Abstract
The term “ranula” is used to describe a diffuse swelling in the floor of the mouth caused by either a mucous extravasation or, less commonly, a mucous retention cyst derived from the major sublingual or submandibular salivary glands. The most common presentation of ranula is a painless, slow-growing, soft, and movable mass located in the floor of the mouth. Ranula may be simple or plunging. Simple ranula often present as masses in the floor of the mouth, limited to the mucous membranes. Diving ranulas extend through the facial plans, usually posterior to the mylohyoid muscle into the neck, and present as cervical masses. Thyroglossal duct cyst, branchial cleft cyst, cystic hygroma, submandibular sialadenitis, intramuscular hemangioma, cystic or neoplastic thyroid disease might be included in differential diagnosis. A variety of surgical procedures have been quoted in the literature ranging from marsupialization, excision of the ranula, sclerotherapy, and excision of the sublingual gland. The recurrence rate varies according to the procedure performed.
Keywords: Marsupialization, mouth floor, ranula, submandibular gland
INTRODUCTION
The term “ranula” is used to describe a diffuse swelling in the floor of the mouth caused by either a mucous extravasation or, less commonly, a mucous retention cyst derived from the major sublingual or submandibular salivary glands.[1] The term ranula is used because this lesion often resembles the swollen abdomen of a frog. They are most common in the second decade of life and in females.[2] The most common presentation of ranula is a painless, slow-growing, soft, and moveble mass located in the floor of the mouth. Usually, the lesion forms to one side of the lingual frenum; however, if the lesion extends deep into the soft tissue, it can cross the midline.[2]
Sublingual glands (SLGs) are the smallest of the paired major salivary glands, weighing about 2 g, and shaped like a flattened almond measuring about 2.5 cm anteroposteriorly, each gland has a row of about 12–20 short ducts that open independently along the summit of the sublingual fold in the floor of the mouth, obstruction of one of these ducts results in formation of a mucous retention cyst in the sublingual space, termed simple ranula, further accumulation of secretions with time results in extension along sublingual space anteriorly and posteriorly, if posterior extension extends or extravasates beyond the free edge of, or through the mylohyoid muscle.[3]
A variety of surgical procedures have been quoted in the literature ranging from marsupialization, excision of the ranula, sclerotherapy, and excision of the sublingual gland. The recurrence rate varies according to the procedure performed.[4]
CASE REPORT
An 18-year-old man, with a large swelling on a left side of his face and neck was coming to the Department of Oral Radiology, School of Dentistry.
The chief complaint was the asymmetry of his face. The patient history showed that he had severe accident 2 years ago and had hospitalized. At that time such a lesion was appearance on the left side of his face and became bigger. He did not report any pain or paresthesia and loosing of teeth.
Because the lesion had grown slowly and there were no pain and loosing teeth, so it seems that it was not a malignant lesion.
In extraoral examination, a diffuse, soft, fluctuant, nontender swelling, about 7×5 cm in size, was present in the left submandibular region, which was extended to the neck. There was no redness, heat, and pain [Figure 1].
Figure 1.

A diffuse, soft, fluctuant swelling presents in the left submandibular region, which was extended to the neck
In intraoral examination there was a small, smooth surface, and movable mass in the floor of the mouth, to one side of the lingual frenum [Figure 2]. The mucous color was normal. Oral mucosa, gingival, was normal and salivary ducts openings were patent. Oral hygiene was poor. The tooth number 47 was carious. There was no displacement and loosing teeth.
Figure 2.

A small, smooth surface, and movable mass in the floor of the mouth, to one side of the lingual frenum
In a panoramic radiography, the tooth number 47 had caries, but there was no lesion in the left side of radiography [Figure 3].
Figure 3.
The tooth number 47 had caries, but there was no lesion in the left side of radiography
According to no redness, heat, pain, and no lesion in the bone in panoramic view, it seems that there was no infection associated with teeth such as abscess or osteomyelitis. On the other hand, salivary duct openings were present and he did not had history of any enlargement of lesion during meals, so we could roll out sialoliths.
The patient had taken Computed tomography (CT) from this field, 4 months ago, which showed a well-defined cystic mass lesion in submandibular space without peripheral enhancement [Figure 4]. It causes posterior displacement of the left submandibular gland and obliteration of the left vallecula and preform sinus.
Figure 4.
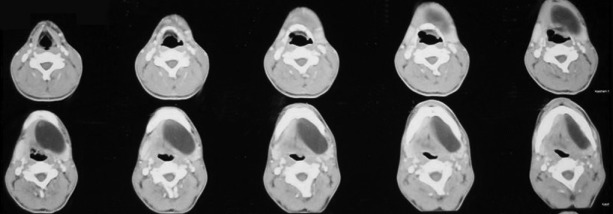
CT showed a well-defined cystic mass lesion in the submandibular space without peripheral enhancement
Since the high-resolution ultrasound is an ideal initial imaging investigation for neck tumors and it is readily available, relatively inexpensive, and does not involve ionizing radiation,[5] sonographic examination was done for the patient. It revealed a space occupying mass with 62×25 mm, which was cyst like with capsule [Figure 5]. It contained concentrated liquid. There was no blood vessel. The cyst was across the midline slightly and had a pressure effect on surrounding structures. From these findings, solid tumors such as pleomorphic adenoma and monomorphic adenoma could be rejected.
Figure 5.
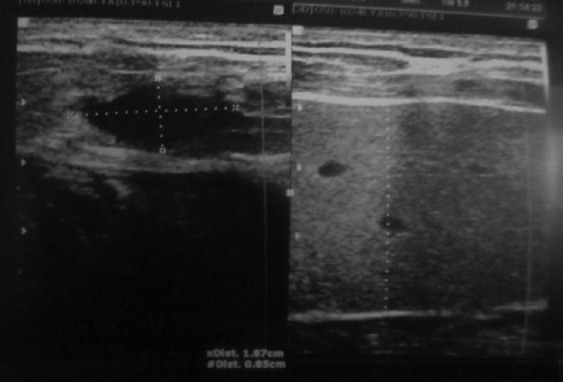
Sonographic examination, revealed space occupying mass with 62×25 mm, which was cyst like with capsule
The patient was referred to oral surgery department for treatment. In Alzahra hospital, the lesion was treated with the marsupialization technique.
Histopatological findings show an area of spilled mucin surrounded by a granulation tissue response. The inflammation includes numerous foamy histiocytes (macrophages) [Figure 6].
Figure 6.
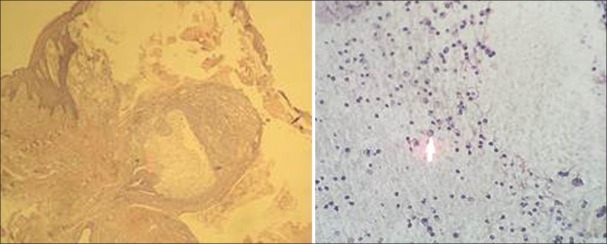
Histopatological findings show the inflammation includes numerous foamy histiocytes (arrow)
DISCUSSION
Ranula develops from extravasation of mucus after trauma to the sublingual gland or obstruction of the ducts.[6,7] Ranula can present at any age. It has been reported from 2 to 61 years of age with a slight female preponderance.[8] Regarding the Patel et al. study a total of 26 ranulas were identified at their institution over an 18-year period. There were 54% male and 46% female patients with an average age of 25.6 and a median age of 26. Of the 26 ranulas identified, 16 were oral (62%) and 10 were plunging (38%).[9]
The etiology is unknown, but it has been described in association with congenital anomalies, trauma, and disease of the sublingual gland.[8]
The pathophysiology involved in extravasation is hypertension in the duct due to obstruction leading to acinar rupture in the salivary gland and then extravasation of the mucus. The initial stage is a traumatic rupture of the excretory duct and the second stage is the extravasation and subsequent accumulation of saliva within the tissue, as shown by experimental studies.[4]
When these extravasation cysts extend into the submandibular or submental space, they are called plunging ranula. These cysts commonly extend into the submandibular triangle, occasionally they may extend superiorly into the parapharyngeal space as far as the base of the skull. They may extend inferiorly to the supraclavicular area and upper mediastinum or posteriorly into the retropharyngeal space.[4,8,10]
The extension of ranula to the submandibular and upper cervical region is related to the herniation of the mylohyoid muscle by the sublingual gland, that happened in this case. Projections of the gland through a hiatus between the anterior and the posterior part of the mylohyoid muscle were reported in 45% of cadaver specimens and it shows the clear involvement of this herniation in cervical extension of the ranulas. In addition, the presence of ectopic sublingual gland tissue, beyond the mylohyoid muscle, may be causally related to a plunging ranula and provides evidence for their possible congenital origin. Surgical interventions have also been implicated in ranula formation. There are reports of plunging ranulas that developed after the excision of a sialolith or transposition of the duct of the sub mandibular gland.[11]
According to Gupta et al., Kalra et al., and Zhao et al. studies the cervical ranula appears as an asymptomatic, continuously enlarging mass that may fluctuate in size. Most reported ranulas are 4–10 cm in size. The overlying skin is usually intact. The mass is fluctuant, freely movable, and nontender.[12–14] The mass is not associated with the thyroid gland or lymph node chains. In some instances, detecting salivary gland herniation of a portion of the sublingual gland through the mylohyoid muscle into the neck may be possible. The mass may not be well defined, but should follow the facial planes of the neck and may extend into the mediastinum. Similar to the oral ranula, the mass tends to cause a lateral swelling; however, it may cross the midline. They have been reported to extend into the submental region, the contralateral neck, the nasopharynx up to the skull base, the retropharynx and even into the upper mediastinum.[15,16] Rarely, large-sized ranulas may cause dysphagia or airway obstruction.
Sialogram, ultrasonography, Magnetic resonance imaging (MRI), CT, and aspiration cytology can be helpful for diagnosis. Aspiration cytology will show mucin with muciphages and biochemical analysis will show increase in amylase and protein content. This is diagnostic of the salivary origin.[4]
The microscopic appearance of a ranula is similar to that of a mucocele in other locations. On microscopic examination, the mucocele shows an area of spilled mucin surrounded by a granulation tissue response. The inflammation usually includes numerous foamy histiocytes (macrophages). In some cases a ruptured salivary duct may be identified feeding into the area. The adjacent minor salivary glands often contain a chronic inflammatory cell infiltrate and dilated ducts.[17]
The diagnosis of a plunging ranula is of clinical significance for there are many benign as well as malignant lesions that have the same appearance during physical examination. In particular, neoplastic and inflammatory lesions of the submandibular and sublingual glands, of the lymphnodes, granulomatous, vascular, nerve or adipose tissue diseases, branchial or thyroglossal duct cysts, dermoid and epidermoid cysts, cystic hygroma and laryngocele could appear as a soft palpable mass of the submandibular region, complicating the diagnosis. There are no specific tests for the diagnosis of cervical ranulas. Differential diagnosis should be based on the history of the lesion that shows up as a cystic fluctuating lesion, gradually increasing in size. Additionally, the fluid of ranulas consists of a higher salivary amylase and protein content compared to serum.[11]
Surgery is the main stay for the management of ranulas. These include incision and drainage, excision of ranula, marsupialization, and marsupialization with packing or complete excision of the sublingual gland.[4] In 1973 Roediger et al. reported that two cases of plunging ranula were treated by primary excision of the sublingual gland through the mouth.[18] Simple marsupialization has fallen into disfavor primarily because of the failure rate, which has been anywhere from 61% to 89%. Marsupialization with packing of the cyst cavity may reduce the recurrence.[4]
Other treatment modalities have also been utilized. Sclerotherapy with OK-432 is a good substitute for surgery.[15] Recurrence was noted in 14.3% and the patient had an average of 1.7 injections. Fukase et al.,[16] used a higher concentration in partially regressed cases and had 100% cure rate.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Peters E, Kola H, Doyle-Chan W. Bilateral congenital oral mucous extravasation cysts. Pediatr Dent. 1999;21:286–9. [PubMed] [Google Scholar]
- 2.Greenberg MS, Glick M, Ship JA. Burket oral medicine. 11th ed. Hamilton: Bcdecker; 2008. p. 203. [Google Scholar]
- 3.El Beltagi AH, El Sayed Ahmed, Al Far, Al Sahmmary N. Horseshoe shaped, anterior crossing ranula, a case report. Eur J Radiol Extra. 2007;64:95–8. [Google Scholar]
- 4.Arunachalam P, Priyadharshini N. Recurrent plunging ranula. J Indian Assoc Pediatr Surg. 2010;15:36–8. doi: 10.4103/0971-9261.69143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong KT, Lee YY, King AD, Ahuja AT. Imaging of cystic or cyst-like neck masses. Clin Radiol. 2008;63:613–22. doi: 10.1016/j.crad.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 6.Catone GA, Merrill RG, Henny FA. Sublingual gland mucus escape phenomenon–Treatment by excision of sublingual gland. J Oral Surg. 1969;27:774–86. [PubMed] [Google Scholar]
- 7.Regezi JA, Sciubba JJ, Jordan RC. In: Oral pathology, clinical pathologic correlations. 3rd ed. Regezi JA, Sciubba JJ, editors. Philadelphia: WB Saunders Company; 1999. pp. 220–2. [Google Scholar]
- 8.Davison MJ, Morton RP, McIvor NP. Plunging ranula: Clinical observations. Head Neck. 1998;20:63–8. doi: 10.1002/(sici)1097-0347(199801)20:1<63::aid-hed10>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 9.Patel MR, Deal AM, Shockley WW. Oral and plunging ranulas: What is the most effective treatment? Laryngoscope. 2009;119:1501–9. doi: 10.1002/lary.20291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hidaka H, Oshima T, Kakehata S, Watanabe K, Toshima M, Suzuki H, et al. Two cases of plunging ranula managed by the intra oral approach. Tohoku J Exp Med. 2003;200:59–65. doi: 10.1620/tjem.200.59. [DOI] [PubMed] [Google Scholar]
- 11.Dietrich EM, Banikas V, Lazaridou M, Papaemmanouil S, Antoniades K. Sublingual-plunging ranula as a complication of supraomohyoid neck dissection. International Journal of Surgery Case Reports. [Last accepted on 2011 Feb 17]. Available from: http://www.elsevier.de/ijscr . [DOI] [PMC free article] [PubMed]
- 12.Gupta A, Karjodkar FR. Plunging ranula: A case report. ISRN Dent. 2011;2011:806928. doi: 10.5402/2011/806928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalra V, Mirza Kh, Malhotra A. Plunging Ranula. J Radiol Case Rep. 2011;5:18–24. doi: 10.3941/jrcr.v5i6.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao YF, Jia Y, Chen XM, Zhang WF. Clinical review of 580 ranulas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:281–7. doi: 10.1016/S1079210404000800. [DOI] [PubMed] [Google Scholar]
- 15.Rho MH, Kim DW, Kwon JS, Lee SW, Sung YS, Song YK, et al. OK — 432 sclerotherapy of plunging ranula in 21 patients: It can be a substitute for surgery. AJNR Am J Neuroradiol. 2006;27:1090–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Fukase S, Ohta N, Inamura K, Aoyagi M. Treatment of ranula with intracystic injection of the streptococcal preparation OK- 432. Ann Otol Rhinol Laryngol. 2003;112:214–20. doi: 10.1177/000348940311200304. [DOI] [PubMed] [Google Scholar]
- 17.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial Pathology. 3rd ed. Philadelphia: Saunders; 2009. pp. 454–7. [Google Scholar]
- 18.Roediger WE, Lloyd P, Lawson HH. Mucous extravasation theory as a cause of plunging ranulas. Br J Surg. 1973;60:720–2. doi: 10.1002/bjs.1800600917. [DOI] [PubMed] [Google Scholar]


