Abstract
Background
Culturally-adapted interventions are needed to reduce diabetes-related morbidity and mortality among Native Hawaiian and Pacific People.
Purpose
To pilot test the effectiveness of a culturally-adapted diabetes self-management intervention.
Methods
Participants were randomly assigned in an unbalanced design to the Partners in Care intervention (n=48) or wait list control group (n=34). Assessments of hemoglobin A1c, understanding of diabetes self-management, performance of self-care activities, and diabetes-related distress were measured at baseline and 3 months (post intervention). Analysis of covariance was used to test between-group differences. The community steering committee and focus group data informed the cultural adaptation of the intervention.
Results
There were significant baseline adjusted differences at 3 months between the Partners in Care and wait list control group in intent-to-treat (p<0.001) and complete case analyses (p<0.0001) for A1c, understanding (p<0.0001), and performing diabetes self-management (p<0.0001).
Conclusions
A culturally-adapted diabetes self-management intervention of short duration was an effective approach to improving glycemic control among Native Hawaiian and Pacific Islanders.
Keywords: Health disparities, Native Hawaiian and Pacific People, diabetes self-management, intervention, culturally adapted, randomized controlled trial, community-based, peer educators
Introduction
Although the overall health of the US population has improved over the last 2 decades, profound disparities persist in the burden of illness and death experienced by racial and ethnic groups (1). Diabetes, in particular, presents a significant public health burden in terms of morbidity, mortality, and economic costs (2). Mortality rates from heart disease as a complication of diabetes, as well as risk for stroke, are two to four times higher in adults with diabetes when compared with non-diabetic individuals. Early detection and treatment, and appropriate self-management is critical to reducing the risk of developing complications and to improve quality of life and health outcomes; however, it requires addressing the many barriers that prevent patients and providers from achieving established treatment goals.
Type 2 Diabetes among Native Hawaiians and Pacific People
Of Hawaii’s 1.3 million residents, 26% identify themselves as Native Hawaiian or Pacific Islander (3). There has been a long-standing concern about the disproportionate burden of type 2 diabetes in these ethnic groups. The overall prevalence of type 2 diabetes in Hawaii in 2008 was 8.2%, comparable to that of the U.S. overall prevalence (4). However there is considerable difference in prevalence by race and ethnicity. Native Hawaiians have the highest prevalence of diagnosed type 2 diabetes ranging from 19% to 22%, and from 16% to 35% for impaired glucose tolerance (5-7). The prevalence of diabetes among Whites and Japanese Americans is 3% and 7%, respectively. Native Hawaiians are an average of seven years younger when diagnosed with diabetes compared to Whites and Japanese Americans. Moreover, Native Hawaiians die of diabetes at a rate of 117 per 100,000 compared to the average rate of 53 per 100,000 for other racial/ethnic groups (8). The extent of unmanaged diabetes in Native Hawaiian and other Pacific Islanders is evident not only in mortality rates, but in medical complications and preventable hospitalizations related to diabetes. Native Hawaiians and Pacific Islanders account for over 50% of chronic dialysis patients in Hawaii (9, 10).
Diabetes Self-Management Education
Type 2 diabetes has been recognized as one of the most challenging chronic illnesses to manage (11). A diagnosis of diabetes imposes multiple daily demands on people with diabetes and their families. The purpose of diabetes education is to support informed decision making, self-care behaviors, problem solving, and active collaboration with the health care team, and to improve clinical outcomes, health status, and quality of life (12). Diabetes self-management education has been shown to be effective in improving self-management behaviors. However, in Hawaii, only an estimated 55% of individuals with diabetes have elected to participate in diabetes education programs, with Native Hawaiians being less likely than Caucasians and Japanese to do so (13, 14). While numerous diabetes self-management education interventions have proven efficacious in improving blood glucose control (15-24), few Native Hawaiians and Pacific Islanders have been included in these studies (25).
The purpose of this study was to evaluate a culturally adapted community-based diabetes self-management intervention, called Partners in Care, among Native Hawaiians and Pacific Islanders. The primary study hypothesis was that the Partners in Care intervention group would experience greater improvements in A1c, a measure of blood glucose control, compared to a group that did not receive the intervention. Our secondary hypotheses were that the Partners in Care intervention group would have greater improvements in understanding and performing self-care activities, and reduced diabetes-related distress compared to the group that did not receive the intervention.
Methods
Study Design
We conducted a two-arm randomized controlled trial (intervention vs. control) of a diabetes self-management educational intervention, called Partners in Care, that was designed to improve A1c and reduce and/or prevent diabetes-related complications. Participants were recruited from 2 community-based health centers and one Native Hawaiian community organization. After participants signed a consent form at their baseline visit, they were randomly assigned to either the Partners in Care intervention or a wait-list control group. After randomization, wait-list control participants were informed that they should continue to manage their diabetes as usual. They did not receive further contact, information, or educational materials from study staff until it was time to schedule the 3 month assessment, and their subsequent voluntary participation in the Partners in Care intervention. All wait list control participants were invited to crossover to the intervention after completion of the 3 month assessment.
From January to February 2011, community peer educators recruited potential participants through flyers and word of mouth to participate in the Partners in Care intervention. Individuals were eligible if they had self-reported physician-diagnosed type 2 diabetes, were 18 years of age or older, self-reported Native Hawaiian, Filipino, or other Pacific Islander ethnic background, English-speaking, and baseline A1c >7%. Of the 91 individuals identified across the three sites, 82 met the eligibility criteria and agreed to participate, gave written informed consent, and completed the baseline survey administered at the community site by study staff (Figure 1). The study protocol was approved by the Native Hawaiian Health System Institutional Review Board and the University of Hawaii Committee on Human Studies.
Figure 1.
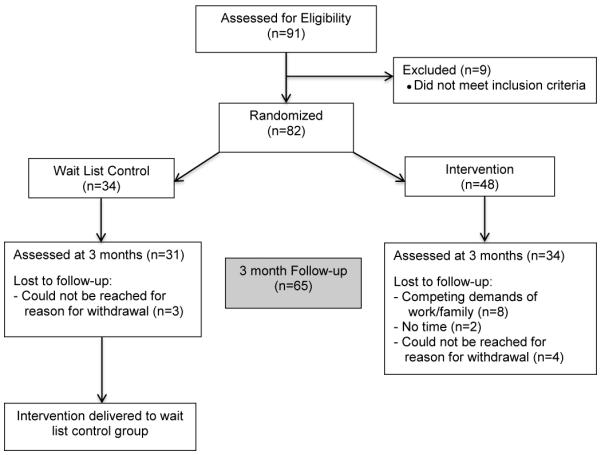
CONSORT diagram of Partners in Care study participation.
The Partners in Care intervention was part of an existing community-based participatory research project called the PILI Òhana Project, comprised of community leaders and health advocates from four distinct community organizations serving Native Hawaiians and Pacific Islanders, and researchers from the University of Hawaii, Department of Native Hawaiian Health. They served as the intervention steering committee and assisted in the planning and implementation of the Partners in Care intervention (26). Given a concern for diabetes-related complications in their communities, the community partners expressed a desire to offer the Partners in Care intervention to individuals as soon as possible. Therefore, an unbalanced randomization was decided upon with 60% randomized to the intervention and 40% to the wait list group. Randomization was based on a computerized random number generator. University study staff prepared sequentially numbered sealed envelopes containing the randomization assignment for each participant for the assessors in each site. Random assignments were made by assessors after informed consent and the baseline assessment were completed at the baseline visit. Randomization procedures resulted in a final sample consisting of approximately 60% in the intervention group and 40% in the wait-list control group.
The Partners in Care intervention was designed to reduce risk factors associated with diabetes complications by increasing participants’ understanding and practice of diabetes self-management activities. Building on culturally relevant knowledge and activities, the program sought to help participants gain knowledge and skills related to blood glucose monitoring, adherence to medication therapy, healthy eating, physical activity, and stress reduction. The curriculum also provided skill-building activities to improve communication with health care providers and help participants become better consumers of diabetes-related healthcare.
The Partners in Care curriculum, previously designed and evaluated with African Americans and Latinos, was adapted for this intervention (27-29). To adapt the intervention, focus groups with Native Hawaiians and Pacific Islanders were conducted to provide guidance regarding the content, format, and method of delivery of the intervention. In the focus groups, participants discussed facilitators and challenges to diabetes self-management, concerns of potential diabetes-related complications, the desire for a group-based educational format to facilitate social support, and to have a program in a convenient community location delivered by people that were from their community and/or Native Hawaiian or Pacific Islander. Participants wanted to know about diabetes medications and possible side effects, the relationship between food consumed and blood glucose, and what types of examinations they should receive from their health care provider, types of diabetes complications and how to prevent them, how to understand glucose numbers and A1c, and how to take action to control blood glucose and A1c.
The peer educators and steering committee members also contributed local and cultural knowledge during adaptation by reviewing written materials and making suggestions for visuals and hands-on activities. Peer educators who delivered Partners in Care had previously delivered an obesity prevention curriculum to community participants and had received prior training in group facilitation, intervention research, survey administration, and recruitment and retention methods. Images of Hawaiì, local foods, physical activities, and people were included to convey relevance to participants. Peer educators from the participating communities delivered the intervention and used “local” language and examples to convey some of the educational content. By using a culturally relevant context to discuss behavior change, the information about diabetes and self-management becomes more meaningful for the intended audience (30). Sociocultural strategies, which presented diabetes in the context of cultural values and characteristics of the participants, were incorporated into the intervention to increase salience. For example, through the use of a story depicting local characters at the beginning of each lesson, and participants sharing personal experiences with diabetes, the tradition of families and communities working together was reinforced. Storytelling allows the facilitator to use metaphors to link an individual’s situation to effective self-management behaviors. Participants were asked to set a goal at the end of each lesson that was related to the lesson topic. At each subsequent lesson, the peer educator devoted time for participants to discuss successes and challenges to achieving their goals. Additional intervention characteristics, one of the stories, and the format are described in detail in Appendix 1 in the Electronic Supplementary Material.
Curriculum materials emphasized American Diabetes Association clinical guideline goals for blood glucose, A1c, blood pressure, and lipids (31). Social cognitive theory provided the conceptual foundation for Partners in Care with an emphasis on behavioral capability, self-control procedures, emotional coping response, and self-efficacy. Social cognitive theory constructs (32, 33) were combined with selected cultural symbols and themes, cultural patterns and concepts, values, norms, and relationships to promote self-care activities (see Appendix 2 in the Electronic Supplementary Material). Intervention activities were hypothesized to improve psychosocial variables of problem solving and social support, along with understanding and performing diabetes self-management activities. These variables were hypothesized to lead to improvements in self-care behaviors such as self-blood glucose monitoring and medication adherence, and in turn lead to improved A1c. Twelve one-hour group meetings were delivered by trained peer educators in 3 community locations from March to May 2011. The peer educators were trained by research staff to deliver the curriculum intervention during a 4-hour group training, and a facilitator’s manual was provided. The materials are written in a conversational tone, in plain English, and intended to be read as a script by the peer educators for the purpose of fidelity to the intervention. Research staff observed two intervention meetings for each peer educator to document fidelity to the curriculum, questions asked by participants, and general satisfaction.
Participants were assessed at baseline and 3 months (post intervention) by trained study staff using a standardized protocol to obtain demographic, clinical, behavioral, and knowledge variables through in-person interview methods. The specific measures were based on the study outcomes of interest, content of the intervention, and the theoretical underpinnings of the study. Participants received a $20 gift card for the completion of each assessment. Survey completion times ranged from 20 to 40 minutes.
Outcome Measures
The primary outcome of this study was A1c which is measured as a percentage of hemoglobin that is glycated (expressed as A1c %). In this study, A1c was measured using a DCA 2000 analyzer (Bayer, West Haven, CT) which requires a small drop of blood from a finger stick, and results are available within 5-6 minutes.
Secondary outcomes of this study were diabetes self-management understanding, performance of self-care activities, and diabetes-related distress. To assess understanding of diabetes self-management, a subscale from the Diabetes Care Profile (34) was used. We chose to use the Understanding subscale because it reflected the information that was provided in Partners in Care. The Understanding subscale consists of 12 questions and asks respondents to rate their understanding of aspects of diabetes self-care on a Likert scale from 1 (Poor) to 5 (Excellent). The numbered responses were summed across the 12 questions and ranged from 12 indicating poor overall understanding of diabetes self-management activities to 60 indicating excellent understanding (35, 36). In our study, the reliability coefficient (Cronbach’s alpha) of the Diabetes Care Profile subscale was 0.93.
To measure performance of diabetes self-care activities, 7 of 11 items in the Summary of Diabetes Self-Care Activities (SDSCA) (37) were used. The SDSCA assesses the frequency with which an individual followed a diabetes self-care routine during the prior 7 days in five domains: diet, exercise, blood glucose monitoring, foot care, and medication adherence. In the survey, each participant indicated the number of days during the past week that s/he: 1) took their recommended insulin or diabetes pills, 2) took the recommended insulin dose or number of diabetes pills, 3) followed a healthful eating plan, 4) tested blood sugar at least as often as the doctor recommended, 5) exercised for at least 30 minutes, 6) checked their feet, and 7) smoked a cigarette. Participants could respond: not at all during the past 7 days, 2-3 days, 4-6 days, or 7 days. Item scores were averaged resulting in an overall score for self-care activity. Scores ranged from 7 (no weekly participation in diabetes self-care activity) to 28 (participation in diabetes self-care activities every day during the past week). The reliability coefficient of the SDSCA in our study was 0.70.
To measure diabetes-related distress, the revised Problem Areas in Diabetes 2 (38) scale was administered. Problem Areas in Diabetes 2 is a 20-item questionnaire that measures a wide range of feelings related to living with diabetes and its treatment, including guilt, anger, depressed mood, worry, and fear. The survey uses a five-point Likert-scale with options ranging from “0-not a problem” to “4-serious problem”. Summing all item scores and multiplying by 1.25 resulted in an overall score from 0-100, with higher scores indicating greater diabetes-related emotional distress. The reliability coefficient in our study was 0.97.
A lipid panel was assessed using the Cholestech analyzer which requires a finger stick sample of blood, and results are available within 5-6 minutes. Finally, at each assessment two measures of systolic and diastolic blood pressure were obtained and averaged for analysis to yield one average measure for systolic blood pressure and one average measure for diastolic blood pressure. Two measures each of height and weight were also taken and averaged for analysis. At the end of each assessment, every participant received a form with their individual clinical values. The values recommended in the American Diabetes Association Standards of Medical Care were presented beside their value for each measure, along with suggestions on how to achieve the recommended values. For example, next to A1c, the suggestion provided was, “Take diabetes medicine as prescribed by your doctor, lose weight by eating healthy and exercising.”
Statistical Analysis
All data were entered and verified, and scores were calculated for multiple-item instruments. Summary statistics including frequency distributions, means and other descriptive analyses of variables were conducted to provide an overview of the characteristics of participants in both groups. We also examined descriptive statistics to ensure that data met statistical test assumptions. T-tests and χ2 were used to test baseline between-group differences. Analyses were conducted using all available data at baseline (n=82) and 3 months (n=65) assuming data were missing at random. Intent-to-treat analyses were also conducted by imputing missing data with the baseline observation carried forward.
To test between-group differences in A1c at 3 months we used the change value (Baseline A1c – 3 month A1c) as the dependent variable in the analysis of covariance (ANCOVA) model adjusting for baseline A1c. In separate models, we tested between-group differences in understanding, self-care activities, and diabetes-related distress using ANCOVA with the change scores from baseline to 3 months as dependent variables and baseline scores as covariates. Despite three significant baseline differences between the intervention and control group, we did not include education, systolic blood pressure, or diet/meal plan adherence as covariates in the final models because: 1) they were not correlated with our outcome (see Appendix 3 in the Electronic Supplementary Material), and 2) including them as covariates yielded the same results (data not shown) as those in the final models reported.
Withdrawal from the study was significantly higher in the intervention group compared to the wait list group (p=0.02). Participants that withdrew from the study were significantly younger (p=0.001) and had a lower score on the Diabetes Care Profile that measured understanding of self-management (p=0.03). Therefore, age and baseline understanding of diabetes self-management were included as covariates in all between group comparisons at 3 months. Effect sizes were obtained in the ANCOVA modeling procedure and are based upon the comparison of the change scores between the intervention and control group. Analyses were conducted using SPSS version 20.0 (SPSS, Inc., Chicago, IL) and SAS 9.2 (SAS Institute Inc., Cary, NC). All reported p-values are for two-sided tests with effects considered statistically significant at p<0.05.
Results
Participants
Of the 82 randomized participants, 48 were assigned to the Partners in Care intervention and 34 to the wait list control group (Table 1). The average age was 53 years in the intervention group and 55 years in the control group. More than half of participants in each group were female and were currently married. There were three significant baseline differences between the treatment groups: educational level, self-report of currently following a diet or meal plan, and systolic blood pressure. Significantly more intervention participants had a high school education or less. Among wait list control participants, systolic blood pressure was significantly higher and more control participants reported currently following a diet or meal plan compared to the intervention group.
Table 1.
Baseline characteristics of Partners in Care study participants by treatment group.
| Variable | Partners in Care N=48 |
Control N=34 |
Group differences (p value) |
|---|---|---|---|
| Age, years, mean (SD) | 53 (12) | 55 (10) | 0.36 |
| Female (%) | 63 | 62 | 0.99 |
| Education, ≤High School (%) | 83 | 62 | 0.04 |
| Marital Status (%) | |||
| Currently Married | 60 | 58 | |
| Never married/divorced/widow | 40 | 42 | 0.82 |
| Employment Status (%) | |||
| Working | 31 | 35 | |
| Looking for Work | 13 | 3 | |
| Other (Retired, student, homemaker) | 56 | 62 | 0.31 |
| Age first told you had diabetes, years, mean (SD) | 38 (18) | 39 (16) | 0.73 |
| Previously taken a diabetes class (%) | 48 | 58 | 0.12 |
| Currently following a diet or meal plan (%) | 23 | 53 | 0.01 |
| Prescribed diabetes pills (%) | 69 | 76 | 0.36 |
| Prescribed insulin (%) | 56 | 46 | 0.32 |
| A1c, mean (SD) | 9.9 (2.0) | 9.8 (2.2) | 0.80 |
| Systolic Blood Pressure, mean (SD) | 190 (27) | 208 (35) | 0.02 |
| Diastolic Blood Pressure, mean (SD) | 113 (23) | 119 (22) | 0.30 |
| Lipids, mean (SD) | |||
| Total Cholesterol | 189 (51) | 195 (51) | 0.56 |
| LDL | 101 (38) | 105 (44) | 0.73 |
| HDL | 36 (10) | 35 (12) | 0.78 |
| Triglycerides | 270 (167) | 272 (135) | 0.94 |
| Body Mass Index, kg/m2, mean (SD) | 36 (12) | 38 (8) | 0.51 |
| Problem Areas in Diabetes Score, mean (SD) | 31 (29) | 24 (24) | 0.30 |
| Diabetes Care Profile, mean (SD) | 30 (9) | 33 (11) | 0.16 |
| Summary of Diabetes Self-Care Attitudes, mean (SD) |
19 (5) | 20 (5) | 0.45 |
Group differences p value based on χ2 and t tests, as appropriate.
- Problem Areas in Diabetes: scored 0-100 with higher numbers indicating more diabetes-related distress.
- Diabetes Care Profile: range from 12-60 with higher scores indicating more understanding of diabetes self-management activities.
- Summary of Diabetes Self-Care Attitudes: Range from 7-28 with higher numbers indicating a higher frequency of engaging in diabetes self-management activities during the past 7 days.
Retention
Of the 48 participants assigned to the intervention, 34 (71%) completed the 3 month assessment. Of the 34 participants allocated to the wait list control group, 31 (91%) completed the 3 month assessment. There was a higher attrition rate in the Partners in Care group (29%) at 3 months than in the wait list group (9%). Among participants that we could reach after they withdrew from the study, 8 of the intervention participants stated that they could not participate due to competing demands of work and family, and 2 intervention participants said that they did not have the time to participate. Despite several attempts to contact the remaining participants that dropped out of the study, four participants randomized to the intervention and three randomized to the wait list control group could not be reached to determine their reasons for dropping out of the study.
Outcome Analyses
As hypothesized, there were significant baseline adjusted differences at 3 months between the Partners in Care and wait list control group in both the intent-to-treat (p=0.001) and complete case analyses (p<0.0001) for A1c, understanding (p<0.0001), and performing diabetes self-management (p<0.0001) (Table 2). Effect size for the change in A1c was small, and moderate for the change in understanding and performing self-management in the complete case analysis. The change in diabetes-related distress was significant only in the complete case analysis (p=0.04).
Table 2.
Intervention effects on primary and secondary outcomes at baseline and 3 months.
| Baseline M (SD) |
3 month M (SD) |
Change ±SE | Group Differences (p value) |
|
|---|---|---|---|---|
| A1c | ||||
| Intention-to-treat | ||||
| Partners in Care (n=48) | 9.9 (2.0) | 8.9 (1.7) | -1.1 ±0.2 | |
| Control (n=34) | 9.8 (2.2) | 9.4 (2.2) | -0.3 ±0.2 | 0.001 |
| Effect Size | 0.13 | |||
| Complete cases | ||||
| Partners in Care (n=34) | 9.7 (2.1) | 8.2 (1.1) | -1.6 ±0.2 | |
| Control (n=31) | 9.8 (2.3) | 9.4 (2.2) | -0.3 ±0.2 | <0.0001 |
| Effect Size | 0.22 | |||
| Diabetes Care Profile | ||||
| Intention-to-treat | ||||
| Partners in Care (n=46) | 30 (9) | 43 (14) | 13.1 ±1.5 | |
| Control (n=34) | 33 (11) | 34 (11) | 1.8 ±1.8 | <0.0001 |
| Effect Size | 0.23 | |||
| Complete cases | ||||
| Partners in Care (n=33) | 32 (10) | 50 (9) | 18.8 ±1.5 | |
| Control (n=29) | 31 (10) | 33 (11) | 1.5 ±1.5 | <0.0001 |
| Effect Size | 0.53 | |||
|
Summary of Diabetes Self-Care Activities |
||||
| Intention-to-treat | ||||
| Partners in Care (n=47) | 19 (5) | 24 (4) | 4.9 ±0.6 | |
| Control (n=34) | 20 (5) | 21 (5) | 1.4 ±0.7 | <0.0001 |
| Effect Size | 0.17 | |||
| Complete cases | ||||
| Partners in Care (n=35) | 19 (4) | 26 (3) | 6.6 ±0.6 | |
| Control (n=26) | 19 (5) | 21 (6) | 1.8 ±0.7 | <0.0001 |
| Effect Size | 0.30 | |||
| Problem Areas in Diabetes | ||||
| Intention-to-treat | ||||
| Partners in Care (n=48) | 31 (29) | 23 (24) | -7.2 ±2.1 | |
| Control (n=34) | 25 (24) | 24 (22) | -2.9 ±2.5 | 0.19 |
| Effect Size | 0.02 | |||
| Complete cases | ||||
| Partners in Care (n=35) | 31 (31) | 20 (22) | -10.2 ±2.5 | |
| Control (n=30) | 24 (23) | 23 (21) | -2.7 ±2.6 | 0.04 |
| Effect Size | 0.07 |
Based on ANCOVAs with the change score from baseline to the 3 month assessment as the dependent variable adjusting for the baseline value of the dependent variables, age, and baseline understanding of diabetes self-management. Unadjusted means are presented in the table. Intent-to-treat analysis with missing data imputed by baseline observation carried forward.
Discussion
Partners in Care was a pilot study using a randomized controlled trial design in which 82 Native Hawaiians and Pacific Islanders were randomized to either a 3 month diabetes self-management intervention or a wait list control group. Our findings suggest that the culturally adapted, community-based diabetes self-management intervention delivered by peer educators over twelve sessions can significantly improve glycemic control and reduce risk factors associated with diabetes complications among Native Hawaiians and Pacific Islanders. Although the effect size for the change in A1c was small, a 1% decrease in A1c is associated with a dramatic reduction in myocardial infarctions, microvascular disease, and death (39).
The Partners in Care intervention findings are consistent with prior studies showing the efficacy of diabetes lifestyle interventions in improving understanding of diabetes self-management, performing self-care activities, and glycemic control (18, 23, 40-47). Similar diabetes education interventions with minority populations have achieved a 1% reduction in A1c post intervention (16, 48). This study also replicates a previously successful diabetes self-management intervention in a different setting, population, geographic location, and peer educators (27). Partners in Care is the first diabetes self-management intervention for Native Hawaiians and Pacific Islanders in Hawaii using a randomized controlled trial design (25).
The Partners in Care intervention was also successful in increasing understanding and performance of diabetes self-management. Effect sizes for understanding and performing self-management were moderate in the complete case analysis and somewhat smaller in the intent-to-treat analysis. While there was a statistically significant change in diabetes-related distress among participants in the complete case analysis, the magnitude of the change was very small. The lack of change in the Problem Areas in Diabetes score may be due, in part, to several of the Filipino participants’ cultural norm of not wanting to complain about the impact of their diabetes on their lives (reported by the Filipino peer educator). When analyzed separately, there was a significant difference in the mean baseline diabetes-related distress score for Filipinos and Native Hawaiians/other Pacific Islanders (5.0 vs 42.0). An alternative method of measuring diabetes-related distress may be needed for some populations.
Risk factors for preventing or delaying the onset of diabetes complications are complex and interdependent. A strength of this study was the way in which this complexity was addressed. The Partners in Care intervention combined community-based peer-led education, cultural components, preliminary formative research (focus groups with individuals from the participating communities), and a defined theoretical framework. Meta-analyses indicate that a combination of these approaches is associated with better outcomes compared to any single approach (49).
Despite the positive results, there are study limitations that deserve mention. While the overall retention rate was fairly high (79%), the attrition rate was higher among younger participants. Future studies should include methods to facilitate younger individual’s participation, such as offering classes after work or on weekends and providing childcare if needed. This study is also limited in that we did not assess the mechanisms contributing to intervention effects. Future studies should investigate components of the intervention and mechanisms by which they influence outcomes.
This study demonstrated that an appropriately designed, community-based program requiring little technology and few health care resources can have positive effects by improving understanding, self-care behaviors, and glycemic control among Native Hawaiians and Pacific People with type 2 diabetes. If the significant improvement in A1c can be sustained, the Partners in Care intervention has the potential to substantially reduce microvascular complications, morbidity, and health care utilization costs (39, 50, 51). Future research efforts should be aimed at confirming, enhancing, and sustaining the effect of this type of intervention among populations where health disparities exist. With the large number of Native Hawaiians and Pacific Islanders suffering from diabetes-related morbidity and mortality, a great need exists for improvement in methods of reaching people with diabetes that are culturally appropriate and have been systematically developed, implemented, and evaluated.
Supplementary Material
Acknowledgements
We are grateful to the Partners in Care study participants, and the community researchers who served as the critical link between the participants and the research team. We also thank our community partners Ke Ola Mamo, Kula no nā Po‘e Hawai‘i, and Kōkua Kalihi Valley Comprehensive Family Services for their guidance and participation.
Funding
This work was supported by the National Institute on Minority Health and Health Disparities (grant number R24MD001660-S1) of the National Institutes of Health and registered on ClinicalTrials.gov (NCT01042886), and the National Institute of Diabetes, Digestive, and Kidney Diseases (1K01DK090091-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of National Center on Minority Health and Health Disparities, the National Institute of Diabetes, Digestive, and Kidney Diseases, or National Institutes of Health.
Footnotes
Conflict of Interest: The authors have no conflict of interest to disclose.
Trial Registration: clinicaltrials.gov Identifier: NCT01093924
Contributor Information
Ka’Imi A. Sinclair, University of Hawaii, Department of Native Hawaiian Health, 651 Ilalo Street, Honolulu, HI, 96813, USA.
C. Thompson, University of Hawaii, Department of Native Hawaiian Health, 651 Ilalo Street, Honolulu, HI, 96813, USA
Emily K. Makahi, Ke Ola Mamo, 1505 Dillingham Blvd, Honolulu, HI, USA.
Cappy Shea-Solatorio, Kula No Na Poè Hawaiì, 2150 Tantalus Drive, Honolulu, HI 96813 USA.
Sheryl R. Yoshimura, Kokua Kalihi Valley Community Health Center, 2239 N. School St., Honolulu, HI 96819, USA.
J. Keawe‘aimoku Kaholokula, University of Hawaii, Department of Native Hawaiian Health, 651 Ilalo Street, Honolulu, HI, 96813, USA
REFERENCES
- 1.National Institutes of Health Strategic Plan on Minority Health Disparities. Retrieved November 20, 2011 from http://www2.niddk.nih.gov/AboutNIDDK/ReportsAndStrategicPlanning/Strategic_Plan_M inority_Health_Disparities.htm.
- 2.American Diabetes Association Economic consequences of diabetes mellitus in the US in 2002. Diabetes Care. 2003;26:917–932. doi: 10.2337/diacare.26.3.917. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Census Bureau State of Hawaii 2010 Census Demographic Profile. Retrieved May 6, 2012 from http://hawaii.gov/dbedt/info/census/Census_2010/demographic.
- 4.The Kaiser Family Foundation: State Health Facts Data Source: Behavioral Risk Factor Surveillance System, 2008; analysis by the National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition and Physical Activity, Centers for Disease Control and Prevention. available at http://apps.nccd.cdc.gov/BRFSS/list.asp?cat=DB&yr=2008&qkey=1363&state=All. Retrieved September, 2009, from statehealthfacts.org. [Google Scholar]
- 5.Grandinetti A, Kaholokula JK, Theriault AG, et al. Prevalence of diabetes and glucose intolerance in an ethnically diverse rural community of Hawaii. Ethn Dis. 2007;17:250–255. [PubMed] [Google Scholar]
- 6.Salvail F, Nguyen D. Have you ever been told by a doctor that you have diabetes? 2009 Apr 6; Retrieved. [Google Scholar]
- 7.Grandinetti A, Mau M, Curb J, et al. Prevalence of glucose intolerance among Native Hawaiians in two rural communities. Diabetes Care. 1998;21:549–554. doi: 10.2337/diacare.21.4.549. [DOI] [PubMed] [Google Scholar]
- 8.Maskarinec G. Diabetes in Hawaii: estimating prevalence from insurance claims data. AJPH. 1997;87:1717–1720. doi: 10.2105/ajph.87.10.1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.TransPacific Renal Network . Selected Demographics 2000. TransPacific Renal Network; San Rafael, CA: 2001. [Google Scholar]
- 10.United States Census Bureau . In: Census 2000 profiles of general demographic characteristics: Hawaii. U.S. Census Bureau, editor. Washington, D.C.: 2001. [Google Scholar]
- 11.Cox D, Gonder-Frederick L. Major developments in behavioral diabetes research. J Cons Clin Psych. 1992;60:628–638. doi: 10.1037//0022-006x.60.4.628. [DOI] [PubMed] [Google Scholar]
- 12.Funnell M, Brown T, Childs B. National standards for diabetes self-management education. Diabetes Care. 2007;30:1630–1637. doi: 10.2337/dc07-9923. [DOI] [PubMed] [Google Scholar]
- 13.Huang T, Salvail F, Nguyen D, et al. Adult diabetes prevalence measured from the HBRFSS. Hawaii State Department of Health; Honolulu, HI: 2004. [Google Scholar]
- 14.Furubayashi J, Look M. Type 2 diabetes in Native Hawaiians and Pacific Islanders in Hawaii. Pac Health Dialog. 2005;12:103–110. [PubMed] [Google Scholar]
- 15.Brown S. Effects of educational interventions in diabetes care: A meta-analysis of findings. Nursing Research. 1988;37:223–230. [PubMed] [Google Scholar]
- 16.Norris S, Engelgau M, Narayan V. Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care. 2001;24:561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- 17.Norris S, Lau J, Smith S, Schmid C, Engelgau M. Self-management education for adults with type 2 diabetes. Diabetes Care. 2002;25:1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 18.Wing R, Goldstein M, Acton K, Birch L. Behavioral science research in diabetes: Lifestyle changes related to obesity, eating behavior, and physical activity. Diabetes Care. 2001;24:117–123. doi: 10.2337/diacare.24.1.117. [DOI] [PubMed] [Google Scholar]
- 19.Whittemore R. Strategies to facilitate lifestyle change associated with diabetes mellitus. J Nurs Scholarship. 2000;32:225–232. doi: 10.1111/j.1547-5069.2000.00225.x. [DOI] [PubMed] [Google Scholar]
- 20.Appel L. Lifestyle modification as a means to prevent and treat high blood pressure. J Am Soc Nephrol. 2003;14:S99–S102. doi: 10.1097/01.asn.0000070141.69483.5a. [DOI] [PubMed] [Google Scholar]
- 21.The Diabetes Prevention Program Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. NEJM. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boule N, Haddad E, Kenny G, Wells G, Sigal R. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus. JAMA. 2001;286:1218–1227. doi: 10.1001/jama.286.10.1218. [DOI] [PubMed] [Google Scholar]
- 23.Gary T, Genkinger J, Guallar E, Peyrot M, Brancati F. Meta-analysis of randomized educational and behavioral intervention in type 2diabetes. Diabetes Educator. 2003;29:488–501. doi: 10.1177/014572170302900313. [DOI] [PubMed] [Google Scholar]
- 24.The Diabetes Prevention Program Study Group The Diabetes Prevention Program: Description of the lifestyle intervention. Diabetes Care. 2002;25:2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mau M, Sinclair K, Saito E, Baumhofer K, Kaholokula J. Cardiometabolic health disparities in Native Hawaiians and other Pacific People. Epidmiol Rev. 2009;31:113–129. doi: 10.1093/ajerev/mxp004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nacapoy AH, Kaholokula JK, West MR, et al. Partnerships to address obesity disparities in Hawai’i: the PILI ‘Ohana Project. Hawaii Med J. 2008;67:237–241. [PMC free article] [PubMed] [Google Scholar]
- 27.Two Feathers J, Kieffer E, Palmisano G, et al. Racial and Ethnic Approaches to Community Health (REACH) Detroit Partnership: Improving diabetes-related outcomes among African American and Latino adults. AJPH. 2005;95 doi: 10.2105/AJPH.2005.066134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spencer M, Rosland A, Kieffer E, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: A randomized controlled trial. AJPH. 2011;101:2253–2260. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Two Feathers J, Kieffer E, Palmisano G, et al. The development, implementation and process evaluation of the REACH Detroit diabetes lifestyle intervention. Diabetes Educator. 2007;33:509–520. doi: 10.1177/0145721707301371. [DOI] [PubMed] [Google Scholar]
- 30.Kreuter M, Lukwago S, Bucholtz D, Clark E, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: Targeted and tailored approaches. Health Educ Behav. 2003;30:133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 31.Standards of medical care in diabetes--2010. Diabetes Care. 2010;33(Suppl 1):S11–61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 33.Baranowski T, Perry C, Parcel G. How individuals, environments, and health behavior interact: Social Cognitive Theory. 2nd Ed. Jossey-Bass; San Francisco: 1997. [Google Scholar]
- 34.Fitzgerald J, Davis W, Connell C, et al. Development and validation of the Diabetes Care Profile. Eval Health prof. 1996;19:208–230. doi: 10.1177/016327879601900205. [DOI] [PubMed] [Google Scholar]
- 35.Fitzgerald JT, Anderson RM, Gruppen LD, et al. The reliability of the Diabetes Care Profile for African Americans. Eval Health prof. 1998;21:52–65. doi: 10.1177/016327879802100103. [DOI] [PubMed] [Google Scholar]
- 36.Cunningham V, Mohler M, Wendel C, et al. Reliability and validity of the DCP among hispanic veterans. Eval Health prof. 2005;28:447–463. doi: 10.1177/0163278705281077. [DOI] [PubMed] [Google Scholar]
- 37.Toobert D, Hampson S, Glasgow R. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 38.Polonsky W, Anderson B, Lohrer P, et al. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 39.United Kingdom Prospective Diabetes Study Group (UKPDS) Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 40.Brown S. Meta-analysis of diabetes patient education research: Variations in intervention effects across subjects. Research in Nursing and Health. 1992;15:409–419. doi: 10.1002/nur.4770150603. [DOI] [PubMed] [Google Scholar]
- 41.Gilliland S, Azen S, Perez G, Carter J. Strong in Body and Spirit: Lifestyle intervention for Native American adults with diabetes in New Mexico. Diabetes Care. 2002;25:78–83. doi: 10.2337/diacare.25.1.78. [DOI] [PubMed] [Google Scholar]
- 42.Brown S, Garcia A, Kouzekanani K, Hanis C. Culturally competent diabetes self-management education for Mexican Americans. Diabetes Care. 2002;25:259–268. doi: 10.2337/diacare.25.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ciliska D, Miles E, O’Brien M, Turl C. Effectiveness of community-based interventions to increase fruit and vegetable consumption. J Nutr Educ Behav. 2000;32:341–352. [Google Scholar]
- 44.Agurs-Collins T, Kumanyika S, Ten Have T, Campbell L. A randomized controlled trial of weight reduction and exercise for diabetes management in older African American subjects. Diabetes Care. 1997;20:1503–1511. doi: 10.2337/diacare.20.10.1503. [DOI] [PubMed] [Google Scholar]
- 45.The Diabetes Prevention Program Reduction in the incidence of type 2 diabete with lifestyle intervention or metformin. NEJM. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26:1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 47.Warsi A, Wang P, LaValley M, Avorn J, Solomon D. Self-management education programs in chronic disease. Arch Intern Med. 2004;164:1641–1649. doi: 10.1001/archinte.164.15.1641. [DOI] [PubMed] [Google Scholar]
- 48.Norris S, Nichols P, Caspersen C, et al. Increasing diabetes self-management education in community settings. Am J Prev Med. 2002;22:39–66. doi: 10.1016/s0749-3797(02)00424-5. [DOI] [PubMed] [Google Scholar]
- 49.Brown S, Hannis C. Culturally competent diabetes education for Mexican Americans: The Starr County Study. Diabetes Educ. 1999;25:226–236. doi: 10.1177/014572179902500208. [DOI] [PubMed] [Google Scholar]
- 50.Khaw K, Wareham N, Luben R, et al. Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of European Prospective Investigation of Cancer and Nutrition (EPIC-Norfolk) BMJ. 2001;322:15–18. doi: 10.1136/bmj.322.7277.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wagner E. Effect of improved glycemic control on health care costs and utilization. JAMA. 2001;285:182–189. doi: 10.1001/jama.285.2.182. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


