Abstract
Objective
The use of estrogen and progesterone to manage vasomotor symptoms (i.e., hot flashes, night sweats) has declined due to concerns over their risks and there is an increased interest in alternate, effective, and low-risk treatments. This study reports the results of a randomized, controlled trial of clinical hypnosis in treating vasomotor symptoms among post-menopausal women.
Methods
Randomized, single-blind, controlled, clinical trial involving 187 post-menopausal women reporting a minimum of seven hot flashes per day, or at least 50 hot flashes a week at baseline between December 2008 and April 2012. Eligible participants received five weekly sessions of either clinical hypnosis or structured-attention control. Primary outcomes were hot flash frequency (subjectively and physiologically recorded) and hot flash score assessed by daily diaries at weeks 2–6, and 12. Secondary outcomes included measures of hot flash related daily interference, sleep quality and treatment satisfaction.
Results
In a modified intent-to-treat analysis that included all randomized participants that provided data, reported subjective hot flash frequency from baseline to week 12 showed a mean reduction of 55.82 hot flashes for the clinical hypnosis intervention (74.16%), versus a 12.89 hot flash reduction (17.13%) for the control (p<.001, 95% CI, 36.15–49.67). Mean reduction in hot flash score was 18.83 (80.32%) for the clinical hypnosis intervention as compared to 3.53 (15.38%) for the control (p<.001, 95% CI, 12.60–17.54). At 12 week follow-up, the mean reduction in physiologically monitored hot flashes was 5.92 (56.86%) for clinical hypnosis and .88 (9.94%) for the control (p<.001, 95% CI, 2.00–5.46). Secondary outcomes were significantly improved compared to control at 12 week follow-up in hot flash related interference (p<.001, 95% CI, 2.74–4.02), sleep quality (p<.001, 95% CI, 3.65–5.84), and treatment satisfaction (p<.001, 95% CI, 7.79–8.59).
Conclusion
Compared to a structured attention control, clinical hypnosis resulted in significant reductions in self-reported and physiologically measured hot flashes as well as hot flash scores in post-menopausal women.
Keywords: hypnosis, hot flash, hot flush, mind-body
Several meta-analyses and a Cochrane review indicate that additional clinical trials are needed to guide clinical practice decisions around the use of non-hormonal therapies for vasomotor symptoms (i.e., hot flashes, night sweats).1–4 Trials are needed to generate a sufficient evidence-base to guide clinical treatment decisions concerning use of non-hormonal therapies for vasomotor symptoms. As many as 80% of women experience vasomotor symptoms and nearly 20% find them intolerable.5 Sudden rushes of heat and sweating are often accompanied by increased heart rate, chills, shivering, clamminess, anxiety, feelings of nausea, a “head-ache”-like sensation, visible reddening and blotching of the face and neck, an increase in core body temperature, increased metabolism, and interrupted sleep.6–18 Symptoms generally wane five to seven years post menopause,19 but can persist in some women for over 20 years; with median symptom duration of approximately four years.20 Alternate non-hormonal pharmacotherapy, such as clonidine, gabapentin, and paroxetine, appear promising, but side-effects and cost can diminish long-term compliance.
Clinical hypnosis, a mind-body therapy designed to facilitate a hypnotic state, coolness and control of symptoms, appears promising, however no large scale, randomized, controlled trials have yet been published. Pilot data showed breast cancer survivors who received five weekly sessions of clinical hypnosis experienced a 69% reduction in hot flashes relative to baseline.21 These results are comparable or superior to results of open label studies with paroxetine and venlafaxine. 22,4,23–25 Thus, the purpose of this randomized controlled trial was to evaluate clinical hypnosis against structured attention control for the treatment of hot flashes in post-menopausal women. Primary outcomes were hot flash frequency (perceived and physiologically measured) and hot flash score (diary frequency × severity). Secondary outcomes were hot flash interference, sleep quality, and treatment satisfaction.
METHODS
Study Design
The study was conducted as a single-blind, randomized, clinical trial in central Texas evaluating the effectiveness of clinical hypnosis compared to an active, structured-attention control. The study was approved by the university institutional review board and all participants provided copies of written informed consent.
Patient Selection
Patients were recruited from December, 2008 to April, 2012 via newspaper advertisements, professional referrals, and television and billboard advertisement. Participants were eligible if they were postmenopausal, 18 years of age or older, had no menstrual period in the past 12 months, no menstrual period in the past 6 months and either (a) a medically documented history of a follicle-stimulating hormone level greater than 40 or (b) a bilateral oophorectomy. Further, participants were required to have a self-reported history of seven hot flashes per day at minimum, or 50 hot flashes per week, at baseline.
Participants were required to have discontinued estrogen/progestin containing products based on FDA draft recommendation for industry26: one week or longer for prior vaginal hormonal products (rings, creams, gels), four weeks or longer for prior transdermal estrogen alone or estrogen/progestin products, eight weeks or longer for prior oral estrogen and/or progestin therapy, eight weeks or longer for prior intrauterine progestin therapy, three months or longer for prior progestin implants and estrogen alone injectable drug therapy, and six months or longer for prior estrogen pellet therapy or progestin injectable drug therapy. Women were excluded if they were receiving any other treatment for hot flashes, using any complementary or alternative medical treatments for vasomotor symptoms (including soy, black cohosh, phytoestrogens, and any other mind-body techniques). Participants were excluded from the study if they had a history of psychosis, borderline personality disorder, or serious psychopathology as these diagnoses are considered to be contraindications for clinical hypnosis.
Data Collection
Potential participants were screened by telephone for eligibility. Women who met the eligibility criteria completed baseline measures including the Hot Flash Symptoms Diary27,28, physiological monitoring of hot flashes, and other secondary outcome measures. Random assignment was made by the study biostatistician from a confidential computer-generated list of permuted blocks of varying size. Participants were randomized by sealed envelope. The envelope was not opened by the research coordinator until the patient completed and provided their baseline data. Participants were then scheduled for five weekly sessions of either clinical hypnosis or structured attention. Participants completed follow-up assessments at weeks 6 and 12. Participants were paid after three intervention or control sessions and at the final follow-up contact, for a possible total of $300.
Treatment
The clinical hypnosis intervention followed a treatment manual and was delivered by therapists who were specifically trained in clinical hypnosis according to established training standards.29 The clinical hypnosis intervention consisted of hypnotic inductions and instruction in the practice of self-hypnosis towards the therapeutic goals of the reduction of hot flashes and improved sleep.30–37 In each 45-minute session, participants were provided specific suggestions for mental imagery for coolness, safe place imagery, and relaxation (individualized based on patient preference). Participants were also provided an audio recording of a hypnotic induction and tasked with the daily practice of self-hypnosis at home. Treatment fidelity and compliance was evaluated at each session by means of a checklist.
The structured attention control condition, designed to match the clinical intervention in therapist-exposure, therapeutic environment, interpersonal exchange, and encouragement was employed based on the recommendations for minimal-effect interventions.38 Structured attention matched the hypnotic intervention in that it consisted of five sessions where discussion of symptoms, attentive listening, interpersonal exchange, avoidance of negative suggestions, monitoring, measurement and encouragement were provided in a therapeutic environment with a clinician trained to deliver the control intervention, using a standard structured attention manual. However, no hypnotic inductions or cooling suggestions were provided. Each structured attention session lasted approximately 45 minutes and fidelity was determined by a checklist. Participants were given a cd that provided information about hot flashes and tasked with daily listening.
Measurements
Hot flash frequency and hot flash score were obtained using the Hot Flash Symptoms Diary 27,28. Participants recorded their hot flashes over seven days by daily frequency and severity, (mild, moderate, severe, and very severe) and the diary was administered at baseline, weeks 2–6, and at 12 week follow-up. This instrument provides a measure of hot flash frequency and hot flash score (product of frequency × severity).
A sternal skin conductance monitoring system was used to objectively measure hot flash frequency. The Biolog® ambulatory recorder39 recorded skin conductance levels using Biopac EL-507 silver/silver chloride electrodes for electrodermal activity and a 0.5 constant voltage circuit.40 Electrodes are 1.0 cm in diameter and filled with 0.5% chloride solid gel. 41 Electrodes are attached 1.5″ below the collarbones and 2″ on either side of the sternal mid-line. The Biolog® is programmed to sample 12-bit skin conductance data at 1 Hz (once per second). Customized software (FlashTrax, version 1.2, UFI, Morro Bay, CA) was used to evaluate hot flashes. Based on published norms,10–13 hot flashes were flagged if there was an increase in sternal skin conductance of at least 2 μmho within a 30 second period, with a 15-minute post-event lock-out. Each skin conductance track was evaluated by a trained expert, verifying that each skin conductance event matched published norms for vasomotor events. Physiological monitoring of hot flashes was recorded for 24-hours at baseline, week 6 and week 12.
Secondary outcomes included a measure of hot flash daily interference and sleep quality. To investigate the impacts of hot flashes on patient overall quality of life, the Hot Flash Related Daily Interference Scale was employed in this study.42 This measure has been shown to be internally consistent and valid.42 Data from this instrument were collected at baseline, week 6 and at 12 week follow-up. To investigate quality of sleep, participants were given the Pittsburg Sleep Quality Index43 at baseline, 6-weeks, and at 12-week follow-up. Treatment satisfaction was assessed at 12-week follow-up by means of a 0–10 rating; with 0 indicating the participant was ‘Dissatisfied’ and 10, ‘Completely Satisfied.’ Adverse events were assessed at each contact by patient self-report, and events were logged and reported to the institutional review board.
Statistical Analyses
The sample size was based on data from a pilot study that compared the hypnosis intervention to a no-treatment control21. We then estimated the power calculations cognizant of the placebo effect in hot flash treatment literature which reported effects of as large as a 30% reduction in hot flash frequencies and hot flash severity scores.27,28 Calculations were conducted using G*Power as it takes into account the expected effect size, desired power, correlation between pre- and post-test main effects, and sphericity.44 Given the effect size (d=.488) in pilot data,21 an alpha of .05, and power of .90, a total sample of 146 (73 in each arm) was determined.
The modified intention-to-treat analysis included all randomized participants who provided diary data, which were analyzed regardless of adherence to protocol. When appropriate, data were assessed for normality and homogeneity. Missing data were accounted for using maximum likelihood imputation.45,46 To test primary outcomes, two ANCOVAs with one between-subjects factor (experimental condition) and one covariate (pretest) were performed. Perceived frequency and physiologically recorded frequency were analyzed separately. In order to examine if the effects of the hypnosis intervention were maintained, analyses using a repeated measure (posttest, follow-up) were also conducted with the 12-week follow-up data. Four separate analyses were conducted. The hypotheses associated with secondary outcomes were tested using a series of ANCOVAs with pretest scores used as the covariate; follow-up data were analyzed using repeated measures ANCOVA analyses were conducted using the SPSS statistical software package, version 19 (SPSS Inc, Chicago, IL).
RESULTS
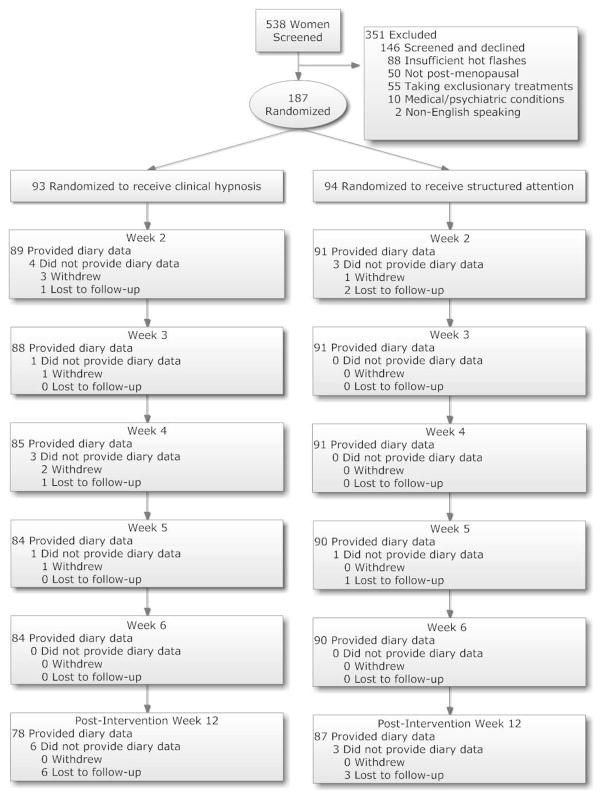
From December 2008 to April 2012, 538 women were screened to determine eligibility upon entrance in the study. Of these, 88 women did not meet the minimum hot flash inclusionary criteria, 50 were not classified as post-menopausal, 55 were receiving other simultaneous treatment for hot flashes, 10 were excluded for prohibitive medical/psychiatric diagnoses, 2 were non-English speaking, and 146 successfully screened, but failed to arrive for their baseline (Figure 1). Those remaining 187 women, who were eligible, provided written informed consent and were randomized at their baseline appointment.
Figure 1.
Participant flow chart.
Groups were matched in terms of age, race, marital status, education, onset of symptoms, and symptoms severity (Table 1). The participants ranged in age from 39–75 with a mean age of 54.61. The sample was largely White (68.8%, 78.7%), with African Americans (21.5%, 11.7%), and Hispanics (6.5%, 6.4%) following. The majority of the sample was married (61.3%, 69.1%), with educational level normally distributed. There were no statistically significant differences between groups in the onset of amenorrhea, menopausal symptoms, hot flashes, hot flash frequencies, and hot flash scores at baseline. Missing data accounted for less than 2% of the data analyzed and was prorated for incomplete diaries.
Table 1.
Patient demographicsa
| Characteristics | Treatment (n=93) | Control (n=94) |
|---|---|---|
| Age group, n (%) | ||
| 18–34 | 0 | 0 |
| 35–44 | 7 (7.5) | 4 (4.3) |
| 45–54 | 42 (45.2) | 43 (45.7) |
| 55–65 | 35(37.6) | 40 (42.6) |
| >65 | 9 (9.7) | 7 (7.4) |
| Age in years, mean (range) | 54.52 (39–75) | 54.71 (39–71) |
|
| ||
| Race, n (%) | ||
| American Indian | 2 (2.2) | 3 (3.2) |
| Asian | 1 (1.1) | 0 |
| African American | 20 (21.5) | 11 (11.7) |
| White | 64 (68.8) | 74 (78.7) |
| Hispanic | 6 (6.5) | 6 (6.4) |
|
| ||
| Marital status, n (%) | ||
| Married | 57 (61.3) | 65 (69.1) |
| Divorced | 8 (8.6) | 10 (10.6) |
| Separated | 5 (5.4) | 5 (5.3) |
| Single | 19 (20.4) | 12 (12.7) |
| Widowed | 4 (4.3) | 2 (2.1) |
|
| ||
| Education, n(%) | ||
| < HS | 10 (10.8) | 6 (6.4) |
| HS Diploma | 26 (28.0) | 26 (27.7) |
| College, Non degree | 20 (21.5) | 20 (21.3) |
| Associate Degree | 12 (12.9) | 12 (12.8) |
| Bachelor’s Degree | 14 (15.1) | 22 (23.4) |
| Graduate Degree | 11 (11.8) | 8 (8.5) |
|
| ||
| BMI, mean (SD) | 29.72 (6.56) | 28.13 (4.95) |
| < 25 | 25 (26.9) | 26 (27.7) |
| 25-<30 | 23 (24.7) | 38 (40.4) |
| ≥ 30 | 45 (48.4) | 30 (31.9) |
|
| ||
| Smoking, n (%) | ||
| Never | 78 (83.8) | 71 (75.5) |
| Once a month | - | 1 (1.1) |
| Twice a month | - | 2 (2.1) |
| Once a week | - | 2 (2.1) |
| Several times a week | 2 (2.2) | 2 (2.1) |
| Daily | 13 (14) | 13 (13.8) |
|
| ||
| Alcohol use,(%) | ||
| Never | 44 (47.3) | 31 (33) |
| Once a month | 11 (11.8) | 15 (16) |
| Twice a month | 11 (11.8) | 15 (16) |
| Once a week | 11 (11.8) | 17 (18.1) |
| Several times a week | 8 (8.6) | 11 (11.7) |
| Daily | 8 (8.6) | 3 (3.2) |
|
| ||
| Mean number of months since onset of | ||
| Amenorrhea | 115.72 | 120.31 |
| Menopausal Symptoms | 102.57 | 106.1 |
| Hot flashes | 89.53 | 91.23 |
|
| ||
| Hot Flash Severity at Baseline | ||
| Mean weekly hot flash frequency | 73.71 | 75.81 |
| Mean hot flash composite score | 22.62 | 23.03 |
|
| ||
| Mean Cognitive Expectancies | ||
| Intervention reducing frequency of hot flashes | 7.33 | 6.88 |
| Intervention reducing severity of hot flashes | 7.53 | 7.15 |
Some percentages may not sum to 100 due to rounding.
Change in Frequency of Hot Flashes
Reductions in subjective reported mean hot flash frequency from baseline to week 6 in the hypnosis intervention showed a mean reduction of 48.07 hot flashes (63.87%) from baseline as compared to a 6.95 reduction in control (9.24%) (Table 2). The mean difference in hot flash frequency between conditions was significant, (p<.001, 95% CI 38.84–47.85). Mean reductions continued into week 12, with follow-up reports of hot flash frequency showing a mean reduction of 55.82 hot flashes from baseline (74.16%), as compared to a 12.89 hot flash reduction (17.13%) for participants in the structured attention condition. The mean difference in hot flash frequency at week 12 follow-up was significant, (p<.001, 95% CI 36.15–49.67).
Table 2.
Change at weeks 6 and 12 in menopause-related symptoms and general impairment.
| Measure | Week | M (SD) | n | M (SD) | n | Change from Baseline | % Improvement | p | d (95% CI) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Structured Attention Control | Clinical Hypnosis | Structured Attention Control | Clinical Hypnosis | Structured Attention Control | Clinical Hypnosis | ||||||
| HF FREQUENCY | Baseline | 75.21 (3.11) | 94 | 75.26 (2.82) | 93 | ||||||
| 6 week | 68.26 (3.10) | 90 | 27.19 (2.48) | 84 | −6.95 | −48.07 | 9.24 | 63.87 | p<.001 | 1.25 (38.84–47.85) | |
| 12 week | 62.32 (3.43) | 87 | 19.44 (1.96) | 78 | −12.89 | −55.82 | 17.13 | 74.16 | p<.001 | 1.27 (36.15–49.67) | |
|
| |||||||||||
| HF-SCORE | Baseline | 22.94 (1.23) | 94 | 23.43 (1.02) | 93 | ||||||
| 6 week | 21.03 (1.15) | 90 | 6.71 (.79) | 84 | −1.91 | −16.72 | 8.32 | 71.36 | p<.001 | 1.23 (12.22–16.86) | |
| 12 week | 19.41 (1.36) | 87 | 4.61 (.56) | 78 | −3.53 | −18.83 | 15.38 | 80.32 | p<.001 | 1.21 (12.60–17.54) | |
|
| |||||||||||
| HF MONITOR | Baseline | 8.85 (.75) | 88 | 10.41 (1.00) | 84 | ||||||
| 6 week | 9.48 (.87) | 78 | 6.15 (.81) | 68 | 0.63a | −4.26 | 7.11‡ | 40.92 | p<.001 | .52 (2.30–5.91) | |
| 12 week | 7.97 (.70) | 70 | 4.49 (.59) | 49 | −0.88 | −5.92 | 9.94 | 56.86 | p<.001 | .67 (2.00–5.46) | |
|
| |||||||||||
| HFRDIS | Baseline | 5.75 (.24) | 94 | 5.87 (.23) | 93 | ||||||
| 6 week | 4.71 (.27) | 90 | 1.85 (.21) | 84 | −1.04 | −4.02 | 18.08 | 69.02 | p<.001 | 1.10 (2.37–3.47) | |
| 12 week | 4.43 (.28) | 87 | 1.05 (.20) | 78 | −1.32 | −4.82 | 22.96 | 82.11 | p<.001 | 1.22 (2.74–4.02) | |
|
| |||||||||||
| SLEEP (PSQI) | Baseline | 11.89 (.48) | 94 | 11.69 (.56) | 93 | ||||||
| 6 week | 10.85 (.51) | 90 | 6.10 (.47) | 84 | −1.04 | −5.59 | 8.75 | 43.49 | p<.001 | 1.04 (3.65–5.84) | |
| 12 week | 10.66 (.55) | 87 | 5.42 (.47) | 78 | −1.23 | −6.27 | 10.34 | 53.63 | p<.001 | 1.07 (3.69–5.93) | |
Abbreviations: HF, Hot Flash; HF-SCORE, Composite Score of Hot FlashFrequency X Hot Flash Severity; HF MONITOR, expert-rated hot flashes via skin conductance recording; HFRDIS, Hot Flash Related Daily Interference Scale, Mean score; HADS, Hospital Anxiety and Depression Scale -Anxiety subtotal; CESD, Center for Epidemiologic Studies -Depression Total Score; PSQI, Pittsburgh Sleep Quality Index -Global score; CI, 95% confidence interval. Effect size measures are Cohen’s d not adjusted for baseline and 95% confidence intervals for mean differences.
Indicates increased hot flashes
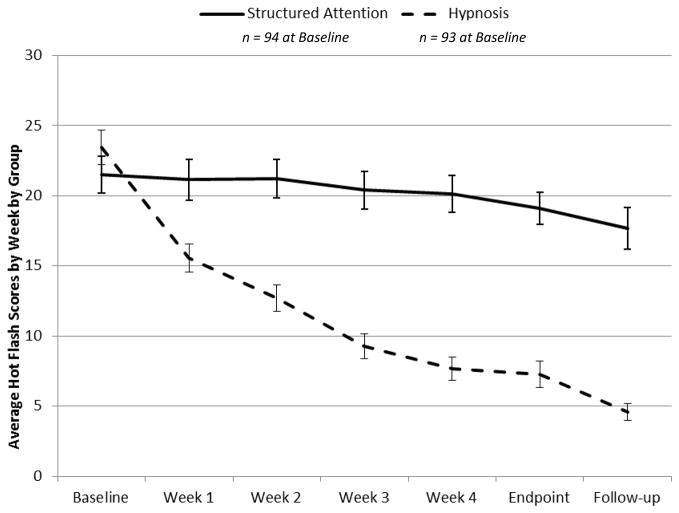
Change in Hot Flash Scores
Mean reductions in hot flash score, (a product of hot flash frequency by hot flash severity) were 16.72 hypnosis group (71.36%) at week 6 from baseline as compared to a 1.91 reduction in hot flash score (8.32% reduction) in control, (p<.001, 95% CI 38.84–47.85). (Figure 2). At 12 week follow-up, participants in the hypnosis intervention reported a continuing reduction of 18.83, (80.32%) from baseline as compared to a 3.53, (15.38%) in the control condition. Mean differences in hot flash scores at week 12 follow-up were significant between conditions (p<.001, 95% CI 12.60–17.54).
Figure 2.
Change in weekly composite hot flash scores.
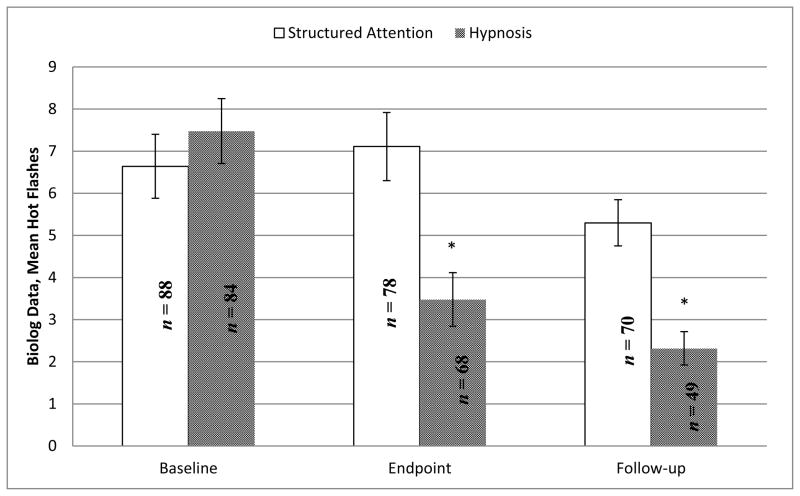
Physiologically Recorded Hot Flashes
There was a mean reduction in physiologically monitored hot flashes of 4.26 (40.92% reduction) at 6 weeks compared to baseline for the hypnosis intervention. Conversely, the structured attention control condition showed a mean increase of .63 (+7%) monitor hot flashes. The mean difference was significant (p<.001, 95% CI 2.30–5.91). At 12 week follow-up, the hypnosis intervention reported a further reduction of 5.92 (56.86%) physiologically monitored hot flashes from baseline, compared to a .88 (9.94%) decrease from baseline in the control condition. The mean difference between the two conditions in the number of physiologically monitored hot flashes was significant (Figure 3, p<.001, 95% CI 2.00–5.46).
Figure 3.
Physiologically verified hot flashes via skin conductance monitoring.
Hot Flash Related Daily Interference
Hot flash related daily interference was assessed using the HFRDIS. In the clinical hypnosis intervention there was a mean score reduction of 4.02 (69.02%) from baseline at six weeks, compared to a mean score reduction of 1.04 (18.08%) from baseline in the structured attention control condition. The mean difference between groups was significant (p<.001, 95% CI 2.37–3.47). At 12 weeks follow-up, the clinical hypnosis participants continued to improve, showing a mean score reduction of 4.82 (82.11%) from baseline as compared to the mean score reduction of 1.32 (22.96%) from baseline in the structured attention control. The mean difference between the participants in the clinical hypnosis condition and control was significant (Table 2, p<.001, 95% CI 2.74–4.02). This suggests participants who receive clinical hypnosis had substantially reduced levels of hot flash related daily interference after treatment, with levels continuing to fall at 12 week follow-up, as compared to the control condition, which showed modest improvement.
Sleep Quality
To evaluate the quality of participants’ sleep post-intervention, the global score from the PSQI was evaluated. In the clinical hypnosis intervention, participants reported a global score reduction of 5.59 (43.49%) at week 6 of the intervention, compared to a 1.04 (8.75%) reduction in the structured attention control condition. The difference between the global scores of the two groups was significant (Table 2, p<.001, 95% CI 3.65–5.84). At follow-up, the clinical hypnosis participants continued to improve, showing a reduction in global score of 6.27 (53.63%) from baseline as compared to a 1.23 (10.34%) reduction in the control condition. This suggests that for participants in the clinical hypnosis intervention, there was substantial improvement in the quality of sleep post-intervention, as compared to the structured attention control, which showed very modest improvement.
Adverse Events
Adverse events were assessed at each session by participant self-report. Adverse events for this study consisted solely of 25 participants reporting mild skin irritation from the skin conductance monitor electrode adhesive, requiring no medical intervention to resolve. There were no other reported adverse events, side effects or unintended effects from clinical hypnosis or the structured attention control.
Participant Satisfaction
Treatment satisfaction in this study was assessed via a rating scale of 0–10, with “0” indicating “Highly Dissatisfied” and “10” indicating “Highly Satisfied.” Generally, participants in both arms found the treatment pleasant. Treatment satisfaction was assessed at 12-week follow-up. The clinical hypnosis intervention group showed a high degree of treatment satisfaction (m=9.33, sd=0.99). Satisfaction with the structured-attention was also positive (m=7.09, sd=3.06). Participants in the clinical hypnosis intervention reported significantly greater levels of satisfaction (p<.001, 95% CI 7.79–8.59).
CONCLUSION
Improvements of at least a 50% reduction in hot flashes and daily interference are considered clinically significant.27,28 As hypothesized, clinical hypnosis significantly reduced hot flashes in post-menopausal women, relative to structured attention control. At 12-week follow up, reductions occurred in hot flash frequency (74.16% vs. 17.13%, p<.001), and in hot flash score (80.32% vs. 15.38%, respectively, p<.001). Also, as hypothesized, significant reductions were found between clinical hypnosis participants and structured attention control in indices of hot flash daily interference scores, (82.11% vs. 22.96%, p<.001) and sleep quality as indicated by global scores on the PSQI, (53.63% vs. 10.34%, p<.001).
Physiologically recorded hot flashes also showed significant reductions in the clinical hypnosis participants compared to control. To our knowledge, this is the first published study to demonstrate a significant reduction in physiologically measured hot flashes in response to a mind-body intervention. At 12 week follow-up, the hypnosis intervention resulted in a 56.86% reduction in physiologically monitored hot flashes from baseline, compared to a 9.94% decrease from baseline in the control condition further adding to evidence of the intervention’s effectiveness.
It has been reported that there is a substantial placebo effect in hot flash treatments.47 Why the placebo effect in hot flash treatment is so substantial is unknown, however supportive care or the act of maintaining a diary may be empowering to participants and thus provide some relief.48 Though the results of the clinical hypnosis intervention in this trial exceeded the effect of the supportive care and diary monitoring provided in the structured attention control condition, the study has several limitations.
The mechanism of action in clinical hypnosis to reduce hot flashes is unknown. As hot flashes involve increases in heart rate, flushing, and sweating, it has been posited that hot flashes are a result of autonomic dysfunction. 49 A theory has been proposed suggesting that hot flashes may be a result of a decrease in parasympathetic tone. 50 Notably, a link between hot flashes and cardiovascular risk has been reported, and this theory suggests that the cause may be a decrease in relative parasympathetic influence, as indicated by reductions in high frequencies of heart rate variability.51–54 A possible mechanism of action for clinical hypnosis could be that regular practice of clinical hypnosis improves parasympathetic tone resulting in reduced hot flash symptoms. This is an empirical question that should be investigated through comparative heart-rate variability analyses in subsequent studies.
A limitation of this study also is that the results may not generalize to all participants with hot flashes, as some hot flashes occur at times other than during the climacteric, (e.g. pregnancy; perimenopause). Due to the nature of mind-body clinical trials, self-selection bias may be a confound to the results of this study. Participants who are negatively predisposed to mind-body therapy, unable to make the substantial time commitments required of a clinical trial of this nature, or unwilling to provide initial hot flash diaries to determine eligibility, may have influenced results. This may suggest that these results might be best interpreted as particularly relevant for women who are more open to mind-body therapy. Also, it should be noted that the sample in this study was largely White, and there is evidence to suggest ethnic and cultural differences may contribute to perceived interference and in reporting hot flash of hot flash frequency and severity among post-menopausal women.55
Treatment satisfaction in this study was assessed via a single question on a rating scale of 0–10. The mean score of 9.33 for the hypnosis intervention reflects a high level of satisfaction and suggest that the intention is likely to be well received in a clinical setting. The mean satisfaction score of 7.09 in the control group was expected to be lower due to the disappointment after a minimal decrease in hot flashes.
The strengths of this study include its’ sample size, the active control condition, the absence of negative side effects, and the inclusion of physiologic measures to diary reports of hot flashes. Future studies should investigate exactly how clinical hypnosis reduces hot flashes and explore efficient methods of dissemination. Safe and effective alternate therapies are needed 56 and clinical hypnosis reduced hot flashes in this study of post-menopausal women, though the mechanism of action is not yet understood.
Acknowledgments
Funding/Support: The project described was supported by Award Number U01 AT004634-05 from the National Center for Complementary and Alternative Medicine. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Complementary and Alternative Medicine or the National Institutes of Health.
Footnotes
Conflict of Interest: Nil.
References
- 1.Rada G, Capurro D, Pantoja T, Corbalan J, Moreno G, Letelier LM, Vera C. Non-hormonal interventions for hot flushes in women with a history of breast cancer. Cochrane Database of Systematic Reviews. 2010;(9) doi: 10.1002/14651858.CD004923.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Nelson HD, Vesco KK, Haney E, et al. Non-hormonal therapies for menopausal hot flashes: Systematic review and meta-analysis. Journal of the American Medical Association. 2006;295 (17):2057–2071. doi: 10.1001/jama.295.17.2057. [DOI] [PubMed] [Google Scholar]
- 3.Nelson HD. Commonly used types of postmenopausal estrogen for the treatment of hot flashes: Scientific review. Journal of the American Medical Association. 2004;291 (13):1610–1620. doi: 10.1001/jama.291.13.1610. [DOI] [PubMed] [Google Scholar]
- 4.Sterns V, Beebe KL, Iyengar M, Dube E. Paroxetine controlled release in the treatment of menopausal hot flashes. Journal of the American Medical Association. 2003;289(21):2827–2834. doi: 10.1001/jama.289.21.2827. [DOI] [PubMed] [Google Scholar]
- 5.Kronenberg F. Hot flashes: Epidemiology and physiology. Annuals of the New York Academy of Science. 1990;592(1):52–86. doi: 10.1111/j.1749-6632.1990.tb30316.x. [DOI] [PubMed] [Google Scholar]
- 6.Berendsen H. The role of serotonin in hot flushes. Maturitas. 2000;36(3):155–164. doi: 10.1016/S0378-5122(00)00151-1. [DOI] [PubMed] [Google Scholar]
- 7.Carpenter JS, Andrykowski MA, Freedman RR, Munn R. Feasibility and psychometrics of an ambulatory hot flash monitoring device. Menopause. 1999;6(3):209–215. doi: 10.1097/00042192-199906030-00006. [DOI] [PubMed] [Google Scholar]
- 8.Casper RF, Yen SS. Neuroendocrinology of menopausal flushes: A hypothesis of flush mechanism. Clinical Endocrinology. 1985;22(3):293–312. doi: 10.1111/j.1365-2265.1985.tbo3243.x. [DOI] [PubMed] [Google Scholar]
- 9.Deecher DC, Dorries K. Understanding the pathophysiology of vasomotor symptoms (hot flushes and night sweats) that occur in perimenopause, menopause, and postmenopause life stages. Archives of Women’s Mental Health. 2007;10(6):247–257. doi: 10.1007/s00737-007-0209-5. [DOI] [PubMed] [Google Scholar]
- 10.Freedman RR. Laboratory and ambulatory monitoring of menopausal hot flashes. Psychophysiology. 1989;26(5):573–579. doi: 10.1111/j.1469-8986.1989.tb00712.x. [DOI] [PubMed] [Google Scholar]
- 11.Freedman RR, Norton D, Woodward S, Cornélissen G. Core body temperature and circadian rhythm of hot flashes in menopausal women. Journal of Clinical Endocrinology and Metabolism. 1995;80(8):2354–2358. doi: 10.1210/jc.80.8.2354. [DOI] [PubMed] [Google Scholar]
- 12.Freedman RR. Biochemical, metabolic, and vascular mechanisms in menopausal hot flashes. Fertility and Sterility. 1998;70(2):332–337. doi: 10.1016/50015-0282(98)00137-x. [DOI] [PubMed] [Google Scholar]
- 13.Freedman RR, Krell W. Reduced thermoregulatory null zone in postmenopausal women with hot flashes. American Journal of Obstetrics and Gynecology. 1999;181(1):66–70. doi: 10.1016/S0002-9378(99)70437-0. [DOI] [PubMed] [Google Scholar]
- 14.Freedman RR. Physiology of hot flashes. American Journal of Human Biology. 2001;13(4):453–464. doi: 10.1002/ajhb.1077. [DOI] [PubMed] [Google Scholar]
- 15.Freedman RR. Hot flashes: Behavioral treatments, mechanisms, and relation to sleep. The American Journal of Medicine. 2005a;118(12b):1245–1305. doi: 10.1016/j.amjmed.2005.09.046. [DOI] [PubMed] [Google Scholar]
- 16.Freedman RR. It’s all in your head [Editorial] Menopause. 2005b;12(5):483. doi: 10.1097/01.gme.0000172272.10219.90. [DOI] [PubMed] [Google Scholar]
- 17.Miller HG, Maria R. Measuring hot flashes: Summary of a National Institutes of Health workshop. Mayo Clinic Proceedings. 2004;79(6):777–781. doi: 10.4065/79.6.777. [DOI] [PubMed] [Google Scholar]
- 18.Shanafelt TD, Barton DL, Adjei AA, Loprinzi CL. Pathophysiology and treatment of hot flashes. Mayo Clinic Proceedings. 2002;77(11):1207–1218. doi: 10.4065/77.11.1207. [DOI] [PubMed] [Google Scholar]
- 19.Dennerstein L, Dudley EC, Hopper JL, Guthrie JR, Burger HG. A prospective population based study of menopausal symptoms. Obstetrics & Gynecology. 2000;96(3):351–358. doi: 10.1016/s0029-7844(00)00930-3. [DOI] [PubMed] [Google Scholar]
- 20.Politi MC, Schleinitz MD, Col NF. Revisiting the duration of vasomotor symptoms of menopause: a meta-analysis. Journal General Internal Medicine. 2007;23(9):1507–1513. doi: 10.1007/S11606-008-0655-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elkins G, Marcus J, Sterns V, Perfect M, Rajab MH, Ruud C, et al. Randomized trial of a hypnosis intervention for the treatment of hot flashes among breast cancer survivors. Journal of Clinical Oncology. 2008;26(31):5022–5026. doi: 10.1200/JCO.2008.16.6389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sterns V, Isaacs C, Rowland J, et al. A pilot trial assessing the efficacy of paroxetine hydrochloride (Paxil) in controlling hot flashes in breast cancer survivors. Annals of Oncology. 2000;11(21):17–22. doi: 10.1023/a:1008382706068. [DOI] [PubMed] [Google Scholar]
- 23.Barton DL, La Vasseur B, Loprinzi C, Novotny P, Wilwerding MB, et al. Venlafaxine for the control of hot flashes: Results of a longitudinal continuation study. Oncology Nursing Forum. 2002;29 (1):33–40. doi: 10.1188/02.ONF.33-40. [DOI] [PubMed] [Google Scholar]
- 24.Loprinzi CL, Sloan JA, Perez EA, et al. Phase III evaluation of fluoxetine for the treatment of hot flashes. Journal of Clinical Oncology. 2002;20:1578–1583. doi: 10.1200/JCO.2002.20.6.1578. [DOI] [PubMed] [Google Scholar]
- 25.Loprinzi C, Kugler J, Sloan J, Mailliard J, LaVasseur B, Barton D, Novotony P, Dakhill S, Rodger K, Rummans T, Christensen B. Venlafaxine in management of hot flashes in survivors of breast cancer: a randomized trial. Lancet. 2000;356(9247):2059–2063. doi: 10.1016/S0140-6736(00)03403-6. [DOI] [PubMed] [Google Scholar]
- 26.Food and Drug Administration, U.S. Department of Health and Human Services. [Accessed April 2, 2012];Guidance for industry: Estrogen and estrogen/progestin drug products to treat vasomotor symptoms and vulvar and vaginal atrophy symptoms-recommendations for clinical evaluation. http://www.fda.gov/downloads/Drugs/DrugSafety/InformationbyDrugClass/UCM135338.pdf.
- 27.Sloan JA, Loprinzi CL, Novotny PJ, Barton BL, Lavasseur BI, Windschitl H. Methodologic lessons learned from hot flash studies. Journal of Clinical Oncology. 2001;19(23):4280–4290. doi: 10.1200/JCO.2001.19.23.4280. [DOI] [PubMed] [Google Scholar]
- 28.Loprinzi CL, Michalak JC, Quell SK, et al. Megestrol Acetate for the Prevention of Hot Flashes. New England Journal of Medicine. 1994;331:347–352. doi: 10.1056/NEJM199408113310602. [DOI] [PubMed] [Google Scholar]
- 29.Elkins GR, Hammond DC. Standards of training in clinical hypnosis: Preparing professionals for the 21st century. American Journal of Clinical Hypnosis. 1998;41(1):55–64. doi: 10.1080/00029157.1998.10404185. [DOI] [PubMed] [Google Scholar]
- 30.Elkins GR, Handel DL. Clinical hypnosis: An essential tool kit for the family practice. Behavioral Medicine in Family Practice: Clinics in Family Practice. 2001;3(1):113–126. doi: 10.1186/1472-6882-11-92. [DOI] [Google Scholar]
- 31.Evans FJ. The domain of hypnosis: A multifactorial model. American Journal of Clinical Hypnosis. 2000;43(1):1–16. doi: 10.1080/00029157.2000.10404252. [DOI] [PubMed] [Google Scholar]
- 32.Hammond DC, Elkins GR. Standards of Training in Clinical Hypnosis. Chicago, IL: American Society of Clinical Hypnosis Press; 1994. [DOI] [PubMed] [Google Scholar]
- 33.Araoz DL. Use of hypnotic techniques with oncology patients. Journal of Psycho-Social Oncology. 1983;1(4):47–54. doi: 10.1300/J. [DOI] [Google Scholar]
- 34.Bridge LR, Benson P, Pietroni PC, Priest RG. Relaxation and imagery in the treatment of breast cancer. British Medical Journal. 1988;297(6657):1169–1172. doi: 10.1136/bmj.297.6657.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burish TG, Snyder SL, Jenkins RA. Preparing patients for cancer chemotherapy: Effect of coping preparation and relaxation interventions. Journal of Consulting and Clinical Psychology. 1991;59 (4):518–525. doi: 10.1037/0022-006x.59.4.518. [DOI] [PubMed] [Google Scholar]
- 36.Decker T, Cline-Elsen J, Gallagher M. Relaxation therapy as an adjunct in radiation oncology. Journal of Clinical Psychology. 1992;48(3):388–393. doi: 10.1002/1097-4679(199205)48:3<388::AID-JCLP2270480318>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 37.Elkins GR, Cheung A, Marcus J, Palamara L, Rajab H. Hypnosis to reduce pain in cancer survivors with advanced disease: A prospective study. Journal of Cancer Integrative Medicine. 2004;2:167–172. [Google Scholar]
- 38.Jensen M, Patterson D. Control conditions in hypnotic-analgesia clinical trials: Challenges and recommendations. The International Journal of Clinical and Experimental Hypnosis. 2005;53(2):170–197. doi: 10.1080/00207140590927536. [DOI] [PubMed] [Google Scholar]
- 39.UFI. Model 3991 SCL. UFI; Morro Bay, CA: [Accessed April 2, 2012]. http://www.UFIservingscience.com/biologs.html. [Google Scholar]
- 40.Lykken D, Venables P. Direct measurement of skin conductance: A proposal for standardization. Psychophysiology. 1971;8(5):656–672. doi: 10.1111/j.1469-8986.1971.tb00501.x. [DOI] [PubMed] [Google Scholar]
- 41.BIOPAC Systems, Inc. EL-507 Disposable EDA Electrode. Goletta, CA: [Accessed February 12, 2012]. http://www.biopac.com/disposable-electrodermal-electrode-100. [Google Scholar]
- 42.Carpenter JS. The hot flash related daily interference scale: A tool for assessing the impact of hot flashes on quality of life following breast cancer. Journal of Pain and Symptom Management. 2001;22 (6):979–989. doi: 10.1016/S0885-3924(01)00353-0. [DOI] [PubMed] [Google Scholar]
- 43.Buysse D, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new measurement for psychiatric practice. Journal of Psychiatric Research. 1989;28 (2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 44.Erdfelder E, Faul F, Buchner A. GPOWER: A general power analysis program. Behavior Research Methods, Instruments, & Computers. 1996;28:1–11. [Google Scholar]
- 45.Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- 46.Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7 (2):147–177. doi: 10.1037//1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- 47.MacLennan AH, Broadbent JL, Lester S, Moore V. Oral oestrogen and combined oestrogen/progestogen therapy versus placebo for hot flushes. Cochrane Database of Systematic Reviews. 2004;(4) doi: 10.1002/14651858.CD002978.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Freeman EW, Guthrie KA, Caan B. Efficacy of escitalopram for hot flashes in healthy menopausal women: A randomized controlled trial. Journal of the American Medical Association. 2011;305(3):267–274. doi: 10.1001/jama.2010.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gorodeski EZ. Autonomic dysfunction: A common mechanism for heart failure and hot flashes? Menopause. 2012;19(4):382–383. doi: 10.1097/gme.0b013e31824c7a3b. [DOI] [PubMed] [Google Scholar]
- 50.Thurston CR, Christie CI, Matthews AK. Hot flash and cardiac vagal control: A link to cardiovascular risk? Menopause. 2010;17(3):456–461. doi: 10.1097/gme.0b013e3181c7dea7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gianaros PJ, May J, Siegle G, Jennings J. Is there a functional neural correlate of individual differences in cardiovascular reactivity? Psychosomatic Medicine. 2005;67:31–39. doi: 10.1097/01.psy.0000151487.05506.dc. [DOI] [PubMed] [Google Scholar]
- 52.Liao D, Cai J, Rosamond W, et al. Cardiac autonomic function and incident coronary heart disease: A population based case cohort study: the ARIC study. American Journal of Epidemiology. 1997;145:696–706. doi: 10.1093/aje/145.8.696. [DOI] [PubMed] [Google Scholar]
- 53.Thayer JF, Lane RD. The role of vagal function in the risk of cardiovasular disease and mortality. Biological Psychology. 2007;74(2):224–242. doi: 10.1016/j.biopsycho.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 54.Thurston RC, Christie IC, Matthews KA. Hot flashes and cardiac vagal control during women’s daily lives. Menopause. 2012;19(4):406–412. doi: 10.1097/gme.0b013e3182337166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Freeman EW, Sherif K. Prevalence of hot flashes and night sweats around the world: A systematic review. Climacteric. 2007;10 (3):197–214. doi: 10.1080/13697130601181486. [DOI] [PubMed] [Google Scholar]
- 56.Archer DF, Sturdee DW, Baber R, et al. Menopausal hot flashes and night sweats: Where are we now? Climacteric. 2011;14(5):515–528. doi: 10.3109/13697137.2011.608596. [DOI] [PubMed] [Google Scholar]