Abstract
Introduction:
Debonding is a common cause of failure encountered with fiber-reinforced composite (FRC) posts, and usually occurs along the post space-dentin adhesive interface. The aim of this in vitro study is to evaluate the regional push-out bond strength of a fiber-reinforced post system, using two resin cements.
Materials and Methods:
In this in vitro study 20 maxillary central incisors were decoronated and the roots were endodontically treated. Following post space preparation, the roots were divided into two groups of 10 specimens each. Fiber-reinforced composite posts were cemented with two resin cement systems: (a) Self-etch system (Panavia F2.0/ED-primer II) and (b) conventional system (Variolink II/Excite DSC). Three slices of each root, with a thickness of 3 mm, were prepared. The push-out test was performed with a universal testing machine at a crosshead speed of 1 mm/minute, and bond strength values were calculated. The data were analyzed with a two-way Analysis of variance (ANOVA) and Scheffe tests (α=.05).
Results:
There were no significant differences between the mean push-out bond strengths of two experimental groups (Panavia F: 12.59±5.44, Variolink II: 12.49±4.52 MPa) (P=0.920), but there were significant differences between the mean push out bond strengths of the root dentin regions (P<0.001).
Conclusion:
Under the conditions of this study, there was no significant difference between the mean push out bond strength of self-etching and the conventional resin cement systems. The coronal region of the root dentin showed a significantly higher bond strength than the apical region.
Keywords: Bond strength, composite resins, dental bonding, fiber reinforced, post and core technique, resin cements
INTRODUCTION
Endodontically treated teeth, with a large amount of coronal tooth structure missing, frequently require the placement of a post inside the root canal, to retain a core for definitive restoration.[1–3] The choice of appropriate restoration for these teeth is influenced by strength and esthetics.[4] Depending on the clinical parameters, the choice may be a metal or an esthetic post and core restoration.[5–7]
Clinical studies have reported success rates of 95 to 99% for teeth restored with fiber-reinforced posts, with no occurrence of root fracture during the study periods.[8,9] The most common cause of failure reported in these studies is not from the root fracture, as occurs with metal or cast posts, but rather from the pull out of the cement, post restoration assembly, as a result of lack of retention of the fiber posts.[7,10] The retention of fiber posts in the roots depends on the bond strength between the post material and a resin luting agent, as well as the bond strength between the resin luting agent and post space dentin.[11–14]
Many in vitro studies have investigated various factors that influence this bond strength. These factors include length, design, diameter, composition, surface treatment of the post, preparing the dentinal surface, the dentin bonding agent, luting cement, and polymerization mode.[3,10,15] The effect of cement type on the retention of the post in endodontically treated teeth has been investigated extensively and it has been found that resin cements can significantly increase the retention of posts and fracture-resistance of the teeth, compared to other cements.[15–17]
Different resin luting agents and corresponding bonding systems have been proposed for cementing tooth-colored posts.[16,18] Several in vitro studies have reported controversial results regarding bond strengths of different luting agents to endodontic posts and root canal dentin.[19–26]
Selecting an appropriate adhesive and luting procedure for bonding posts to root dentin is an important challenge.[27–29] According to adhesive dentistry, two strategies can be used to allow the bonding agents to react with the dentin.[6] Some systems use etch-and-rinse with phosphoric acid to eliminate the smear layer and demineralize the underlying dentin. This step is followed by application of a hydrophilic monomer that penetrates the conditioned dentin surface. Other systems use self-etching primers, with no rinsing step, which cause less aggressive demineralization and are followed by the application of an adhesive resin.[30]
The bond strength of fiber posts to root canal dentin may be varied in different regions of the root canal.[18,30,31] This difference may arise from the difficulty of reaching the curing light to more apical parts of the root canal, difficulty of direct vision to the deeper regions of the root canal, and difficulty of moisture control and adhesive application in the apical region of the root canals.[16] The aim of the present study is to compare the push-out bond strength of a glass fiber reinforced composite post system, cemented with a self-etch and conventional resin cement systems, in different root canal regions.
The null hypotheses were: (1) Self etching and conventional resin cements provide the same bond strength for glass fiber reinforced composite post, and (2) there are no differences between the bond strengths of different post space regions.
MATERIALS AND METHODS
In this in vitro study, 20 human maxillary central incisors with 15 mm length (from 1 mm above the cementoenamel junction to the apex), extracted for periodontal reasons, were selected. The specimens were free of cracks, carious lesions, fractures, and resorption, with fully developed apices and without previous endodontic treatments, posts, or crowns. They were cleaned off soft tissues and calculus, and placed in 2.5% sodium hypochlorite for two hours, for surface disinfection, and then stored in 0.1% NaN3 solution until use.
The coronal part of each tooth was removed 1 mm above the cementoenamel junction with diamond disks (Ref.070, D and Z, Berlin, Germany), mounted on a dental lathe machine (KaVo Polishing Unit. EWL 80, Leutkrich, Germany) at low speed, under constant water irrigation, to achieve a uniform length of 15 mm. The canal working length was established 1 mm short of the apical foramen. The step-back technique was used for canal instrumentation. Obturation was performed using AH26 (Dentsply Caulk, Milford, Germany) and gutta-percha (Aria Dent, Asia Chemi Teb Co., Tehran, Iran), with the vertical condensation method. After completion of endodontic treatment, the coronal root canal openings were filled with a provisional restorative material (GC Caviton; GC Dental Products Corp., Tokyo, Japan), and the teeth were stored in 100% humidity for one week at 37°C, to allow the sealer to set. After one week, the gutta-percha was removed from the coronal aspect of each root with a Gates Glidden drill #3 (Dentsply-Maillefer, Ballaigues, Switzerland) leaving 4 mm gutta percha in the apices, to preserve the apical seal. The post spaces were prepared to a depth of 10 mm with the appropriate drills (Fibio, Anthogyr, Sallanches, France). A new drill was used for every five specimens.
Post size 3 was tried, to ensure that the posts would reach the bottom of the post space. All posts were marked at a distance of 10 mm from the apical end, and were cut to that size with diamond disks. The shortened posts were cleaned with 70% ethanol for 60 seconds, rinsed with distilled water, and air dried. Before the cementation procedures, the post surfaces did not undergo any pretreatment.
The prepared roots were randomly divided into two groups of 10 specimens each for cementation procedures [Table 1].
Table 1.
Materials tested
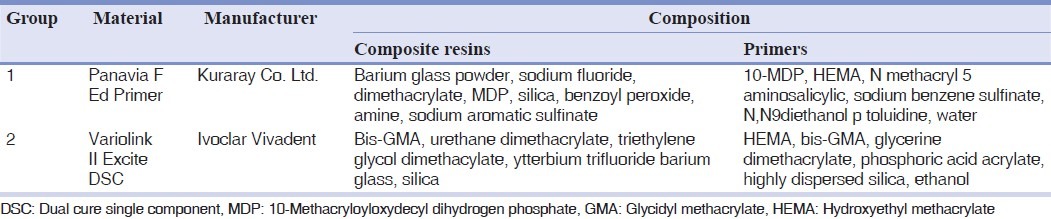
In group 1, the posts were luted with Panavia F 2.0 (Kuraray Medical, Inc., Okayama, Japan) after conditioning the dentin with ED-Primer (A and B liquid mixture, Kuraray) for 60 seconds, using a microbrush. The post space was gently air-dried and the excess primer was removed with paper points (Aria Dent).
In group 2, Variolink II (Ivoclar Vivadent, Schaan, Liechtenstein) was used as the luting agent. The canals were etched using 35% phosphoric acid (Ultra-Etch, Ultradent, South Jordan, UT, USA) for 15 seconds and rinsed with distilled water. Excess water was removed from the post spaces with a gentle stream of air and paper points. The Excite DSC (Ivoclar Vivadent), dual-polymerizing, single-bottle bonding agent was applied for 10 seconds with a microbrush coated with chemical initiators and the excess bonding agent was removed with paper points and gently air-dried. The bonding agent was polymerized with a halogen light unit, with 500-mW/cm2 intensity (Coltolux 50, Coltene, Altstatten, Switzerland), for 20 seconds, with the tip of the light unit directly in contact with the canal orifice.
For cementation of fiber posts, equal amounts of luting pastes (Panavia F 2.0 and Variolink II) were mixed and applied onto the surface of the posts and into the root canals with a Lentulo spiral instrument (Dentsply/Maillefer). The posts were inserted into the canal, to a full depth, by using gentle finger pressure, and the excess was immediately removed with a disposable brush. For Panavia F 2.0 the remaining cement around the post was protected with oxygen-inhibiting gel (Oxyguard II, Kuraray). For Variolink II, after the initial chemical polymerization, light curing was performed for 60 seconds in such a way that the tip of the light unit was directly in contact with the coronal end of the posts. The light output was monitored to ensure accurate light intensity before each exposure by using the light meter (Coltolux, Coltene).
After the cementation procedures, all specimens were stored in sterile saline in a light-proof box for one week at 37°C. Next, each root was sectioned perpendicular to the long axis with a diamond disk at low speed under constant distilled water cooling to create 3 mm-thick slices. In this manner; from each root, three post/dentin sections (coronal, middle, and apical) were obtained. Due to the tapered design of the fiber posts, post diameters were measured on each surface of the post/dentin sections, using digital calipers (Electronic digital caliper, Minova Co, Japan), with 0.01 mm accuracy.
The push-out test was performed by using the universal testing machine (TLCLO, Dartec Ltd., Stourbridge, England) at a crosshead speed of 1 mm/ minute, using a pin (diameter, 1.0 mm) on the center of the apical aspect of the post surface in an apical-coronal direction, without stressing the surrounding post space walls. The peak force (N) required to extrude the post from the root slice was recorded. To express the bond strength in MPa, the load at failure (N) was divided by the area of the bonded interface, which was calculated with the following formula:
![]()
where π was the constant 3.14, r1 was the coronal post radius, r2 was the apical post radius, and h was the thickness of the slice in millimeters.
The collected data were analyzed (SPSS/PC 16.0; Statistical package for the social sciences (SPSS) Inc, Chicago, Ill) using two-way analysis of variance (ANOVA) and Post Hoc Scheffe tests at P<0.05 levels of significance.
RESULTS
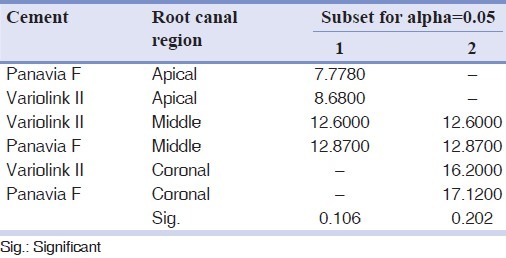
The mean push-out bond strength values (MPa) of the test groups in different root canal regions are shown in Table 2. The two-way ANOVA showed no significant differences between the mean push-out bond strength values recorded for two experimental groups (two types of cement systems) and there was no interaction between the type of resin cement system and different root canal regions (P=0.920 and P=0.731, respectively) [Table 3]. Otherwise, significant differences were observed among the bond strength values of the root dentin regions (P<0.001). The lowest bond strength values were obtained in the apical regions. The Post Hoc Scheffe test revealed that in both resin cement systems, there were significant differences between the coronal and apical regions [Table 4].
Table 2.
Descriptive statistics of push-out bond strength values (MPa) of two groups in different root canal regions
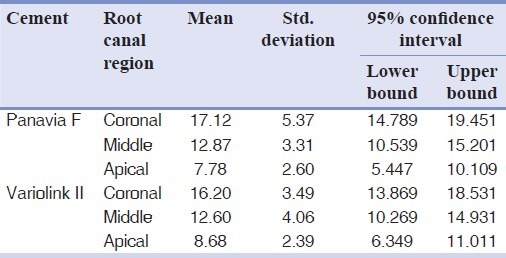
Table 3.
Two-way ANOVA
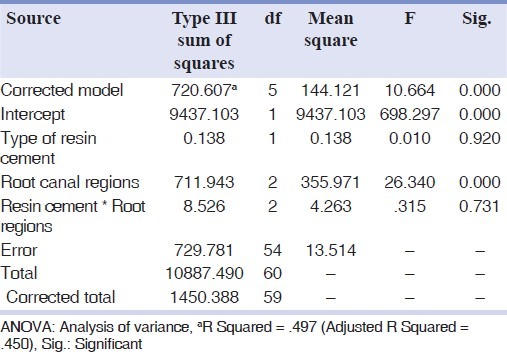
Table 4.
Scheffe test for push-out bond strength values (MPa) of two groups in different root canal regions
DISCUSSION
The results of this in vitro study support the first hypothesis that self-etching and conventional resin cements provide the same bond strength of a glass fiber reinforced composite post. However, the hypothesis that there are no differences between the bond strengths in different post space regions has been rejected.
In the case of the first hypothesis, our result was in agreement with some previous studies.[6,12,13,31–34] Noirrit et al.[6] stated that the hybrid layer and resin tags that resulted from both bonding systems (self-etch and total-etch) were nearly the same, although the conditioning of the canal walls was different. Micromorphological investigations showed that etching the dentin with phosphoric acid (PH≈2) (as used in the ‘etch-and-rinse’ systems) completely dissolved the smear layer and exposed the tubule apertures, collagen fibrils, and interfibrillar spaces, while the use of self-etch bonding systems had a variable effect on the smear layer.[6,11,18,28] These facts might be able to demonstrate the first hypothesis.
Bitter et al.[18] found a significant difference between these two types of luting agents when used as luting glass fiber reinforced composite posts on root canal dentin. They noted that the hybrid layer appeared thinner with the ‘self-etch’ system, than with the ‘etch-and-rinse’ system. They concluded that demineralization by phosphoric acid led to a deeper penetration of the adhesive than did a self-etch system, which could not completely penetrate the smear layer. Akgungor and Akkayan[11] and Yoshiyama et al.[35] stated that a system with a self-etching primer and light-polymerized bonding agent provided a significantly higher bond strength to root canal dentin than the self-etching bonding agents and the strength of this bond was not dependent on the hybrid layer thickness. In contrast, some authors[19,28,36] stated that simplified self-etch and self-adhesive resin cements, such as Panavia 21, exhibited an etching potential insufficient (even with a PH of ≈ 2.0) to dissolve the thick smear layers created in the post-space preparation, with slow-speed drills. They stated that this fact yielded to the high shrinkage stress in the thin cement layer and the consequent opening of interfacial gaps might account for the relatively low push-out strength recorded for ED Primer/Panavia 21 as compared to the results obtained with the use of the total-etch system, Excite DSC/Variolink II. However, they proposed the use of self-adhesive resin cements for intra-canal posts, because of their simple luting procedure.[37]
In the case of the second hypothesis, our result was in agreement with the previous studies that reported higher bond strength for coronal dentin than values for the middle and apical sections of the root.[4,6,23,33,34,38–40] According to Akgungor and Akkayan,[11] the self-etching primer Clearfil Liner Bond 2V did not show regional differences in post-space bonding, unlike the single bottle adhesive Excite, which exhibited significantly lower strength at the apical level. Goracci et al.[19] observed a higher bond strength in the coronal sections for Excite/Variolink II, but similar values for RelyX Unicem.
It has been shown that tubule density is greater in the coronal and middle thirds than in the apical region of the root canal,[41] and the diameter of the tubules decreases in the apical direction.[29] The difference in the number of tubules may explain why the strongest adhesion is achieved in the most coronal regions. In the presence of a greater number of tubules per mm2a stronger bond will be expected, because the adhesion may be enhanced by the penetration of the resin into the tubules.[42] Furthermore, it is shown that dentin hybridization is not uniform in the apical region of the root canal dentin and the lateral branches of the resin tags are not observed in the apical part of the interface post-adhesive system.[41]
Some methodological factors might have contributed to the discrepancies in bond strength values, such as, better accessibility of the coronal portion of the root canal, which made it easier to etch and apply the adhesive agents.[33,39] In addition, a reduction of light energy during transmission would decrease polymerization of the bonding agent at the medium and apical regions.[29]
However, some other studies[7,31,43] found no significant differences in the bond strengths between the different regions of the bonded posts to root canal dentin.
In this study, the mode of pushing out fiber posts was not evaluated. The specimens were prepared with no coronal tooth structure. However, it was suggested that the amount of remaining coronal tooth structure played a major role in the longevity of the restoration of endodontically treated teeth.[44]
In the present study, the influences of fatigue loading and thermal cycling on the push-out bond strength of the glass fiber reinforced composite post system were not investigated.
CONCLUSION
Within the limitations of this in vitro study, the following conclusions were drawn:
There was no significant difference between the push-out bond strengths of glass fiber reinforced composite posts for self-etching and conventional resin cements
The coronal region of the root dentin showed a significantly higher bond strength of the glass fiber reinforced composite post than the apical region.
Footnotes
Source of Support: Grant No. 388060 from Research Council of Isfahan University of Medical Sciences, Isfahan, Iran.
Conflict of Interest: None declared.
REFERENCES
- 1.Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: A literature review. J Endod. 2004;30:289–301. doi: 10.1097/00004770-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Morgano SM. Restoration of pulpless teeth: Application of traditional principles in present and future contexts. J Prosthet Dent. 1996;75:375–80. doi: 10.1016/s0022-3913(96)90028-1. [DOI] [PubMed] [Google Scholar]
- 3.Balbosh A, Kern M. Effect of surface treatment on retention of glass-fiber endodontic posts. J Prosthet Dent. 2006;95:218–23. doi: 10.1016/j.prosdent.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Kalkan M, Usumez A, Ozturk AN, Belli S, Eskitascioglu G. Bond strength between root dentin and three glass-fiber post systems. J Prosthet Dent. 2006;96:41–6. doi: 10.1016/j.prosdent.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Torbjoner A, Karlsson S, Syverud M, Hensten-Pettersen A. Carbon fiber reinforced root canal posts, mechanical and cytotoxic properties. Eur J Oral Sci. 1996;104:605–11. doi: 10.1111/j.1600-0722.1996.tb00149.x. [DOI] [PubMed] [Google Scholar]
- 6.Esclassan Noirrit E, Grégoire G, Cournot M. Morphological study of fiber-reinforced post-bonding system-root dentin interface by evaluation of two bonding systems. J Dent. 2008;36:204–13. doi: 10.1016/j.jdent.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Aksornmuang J, Foxton RM, Nakajima M, Tagami J. Microtensile bond strength of a dual-cure resin core material to glass and quartz fibre posts. J Dent. 2004;32:443–50. doi: 10.1016/j.jdent.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Monticelli F, Grandini S, Goracci C, Ferrari M. Clinical behavior of translucent-fiber posts: A 2-year prospective study. Int J Prosthodont. 2003;16:593–6. [PubMed] [Google Scholar]
- 9.Malferrari S, Monaco C, Scotti R. Clinical evaluation of teeth restored with quartz fiber-reinforced epoxy resin posts. Int J Prosthodont. 2003;16:39–44. [PubMed] [Google Scholar]
- 10.D’Arcangelo C, Cinelli M, De Angelis F, D’Amario M. The effect of resin cement film thickness on the pull out strength of a fiber-reinforced post system. J Prosthet Dent. 2007;98:193–8. doi: 10.1016/S0022-3913(07)60055-9. [DOI] [PubMed] [Google Scholar]
- 11.Akgungor G, Akkayan B. Influence of dentin bonding agents and polymerization modes on the bond strength between translucent fiber posts and three dentin regions within a post space. J Prosthet Dent. 2006;95:368–78. doi: 10.1016/j.prosdent.2006.02.027. [DOI] [PubMed] [Google Scholar]
- 12.Ferrari M, Vichi A, Grandini S, Geppi S. Influence of microbrush on efficacy of bonding into root canals. Am J Dent. 2002;15:227–31. [PubMed] [Google Scholar]
- 13.Mannocci F, Innocenti M, Ferrari M, Watson TF. Confocal and scanning electron microscopic study of teeth restored with fiber posts, metal posts, and composite resins. J Endod. 1999;25:789–94. doi: 10.1016/s0099-2399(99)80298-2. [DOI] [PubMed] [Google Scholar]
- 14.Vichi A, Grandini S, Ferrari M. Comparison between two clinical procedures for bonding fiber posts into a root canal: A microscopic investigation. J Endod. 2002;28:355–60. doi: 10.1097/00004770-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Nergiz I, Schmage P, Ozcan M, Platzer U. Effect of length and diameter of tapered posts on the retention. J Oral Rehabil. 2002;29:28–34. doi: 10.1046/j.1365-2842.2002.00806.x. [DOI] [PubMed] [Google Scholar]
- 16.Sahafi A, Peutzfeldt A, Asmussen E, Gotfredsen K. Bond strength of resin cement to dentin and to surface-treated posts of titanium alloy, glass fiber, and zirconia. J Adhes Dent. 2003;5:153–62. [PubMed] [Google Scholar]
- 17.Rosin M, Splieth C, Wilkens M, Meyer G. Effect of cement type on retention of a tapered post with a self-cutting double thread. J Dent. 2000;28:577–82. doi: 10.1016/s0300-5712(00)00045-2. [DOI] [PubMed] [Google Scholar]
- 18.Bitter K, Priehn K, Martus P, Kielbassa AM. In vitro evaluation of push-out bond strengths of various luting agents to tooth-colored posts. J Prosthet Dent. 2006;95:302–10. doi: 10.1016/j.prosdent.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 19.Goracci C, Tavares AU, Fabianelli A, Monticelli F, Raffaelli O, Cardoso PC, et al. The adhesion between fiber posts and root canal walls: Comparison between microtensile and push-out bond strengths measurements. Eur J Oral Sci. 2004;112:353–61. doi: 10.1111/j.1600-0722.2004.00146.x. [DOI] [PubMed] [Google Scholar]
- 20.Hedlund SO, Johansson NG, Sjogren G. Retention of prefabricated and individually cast root canal posts in vitro. Br Dent J. 2003;195:155–8. doi: 10.1038/sj.bdj.4810405. [DOI] [PubMed] [Google Scholar]
- 21.O’Keefe KL, Miller BH, Powers JM. In vitro tensile bond strength of adhesive cements to new post materials. Int J Prosthodont. 2000;13:47–51. [PubMed] [Google Scholar]
- 22.Sahafi A, Peutzfeldt A, Asmussen E, Gotfredsen K. Retention and failure morphology of prefabricated posts. Int J Prosthodont. 2004;17:307–12. [PubMed] [Google Scholar]
- 23.Perdigao J, Geraldeli S, Lee IK. Push-out bond strengths of tooth colored posts bonded with different adhesive systems. Am J Dent. 2004;17:422–6. [PubMed] [Google Scholar]
- 24.Asmussen E, Attal JP, Degrange M. Factors affecting the adherence energy of experimental resin cements bonded to a nickel-chromium alloy. J Dent Res. 1995;74:715–20. doi: 10.1177/00220345950740021501. [DOI] [PubMed] [Google Scholar]
- 25.Caputo AA, Standlee JP. Endodontic dowel retention with resinous cements. J Prosthet Dent. 1992;68:913–7. doi: 10.1016/0022-3913(92)90550-t. [DOI] [PubMed] [Google Scholar]
- 26.Mendoza DB, Eakle WS. Retention of posts cemented with various dentinal bonding cements. J Prosthet Dent. 1994;72:591–4. doi: 10.1016/0022-3913(94)90290-9. [DOI] [PubMed] [Google Scholar]
- 27.Zicari F, Couthino E, De Munck J, Poitevin A, Scotti R, Naert I, et al. Bonding effectiveness and sealing ability of fiber-post bonding. Dent Mater. 2008;24:967–77. doi: 10.1016/j.dental.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 28.Rathke A, Haj-Omer D, Muche R, Haller B. Effectiveness of bonding fiber posts to root canals and composite core build-ups. Eur J Oral Sci. 2009;117:604–10. doi: 10.1111/j.1600-0722.2009.00668.x. [DOI] [PubMed] [Google Scholar]
- 29.Topcu FT, Erdemir U, Sahinkesen G, Mumcu E, Yildiz E, Uslan I. Push-out bond strengths of two fiber post types bonded with different dentin bonding agents. J Biomed Mater Res B Appl Biomater. 2010;93:359–66. doi: 10.1002/jbm.b.31590. [DOI] [PubMed] [Google Scholar]
- 30.Lopes GC, De Carvalho Cardoso P, Cardoso Vieira L, Baratieri L. Microtensile bond strength to root canal vs. pulp chamber dentin: effect of bonding strategies. J Adhes Dent. 2004;6:129–33. [PubMed] [Google Scholar]
- 31.Foxton RM, Nakajima M, Tagami J, Miura H. Adhesion to root canal dentine using one and two-step adhesives with dual-cure composite core materials. J Oral Rehabil. 2005;32:97–104. doi: 10.1111/j.1365-2842.2004.01404.x. [DOI] [PubMed] [Google Scholar]
- 32.Inoue S, Vargas MA, Abe Y, Yoshida Y, Lambrechts P, Vanherle G, et al. Microtensile bond strength of eleven contemporary adhesives to dentin. J Adhes Dent. 2001;3:237–45. [PubMed] [Google Scholar]
- 33.Perdigao J, Lopes MM, Gomes G. Interfacial adaptation of adhesive materials to root canal dentin. J Endod. 2007;33:259–63. doi: 10.1016/j.joen.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 34.Giachetti L, Grandini S, Calamai P, Fantini G, Scaminaci Russo D. Translucent fiber post cementation using light- and dual-curing adhesive techniques and a self-adhesive material: push-out test. J Dent. 2009;37:638–42. doi: 10.1016/j.jdent.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 35.Yoshiyama M, Matsuo T, Ebisu S, Pashley D. Regional bond strengths of self-etching/self-priming adhesive systems. J Dent. 1998;26:609–16. doi: 10.1016/s0300-5712(97)00046-8. [DOI] [PubMed] [Google Scholar]
- 36.Goracci C, Sadek FT, Fabianelli A, Tay FR, Ferrari M. Evaluation of the adhesion of fiber posts to intraradicular dentin. Oper Dent. 2005;30:627–35. [PubMed] [Google Scholar]
- 37.Goracci C, Grandini S, Bossù M, Bertelli E, Ferrari M. Laboratory assessment of the retentive potential of adhesive posts: A review. J Dent. 2007;35:827–35. doi: 10.1016/j.jdent.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 38.Kurtz JS, Perdigao J, Geraldeli S, Hodges JS, Bowles WR. Bond strengths of tooth-colored posts, effect of sealer, dentin adhesive, and root region. Am J Dent. 2003;16:31–6. [PubMed] [Google Scholar]
- 39.Mallmann A, Jacques LB, Valandro LF, Mathias P, Muench A. Microtensile bond strength of light- and self-cured adhesive systems to intraradicular dentin using a translucent fiber post. Oper Dent. 2005;30:500–6. [PubMed] [Google Scholar]
- 40.Mumcu E, Erdemir U, Topcu FT. Comparison of micro push-out bond strengths of two fiber posts luted using simplified adhesive approaches. Dent Mater J. 2010;29:286–96. doi: 10.4012/dmj.2009-089. [DOI] [PubMed] [Google Scholar]
- 41.Vichi A, Grandini S, Davidson CL, Ferrari M. An SEM evaluation of several adhesive systems used for bonding fiber posts under clinical conditions. Dent Mater. 2002;18:495–502. doi: 10.1016/s0109-5641(01)00065-3. [DOI] [PubMed] [Google Scholar]
- 42.Chapell RP, Cobb CM, Spencer P, Eick JD. Dentin tubule anastomosis: A potential factor in dentinal adhesive bonding? J Prosthet Dent. 1994;72:183–8. doi: 10.1016/0022-3913(94)90078-7. [DOI] [PubMed] [Google Scholar]
- 43.Gaston BA, West LA, Liewehr FR, Fernandes C, Pashley DH. Evaluation of regional bond strength of resin cement to endodontic surfaces. J Endod. 2001;27:321–4. doi: 10.1097/00004770-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 44.Zalkind M, Shkury S, Stern N, Heling I. Effect of prefabricated metal post-head design on the retention of various core materials. J Oral Rehabil. 2000;27:483–7. doi: 10.1046/j.1365-2842.2000.00535.x. [DOI] [PubMed] [Google Scholar]


