Abstract
DNA vaccines combine remarkable genetic and chemical stability with proven safety and efficacy in animal models, while remaining less immunogenic in humans. In contrast, live-attenuated vaccines have the advantage of inducing rapid, robust, long-term immunity after a single-dose vaccination. Here we describe novel iDNA vaccine technology that is based on an infectious DNA platform and combines advantages of DNA and live attenuated vaccines. We applied this technology for vaccination against infection with Venezuelan equine encephalitis virus (VEEV), an alphavirus from the Togaviridae family. The iDNA vaccine is based on transcription of the full-length genomic RNA of the TC-83 live-attenuated virus from plasmid DNA in vivo. The in vivo-generated viral RNA initiates limited replication of the vaccine virus, which in turn leads to efficient immunization. This technology allows the plasmid DNA to launch a live-attenuated vaccine in vitro or in vivo. Less than 10 ng of pTC83 iDNA encoding the full-length genomic RNA of the TC-83 vaccine strain initiated replication of the vaccine virus in vitro. In order to evaluate this approach in vivo, BALB/c mice were vaccinated with a single dose of pTC83 iDNA. After vaccination, all mice seroconverted with no adverse reactions. Four weeks after immunization, animals were challenged with the lethal epidemic strain of VEEV. All iDNA-vaccinated mice were protected from fatal disease, while all unvaccinated controls succumbed to infection and died. To our knowledge, this is the first example of launching a clinical live-attenuated vaccine from recombinant plasmid DNA in vivo.
Keywords: DNA vaccine, live attenuated virus, infectious DNA, Venezuelan equine encephalitis, VEE, TC-83
1. Introduction
DNA vaccines represent a promising technology due to their safety, ease of production, genetic stability, no need for cold chain, and activation of innate immunity pathways [1, 2]. However, the clinical application of DNA vaccines has been limited. While DNA vaccines have been recently approved for veterinary applications, low immunogenicity in humans is the major obstacle [3]. In contrast, live-attenuated vaccines are among the most cost-effective and broadly used public health interventions representing approximately 60% of all licensed vaccines and providing long-term immunity following a single-dose vaccination [4]. Live vaccines have own limitations including the need for biocontainment during production, cold chain requirements, and safety concerns due to the possibility of reversion, especially for RNA viruses. These limitations have restricted the use and approval of live-attenuated viral vaccines due to potential adverse events in immunocompromized individuals and the possibility of genetic reversion to the virulent, wild-type phenotype. One example of restricted use of live vaccine is the TC-83 vaccine for Venezuelan equine encephalitis virus (VEEV). VEEV causes epizootics and epidemics in the North, Central, and South America including an outbreak in Texas in 1971 [5, 6]. Climate, ecological changes and international travel have increased the risk of VEEV re-emergence [7–9]. The virus can also be easily produced in large quantities and aerosolized as a biological weapon [7, 10]. The potentially threatening effects of the VEEV re-emergence demand an effective vaccine [11].
The experimental, live-attenuated TC-83 vaccine [12] is currently the only live vaccine used under an Investigational New Drug (IND) protocol for immunization of medical personnel at risk [7, 13, 14]. The TC-83 vaccine provides protection against many epizootic viruses of the VEEV complex [15] including IAB, IC, and IE. However, the vaccine can cause adverse effects such as headache and fever in approximately 23% of vaccinees. Another approximately 18% of vaccine recipients do not develop sufficient neutralizing antibody titers [16]. Genetic reversions in the TC-83 virus have been associated with adverse effects [17]. RNA viruses have high rates of mutations [18, 19], which contribute to genetic instability and accumulation of potentially harmful mutations during virus passages for vaccine production.
Due to its long record of clinical use, TC-83 represents a logical starting point for preparation of a safer and better vaccine against VEEV [17]. Here, we describe a novel immunization DNA (iDNA) vaccine platform that potentially can overcome the weaknesses of the TC-83 vaccine by combining the advantages of DNA immunization with the efficacy of live-attenuated vaccine. The pTC83 iDNA vaccine represents a recombinant plasmid that encodes the entire genomic RNA of TC-83 virus under control of eukaryotic promoter. Upon vaccination, iDNA plasmid drives transcription of viral RNA in vivo and initiates limited replication of a genetically defined, TC-83-like vaccine virus. Thus, a live attenuated vaccine is launched from iDNA in vivo, with no need for external cell substrates or virus passages for vaccine production, which minimizes the potential for reversions or adverse effects, ensures genetic stabilization, and results in efficient immunization. Thus, iDNA vaccine technology allows effective conversion of DNA immunization into a highly immunogenic live attenuated vaccine and combines advantages of both vaccine platforms.
2. Materials and Methods
2.1. Cells and viruses
Baby hamster kidney (BHK-21), Chinese hamster ovary (CHO) and Vero cell lines were obtained from the American Type Culture Collection (Manassas, VA) and maintained in a humidified incubator at 37°C in 5% CO2 in αMEM supplemented with 10% fetal bovine serum (FBS) and gentamicin sulfate (10 µg/ml) (Life Technologies, Carlsbad, CA). The TC-83 live-attenuated vaccine was obtained from the U.S. Army Medical Research and Materiel Command (Fort Detrick, MD), amplified once in CHO cells and stored at −80° C. The Trinidad donkey strain of VEEV, a 1943 subtype IAB isolate from an epidemic/epizootic [20], is a standard challenge stock and was used at the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID, Fort Detrick, MD). VEEV strain 3908 virus, a 1995 epidemic subtype IC isolate (Weaver et al., 1996), is a standard challenge stock that was used at the University of Texas Medical Branch (UTMB, Galveston, TX).
2.2. Plasmids and iDNA preparation
TC-83 vaccine virus was propagated in CHO cells in 75 cm2 flask. At 48 hr post infection, the virus was harvested, clarified, and frozen at −80° C in 1 ml aliquots. Viral RNA was extracted by Trizol LS (Life Technologies). Four cDNA fragments were generated by using One-Step RT-PCR system with specific oligonucleotide primers. Then, cDNA fragments were assembled within pcDNA3.1-derived plasmid under control of CMV promoter.
2.3. Transfections and in vitro assays
CHO and Vero cells were transfected by electroporation of plasmid iDNA at concentrations ranging from 8 ng to 5 µg in 75 cm2 flasks. Transfection of CHO and Vero cells was done essentially as described previously [21]. As controls, cells were infected with 102 to 105 PFU of TC-83 virus. For virus growth curves, virus samples were harvested at indicated intervals and quantitated in duplicates by a standard plaque assay in Vero cells.
2.4. Immunizations and challenge
The iDNA plasmid was isolated from E.coli by an endotoxin-free method (Qiagen, Valencia, CA) and formulated in phosphate-buffered saline (PBS) to a concentration of 1 mg/ml. Prior to vaccinations, three-week-old female BALB/c mice were anesthetized with isoflurane. Mice were vaccinated intramuscularly (i.m.) with 50 µl of iDNA in the medial thighs, followed by in vivo electroporation at an amplitude of 100 V with pulse duration of 50 msec and an interval between pulses of 200 msec. Controls similarly received unrelated pcDNA3.1- based plasmid DNA in PBS. Animals were electroporated at the site of injection using a two-pin electrode and a square wave electroporator (ECM 830, BTX Genetronics, San Diego, CA). Blood samples were collected from the retro-orbital sinus to detect viremia during 3 days after vaccination by amplification of plasma virus with Vero cells. In order to confirm that the vaccine virus launched from the iDNA in vivo maintained the TC-83 E2 sequence, the E2 gene from the plasma virus was amplified by using the following primers: 8559-GGAGATCCACCGAGGAGCTG-8578; 9157-GGAATGCGAGTGTGGCGGCAC-9177; 9190-GGCGGCACAAAGATCTCCGAG-9170; and 9850-GCCGAGACCACCTGGGAGTCC-9830. The E2 cDNA fragments were cloned into pCR2.1-TOPO and DNA sequence was determined.
After vaccinations, animals were observed daily for clinical signs of infection, and body weights were determined on days 1–7, 14 and 21 after vaccination. Sera were collected on day 21 after vaccination, shortly before viral challenge. Western blot, plaque reduction neutralization assay (PRNT) and an indirect immunofluorescence assay (IFA) were performed to determine antibody responses to TC-83. Mice were then transferred into BSL3 facility and challenged with virulent VEEV strain 3908 at a dose of 105 PFU in 100 µl by the subcutaneous (s.c.) route. Blood samples were collected to detect viremia for 3 days after challenge. Alternatively to electroporation, iDNA vaccination of BALB/c/mice with pTC83 was performed by using an in vivo transfection reagent. The TransIT gene delivery polymer (Mirus, Madison, WI) was used for transfecting iDNA vaccine intravenously (i.v.) according to the manufacturer’s instructions. The statistical significance of differences in virus titers between vaccinated and control animals were determined by Student's t test.
2.5. Serology
Neutralizing antibodies against TC-83 virus were determined in Vero cells by PRNT80. Serologic assays also included western blot and IFA. For western blot, the TC-83 viral proteins were separated using 4–12% gradient SDS-PAGE and probed with mouse antisera. For IFA, CHO cells were grown in 8-well chamber slides, and virus samples were diluted at 10-fold increments in the αMEM containing 10% FBS and absorbed (0.1 ml/well) onto CHO cell monolayers for 1 h at 37°C. Then, 0.3 ml of the medium was added per well and incubation was continued for indicated times. Cells were fixed with cold acetone and probed with indicated antisera, followed by fluorescein-labeled IgG (H&L).
3. Results
3.1. Preparation of pTC83 iDNA
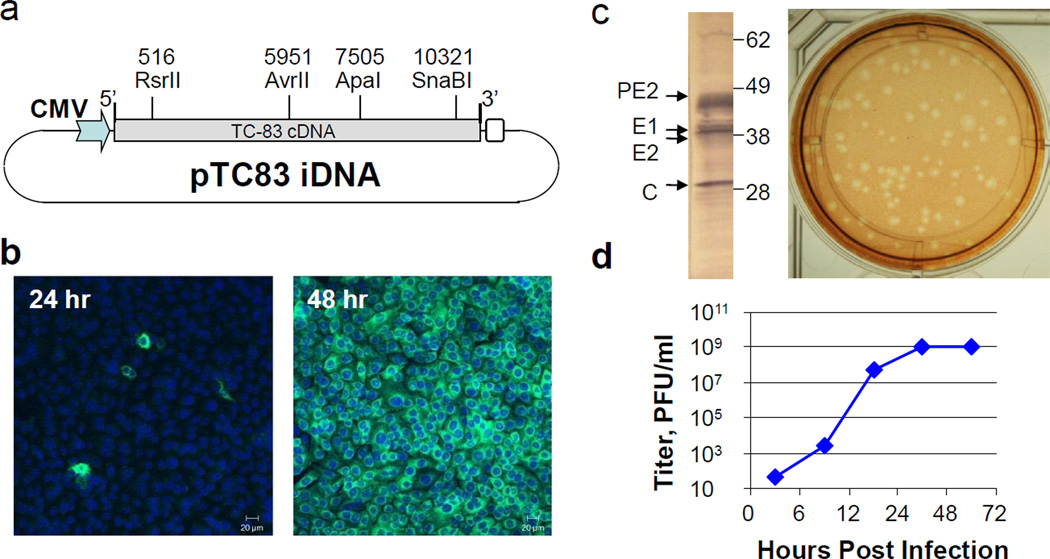
Four cDNA fragments derived from TC-83 viral RNA by RT-PCR were combined within the pcDNA3.1-derived plasmid that resulted in the pTC83 iDNA plasmid containing the full-length cDNA of TC-83 genomic RNA downstream from the CMV major immediate-early promoter (Fig. 1a). Since the authentic 5’ and 3’-termini of RNA are critically important for alphavirus replication [8], the distance between the CMV promoter and the start of RNA polymerase transcription was optimized to ensure transcription of the functional TC-83 genomic RNA. A ribozyme sequence derived from the hepatitis delta virus was inserted downstream from the TC-83 3’-terminal poly-A sequence.
Fig. 1. Preparation of pTC83 iDNA containing the full-length TC-83 cloned genome and generation of TC-83 virus in transfected CHO cells.
(a) Schematic representation of pTC83 plasmid. Restriction sites used for preparation of the full-length TC-83 clone are indicated.
(b) Indirect immunofluorescence assay (IFA) of CHO cells transfected with pTC83 iDNA. IFA was performed at 24 hr (left panel) and 48 hr post electroporation. In order to visualize nuclei in transfected cells, the 4',6-diamidino-2-phenylindole (DAPI) stain was used.
(c) Western blot of CHO cells transfected with pTC83 iDNA (left panel) and plaque assay of the supernatant from CHO cells transfected with pTC83 iDNA (right panel). Western blot was performed at 24 hr post electroporation using ATCC antiserum against VEEV. Plaque assay was carried out in Vero cell monolayers.
(d) Replication of iDNA-derived TC-83 virus in infected Vero cells. Vero cells were infected with 100 PFU of iDNA-derived TC-83 virus. Plaque titer was determined in duplicates, error bars are not visible at the log scale shown.
3.2. Generation of virus from iDNA in vitro
The pTC83 iDNA vaccine was transfected into CHO cells by electroporation. Transfected cells were seeded into chamber slides and expression of TC-83 antigens was detected in by IFA at 24 hr post transfection by using ATCC TC-83-specific rabbit antiserum (Fig. 1b). The TC-83 antigens were expressed in the cytoplasm of transfected cells. By 48 hr, all cells were positive for TC-83 antigens, thus confirming virus replication (Fig. 1b). Expression of the TC-83 proteins was confirmed by SDS-PAGE and western blot (Fig. 1c). The results for transfected Vero cells were similar to these of CHO cells (data not shown). Presence of the replicating virus was confirmed by direct plaque assay of the cell culture media samples (Fig. 1c), as well as by virus amplification and growth curve using infection of Vero cells (Fig. 1d). For amplification and growth curve, Vero cells were inoculated with 100 PFU of the virus harvested from pTC83 iDNA-transfected CHO cells. Incubation was continued for 72 hr. Consistent with previous observations [22], the virus replicated rapidly and reached a titer of 109 PFU/ml in Vero cells at 30 hr postinfection (Fig. 1d).
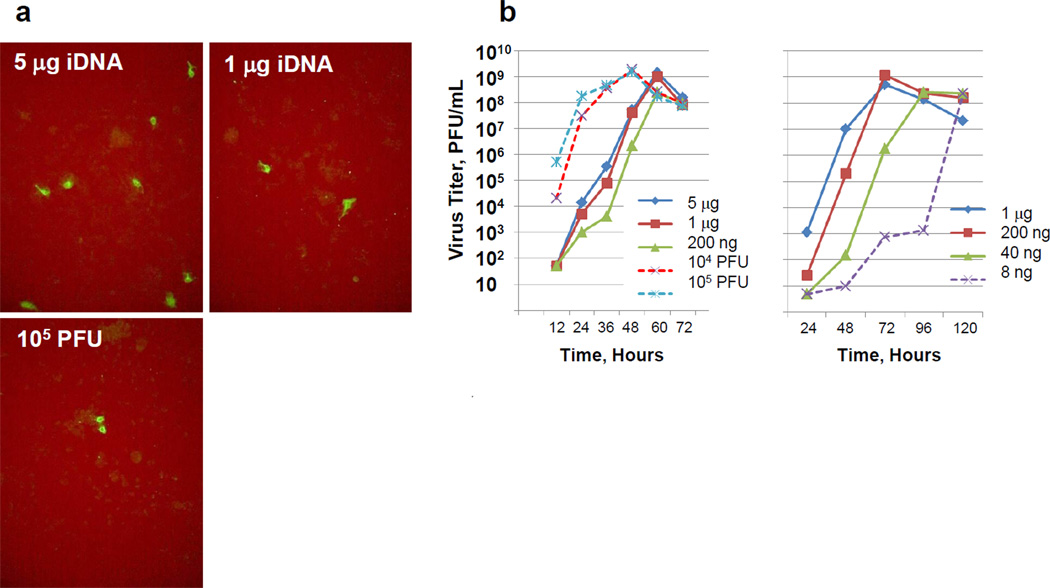
In infected cells (Fig. 1d), virus replicated more rapidly than in iDNA-transfected cells (Fig. 1b). Therefore, in the next experiment, we compared replication kinetics of the virus in (a) iDNA-transfected cells and (b) in TC-83 infected cells. Briefly, 107 of CHO cells in 75 cm2 flasks were either transfected by electroporation with 5 µg, 1 µg, or 200 ng of pTC83 iDNA, or infected with 104 PFU or 105 PFU of the iDNA-derived TC-83 virus. In order to confirm transfection with iDNA or infection with the virus, IFA was carried out using anti-TC-83 antiserum at 9 hr after transfection or infection (Fig. 2a). The number of fluorescent cells expressing TC-83 antigens depended on the amount of iDNA in transfection. For example, transfection with 5 µg resulted in a higher efficacy as compared to transfection with 1 µg of iDNA (Fig. 2a). Transfection of 1 µg of iDNA and infection with 105 PFU of TC-83 virus resulted in a comparable number of antigen-expressing cells (Fig. 2a). Samples of the growth medium were collected from transfected and infected cells every 12 hr and the viruses were quantitated by plaque assay (Fig. 2b). Virus-infected cells rapidly reached maximum titer, whereas in iDNA-transfected cells, a delay in virus replication was observed (Fig. 2b, left panel). In the next experiment, in order to determine if the virus can be generated with a minimal amount of iDNA, CHO cells were transfected with 1 µg, 200 ng, 40 ng, or 8 ng of iDNA. The virus was detected in all transfections, including transfection with 8 ng of plasmid DNA (Fig. 2b, right panel). Virus replication correlated with the amount of iDNA in transfection, and the virus titer reached 108–109 PFU/ml.
Fig. 2. Replication kinetics of TC-83 virus in virus-infected and iDNA-transfected CHO cells.
(a) IFA of CHO cells transfected with 5 µg or 1 µg of iDNA (upper panel) or with 105 PFU of TC-83 virus (lower panel).
(b) Growth curves of TC-83 viruses in virus-infected and in iDNA-transfected CHO cells. Left panel, CHO cells were either infected with 104–105 PFU of virus, or transfected with 0.2–5 µg of pTC83 iDNA. Right panel, CHO cells were transfected with 8 ng to 1 µg of pTC83 iDNA. Plaque titer was determined in duplicates, error bars are not visible at the scale shown.
3.3. Virus generated in vitro from iDNA is attenuated in mice
To confirm that TC-83 virus derived from iDNA had an attenuated phenotype in vivo, we used the virus that was harvested from CHO cells transfected with pTC83 iDNA. Briefly, 104 PFU were inoculated subcutaneously (s.c.) into 10 BALB/c mice in the BSL3 lab. For control purposes, ten BALB/c mice were similarly inoculated with 104 PFU of virulent IAB Trinidad strain of VEEV. All control animals that received Trinidad strain of VEEV, died by day 7 after inoculation (Table 1). In contrast, all mice inoculated with iDNA-derived virus remained healthy with no detectable adverse effects, demonstrating the highly attenuated phenotype of the virus in BALB/c mice.
Table 1.
Virus derived in vitro from pTC83 iDNA is attenuated in BALB/c mice.
| Virus | Dose | Route | Morbidity | Mortality |
|---|---|---|---|---|
| TC-83 virus from iDNAa | 104 PFU | s.c. | 0/10 | 0/10 |
| VEEV, Trinidad strain | 104 PFU | s.c. | 10/10 | 10/10 |
Derived by transfection of CHO cells with pTC83 iDNA containing the full-length RNA of TC-83 virus downstream from the CMV promoter.
3.4. Generation of virus from iDNA in vivo
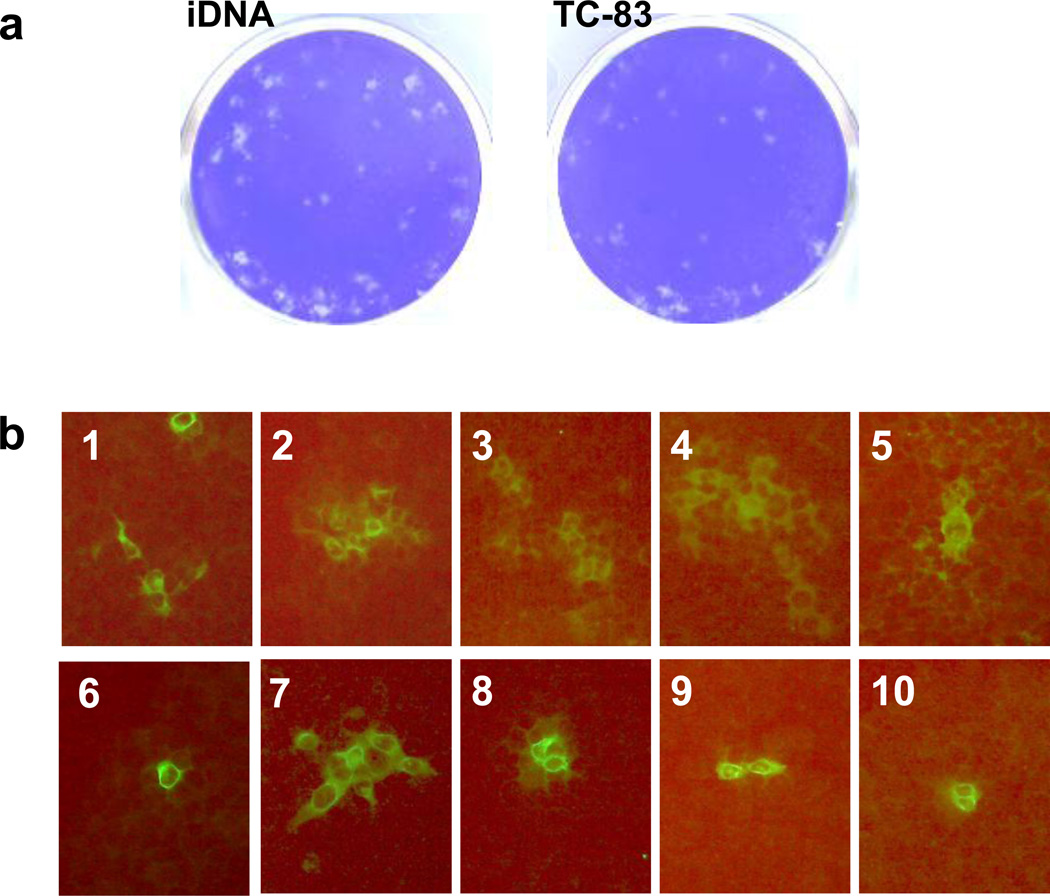
In order to evaluate if iDNA can generate TC-83 vaccine virus in vivo, we injected BALB/c mice with pTC83 iDNA intravenously (i.v.) by using TransIT In Vivo transfection reagent (Mirus, Madison, WI). As a control, another group of mice was injected with 1000 PFU of TC-83 virus subcutaneously (s.c.). Following injections, blood samples were taken and analyzed for viremia. Virus could not be detected by direct plaque assay (detection limit < 50 PFU/ml). However, replicating virus was detected in plasma samples by co-cultivation (amplification) in Vero cells followed by plaque assay (Fig. 3a). RNA was isolated from the recovered virus, and TC-83 fragment nt 8559–9850 containing the entire E2 gene was generated by RT-PCR. The E2 gene encodes the major attenuating mutation E2-120 [23], and the presence of this mutation was confirmed in the virus by cDNA sequencing.
Fig. 3. Detection of TC-83 virus and antibody in vivo.
(a) Detection of viremia in plasma samples collected from pTC83 iDNA-vaccinated BALB/c mice. BALB/c mice were injected intravenously (i.v.) with mixture of pTC83 iDNA and TransIT transfection reagent (Mirus, Madison, WI). Plasma samples were collected on day 1 post inoculation and incubated with Vero cells for virus amplification. At day 3, culture medium was collected and assayed by plaque titration using Vero cell monolayers. Left panel, TC83 virus recovered from plasma of iDNA-inoculated mice. Right panel, virus recovered from plasma after immunization with prototype VEEV TC-83 vaccine.
(b) Detection of serum antibody in the plasma samples 1–10 from pTC83 iDNA-vaccinated BALB/c mice, by IFA. Ten BALB/c mice were vaccinated by electroporation with pTC83 iDNA. Plasma samples from individual mice were collected on day 21 post vaccination and probed with monolayers of CHO cells infected with TC-83-virus at MOI=0.1. Plasma samples were used at 1:20 dilution.
3.5. Immunogenicity and efficacy of iDNA vaccine in mice
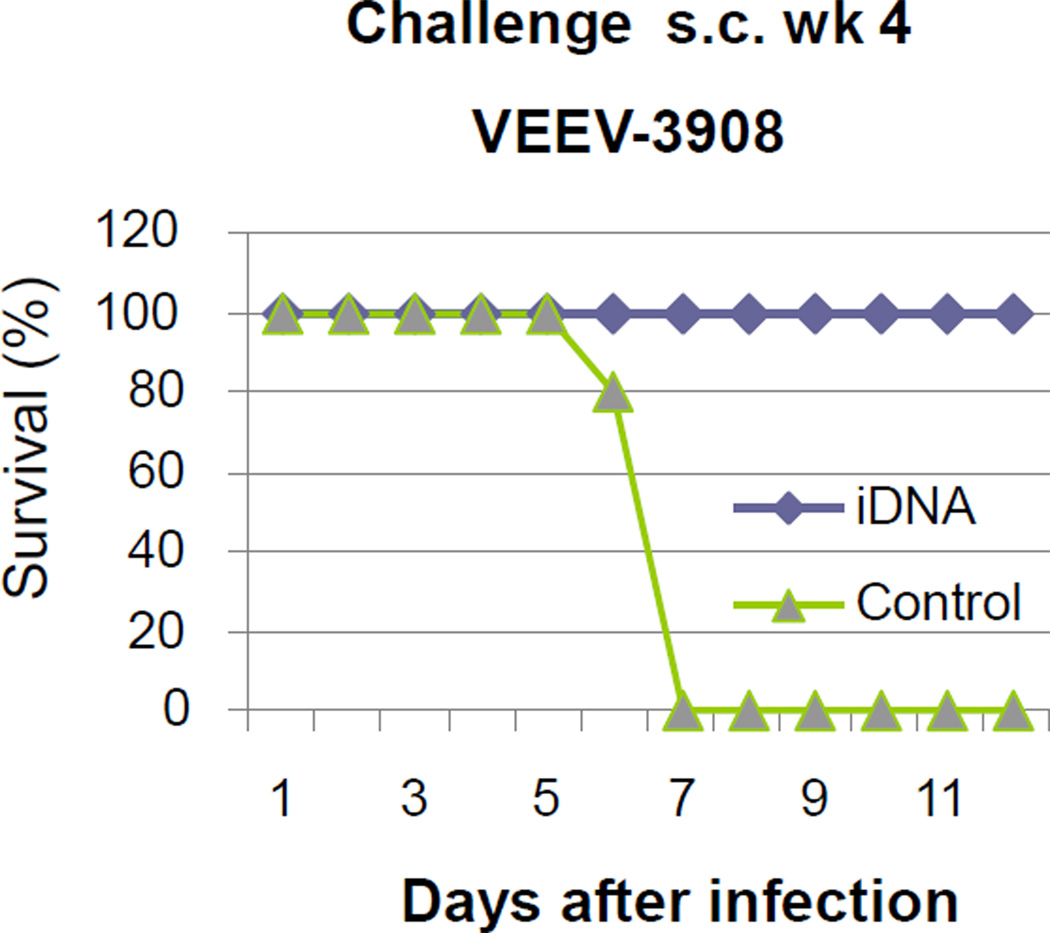
To determine if generation of TC-83 vaccine virus from iDNA in vivo results in induction of protective immune response, ten BALB/c mice were vaccinated with 50 µg of pTC-83 iDNA intramuscularly (i.m.) followed by in vivo electroporation. Animals showed no adverse effects to the procedure and remained healthy after vaccinations, similarly to unvaccinated controls. Blood samples were collected for three days post vaccination for detection of vaccine virus, as well as at day 21 for seroconversion. Vaccine virus was detected in the plasma at day 3 post vaccination by virus amplification as described above. By day 21, all vaccinated mice seroconverted as determined by IFA (Fig. 3b) and by plaque reduction neutralization assay (Table 2). As expected, no antibody to TC-83 (p<0.05) was detected in unvaccinated control animals (Table 2). At day 28 post vaccinations, animals were transferred to the BSL3 facility and challenged s.c. with 105 PFU of virulent IC VEEV-3908 virus [24]. All iDNA-vaccinated animals survived challenge (Fig. 4). Furthermore, five out of ten challenged animals did not have any detectable viremia after challenge (Table 2). The remaining five animals had low-level viremia as compared to unvaccinated control animals. In contrast to iDNA-vaccinated mice, all unvaccinated control animals developed high levels of viremia, lost in average 32% of weight, and succumbed to infection and died by day 7 post challenge (Fig. 4; Table 2).
Table 2.
Immunogenicity and efficacy of pTC83 iDNA vaccine in BALB/c mice.
| Vaccine | No. of animals |
PRNT80, Titer Range (GMT) |
Challenge dose, s.c.a |
Viremia/ Total(%) |
Viremia Range, Log10PFU/mlb |
Survival, % |
|---|---|---|---|---|---|---|
| iDNA | 10 | 10–320 (40.2)c | 105 PFU | 5/10 (50%) | 0.9–3.8 | 10/10 (100%) |
| Mock | 5 | <10 | 105 PFU | 5/5 (100%) | 4.3–5.0 | 0/5 (0%) |
Challenge was done with 1×105 408 PFU in 100 µl of VEE-3908 virus.
Day 1 post-challenge.
In unrelated experiment in BALB/c mice, TC-83 vaccination resulted in the PRNT80 titer of 1:640.
Fig. 4.
Survival of BALB/c mice after challenge with VEEV. Mice were vaccinated by electroporation with 50 µg of pTC83 iDNA. On day 28 after vaccination, mice were transferred into BSL3 facility and challenged s.c. with 105 PFU of VEEV virus. Mice were daily monitored for signs of illness and deaths. Uniform lethality was observed for control mice while all iDNA-vaccinated mice survived challenge.
4. Discussion
VEEV is a veterinary and human pathogen capable of causing explosive outbreaks. Humans and equids can be infected by a wide variety of mosquito vectors, including Culex, Mansonia, Psorophora, and Aedes species [25], and the population of susceptible mosquitoes is already flourishing in the U.S. [9, 26–28]. The initial VEEV symptoms are similar to influenza and are difficult to diagnose [10]. Several approaches to VEEV vaccines are being developed including recombinant subunit [29], inactivated [30–33], DNA [34, 35], and live attenuated vaccines [22, 36, 37]. These approaches resulted in the promising vaccines and have considerably improved understanding of immunity to VEEV. However, in the absence of FDA-approved VEEV vaccines, live attenuated vaccine TC-83 is still the only vaccine in the U.S. used to protect at-risk personnel [38]. TC-83 causes adverse effects in some individuals, while others do not respond to vaccination. A recent study suggests that these differences in the response to vaccine may be determined by variances in activation of immune signaling pathways [38]. However, while several commercial vaccines caused life-threatening complications during clinical use [39], there were no serious life-threatening complications reported for the TC-83 vaccine. Although limited to at-risk individuals, the clinical history of TC-83 may warrant efforts to use it for the development of improved VEEV vaccines. Recently, live vaccines RotaTeq, Zostavax and FluMist have been licensed demonstrating that live vaccines can be configured to meet stringent FDA safety standards [40].
Infectious clone technology has been broadly used for VEEV vaccine development [41, 42]. Since VEEV is a cytoplasmic virus, previous efforts were focused on in vitro transcription and transfection of the full-length RNA in order to generate the virus in vitro [41, 42]. Because of chemical instability, RNA is not suitable for vaccination in vivo. Unlike in the previous studies involving RNA transfection into cytoplasm, in the proposed iDNA approach, the full-length RNA is transcribed in the nucleus and transported into the cytoplasm. Plasmid DNA can easily be highly purified and used in vitro and in vivo. In our experiments, only 8 ng of iDNA was sufficient to start replication of the TC-83 virus in CHO cells (Fig. 2b). A similar approach has been described for Sindbis virus [43]. A method of generating live-attenuated paramyxovirus vaccines in Vero cells entirely from plasmids has been also reported [44]. Racaniello and Baltimore have shown that cultured mammalian cells transfected with plasmid containing cloned complementary DNA copy of the poliovirus RNA genome produced infectious poliovirus [45]. DNA vaccine coding for the full-length infectious Kunjin virus RNA protected mice against the New York strain of West Nile virus [46]. However, to our knowledge this is the first report of using DNA for delivery of known clinical live attenuated vaccine in vivo such as TC-83 vaccine. Our data suggest that iDNA technology may improve the TC-83 vaccine including reducing observed adverse reactions that need to be addressed [16, 47]. Adverse effects have often been associated with reversion mutations [17]. In the TC-83, nucleotide 3 in the 5’ region and amino acid 120 within E2 glycoprotein have been associated with attenuation [23]. However, because RNA viruses, including the TC-83, exist as populations of viruses sometimes called quasispecies [17, 48], genetic variants including reversion mutations may be present in the vaccine virus preparation. Virus passages during vaccine preparation may further contribute to the genetic diversity. By launching the vaccine virus from iDNA in vivo, a greater genetic uniformity of the vaccine virus is achieved, while multiple passages of vaccine virus are avoided, which can minimize the possibility of reversion mutations and improve vaccine safety. Furthermore, vaccine synthesis occurs directly in vivo, which minimizes adverse reactions resulting from the impurities derived from cell culture. Adverse reactions to substrate-derived impurities are known for other vaccines including influenza [49]. Taken together, the iDNA vaccine can minimize the potential for adverse effects due to reversion mutations or adventitious agents. Additionally, vaccine synthesis in vivo and the need for transcription of RNA in the nucleus can explain the delayed virus replication from iDNA (Fig. 3b). Delayed replication may also contribute to safety as compared to standard live vaccines, as this can delay virus entry into the blood stream and organs that potentially can reduce adverse effects.
Furthermore, we hypothesize that iDNA can stimulate immune system via unmethylated CpG motifs of bacterial origin and/or double-stranded structure of DNA that in theory may improve immunogenicity and reduce the number of non-responders, although this remains to be tested. Double-stranded DNA activates the stimulator of interferon genes/TANK-binding kinase 1 (STING/TBK1)-dependent innate immune signaling pathways. Type-I interferons (IFNs), induced in vivo by the STING/TBK1 pathway, were found to be crucial for both direct and indirect antigen presentation via distinct cell types including dendritic and muscle cells [50, 51]. IFN and IFN-induced pathways are involved in the TC-83 vaccination [38]. Other immune modulators may also play role in the virus replication [52].
In summary, the iDNA has genetic and chemical stability of DNA vaccines with no requirement for cold chain. This is important for VEEV geographic areas with warm climate and limited cold chain infrastructure. Furthermore, similarly to live vaccines, iDNA can induce strong protective immunity following a single-dose vaccination as shown in this study. To our knowledge, this is the first report of in vivo delivery of existing clinical live attenuated vaccine by using DNA immunization. More experiments are needed including challenges with higher dose or multiple subtypes of VEEV, studies of the longevity of immune response, persistence of the iDNA vector in vivo, and examination of organs for the signs of replicating virus following vaccination with iDNA. Potentially, the iDNA platform can be configured to other live attenuated virus vaccines and improve their production by eliminating many steps of conventional manufacturing process.
Highlights.
-
-
Novel iDNA platform was used for vaccination against VEEV alphavirus
-
-
Less than 10 ng of pTC83 iDNA initiated replication of the vaccine virus in vitro
-
-
BALB/c mice vaccinated with a single dose of pTC83 iDNA have seroconverted
-
-
After challenge with VEEV, all pTC-83-vaccinated mice were protected
-
-
Proposed platform allows conversion of live attenuated virus into DNA vaccine
Acknowledgements
Authors thank Michael Parker, Elena Klyushnenkova, Marco Goicochea, Ruth Florese, Rachmat Hidajat and Brian Nickols for their contributions to this study. The authors declare that they have no competing financial interests. Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number R43AI094863. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dupuy LC, Schmaljohn CS. DNA vaccines for biodefense. Expert review of vaccines. 2009 Dec;8(12):1739–1754. doi: 10.1586/erv.09.132. [DOI] [PubMed] [Google Scholar]
- 2.Liu MA, Wahren B, Karlsson Hedestam GB. DNA vaccines: recent developments and future possibilities. Human gene therapy. 2006 Nov;17(11):1051–1061. doi: 10.1089/hum.2006.17.1051. [DOI] [PubMed] [Google Scholar]
- 3.Saade F, Petrovsky N. Technologies for enhanced efficacy of DNA vaccines. Expert review of vaccines. 2012 Feb;11(2):189–209. doi: 10.1586/erv.11.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Plotkin SA, Orenstein WA. Vaccines. 4th ed. Philadelphia, Pa: Saunders; 2004. [Google Scholar]
- 5.Smart DL, Trainer DO. Serologic evidence of Venezuelan equine encephalitis in some wild and domestic populations of southern Texas. Journal of wildlife diseases. 1975 Apr;11(2):195–200. doi: 10.7589/0090-3558-11.2.195. [DOI] [PubMed] [Google Scholar]
- 6.Weaver SC, Pfeffer M, Marriott K, Kang W, Kinney RM. Genetic evidence for the origins of Venezuelan equine encephalitis virus subtype IAB outbreaks. Am J Trop Med Hyg. 1999 Mar;60(3):441–448. doi: 10.4269/ajtmh.1999.60.441. [DOI] [PubMed] [Google Scholar]
- 7.Kitchen LW, Vaughn DW. Role of U.S. military research programs in the development of U.S.-licensed vaccines for naturally occurring infectious diseases. Vaccine. 2007 Oct 10;25(41):7017–7030. doi: 10.1016/j.vaccine.2007.07.030. [DOI] [PubMed] [Google Scholar]
- 8.Strauss JH, Strauss EG. The alphaviruses: gene expression, replication, and evolution. Microbiological reviews. 1994 Sep;58(3):491–562. doi: 10.1128/mr.58.3.491-562.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weaver SC, Ferro C, Barrera R, Boshell J, Navarro JC. Venezuelan equine encephalitis. Annual review of entomology. 2004;49:141–174. doi: 10.1146/annurev.ento.49.061802.123422. [DOI] [PubMed] [Google Scholar]
- 10.Lemon SM. Institute of Medicine (U.S.). Committee on a Strategy for Minimizing the Impact of Naturally Occurring Infectious Diseases of Military Importance. National Academies Press; 2002. Protecting our forces: improving vaccine acquisition and availability in the U.S. military. [PubMed] [Google Scholar]
- 11.Paessler S, Weaver SC. Vaccines for Venezuelan equine encephalitis. Vaccine. 2009 Nov 5;27(Suppl 4):D80–D85. doi: 10.1016/j.vaccine.2009.07.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berge TO, Banks IS, Tigertt WD. Attenuation of Venezuelan equine encephalomyelitis virus by in vitro cultivation in guinea-pig heart cells. Am J Trop Med Hyg. 1961;73:209–218. [Google Scholar]
- 13.Grabenstein JD, Pittman PR, Greenwood JT, Engler RJ. Immunization to protect the US Armed Forces: heritage, current practice, and prospects. Epidemiologic reviews. 2006;28:3–26. doi: 10.1093/epirev/mxj003. [DOI] [PubMed] [Google Scholar]
- 14.Hoke CH., Jr History of U.S. military contributions to the study of viral encephalitis. Military medicine. 2005 Apr;170(4 Suppl):92–105. doi: 10.7205/milmed.170.4s.92. [DOI] [PubMed] [Google Scholar]
- 15.Phillpotts RJ, Wright AJ. TC-83 vaccine protects against airborne or subcutaneous challenge with heterologous mouse-virulent strains of Venezuelan equine encephalitis virus. Vaccine. 1999 Feb 26;17(7–8):982–988. doi: 10.1016/s0264-410x(98)00315-6. [DOI] [PubMed] [Google Scholar]
- 16.Pittman PR, Makuch RS, Mangiafico JA, Cannon TL, Gibbs PH, Peters CJ. Long-term duration of detectable neutralizing antibodies after administration of live-attenuated VEE vaccine and following booster vaccination with inactivated VEE vaccine. Vaccine. 1996 Mar;14(4):337–343. doi: 10.1016/0264-410x(95)00168-z. [DOI] [PubMed] [Google Scholar]
- 17.Kenney JL, Volk SM, Pandya J, Wang E, Liang X, Weaver SC. Stability of RNA virus attenuation approaches. Vaccine. 2011 Mar 9;29(12):2230–2234. doi: 10.1016/j.vaccine.2011.01.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coffey LL, Beeharry Y, Borderia AV, Blanc H, Vignuzzi M. Arbovirus high fidelity variant loses fitness in mosquitoes and mice. Proceedings of the National Academy of Sciences of the United States of America. 2011 Sep 20;108(38):16038–16043. doi: 10.1073/pnas.1111650108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weaver SC, Bellew LA, Gousset L, Repik PM, Scott TW, Holland JJ. Diversity within natural populations of eastern equine encephalomyelitis virus. Virology. 1993 Aug;195(2):700–709. doi: 10.1006/viro.1993.1421. [DOI] [PubMed] [Google Scholar]
- 20.Berge TO, Gleiser CA, Gochenour WS, Jr, Miesse ML, Tigertt WD. Studies on the virus of Venezuelan equine encephalomyelitis. II. Modification by specific immune serum of response of central nervous system of mice. Journal of immunology. 1961 Nov;87:509–517. [PubMed] [Google Scholar]
- 21.Messer WB, Yount B, Hacker KE, Donaldson EF, Huynh JP, de Silva AM, et al. Development and characterization of a reverse genetic system for studying dengue virus serotype 3 strain variation and neutralization. PLoS neglected tropical diseases. 2012;6(2):e1486. doi: 10.1371/journal.pntd.0001486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paessler S, Ni H, Petrakova O, Fayzulin RZ, Yun N, Anishchenko M, et al. Replication and clearance of Venezuelan equine encephalitis virus from the brains of animals vaccinated with chimeric SIN/VEE viruses. Journal of virology. 2006 Mar;80(6):2784–2796. doi: 10.1128/JVI.80.6.2784-2796.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kinney RM, Chang GJ, Tsuchiya KR, Sneider JM, Roehrig JT, Woodward TM, et al. Attenuation of Venezuelan equine encephalitis virus strain TC-83 is encoded by the 5'-noncoding region and the E2 envelope glycoprotein. Journal of virology. 1993 Mar;67(3):1269–1277. doi: 10.1128/jvi.67.3.1269-1277.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greene IP, Paessler S, Anishchenko M, Smith DR, Brault AC, Frolov I, et al. Venezuelan equine encephalitis virus in the guinea pig model: evidence for epizootic virulence determinants outside the E2 envelope glycoprotein gene. The American journal of tropical medicine and hygiene. 2005 Mar;72(3):330–338. [PubMed] [Google Scholar]
- 25.Scherer WF, Cupp EW, Dziem GM, Breener RJ, Ordonez JV. Mesenteronal infection threshold of an epizootic strain of Venezuelan encephalitis virus in Culex (Melanoconion) taeniopus mosquitoes and its implication to the apparent disappearance of this virus strain from an enzootic habitat in Guatemala. Am J Trop Med Hyg. 1982 Sep;31(5):1030–1037. doi: 10.4269/ajtmh.1982.31.1030. [DOI] [PubMed] [Google Scholar]
- 26.Brault AC, Powers AM, Ortiz D, Estrada-Franco JG, Navarro-Lopez R, Weaver SC. Venezuelan equine encephalitis emergence: enhanced vector infection from a single amino acid substitution in the envelope glycoprotein. Proceedings of the National Academy of Sciences of the United States of America. 2004 Aug 3;101(31):11344–11349. doi: 10.1073/pnas.0402905101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deardorff ER, Weaver SC. Vector competence of Culex (Melanoconion) taeniopus for equine-virulent subtype IE strains of Venezuelan equine encephalitis virus. Am J Trop Med Hyg. Jun;82(6):1047–1052. doi: 10.4269/ajtmh.2010.09-0556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scherer WF, Weaver SC, Taylor CA, Cupp EW, Dickerman RW, Rubino HH. Vector competence of Culex (Melanoconion) taeniopus for allopatric and epizootic Venezuelan equine encephalomyelitis viruses. Am J Trop Med Hyg. 1987 Jan;36(1):194–197. doi: 10.4269/ajtmh.1987.36.194. [DOI] [PubMed] [Google Scholar]
- 29.Hodgson LA, Ludwig GV, Smith JF. Expression, processing, and immunogenicity of the structural proteins of Venezuelan equine encephalitis virus from recombinant baculovirus vectors. Vaccine. 1999 Mar 5;17(9–10):1151–1160. doi: 10.1016/s0264-410x(98)00335-1. [DOI] [PubMed] [Google Scholar]
- 30.Fine DL, Jenkins E, Martin SS, Glass P, Parker MD, Grimm B. A multisystem approach for development and evaluation of inactivated vaccines for Venezuelan equine encephalitis virus (VEEV) Journal of virological methods. 2010 Feb;163(2):424–432. doi: 10.1016/j.jviromet.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martin SS, Bakken RR, Lind CM, Garcia P, Jenkins E, Glass PJ, et al. Evaluation of formalin inactivated V3526 virus with adjuvant as a next generation vaccine candidate for Venezuelan equine encephalitis virus. Vaccine. 2010 Apr 19;28(18):3143–3151. doi: 10.1016/j.vaccine.2010.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martin SS, Bakken RR, Lind CM, Garcia P, Jenkins E, Glass PJ, et al. Comparison of the immunological responses and efficacy of gamma-irradiated V3526 vaccine formulations against subcutaneous and aerosol challenge with Venezuelan equine encephalitis virus subtype IAB. Vaccine. 2010 Jan 22;28(4):1031–1040. doi: 10.1016/j.vaccine.2009.10.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sharma A, Gupta P, Glass PJ, Parker MD, Maheshwari RK. Safety and protective efficacy of INA-inactivated Venezuelan equine encephalitis virus: implication in vaccine development. Vaccine. 2011 Jan 29;29(5):953–959. doi: 10.1016/j.vaccine.2010.11.033. [DOI] [PubMed] [Google Scholar]
- 34.Dupuy LC, Richards MJ, Ellefsen B, Chau L, Luxembourg A, Hannaman D, et al. A DNA vaccine for venezuelan equine encephalitis virus delivered by intramuscular electroporation elicits high levels of neutralizing antibodies in multiple animal models and provides protective immunity to mice and nonhuman primates. Clin Vaccine Immunol. 2011 May;18(5):707–716. doi: 10.1128/CVI.00030-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dupuy LC, Richards MJ, Reed DS, Schmaljohn CS. Immunogenicity and protective efficacy of a DNA vaccine against Venezuelan equine encephalitis virus aerosol challenge in nonhuman primates. Vaccine. 2010 Oct 28;28(46):7345–7350. doi: 10.1016/j.vaccine.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 36.Paessler S, Fayzulin RZ, Anishchenko M, Greene IP, Weaver SC, Frolov I. Recombinant sindbis/Venezuelan equine encephalitis virus is highly attenuated and immunogenic. Journal of virology. 2003 Sep;77(17):9278–9286. doi: 10.1128/JVI.77.17.9278-9286.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fine DL, Roberts BA, Teehee ML, Terpening SJ, Kelly CL, Raetz JL, et al. Venezuelan equine encephalitis virus vaccine candidate (V3526) safety, immunogenicity and efficacy in horses. Vaccine. 2007 Feb 26;25(10):1868–1876. doi: 10.1016/j.vaccine.2006.10.030. [DOI] [PubMed] [Google Scholar]
- 38.Erwin-Cohen R, Porter A, Pittman P, Rossi C, Dasilva L. Host responses to live-attenuated Venezuelan equine encephalitis virus (TC-83): Comparison of naive, vaccine responder and nonresponder to TC-83 challenge in human peripheral blood mononuclear cells. Human vaccines & immunotherapeutics. 2012 Aug 1;8(8) doi: 10.4161/hv.20300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Update: vaccine side effects, adverse reactions, contraindications, and precautions. Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recommendations and reports : Morbidity and mortality weekly report Recommendations and reports / Centers for Disease Control. 1996 Sep 6;45(RR-12):1–35. [PubMed] [Google Scholar]
- 40.Vaughn JA, Miller RA. Update on immunizations in adults. American family physician. 2011 Nov 1;84(9):1015–1020. [PubMed] [Google Scholar]
- 41.Davis NL, Brown KW, Greenwald GF, Zajac AJ, Zacny VL, Smith JF, et al. Attenuated mutants of Venezuelan equine encephalitis virus containing lethal mutations in the PE2 cleavage signal combined with a second-site suppressor mutation in E1. Virology. 1995 Sep 10;212(1):102–110. doi: 10.1006/viro.1995.1458. [DOI] [PubMed] [Google Scholar]
- 42.Davis NL, Willis LV, Smith JF, Johnston RE. In vitro synthesis of infectious venezuelan equine encephalitis virus RNA from a cDNA clone: analysis of a viable deletion mutant. Virology. 1989 Jul;171(1):189–204. doi: 10.1016/0042-6822(89)90526-6. [DOI] [PubMed] [Google Scholar]
- 43.Steel JJ, Henderson BR, Lama SB, Olson KE, Geiss BJ. Infectious alphavirus production from a simple plasmid transfection+ Virology journal. 2011;8:356. doi: 10.1186/1743-422X-8-356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Surman SR, Collins PL, Murphy BR, Skiadopoulos MH. An improved method for the recovery of recombinant paramyxovirus vaccine candidates suitable for use in human clinical trials. Journal of virological methods. 2007 Apr;141(1):30–33. doi: 10.1016/j.jviromet.2006.11.024. [DOI] [PubMed] [Google Scholar]
- 45.Racaniello VR, Baltimore D. Cloned poliovirus complementary DNA is infectious in mammalian cells. Science (New York, NY. 1981 Nov 20;214(4523):916–919. doi: 10.1126/science.6272391. [DOI] [PubMed] [Google Scholar]
- 46.Hall RA, Nisbet DJ, Pham KB, Pyke AT, Smith GA, Khromykh AA. DNA vaccine coding for the full-length infectious Kunjin virus RNA protects mice against the New York strain of West Nile virus. Proceedings of the National Academy of Sciences of the United States of America. 2003 Sep 2;100(18):10460–10464. doi: 10.1073/pnas.1834270100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Steele KE, Davis KJ, Stephan K, Kell W, Vogel P, Hart MK. Comparative neurovirulence and tissue tropism of wild-type and attenuated strains of Venezuelan equine encephalitis virus administered by aerosol in C3H/HeN and BALB/ c mice. Veterinary pathology. 1998 Sep;35(5):386–397. doi: 10.1177/030098589803500508. [DOI] [PubMed] [Google Scholar]
- 48.Khromava AY, Eidex RB, Weld LH, Kohl KS, Bradshaw RD, Chen RT, et al. Yellow fever vaccine: an updated assessment of advanced age as a risk factor for serious adverse events. Vaccine. 2005 May 9;23(25):3256–3263. doi: 10.1016/j.vaccine.2005.01.089. [DOI] [PubMed] [Google Scholar]
- 49.Pushko PRB, Tumpey T, Smith G. Engineering Better Influenza Vaccines: Traditional and New Approaches. In: Khudyakov YE, editor. Medicinal Protein Engineering. Boca Raton: CRC Press; 2009. pp. 169–204. 2009. [Google Scholar]
- 50.Coban C, Koyama S, Takeshita F, Akira S, Ishii KJ. Molecular and cellular mechanisms of DNA vaccines. Human vaccines. 2008 Nov-Dec;4(6):453–456. doi: 10.4161/hv.4.6.6200. [DOI] [PubMed] [Google Scholar]
- 51.Coban C, Kobiyama K, Aoshi T, Takeshita F, Horii T, Akira S, et al. Novel strategies to improve DNA vaccine immunogenicity. Current gene therapy. 2011 Dec;11(6):479–484. doi: 10.2174/156652311798192815. [DOI] [PubMed] [Google Scholar]
- 52.Kehn-Hall K, Narayanan A, Lundberg L, Sampey G, Pinkham C, Guendel I, et al. Modulation of GSK-3beta activity in Venezuelan equine encephalitis virus infection. PloS one. 2012;7(4):e34761. doi: 10.1371/journal.pone.0034761. [DOI] [PMC free article] [PubMed] [Google Scholar]