Abstract
Background:
Dry socket is one of the most prevalent complications occurring after tooth extraction. The prevalence of such condition has been reported to be highly different, ranging from 0.5 to 68.4%. The etiology and pathogenesis of this entity are not clearly known and many related predisposing factors have been discussed. The goal of this study was to evaluate the relative prevalence of this entity after tooth extraction and determine the contributing factors in patient referring to Yazd dental clinics.
Materials and Methods:
This cross-sectional prospective study was carried out at Yazd dental clinics (from May 2010 to Jun 2010). Four thousand seven hundred and seventy nine patients were selected and included in our study. Characteristics such as: age, gender, site of extraction, number of extracted tooth, trauma during extraction, oral hygiene, smoking, systemic disease, menstrual cycle, history of dental infection and oral contraceptive pill intake were determined and data was analyzed using descriptive statistical analysis and Fisher's exact test. P value ≤0.05 was considered significant.
Results:
Over the two-month period of the study, among of 4,779 patients, 28 patients returned with dry socket phenomena. Our results showed that the incidence of dry socket was 0.6% and females were more common involved than males (0.08% versus 0.04%). The ratio of mandible to maxilla was 2.5 to1 and mandibular third molars were more often involved than other teeth. Trauma, poor oral hygiene and smoking had increased the incidence of dry socket.
Conclusion:
The results of our study suggested that trauma during surgery or extraction and poor oral hygiene are important factors that increase the incidence of dry socket, these factors should be considered before and after tooth extractions.
Keywords: Dry socket, oral surgery, tooth extraction
INTRODUCTION
Dry socket is the most common complication after tooth extraction.[1] The clinical features of this complication including severe throbbing pain, oral malodor and unpleasant taste. Onset of symptoms is 42-72 h after tooth extraction and there is no any redness or purulent discharge of the affected sites.[1,2]
The main complaint of affected patient is severe pain that causes impairment in daily activities. This pain can be referred to forehead, ears and neck and is resistant to pain relief drugs.[2]
The pathogenesis of this pain after extraction is not completely known, but several factors have been suggested as predisposing factors including trauma to the alveolar socket, infection at the site of tooth extraction, presence of vasoconstrictor in local anesthesia, smoking, intake of oral contraceptive pill (OCP), menstruation, residual foreign bodies, root segments in alveolar bone, extra irrigation or severe curettage, ejection of saliva after extraction. The numbers of tooth extractions and the amount of bleeding may also be effective.[3]
Treatment of this condition needs correct diagnosis that can be facilitated by its clinical symptoms including unusual severe pain, lack of a blood clot in the socket, presence of necrotic material and oral malodor. Because of its unknown etiology, the treatment is only palliative intervention with prescribing anti-inflammatory drugs. For prevention of dry socket some drugs have been suggested like anti-fibrinolytic, irrigation, disinfectants and topical antibiotics.[4,5]
MATERIALS AND METHODS
This cross-sectional prospective study consisted of patients referred to Yazd dental clinics for tooth extraction from May 2010 to Jun 2010.
Four thousand seven hundred and seventy nine patients were selected and included in our study. A questionnaire with relevant information including age, gender, site of tooth extraction, history of systemic disease, drug sensitivity, smoking, intake of OCP, women menstrual status, level of oral hygiene, tooth extraction with damage, curettage and extra irrigation, previous dental infections and used methods to relief pain, was filled for all samples. Among them, just 28 patients returned with dry socket phenomena. All collected data was analyzed by SPSS software using descriptive analysis and Fisher exact test. P value ≤0.05 was considered significant.
RESULTS
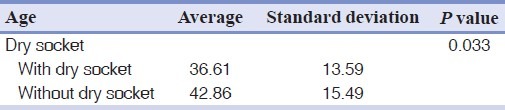
During 2-months of our study, only 28 people were diagnosed with dry socket. In our study, the average age of people with dry socket was 36.61±13.59 years and without dry socket 42.86±15.49 years [Table 1].
Table 1.
Mean age in the group with and without dry socket
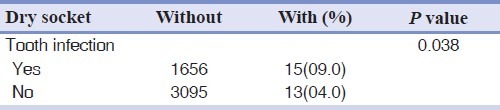
The results presented higher prevalence in female than male (0.08% versus 0.04) [Table 2] and lower jaw was more involved than upper jaw (2.5 times) [Table 3]. The incidence of dry socket in teeth extractions without injury had been reported 0.04% while in damage cases were 1% [Table 4]. Tooth infection also showed statistical significant difference (P=0.038) [Table 5].
Table 2.
Dry socket distribution based on gender
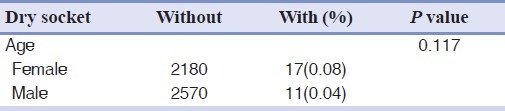
Table 3.
Dry socket distribution based on extraction sit
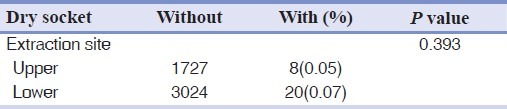
Table 4.
Dry socket distribution based on tooth injury
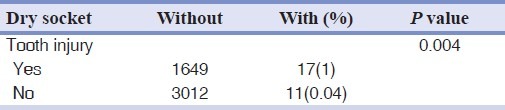
Table 5.
Dry socket distribution based on tooth infection
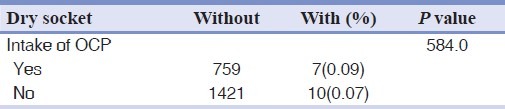
Also some factors such as smoking, taking OCP and menstruation increased the chance of dry socket development, but these relations did not show any significant statistical difference (P=0.911, 0.584 and 0.302 respectively) [Tables 6–8].
Table 6.
Dry socket distribution based on smoking
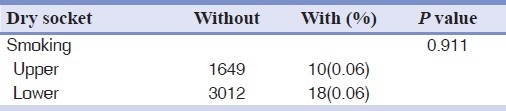
Table 8.
Dry socket distribution based on menstruation status
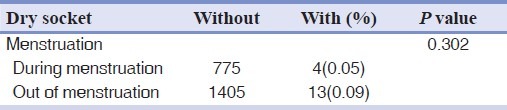
Table 7.
Dry socket distribution based on oral contraceptive pill intake
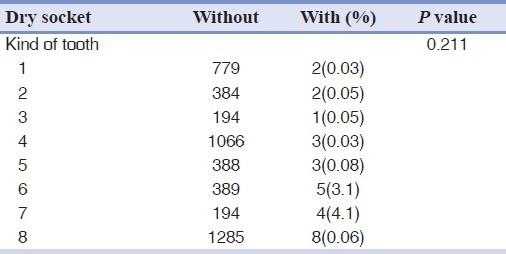
The more affected teeth in this study were third molar, first molar, second molar, premolars, canine and incisors, respectively. But the difference was not statistically significant (P=0.211) [Table 9].
Table 9.
Dry socket distribution based on kind of tooth
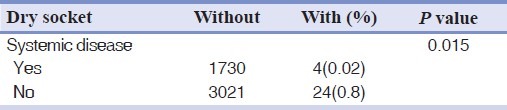
The incidence of dry socket differed significantly with the level of oral hygiene and patients systemic disease. (0.015 and 0.004 respectively) [Tables 10 and 11].
Table 10.
Dry socket distribution based on oral health level
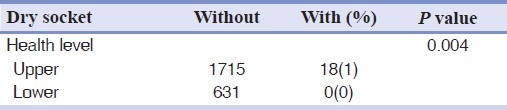
Table 11.
Dry socket distribution based on systemic disease
Totally, some factors showed significant correlation with dry socket occurrence including age, tooth infection, level of hygiene and systemic disease while other did not show any significant difference.
DISCUSSION
The most common complication after tooth extraction is dry socket. A distinct etiology is not determined, but generally increase of fibrinolytic activities is considered as main etiologic factor that can dissolve the blood clot. When some anti-fibrinolytic agents were placed at the site of tooth extraction, incidence of dry socket was reduced.[1]
Surgical damage leading to release of different tissue agents and inoculation of bacterial agents are two main factors for beginning of local fibrinolytic activities.[2]
The prevalence of dry socket in the present study was 0.6% that approximately was lower than previous studies, that it may be related to racial and geographical factors. Amaratunga[6] (3.5%), Wagaiya[7] (3.3%), Ogini[8] (4.1%), Larsen[9] (4.8%), Ognnlewe[10] (5.6%), Singh[11] (2%), Bortoluzi[12] (0.6%), Khorasani[13] (0.85%) and Kadkhodaei[14] (2.9%) have reported these prevalence. These wide ranges of prevalence are probably related to the differences between diagnostic criteria of this condition.
In our study, the average age of people with dry socket was 36.61±13.59 years and without dry socket 42.86±15.49 years similar to the Ogunlewe[10] and Khorasani[13] study. It can be attributed to more acute periodontal infection and pericoronitis in this age range.[3,4] Generally, this complication can be seen more during third molar surgery and in fourth decade of life.[5]
The prevalence of dry socket incidence in our study in female was more than male (0/8% versus 0/4%) but the difference was not statistically significant. Amaratunga,[6] Ognnlewe,[10] Wagaiya,[7] Ogini[8] and Khorasani[13] reported same results with predisposing factors such as malnutrition, iron and vitamin deficiencies, usage of oral contraceptive and menstruation in women. Although, the incidence of dry socket in females are more than males, but did not show any statistical significant differences (P=0.117).
In this study, the incidence of dry socket in mandible was more than maxilla (0.07 versus 0.05) but it was not statistically significant (P=0.393).
Similar to Khorasani[13] et al. study, incidence of mandible was 2/5 times, while in Ogini[15] was 3 times more than maxilla. This can be attributed to better blood supply to the maxillary tooth. Some researchers believe that the etiology of more incidence of dry socket in lower jaw is related to more bone density, lower blood supply and reduced capacity of granulation tissue production.[5–8]
The more affected teeth in this study were third molar, first molar, second molar, premolars, canine and incisors, respectively. Approximately same as Khorasani,[13] Wagaiyu[7] and Upadhyaya[16] studies. The more involvement of third molar can be attributed to more bone thickness in this area, wideness of roots, lack of easy access for cleansing surgical site by the patients, and in addition, the amounts of the mandibular third molar surgery in respect to other teeth extraction.[5,10]
The incidence of dry socket in teeth extractions without injury had been reported 0.4% while in damage cases were 1% comparable to previous studies.[5,6,12,13,17,18]
Also, the incidence of dry socket in cases with history of tooth infection was 0.09% and in cases without infection was 0.04% that was statistically significant. Similar results were reported by Khorasani,[13] Hashemi[19] and Ogini.[15]
Relative distribution of dry socket in addicted and non addicted individuals was not statistically significant (P=0.911) while Fazakerley,[20] Bortoluzzig[12] and Khorasani[13] reported different findings. Also the incidence of dry socket differed significantly with the level of hygiene and/or their systemic disease (0.015 and 0.004 respectively).
CONCLUSION
The results of our study suggested that trauma during surgery or extraction and poor hygiene are important factors that increase the incidence of dry socket, these factors should be considered before and after tooth extractions.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Heasman PA, Jacobs DJ. A clinical investigation into the incidence of dry socket. Br J Oral Maxillofac Surg. 1984;22:115–22. doi: 10.1016/0266-4356(84)90023-8. [DOI] [PubMed] [Google Scholar]
- 2.Swanson AE. A double-blind study on the effectiveness of tetracyclin in reducing the incidence of fibrinolyticalveolitis. J Oral Maxillofac Surg. 1989;47:165–7. doi: 10.1016/s0278-2391(89)80110-7. [DOI] [PubMed] [Google Scholar]
- 3.Torres-Lagares D, Serrera-Figallo MA, Romero-Ruíz MM, Infante-Cossío P, García-Calderón M, Gutiérrez-Pérez JL. Update on dry socket: a review of the literature. (77-81).Med Oral Patol Oral Cir Bucal. 2005;10:81–5. [PubMed] [Google Scholar]
- 4.Birn H. Etiology and pathogenesis in fibrinolyticalveolitis (dry socket) Int J Oral Surg. 1973;2:211–63. [Google Scholar]
- 5.MacGregor AJ. Aetiology of dry socket: A clinical investigation. Br J Oral Surg. 1968;6:49–58. doi: 10.1016/s0007-117x(68)80026-5. [DOI] [PubMed] [Google Scholar]
- 6.Amaratunga NA, Senaratne CM. A clinical study of dry socket in Sri Lanka. Br J Oral Maxillofac Surg. 1988;26:410–8. doi: 10.1016/0266-4356(88)90094-0. [DOI] [PubMed] [Google Scholar]
- 7.Wagaiyu EG, Kaimenyi JT. Frequency of alveolar osteitis (dry socket) at Kenyatta National Hospital Dental Outpatient Clinic–a retrospective study. East Afr Med J. 1989;66:658–62. [PubMed] [Google Scholar]
- 8.Oginni FO, Fatusi OA, Alagbe AO. A clinical evaluation of dry socket in a Nigerian teaching hospital. J Oral Maxillofac Surg. 2003;61:871–6. doi: 10.1016/s0278-2391(03)00248-9. [DOI] [PubMed] [Google Scholar]
- 9.Larsen PE. The effect of a chlorhexidine rinse on the incidence of alveolar osteitis following the surgical removal of impacted third molars. J Oral Maxillofac Surg. 1991;49:932–7. doi: 10.1016/0278-2391(91)90055-q. [DOI] [PubMed] [Google Scholar]
- 10.Ogunlewe MO, Adeyemo WL, Ladeinde AL, Taiwo OA. Incidence and pattern of presentation of dry socket following non-surgical tooth extraction. Nig Q J Hosp Med. 2007;17:126–30. [PubMed] [Google Scholar]
- 11.Singh AS, Mohamed A, Bouckaert MM. A clinical evaluation of dry sockets at the Medunsa Oral Health Centre. (492-3).SADJ. 2008;63:490. [PubMed] [Google Scholar]
- 12.Bortoluzzi MC, Manfro R, De Déa BE, Dutra TC. Incidence of dry socket, alveolar infection, and postoperative pain following the extraction of erupted teeth. J Contemp Dent Pract. 2010;11:e033–40. [PubMed] [Google Scholar]
- 13.Khorasani M, Razavi F. The prevalence and risk factors of dry socket in dental surgery clients following tooth extraction at Qazvin Faculty of Dentistry JQUMS. 2006;10:29–35. [Google Scholar]
- 14.Kadkhodaei M, Asadi A. Incidence of dental dry socket following tooth extraction. Gilan Medi Sci Univ. 1385;62:25–20. [Google Scholar]
- 15.Oginni FO. Dry socket: A prospective study of prevalent risk factors in a Nigerian population. J Oral Maxillofac Surg. 2008;66:2290–5. doi: 10.1016/j.joms.2008.01.063. [DOI] [PubMed] [Google Scholar]
- 16.Upadhyaya C, Humagain M. Prevalence of dry socket following extraction of permanent teeth at Kathmandu University Teaching hospital (KUTH), Dhulikhel, Kavre, Nepal: A study. Kathmandu Univ Med J. 2110;8:18–24. doi: 10.3126/kumj.v8i1.3216. [DOI] [PubMed] [Google Scholar]
- 17.Bergduhl M, Hedstrom L. Metronidazole for the prevention of dry socket after removal of partially impacted mandibular third molar. Br J Oral Maxillofac Surg. 2004;42:555–8. doi: 10.1016/j.bjoms.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 18.Johnson WS, Blanton EE. An evaluation of 9-aminoacridine\gelfoam to reduce dry socket formation. Oral Surg Oral Med Oral Pathol. 1988;66:167–70. doi: 10.1016/0030-4220(88)90086-2. [DOI] [PubMed] [Google Scholar]
- 19.Hashemi M. Evaluation of the amount of dry socket incidence in reffering patients to the dental school of Tehran University. Tehran Med Sci J. 1380;14:5–11. [Google Scholar]
- 20.Fazakerley M, Field EA. Dry socket: A painful post-extraction complication (a review) Dent Update. 1991;18:31–4. [PubMed] [Google Scholar]


