4.25 | 2.41 | 11.15* | 2.16 | 8.67* |
| Week 4 | 1.79 | 5.98 | 1.59 | 4.90 | 1.80 | 6.05 | 1.63 | 5.09 |
| Week 5 | 1.93 | 6.89* | 1.77 | 5.88* | 2.32 | 10.15* | 2.25 | 9.51* |
| Week6 | 0.88 | 2.42 | 0.77 | 2.16 | 2.00 | 7.38 | 1.83 | 6.25 |
| Parent Participants (1 or 2) | 1.90 | 6.68** | 1.84 | 6.30** | ||||
| Intake UA‡(pos/neg for THC†) | −1.79 | 0.17** | −1.78 | 0.17** | ||||
| Cannabis Dependence (yes/no) | −0.26 | 0.77 | - | - | ||||
| −2LL | 219.57 | 188.02 | 178.82 | 175.58 | ||||
Note. Weeks 1 through 6 were tested as predictors as weeks 7 through 13 initiation of new abstinence was too infrequent to include in the models. Predictor reference categories: No. of Parent Participants: 2; Intake Urinalysis: negative; Dependence status; not dependent,
p < .05,
p <.001.
Delta-9-Tetrahydrocannabinol;
Urinalysis;
Odds Ratio.
3.3. Initiation of 6 or More Weeks of Abstinence
We observed that 51% of adolescents achieved at least 6 weeks of marijuana abstinence. Table 2 presents baseline demographic and substance use variables of the sample by abstinence status. Chi-square comparisons revealed significant differences between participants who achieved ≥ 6 weeks marijuana abstinence versus those who did not. Urinalysis at intake and the number of parents participating in treatment were identified as predictor variables (see Table 2). Of the variables tested, adolescents that attained 6 or more weeks of abstinence were more likely to have 2 parents participating in the treatment (86% vs. 50%) and to have a negative urine toxicology screen result at intake (54% vs. 15%). These 2 significant predictors are included in the hazard model (see below). Other variables (i.e. treatment condition, legal involvement, tobacco use, dependence status) did not differ significantly between conditions.
Estimated sample survivor probabilities for the CM condition and comparison condition by treatment week (i.e., week 1 through 9) were calculated. The survivor probabilities of the two treatment conditions did not significantly differ, although Figure 3 shows a marginally higher probability of teens in the CM treatment achieving ≥ 6 weeks of abstinence. The median survival time for the onset of 6 weeks or more of marijuana abstinence was week 2 in the comparison condition and week 1 in the CM condition. Overall, the survival probabilities show that half of all adolescents achieved at least six weeks of abstinence, and (94%) of those adolescents did so by week 6.
Figure 3.
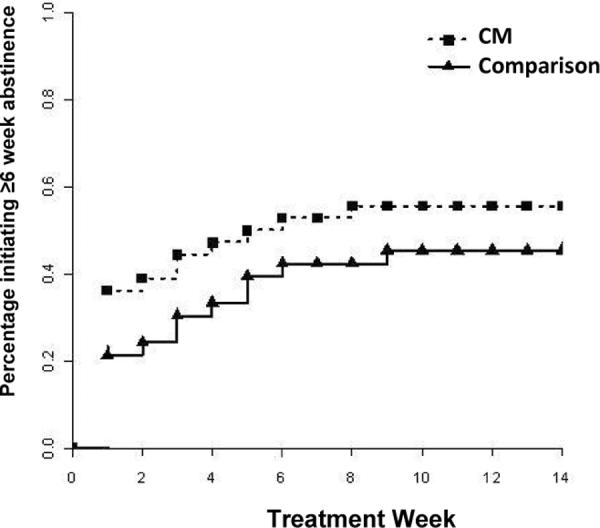
Survival function for initiation of 6 weeks of abstinence by treatment condition
Hazard probabilities are shown (Figure 4) for the CM condition and comparison condition by treatment week. The hazard function showed that close to 45% of participants in the CM condition and about 25% of the comparison condition who ever initiated 6 weeks of abstinence, did so in week 1. Overall, only 1 adolescent from each treatment condition initiated 6 weeks of abstinence beyond week 6 of treatment.
Figure 4.
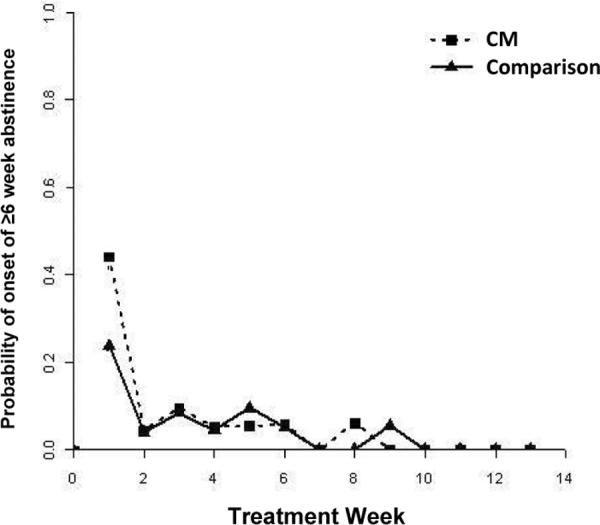
Hazard function for initiation of 6 weeks of abstinence by treatment condition
Maximum likelihood binary logistic regression was used to fit the discrete-time hazard model for onset of 6 or more weeks of marijuana abstinence. As indicated earlier, onset of abstinence in weeks 7 through 13 did not provide sufficient information to model initiation of abstinence therefore weeks 1 through 6 were included as predictors in the time-only model (Table 3). As shown in Table 3, three time variables were shown to be associated with the initiation of ≥ 6 weeks abstinence. Those were onset of abstinence in week 1 (OR = 44.86, p < .001), onset of abstinence in week 3 (OR = 11.15, p < .05), and onset of abstinence in week 5 (OR = 10.15, p < .05). The second model for ≥ 6 weeks of abstinence included two significant predictor variables (number of parents participating and urinalysis toxicology result at intake). This model showed onset of abstinence in week 1 (p < .001), onset of abstinence in week 3 (p < .05), onset of abstinence in week 5 (p < .05), two parents participating (p < .001), and negative urinalysis THC result at intake (p < .001) were significantly associated with ≥ 6 weeks of abstinence. However, using decrement-to-chi-square testing (i.e., −2 LL test) (Willett & Singer, 1993), the difference between the 2 models was not significant indicating the addition of the two predictors, 2 parents participating and negative urinalysis result, did not significantly improve the overall model fit (χ2 (2) = 178.82 – 175.58 = 3.24, p = n.s.).
4. Discussion
Despite advances in adolescent treatments, many youth that present for marijuana and other substance use disorders will not show a clear positive response to treatment (Brown, D'Amico, McCarthy, & Tapert, 2001). This study sought to identify the earliest time point by which one could determine whether or not the teen was likely to respond to two behavioral treatments. The time of onset of treatment response operationalized as the initiation of drug abstinence did not differ across the two treatments. Clearly, a positive treatment response whether operationalized by a minimal abstinence period (≥1 week of abstinence), or a more substantial response (≥ 6 weeks of abstinence), almost always occurred very early in treatment and rarely occurred subsequent to Week 6. In fact, 94% of the teens that achieved at least 1 or 6 weeks of abstinence achieved it by the 6th week of treatment. Similar findings have been described in adult trials that report positive response to treatment occurs by the 6th week of treatment for adult cannabis abusers (Moore & Budney, 2003), and within the first few weeks or not at all in studies of cocaine dependence treatment (Kampman et al., 2002; Plebani, Kampman, & Lynch, 2009; Weinstock, et al., 2010) and women treated for alcohol dependence (Hildebrandt, McCrady, Epstein, Cook, & Jensen, 2010).
Identifying a reliable time point for determining whether an individual will respond or not to a specific treatment can provide important information relevant to directing treatment approaches and guiding decisions about whether to continue treatment as usual or initiate an alternate treatment strategy. For example, in both the comparison and CM treatments, one could argue that major treatment adjustments should commence if a teen does not initiate abstinence by week 6. Potential adjustments might include increased magnitude voucher earnings, offering a more intensive outpatient approach, or a brief stay in restricted environment. Such adjustments would be consistent with the concept of stepped care approaches that have been utilized effectively with adults (Borsari, et al., 2011; Kidorf, et al., 2007; King, et al., 2006). The time of onset of treatment response can also inform research protocols designed to determine the most effective treatment strategies for a clinical population. For example, the major finding from this study (no treatment response is likely after 6 weeks) might inform the parameters of a Sequential Multiple Assignment Randomized Trial (SMART) designed to investigate adaptive treatment strategies (Collins, Murphy, & Strecher, 2007). SMART trials test predetermined clinical strategies based on whether or not certain outcome criteria are reached at specific time points. Based on the current findings, a SMART design might involve randomizing treatment nonresponders at the conclusion of week 6 to either an alternate form of treatment, an intensified version of the initial treatment, or remaining with the original treatment. Comparison of alternative overall strategies would determine whether altering or adjusting treatment at that specific time point improves outcomes.
To assist in determining which youth would be more likely to show a positive treatment response and inform future effectiveness trials, this study also identified two significant variables that predicted the initiation of 6 or more weeks of abstinence: urinalysis toxicology result at intake and number of parents participating in treatment. Youth that were abstinent for 6 or more weeks were more likely to have presented to treatment with a substance negative urine screen, which is consistent with studies conducted with adults that show negative drug urinalysis at treatment intake are predictive of better treatment outcomes (Moore & Budney, 2002; Sofuoglu, Gonzalez, Poling, & Kosten, 2003; Tzilos, Rhodes, Ledgerwood, & Greenwald, 2009). Marijuana abstinence prior to treatment could be associated with the individual's motivation and ability to stop substance use. Teens who initiated 6 or more weeks of abstinence also were significantly more likely to have 2 parents involved in their treatment. Having 2 parents involved in treatment might positively relate to treatment response by indicating better initial family functioning, greater parental monitoring, increased parental involvement in the teen's activities, and more awareness of the teen's plans and whereabouts, which have been shown to play an important in reducing substance use (Barnes, Hoffman, Welte, Farrell, & Dintcheff, 2006; Bobakova, Geckova, Klein, Reijneveld, & van Dijk, 2012; Kim & Neff, 2010). The number of parents involved in the youth's treatment may be useful for initial treatment assignment or for use as a tailoring variable to examine in comparison trials.
4.1. Limitations
The generalizability of this study is limited by its relatively small sample size and the participation of primarily Caucasian families with a high proportion of two-parents participating in treatment with relatively high levels of education. These participants lived in small metropolitan or rural communities and the teens were primarily males who reported marijuana as their primary drug of abuse. Potential racial, ethnic, living environment, and socioeconomic influences on initiation of abstinence and the predictor variables could not be assessed. Families of different races, ethnicities, and socioeconomic status may not achieve the same rates of abstinence, may have a lower percentage of two-parent participating families or types of guardians that participate, and a lower percentage of teens entering treatment with a negative urine specimen. Moreover, male and female teens may differ in the timing of their treatment response. In addition, these analyses should be considered exploratory, as we did not control for multiple comparisons as (all analyses were repeated twice for ≥ 1 week abstinence and ≥ 6 weeks abstinence, and the original study was not designed or powered specifically to address the issues assessed in this study. There is a clear need for replication of these findings with a larger and more diverse sample of adolescents.
Last, the results of this study were determined in the context of two behavioral treatments that included parent involvement and tested the initiation of abstinence as a marker of treatment progress. These findings might not apply to other types of treatment or other markers of treatment response (e. g., harm reduction indicators).
4.2. Conclusions
Positive treatment responses to adolescent and adult treatments are likely to become evident relatively early in the treatment process. Similarly, certain socio-demographic variables might serve as indicators of the potential success or failure of specific treatments. This study showed that very few teens achieved abstinence after the sixth week of treatment. Clinical strategies that consider such data, such as stepped care treatment approaches, are necessary to enhance the overall efficacy and cost effectiveness of substance abuse treatment programming. SMART experimental designs are an approach that might be used to evaluate alternative strategies based on identification of variables related to treatment responding. The use of tailored treatment approaches and the utilization of research designs that evaluate adaptive clinical strategies are needed to improve upon the modest abstinence rates commonly observed in adolescent treatments.
Acknowledgements
This work was supported by NIDA grants DA015186 and T32-DA022981, NIAAA grant AA016917, and by Award Number 1UL1RR029884 from the National Center for Research Resources awarded to the Translational Research Institute at the University of Arkansas for Medical Sciences. We would like to thank the staff at the Treatment Research Center at the University of Vermont, especially Heath Rocha, as well as the participating families. Limited portions of these analyses were presented at the 2011 College on Problem of Drug Dependence meeting.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barnes GM, Hoffman JH, Welte JW, Farrell MP, Dintcheff BA. Effects of Parental Monitoring and Peer Deviance on Substance Use and Delinquency. Journal of Marriage and Family. 2006;68(4):1084–1104. doi: 10.1111/j.1741-3737.2006.00315.x. [Google Scholar]
- Bobakova D, Geckova AM, Klein D, Reijneveld SA, van Dijk JP. Protective factors of substance use in youth subcultures. Addictive Behaviors. 2012;37(9):1063–1067. doi: 10.1016/j.addbeh.2012.04.014. doi: 10.1016/j.addbeh.2012.04.014. [DOI] [PubMed] [Google Scholar]
- Borsari B, Capone C, Mastroleo NR, Monti P. Clinical considerations in the treatment of substance use disorders with veterans. Journal of Contemporary Psychotherapy. 2011;41(4):247–253. doi: 10.1007/s10879-011-9172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, D'Amico EJ, McCarthy DM, Tapert SF. Four-year outcomes from adolescent alcohol and drug treatment. J Stud Alcohol. 2001;62(3):381–388. doi: 10.15288/jsa.2001.62.381. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, Rounsaville BJ. Enduring effects of a computer-assisted training program for cognitive behavioral therapy: a 6-month follow-up of CBT4CBT. Drug and Alcohol Dependence. 2009;100((1–2):178–181. doi: 10.1016/j.drugalcdep.2008.09.015. doi: S0376-8716(08)00360-8 [pii] 10.1016/j.drugalcdep.2008.09.015 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cary PL. The marijuana detection window: Determining the length of time cannabinoids will remain detectable in urine following smoking. A critical review of relevant research and cannabinoid detection guidance for drug courts. Drug Court Practitioner Fact Sheet. 2006;IV(2):1–16. [Google Scholar]
- Charney DA, Zikos E, Gill KJ. Early recovery from alcohol dependence: Factors that promote or impede abstinence. Journal of Substance Abuse Treatment. 2010;38(1):42–50. doi: 10.1016/j.jsat.2009.06.002. doi: 10.1016/j.jsat.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. American Journal of Preventive Medicine. 2007;32(5 Suppl):S112–118. doi: 10.1016/j.amepre.2007.01.022. doi: S0749-3797(07)00051-7 [pii] 10.1016/j.amepre.2007.01.022 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox DR. Regression models and life tables. Journal of the Royal Statistical Society. 1972;34(Series B):187–202. [Google Scholar]
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, Funk R. The cannabis youth treatment (CYT) study: Main findings from two randomized trials. Journal of Substance Abuse Treatment. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Diamond GS, Godley SH, Liddle HA, Sampl S, Webb CPM, Tims FM, Meyers R. Five outpatient treatment models for adolescent marijuana use: A description of the Cannabis Youth Treatment interventions. Addiction. 2002;97(1):S70–S83. doi: 10.1046/j.1360-0443.97.s01.3.x. doi: 10.1046/j.1360-0443.97.s01.3.x. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Nelson SE, Kavanagh K. The family check-up with high-risk young adolescents: Preventing early-onset substance use by parent monitoring. Behavior Therapy. 2003;34:553–571. [Google Scholar]
- Gaalema DE, Higgins ST, Bradsreet MP, Heil SH, Bernstein IM. Using NicAlert strips to verify smoking status among pregnant cigarette smokers. Drug and Alcohol Dependence. 2011;119(1–2):130–133. doi: 10.1016/j.drugalcdep.2011.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Badger GJ, Budney AJ. Initial abstinence and success in achieving longer-term cocaine abstinence. Experimental and Clinical Psychopharmacology. 2000;8(3):377–386. doi: 10.1037//1064-1297.8.3.377. [DOI] [PubMed] [Google Scholar]
- Hildebrandt T, McCrady B, Epstein E, Cook S, Jensen N. When should clinicians switch treatments? An application of signal detection theory to two treatments for women with alcohol use disorders. Behaviour Research and Therapy. 2010;48(6):524–530. doi: 10.1016/j.brat.2010.03.001. doi: 10.1016/j.brat.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudziak JJ, Copeland W, Stanger C, Wadsworth M. Screening for DSM-IV externalizing disorders with the Child Behavior Checklist: A receiver-operating characteristic analysis. The Journal of Child Psychology and Psychiatry. 2004;45(7):1299–1307. doi: 10.1111/j.1469-7610.2004.00314.x. doi: 10.1111/j.1469-7610.2004.00314.x. [DOI] [PubMed] [Google Scholar]
- Huestis MA, Verstraete A, Kwong TC, Morland J, J. VM, de la Torre R. Oral fluid testing: promises and pitfalls. Clinical Chemistry and Laboratory Medicine. 2011;57(6):805–810. doi: 10.1373/clinchem.2010.152124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampman KM, Volpicelli JR, Mulvaney FD, Rukstalis M, Alterman AI, Pettinati H. Cocaine withdrawal severity and urine toxicology results from treatment entry predict outcome in medication trials for cocaine dependence. Addictive Behaviors. 2002;27:251–260. doi: 10.1016/s0306-4603(01)00171-x. [DOI] [PubMed] [Google Scholar]
- Kenford SL, Fiore MC, Jorenby DE, Smith SS, Wetter D, Baker T. Predicting smoking cessation: Who will quit with and without the nicotine patch. JAMA. 1994;271(8):589–594. doi: 10.1001/jama.271.8.589. [DOI] [PubMed] [Google Scholar]
- Kidorf M, Neufeld K, King VL, Clark M, Brooner RK. A stepped care approach for reducing cannabis use in opioid-dependent outpatients. Journal of Substance Abuse Treatment. 2007;32(4):341–347. doi: 10.1016/j.jsat.2006.09.005. doi: 10.1016/j.jsat.2006.09.005. [DOI] [PubMed] [Google Scholar]
- Kim Y-M, Neff JA. Direct and indirect effects of parental influence upon adolescent alcohol use: A structural equation modeling analysis. Journal of Child & Adolescent Substance Abuse. 2010;19(3):244–260. doi: 10.1080/1067828x.2010.488963. [Google Scholar]
- King VL, Kidorf MS, Stoller KB, Schwartz R, Kolodner K, Brooner RK. A 12-month controlled trial of methadone medical maintenance integrated into an adaptive treatment model. Journal of Substance Abuse Treatment. 2006;31(4):385–393. doi: 10.1016/j.jsat.2006.05.014. doi: 10.1016/j.jsat.2006.05.014. [DOI] [PubMed] [Google Scholar]
- McCallum T. Drugs: Parents and young people. Health Education Unit, the University of Sydney; Sydney: 1994. [Google Scholar]
- Moore BA, Budney AJ. Abstinence at intake for marijuana dependence treatment predicts response. Drug and Alcohol Dependence. 2002;67:249–257. doi: 10.1016/s0376-8716(02)00079-0. [DOI] [PubMed] [Google Scholar]
- Moore BA, Budney AJ. Relapse in outpatient treatment for marijuana dependence. Journal of Substance Abuse Treatment. 2003;25:85–89. doi: 10.1016/s0740-5472(03)00083-7. [DOI] [PubMed] [Google Scholar]
- Petry N, Simic F. Recent advances in the dissemination of contingency management techniques: Clinical and research perspectives. Journal of Substance Abuse Treatment. 2002;23:81–86. doi: 10.1016/s0740-5472(02)00251-9. doi: 10.1016/s0740-5472(02)00251-9. [DOI] [PubMed] [Google Scholar]
- Plebani JG, Kampman KM, Lynch KG. Early abstinence in cocaine pharmacotherapy trials predicts successful treatment outcomes. Journal of Substance Abuse Treatment. 2009;27(313–317) doi: 10.1016/j.jsat.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA . National Admissions to Substance Abuse Treatment Services. 2011. Treatment Episode Data Set (TEDS). 1999 – 2009; pp. S–56. (DASIS Series). HHS Publication No. (SMA) 11-4646) [Google Scholar]
- Sampl S, Kadden R. Motivational Enhancement Therapy and Cognitive Behavioral Therapy for Adolescent Cannabis Users: 5 Sessions. Vol. 1. Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2001. [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biological methods. Human Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Sofuoglu M, Gonzalez G, Poling J, Kosten TR. Prediction of treatment outcome by baseline urine cocaine results and self-reported cocaine use for cocaine and opioid dependence. The American Journal of Drug and Alcohol Abuse. 2003;29(4):713–727. doi: 10.1081/ada-120026256. doi: 10.1081/ada-120026256. [DOI] [PubMed] [Google Scholar]
- Stanger C, Budney AJ, Kamon JL, Thostensen J. A randomized trial of contingency management for adolescent marijuana abuse and dependence. Drug and Alcohol Dependence. 2009;105:240–247. doi: 10.1016/j.drugalcdep.2009.07.009. doi: 10.1016/j.drugalcdep.2009.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens VJ, Hollis JF. Prevention smoking relapse, using an individually tailored skills-training technique. Journal of Consulting and Clinical Psychology. 1989;57(3):420–424. doi: 10.1037//0022-006x.57.3.420. [DOI] [PubMed] [Google Scholar]
- Tzilos GK, Rhodes GL, Ledgerwood DM, Greenwald MK. Predicting cocaine group treatment outcome in cocaine-abusing methadone patients. Experimental and Clinical Psychopharmacology. 2009;17(5):320–325. doi: 10.1037/a0016835. doi: 10.1037/a0016835. [DOI] [PubMed] [Google Scholar]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):238–261. doi: 10.1080/15374410701820133. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]
- Webb C, Scudder M, Kaminer Y, Kadden R. The Motivational Enhancement Therapy and Cognitive Behavioral Therapy for Adolescent Cannabis Users. Vol. 2. Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; Rockville, MD: 2001. [Google Scholar]
- Weinstock J, Rash CJ, Petry NM. Contingency management for cocaine use in methadone maintenance patients: when does abstinence happen? Psychology of Addictive Behaviors. 2010;24(2):282–291. doi: 10.1037/a0017542. doi: 10.1037/a0017542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett JB, Singer JD. Investigating onset, cessation, relapse, and recovery: Why you should, and how you can, use discrete-time survival analysis to examine event occurrence. Journal of Consulting and Clinical Psychology. 1993;61(6):952–965. doi: 10.1037//0022-006x.61.6.952. [DOI] [PubMed] [Google Scholar]


