Abstract
The platform switching (PLS) concept was introduced in the literature in 2005. The biological benefits and clinical effectiveness of the PLS technique have been established by several studies. In this article different aspects of PLS concept are discussed. Crestal bone loss, biologic width, and stress distribution in this concept are comprehensively reviewed. In this article the relative published articles from 1990 to 2011 have been evaluated by electronic search. Because of controversial results especially in immediate loading and animal studies, further modified research is needed to establish the mechanism and effect of the PLS technique. Essential changes in studies including using the control group for accurate interpretation of results and long-term observation, particularly through, randomized, prospective, multicenter trials with large numbers of participants, and implants are necessary.
Keywords: Alveolar bone loss, dental implants, dental implant-abutment design, platform switching
INTRODUCTION
In 1991, 3i Implant Innovations (BIOMET 3i Inc., FL) aimed to construct wide-diameter implants with the larger diameter restorative platforms than standard implants. But, for some time, corresponding prosthetic components were unavailable; hence, standard prosthetic abutments (4.1 mm diameter) were used instead of abutments that matched the 5 and 6 mm implant diameters. The consequence of this form of treatment was an unintentional “change of platform”, which became known as platform switching (PLS).[1] This concept was introduced in the literature by Lazzara and Porter, and Gardner.[1,2]
The biological benefits and clinical effectiveness of the PLS technique have been established by several studies.[3–7] In this article different aspects of platform switching concept will be discussed. Crestal bone loss, biologic width, and stress distribution in this concept will be comprehensively reviewed.
CRESTAL BONE LOSS AND PLS
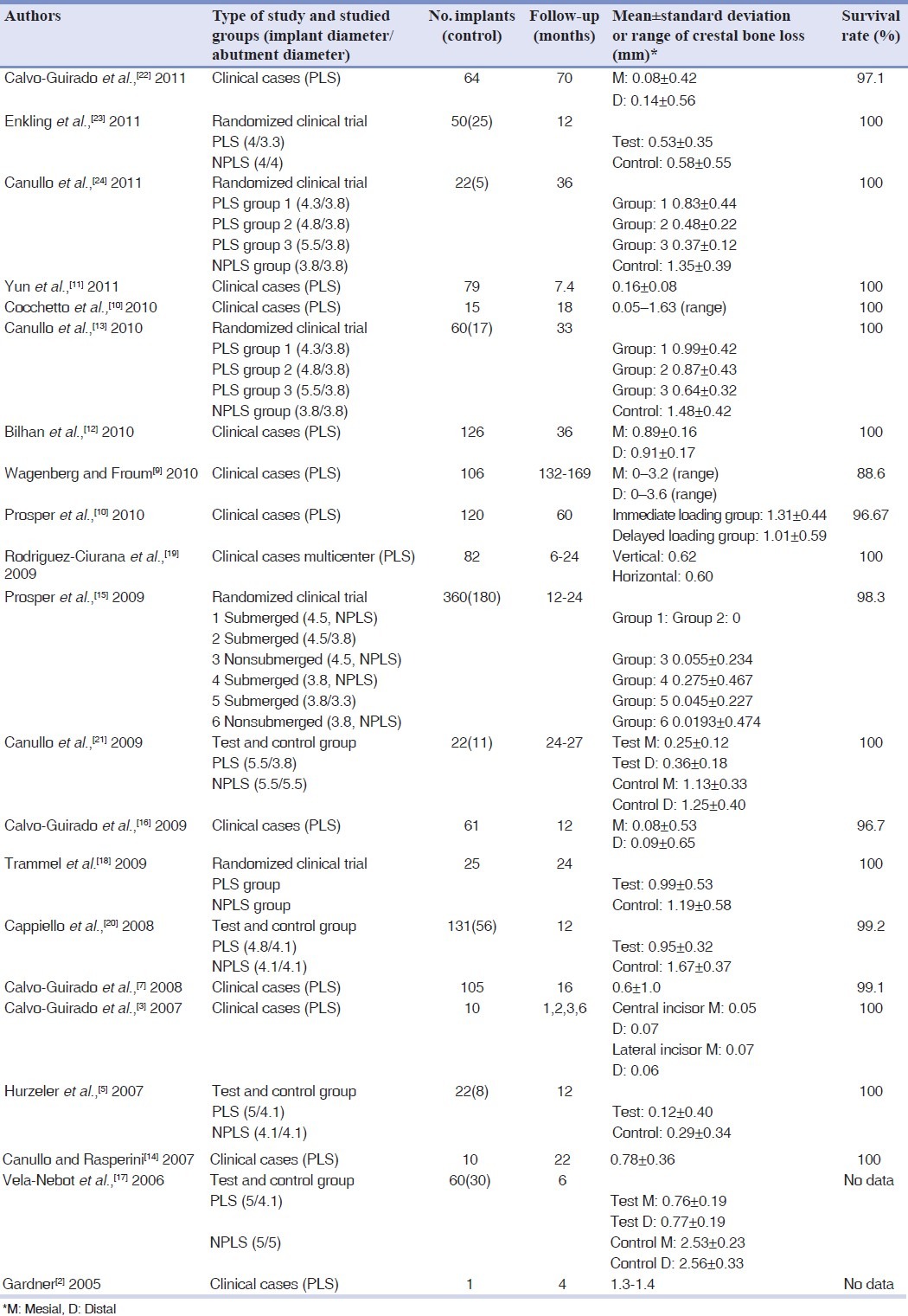
In the studies on PLS, including data with a follow-up period of 4–169 months, the documented bone loss varies between 0.05 and 1.4 mm [Table 1].[2,3,5,7–24]
Table 1.
Investigations regarding crestal bone loss of platform switching (PLS) and nonplatform switched (NPLS) implants
Crestal bone loss is a major criterion for implant success, which includes the evaluation of crestal bone level changes over time.[25–27] This has been the initial diagnostic instrument used to depict periimplant states.[28,29] Albrektsson et al.,[25] Lang et al.,[30] and Roos et al.,[31] determined that a successful implant is defined in terms of marginal bone loss around an implant restoration, with no more than 1.5 mm during the first year and no more than 0.2 mm during each succeeding year. Bone resorption around the implant neck is frequently observed after loading by a reduction in bone dimension, both horizontally and vertically,[32] and appears to depend on both biological and mechanical factors, such as surgical trauma to the periosteum,[33] characteristics of the implant neck design,[34,35] location of the implant/abutment joint,[3] micromovements of the implant, and prosthetic components,[3,36] the size of the microgap between the implant and the abutment,[37] bacterial colonization of the implant sulcus,[38] biologic width,[39] and imbalance in the host parasite equilibrium.[40]
Cappiello et al.,[20] in a clinical and radiographic prospective study showed that PLS decreased bone resorption to 0.95 mm compared to 1.67 mm in the control group. The aim of the study was to evaluate the biologic effect of PLS.
Prosper et al.,[15] in the first randomized prospective study of 360 implants, compared expanded platforms versus cylindrical implants involving abutments of the same size, placed in 60 partially edentulous patients. The results showed lower amount of bone loss in the group with reduced platforms, with the preservation of up to 98.3% versus 66.1% after 12 months, and 97.2% versus 53.3% after 2 years for two groups respectively.
Several controlled clinical trials have shown that implants with PLS had significantly less bone resorption compared with traditional matching implant–abutment connection.[5,17,20] Canullo et al.[13] in a randomized controlled trial study established a relationship between the extent of PLS and the amount of marginal bone loss for the first time.
Wagenberg and Froum[9] in a prospective study evaluated implant survival, and crestal bone levels around implants that used the PLS concept and followed for a minimum of 11 years. Seventy-one of the 94 implants (75.5%) showed no bone loss on the mesial aspect, and 67 implants (71.3%) showed no bone loss on the distal aspect. This is the longest follow-up to a prospective investigation of platform-switched implants and confirms the concept for preservation of crestal bone levels.
The beneficial effect of PLS on bone loss in immediate loading or placement studies remains controversial, because most studies do not have the control group.[3,4,14,16]
Crespi et al.,[41] revealed the influence of PLS on crestal bone level changes at 1, 3, 6, 12, and 24 months. Implants with PLS (n=30), and external hexagon (n=34), were positioned immediately after tooth extraction and were loaded immediately. Results showed no differences in bone level changes between PLS, and conventional external-hexagons implants after 24 months. Canullo et al.,[21] evaluated bone level response around single, immediately placed and provisionalized PLS implants. The mean follow-up period was 25 months and the average bone resorption level in the PLS group (0.3±0.16 mm) was smaller than that in the non-PLS group (1.10±0.35 mm), and this difference was statistically significant (P<0.005).
BIOLOGIC WIDTH AND PLS
The periimplant soft-tissue seal comprise of a junctional epithelium and connective tissue. This biologic soft-tissue coats the implant supporting bone in a 3 to 4 mm wide zone.[42,43]
Cochran et al.,[39] and Hermann et al.,[44] were reported preimplant histometric outcomes and confirmed the presence of biologic width. This is true for any implant patients, whether on one-stage or in two-stage placement protocols on two-piece implants.[42,44,45] Tarnow et al.,[46,47] showed that not only this width progresses apically, but also a lateral component of the biologic width exists around implants. This lateral component varies from 1.04 mm when two adjoining implants are placed less than 3 mm apart to 0.45 mm when the implants are placed more than 3 mm apart.
Inhibition of bone resorption is an important factor in achieving good esthetic results in the maxillary aesthetic zone and providing sufficient bone to support the implants. Vertical bone resorption, which often extends 1–2 mm below the implant-abutment interface, may lead to a possible biomechanical disadvantage by increasing stress values at the bone-implant interface.[44,45] Horizontal bone loss may cause resorption of the buccal plate, loss of the interproximal bone peak, and loss of support for the adjacent interimplant papilla.[47]
Results from Lazzara and Porter[1] showed the history and importance of the microgap and the reconstruction of a biologic width around dental implants.
The saucerization procedure leads to wound healing by means of lack of bone apposition, and fibrous scar tissue formation. This zone of connective tissue is infiltrated by chronic inflammatory cells and is always present around the implant–abutment junction (IAJ) of two-piece implant systems.[20] Ericsson et al.,[38,48] have identified an inflammatory connective tissue (ICT) zone infiltrate in the junctional epithelium of the periimplant mucosa. This inflammatory zone developed vertically for about 0.5–0.75 mm coronal and 0.5–0.75 mm apical to the implant–abutment junction (IAJ). An approximately 1 mm wide layer of healthy connective tissue separates the ICT from bone.[49] This tissue provides protection and reinforcement of the crestal bone, by prevention the passage of microorganisms.[43] In an experimental study in dog, the thickness of this mucosal seal was approximately 3 mm and intentional reduction of this protective layer to 2 mm or less lead to greater crestal bone loss.[42]
Luongo et al.,[49] reported that at the IAJ, it was possible to clearly distinguish a zone of ICT infiltrate in which the presence of plasma cells and lymphocytes was detectible. A noteworthy finding was that this inflammatory infiltrate extended vertically for 0.35 mm coronal to the IAJ along the healing abutment, while in the horizontal direction, it did not exceed the length of the implant with PLS. Rodriquez-Ciurana et al.,[19] indicated that the biologic width around the platform-switched implants are located more coronally than the biologic width around the nonplatform switched implants.
In animal experiments Becker et al.,[50,51] could not differentiate the PLS and control groups statistically but concluded that PLS could prevent the apical down-growth of the barrier epithelium in 28 days.
The PLS technique causes the margin of the IAJ inward, toward the central axis of the implant. The inward movement of the IAJ is believed to shift the inflammatory cell infiltrate to the central axis of the implant and away from the adjacent crestal bone, which is thought of limiting crestal bone resorption. This may result in a reduced inflammatory effect within the surrounding soft tissue and crestal bone. Consequently, (I) a biologic width dimension forms without an increase in loss of crestal bone around dental implants; (II) the relative impact of bacterial leakage at the microgap on bone remodeling around dental implants decreases; and (III) soft-tissue levels that helps to avoid esthetic deformities, phonetic problems, and food impaction preserves.
STRESS–STRAIN RESPONSE AND PLS
Several studies have described methods (photoelastic analysis, strain gauge placement, finite-element analysis (FEA)) for evaluating the biomechanical advantages of the PLS.[52–59] Maeda et al.,[56] in a FEA concluded that the PLS configuration shifted the stress concentration away from the peri-implant marginal bone but increases the stress in the abutment or the abutment screw. Canullo et al.,[60] performed a 3D finite element analysis on three different implant abutment configurations: A 3.8 mm implant with a matching diameter abutment (Standard Control Design, SCD), a 5.5 mm implant with matching diameter abutment (Wider Control Design, WCD), and a 5.5 mm implant with a 3.8 mm abutment (Experimental Design, ED). Their results showed that the ED configuration minimized the stresses at the implant/abutment interface region. This reduction was 160% compared to SCD and 33% compared to WCD. Pessoa et al.,[61] in a computed tomography-based three-dimensional FEA demonstrated that the platform-switched designs can be considered a valid treatment option, equivalent to the conventional matching diameter abutment–implant configurations.
Pellizzer et al.,[59] in a photoelastic analysis found no significant difference between wide-diameter and PLS implants with respect to the magnitude of stress but stress concentration decreased in the cervical region of the platform-switching implant.
Sabet et al.,[57] using strain gages evaluated the effect of PLS on strain developed around implants supporting mandibular overdenture. The results showed that the increasing amount of strain developed because decreasing the abutment size does not favor the use of PLS in implant-supported mandibular overdentures.
Stress concentrations on PLS implants are located at the center of the implant–abutment joint (at the level of the implant screw) will be helpful in reducing crestal bone resorption.
REVENUE OF PLS
Concerns exist about loss of implant papilla and exposing the metal collar at the implant shoulder in the esthetic zone.[62–67] As a consequence, the PLS technique has been developed to either preserve or regenerate the interimplant soft tissue and impede an unsightly metal display.
In a situation in which limitation of the residual bone height, poor-quality bone, and narrow edentulous sectors exist and cannot be resolved, an alternative approach, which may possibly be used to overcome these problems, is the PLS technique.
Differences in interpretation of function of the PLS technique have been noted in several studies.[11,17,44,56,68] However, clinical advantages of the PLS technique may be the cause of a reduction in the crestal bone loss and maintaining the counterpart soft tissue around the implant. Therefore, PLS can preserve soft and hard tissues and may provide better biological, mechanical, and esthetic outcomes.
CONCLUSION
Because of controversial results especially in immediate loading and animal studies, further modified research is needed to establish the mechanism and effect of the PLS technique. Therefore, essential changes in studies including using the control group for accurate interpretation of results and long-term observation, particularly through, randomized, prospective, multicenter trials with large numbers of participants and implants are necessary.
The four common clinical conditions requiring a selective PLS technique are as follows:
Where anatomic structures such as the sinus cavity, the nasal floor, the incisive canal, and the alveolar nerve limit the residual bone height.
Where implants must be placed less than 3 mm apart (between 1.5 and 3 mm) in narrow edentulous sectors.
Where using short implants and in atrophic areas.
When achieving good esthetic results in the anterior maxilla is more important.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Lazzara RJ, Porter SS. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26:9–17. [PubMed] [Google Scholar]
- 2.Gardner DM. Platform switching as a means to achieving implant esthetics. N Y State Dent J. 2005;71:34–7. [PubMed] [Google Scholar]
- 3.Calvo Guirado JL, Saez Yuguero MR, Pardo Zamora G, Munoz Barrio E. Immediate provisionalization on a new implant design for esthetic restoration and preserving crestal bone. Implant Dent. 2007;16:155–64. doi: 10.1097/ID.0b013e31805816c9. [DOI] [PubMed] [Google Scholar]
- 4.Degidi M, Iezzi G, Scarano A, Piattelli A. Immediately loaded titanium implant with a tissue-stabilizing/maintaining design (‘beyond platform switch’) retrieved from man after 4 weeks: A histological and histomorphometrical evaluation. A case report. Clin Oral Implants Res. 2008;19:276–82. doi: 10.1111/j.1600-0501.2007.01449.x. [DOI] [PubMed] [Google Scholar]
- 5.Hurzeler M, Fickl S, Zuhr O, Wachtel HC. Peri-implant bone level around implants with platform-switched abutments: Preliminary data from a prospective study. J Oral Maxillofac Surg. 2007;65(7 Suppl 1):33–9. doi: 10.1016/j.joms.2007.03.024. [DOI] [PubMed] [Google Scholar]
- 6.Baumgarten H, Cocchetto R, testori T, Meltzer A, Porter S. A new implant design for crestal bone preservation: Initial observations and case report. Pract Proced Aesthet Dent. 2005;17:735–40. [PubMed] [Google Scholar]
- 7.Calvo Guirado JL, Ortiz Ruiz AJ, Gomez Moreno G, Lopez Mari L, Bravo Gonzalez LA. Immediate loading and immediate restoration in 105 expanded-platform implants via the Diem System after a 16-month follow-up period. Med Oral Patol Oral Cir Bucal. 2008;13:E576–81. [PubMed] [Google Scholar]
- 8.Yun HJ, Park JC, Yun JH, Jung UW, Kim CS, Choi SH, et al. A short-term clinical study of marginal bone level change around microthreaded and platform-switched implants. J Periodontal Implant Sci. 2011;41:211–7. doi: 10.5051/jpis.2011.41.5.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wagenberg B, Froum SJ. Prospective study of 94 platform-switched implants observed from 1992 to 2006. Int J Periodontics Restorative Dent. 2010;30:9–17. [PubMed] [Google Scholar]
- 10.Prosper L, Crespi R, Valenti E, Cappare P, Gherlone E. Five-year follow-up of wide-diameter implants placed in fresh molar extraction sockets in the mandible: Immediate versus delayed loading. Int J Oral Maxillofac Implants. 2010;25:607–12. [PubMed] [Google Scholar]
- 11.Cocchetto R, Traini T, Caddeo F, Celletti R. Evaluation of hard tissue response around wider platform-switched implants. Int J Periodontics Restorative Dent. 2010;30:163–71. [PubMed] [Google Scholar]
- 12.Bilhan H, Mumcu E, Erol S, Kutay O. Influence of platform-switching on marginal bone levels for implants with mandibular overdentures: A retrospective clinical study. Implant Dent. 2010;19:250–8. doi: 10.1097/ID.0b013e3181dc9d1a. [DOI] [PubMed] [Google Scholar]
- 13.Canullo L, Fedele GR, Iannello G, Jepsen S. Platform switching and marginal bone-level alterations: The results of a randomized-controlled trial. Clin Oral Implants Res. 2010;21:115–21. doi: 10.1111/j.1600-0501.2009.01867.x. [DOI] [PubMed] [Google Scholar]
- 14.Canullo L, Rasperini G. Preservation of peri-implant soft and hard tissues using platform switching of implants placed in immediate extraction sockets: A proof-of-concept study with 12- to 36-month follow-up. Int J Oral Maxillofac Implants. 2007;22:995–1000. [PubMed] [Google Scholar]
- 15.Prosper L, Redaelli S, Pasi M, Zarone F, Radaelli G, Gherlone EF. A randomized prospective multicenter trial evaluating the platform-switching technique for the prevention of postrestorative crestal bone loss. Int J Oral Maxillofac Implants. 2009;24:299–308. [PubMed] [Google Scholar]
- 16.Calvo-Guirado JL, Ortiz-Ruiz AJ, Lopez-Mari L, Delgado-Ruiz R, Mate-Sanchez J, Bravo Gonzalez LA. Immediate maxillary restoration of single-tooth implants using platform switching for crestal bone preservation: A 12-month study. Int J Oral Maxillofac Implants. 2009;24:275–81. [PubMed] [Google Scholar]
- 17.Vela-Nebot X, Rodriguez-Ciurana X, Rodado-Alonso C, Segala-Torres M. Benefits of an implant platform modification technique to reduce crestal bone resorption. Implant Dent. 2006;15:313–20. doi: 10.1097/01.id.0000226788.19742.32. [DOI] [PubMed] [Google Scholar]
- 18.Trammell K, Geurs NC, O’Neal SJ, Liu PR, Haigh SJ, McNeal S, et al. A prospective, randomized, controlled comparison of platform-switched and matched-abutment implants in short-span partial denture situations. Int J Periodontics Restorative Dent. 2009;29:599–605. [PubMed] [Google Scholar]
- 19.Rodriguez-Ciurana X, Vela-Nebot X, Segala-Torres M, Rodado-Alonso C, Mendez-Blanco V, Mata-Bugueroles M. Biomechanical repercussions of bone resorption related to biologic width: A finite element analysis of three implant-abutment configurations. Int J Periodontics Restorative Dent. 2009;29:479–87. [PubMed] [Google Scholar]
- 20.Cappiello M, Luongo R, Di Iorio D, Bugea C, Cocchetto R, Celletti R. Evaluation of peri-implant bone loss around platform-switched implants. Int J Periodontics Restorative Dent. 2008;28:347–55. [PubMed] [Google Scholar]
- 21.Canullo L, Goglia G, Iurlaro G, Iannello G. Short-term bone level observations associated with platform switching in immediately placed and restored single maxillary implants: A preliminary report. Int J Prosthodont. 2009;22:277–82. [PubMed] [Google Scholar]
- 22.Calvo-Guirado JL, Gomez-Moreno G, Lopez-Mari L, Guardia J, Negri B, Martinez-Gonzalez JM. Crestal bone loss evaluation in osseotite expanded platform implants: A 5-year study. Clin Oral Implants Res. 2011;22:1409–14. doi: 10.1111/j.1600-0501.2010.02130.x. [DOI] [PubMed] [Google Scholar]
- 23.Enkling N, Johren P, Klimberg V, Bayer S, Mericske-Stern R, Jepsen S. Effect of platform switching on peri-implant bone levels: A randomized clinical trial. Clin Oral Implants Res. 2011;22:1185–22. doi: 10.1111/j.1600-0501.2010.02090.x. [DOI] [PubMed] [Google Scholar]
- 24.Canullo L, Iannello G, Gotz W. The influence of individual bone patterns on peri-implant bone loss: Preliminary report from a 3-year randomized clinical and histologic trial in patients treated with implants restored with matching-diameter abutments or the platform-switching concept. Int J Oral Maxillofac Implants. 2011;26:618–30. [PubMed] [Google Scholar]
- 25.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 26.Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989;62:567–72. doi: 10.1016/0022-3913(89)90081-4. [DOI] [PubMed] [Google Scholar]
- 27.Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants.1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990;1:33–40. doi: 10.1034/j.1600-0501.1990.010105.x. [DOI] [PubMed] [Google Scholar]
- 28.Branemark PI, Hansson BO, Adell R, Breine U, Lindström J, Hallén O, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1–132. [PubMed] [Google Scholar]
- 29.Adell R, Lekholm U, Rockler B, Branemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 30.Lang NP, Karring T, Stream C. Proceedings of the First European Workshop on Periodontology. London: Quintessence; 1994. pp. 365–9. [Google Scholar]
- 31.Roos J, Sennerby L, Lekholm U, Jemt T, Grondahl K, Albrektsson T. A qualitative and quantitative method for evaluating implant success: A 5-year retrospective analysis of the Branemark implant. Int J Oral Maxillofac Implants. 1997;12:504–14. [PubMed] [Google Scholar]
- 32.Cardaropoli G, Lekholm U, Wennstrom JL. Tissue alterations at implant-supported single-tooth replacements: A 1-year prospective clinical study. Clin Oral Implants Res. 2006;17:165–71. doi: 10.1111/j.1600-0501.2005.01210.x. [DOI] [PubMed] [Google Scholar]
- 33.Gomez-Roman G. Influence of flap design on peri-implant interproximal crestal bone loss around single-tooth implants. Int J Oral Maxillofac Implants. 2001;16:61–7. [PubMed] [Google Scholar]
- 34.Palmer RM, Palmer PJ, Smith BJ. A 5-year prospective study of Astra single tooth implants. Clin Oral Implants Res. 2000;11:179–82. doi: 10.1111/j.1600-0501.2000.tb00012.x. [DOI] [PubMed] [Google Scholar]
- 35.Shin YK, Han CH, Heo SJ, Kim S, Chun HJ. Radiographic evaluation of marginal bone level around implants with different neck designs after 1 year. Int J Oral Maxillofac Implants. 2006;21:789–94. [PubMed] [Google Scholar]
- 36.Duyck J, Ronold HJ, van Oosterwyck H, Naert I, Vander Sloten J, Ellingsen JE. The influence of static and dynamic loading on marginal bone reactions around osseointegrated implants: An animal experimental study. Clin Oral Implants Res. 2001;12:207–18. doi: 10.1034/j.1600-0501.2001.012003207.x. [DOI] [PubMed] [Google Scholar]
- 37.Hermann JSSJ, Buser D, Schenk RK, Cochran DL. Influence of the size of the microgap on crestal bone changes around titanium implants: A histometric evaluation of unloaded non-submerged implants in the canine mandible. J Clin Periodontol. 2001;72:1372–83. doi: 10.1902/jop.2001.72.10.1372. [DOI] [PubMed] [Google Scholar]
- 38.Ericsson I, Persson LG, Berglundh T, Marinello CP, Lindhe J, Klinge B. Different types of inflammatory reactions in peri-implant soft tissues. J Clin Periodontol. 1995;22:255–61. doi: 10.1111/j.1600-051x.1995.tb00143.x. [DOI] [PubMed] [Google Scholar]
- 39.Cochran DL, Hermann JS, Schenk RK, Higginbottom FL, Buser D. Biologic width around titanium implants. A histometric analysis of the implanto-gingival junction around unloaded and loaded nonsubmerged implants in the canine mandible. J Clin Periodontol. 1997;68:186–98. doi: 10.1902/jop.1997.68.2.186. [DOI] [PubMed] [Google Scholar]
- 40.Mombelli A, Lang NP. The diagnosis and treatment of peri-implantitis. Periodontol 2000. 1998;17:63–76. doi: 10.1111/j.1600-0757.1998.tb00124.x. [DOI] [PubMed] [Google Scholar]
- 41.Crespi R, Cappare P, Gherlone E. Radiographic evaluation of marginal bone levels around platform-switched and non-platform-switched implants used in an immediate loading protocol. Int J Oral Maxillofac Implants. 2009;24:920–6. [PubMed] [Google Scholar]
- 42.Berglundh T, Lindhe J. Dimension of the periimplant mucosa. Biological width revisited. J Clin Periodontol. 1996;23:971–3. doi: 10.1111/j.1600-051x.1996.tb00520.x. [DOI] [PubMed] [Google Scholar]
- 43.Berglundh T, Lindhe J, Ericsson I, Marinello CP, Liljenberg B, Thomsen P. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991;2:81–90. doi: 10.1034/j.1600-0501.1991.020206.x. [DOI] [PubMed] [Google Scholar]
- 44.Hermann JS, Schoolfield JD, Nummikoski PV, Buser D, Schenk RK, Cochran DL. Crestal bone changes around titanium implants: A methodologic study comparing linear radiographic with histometric measurements. Int J Oral Maxillofac Implants. 2001;16:475–85. [PubMed] [Google Scholar]
- 45.Hermann JS, Cochran DL, Nummikoski PV, Buser D. Crestal bone changes around titanium implants. A radiographic evaluation of unloaded nonsubmerged and submerged implants in the canine mandible. J Clin Periodontol. 1997;68:1117–30. doi: 10.1902/jop.1997.68.11.1117. [DOI] [PubMed] [Google Scholar]
- 46.Tarnow D, Elian N, Fletcher P, Froum S, Magner A, Cho SC, et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants. J Periodontol. 2003;74:1785–8. doi: 10.1902/jop.2003.74.12.1785. [DOI] [PubMed] [Google Scholar]
- 47.Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Clin Periodontol. 2000;71:546–9. doi: 10.1902/jop.2000.71.4.546. [DOI] [PubMed] [Google Scholar]
- 48.Ericsson I, Berglundh T, Marinello C, Liljenberg B, Lindhe J. Long-standing plaque and gingivitis at implants and teeth in the dog. Clin Oral Implants Res. 1992;3:99–103. doi: 10.1034/j.1600-0501.1992.030301.x. [DOI] [PubMed] [Google Scholar]
- 49.Luongo R, Traini T, Guidone PC, Bianco G, Cocchetto R, Celletti R. Hard and soft tissue responses to the platform-switching technique. Int J Periodontics Restorative Dent. 2008;28:551–7. [PubMed] [Google Scholar]
- 50.Becker J, Ferrari D, Herten M, Kirsch A, Schaer A, Schwarz F. Influence of platform switching on crestal bone changes at non-submerged titanium implants: A histomorphometrical study in dogs. J Clin Periodontol. 2007;34:1089–96. doi: 10.1111/j.1600-051X.2007.01155.x. [DOI] [PubMed] [Google Scholar]
- 51.Becker J, Ferrari D, Mihatovic I, Sahm N, Schaer A, Schwarz F. Stability of crestal bone level at platform-switched non-submerged titanium implants: A histomorphometrical study in dogs. J Clin Periodontol. 2009;36:532–9. doi: 10.1111/j.1600-051X.2009.01413.x. [DOI] [PubMed] [Google Scholar]
- 52.Schrotenboer J, Tsao YP, Kinariwala V, Wang HL. Effect of microthreads and platform switching on crestal bone stress levels: A finite element analysis. J Clin Periodontol. 2008;79:2166–72. doi: 10.1902/jop.2008.080178. [DOI] [PubMed] [Google Scholar]
- 53.Schrotenboer J, Tsao YP, Kinariwala V, Wang HL. Effect of platform switching on implant crest bone stress a finite element analysis. Implant Dent. 2009;18:260–9. doi: 10.1097/ID.0b013e31819e8c1d. [DOI] [PubMed] [Google Scholar]
- 54.Canay S, Akca K. Biomechanical aspects of bone-level diameter shifting at implant-abutment interface. Implant Dent. 2009;18:239–48. doi: 10.1097/ID.0b013e318198ffd1. [DOI] [PubMed] [Google Scholar]
- 55.Baggi L, Cappelloni I, Di Girolamo M, Maceri F, Vairo G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry a three-dimensional finite element analysis. J Prosthet Dent. 2008;100:422–31. doi: 10.1016/S0022-3913(08)60259-0. [DOI] [PubMed] [Google Scholar]
- 56.Maeda Y, Miura J, Taki I, Sogo M. Biomechanical analysis on platform switching is there any biomechanical rationale? Clin Oral Implants Res. 2007;18:581–4. doi: 10.1111/j.1600-0501.2007.01398.x. [DOI] [PubMed] [Google Scholar]
- 57.Sabet ME, El-Korashy DI, El-Mahrouky NA. Effect of platform switching on strain developed around implants supporting mandibular overdenture. Implant Dent. 2009;18:362–70. doi: 10.1097/ID.0b013e3181b4f98c. [DOI] [PubMed] [Google Scholar]
- 58.Pellizzer E, Verri F, Falcon-Antenucci RM, Santiago JJ, de Carvalho PS, Moraes SL, et al. Stress analysis in platform switching implants. A three-dimensional finite element study. J Oral Implantol. 2010 doi: 10.1563/AAID-JOI-D-10-00041. [In press] [DOI] [PubMed] [Google Scholar]
- 59.Pellizzer EP, Falcon-Antenucci RM, de Carvalho PS, Santiago JF, de Moraes SL, de Carvalho BM. Photoelastic analysis of the influence of platform switching on stress distribution in implants. J Oral Implantol. 2010;36:419–24. doi: 10.1563/AAID-JOI-D-09-00077. [DOI] [PubMed] [Google Scholar]
- 60.Canullo L, Pace F, Coelho P, Sciubba E, Vozza I. The influence of platform switching on the biomechanical aspects of the implant-abutment system. A three dimensional finite element study. Med Oral Patol Oral Cir Bucal. 2011;16:E852–6. doi: 10.4317/medoral.17243. [DOI] [PubMed] [Google Scholar]
- 61.Pessoa RS, Vaz LG, Marcantonio E, Jr, Vander Sloten J, Duyck J, Jaecques SV. Biomechanical evaluation of platform switching in different implant protocols computed tomography-based three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2010;25:911–9. [PubMed] [Google Scholar]
- 62.Leblebicioglu B, Rawal S, Mariotti A. A review of the functional and esthetic requirements for dental implants. J Am Dent Assoc. 2007;138:321–9. doi: 10.14219/jada.archive.2007.0164. [DOI] [PubMed] [Google Scholar]
- 63.de Oliveira RR, Novaes AB, Jr, Papalexiou V, Muglia VA, Taba M., Jr Influence of interimplant distance on papilla formation and bone resorption a clinical-radiographic study in dogs. J Oral Implantol. 2006;32:218–27. doi: 10.1563/793.1. [DOI] [PubMed] [Google Scholar]
- 64.Khatami AH, Al-Ajmi M, Kleinman A. Preservation of the gingival architecture with the scalloped implant design a clinical report. J Oral Implantol. 2006;32:167–70. doi: 10.1563/798.1. [DOI] [PubMed] [Google Scholar]
- 65.Lops D, Chiapasco M, Rossi A, Bressan E, Romeo E. Incidence of inter-proximal papilla between a tooth and an adjacent immediate implant placed into a fresh extraction socket 1-year prospective study. Clin Oral Implants Res. 2008;19:1135–40. doi: 10.1111/j.1600-0501.2008.01580.x. [DOI] [PubMed] [Google Scholar]
- 66.Novaes AB, Jr, Barros RR, Muglia VA, Borges GJ. Influence of interimplant distances and placement depth on papilla formation and crestal resorption a clinical and radiographic study in dogs. J Oral Implantol. 2009;35:18–27. doi: 10.1563/1548-1336-35.1.18. [DOI] [PubMed] [Google Scholar]
- 67.Froum SJ, editor. Dental implant complications etiology, prevention, and treatment. 1 ed. United States: Wiley-Blackwell; 2010. p. 149. (184, 198). [Google Scholar]
- 68.Canullo L, Iannello G, Penarocha M, Garcia B. Impact of implant diameter on bone level changes around platform switched implants preliminary results of 18 months follow-up a prospective randomized match-paired controlled trial. Clin Oral Implants Res. 2011 Nov 24; doi: 10.1111/j.1600-0501.2011.02297.x. doi: 10.1111/j.1600-0501.2011.02297.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


