Fournier's gangrene (FG) is an acute necrotizing fasciitis that involves the skin and subcutaneous tissue on the scrotum, perineum, and abdominal wall [1]. It is a potentially fatal disease, with a reported mortality rate between 3% and 67% [2]. Broad-spectrum antibiotics, aggressive fluid therapy, and early surgical debridement are essential for the management of FG [3]. After primary treatment, FG may produce tissue defects of various sizes that need reconstructive procedures. We experienced a case of extensive defects involving the bilateral groin, pubic area, and scrotum after FG, for which we performed single-stage reconstruction using bilateral pedicled anterolateral thigh (ALT) flaps and gracilis myocutaneous flaps.
A 55-year-old male patient with a body mass index of 19.1 visited our hospital for treatment of inguinal and scrotal necrosis which developed within one day after the onset of scrotal edema and pain. The patient had a history of diabetes and hypertension. Seven days before visiting our hospital, he was diagnosed with a perianal abscess at another hospital. Initially, the patient had necrosis around the scrotum, anus, and groin area, which were accompanied by a foul odor and pus discharge. We immediately administered broad-spectrum antibiotics and performed aggressive fluid supplement therapy. On the second day, surgical debridement was performed. However, the area of the skin necrosis extended to the lower abdomen, bilateral flank, and lower costal margin. To prevent wound contamination from urine, a urethral catheter was inserted. However, the patient was unable to undergo a diverting colostomy because of the widespread presence of abdominal defects and inflammation. We continuously treated him with debridement and wet dressings, and to promote granulation tissue growth, we treated him with negative pressure wound therapy. Due to the repeated debridement and wound dressings, his wound condition improved with healthy granulation tissue formation (Fig. 1). On hospital day 67, the bilateral defects in the groin with an exposed iliac crest were reconstructed with bilateral pedicled ALT flaps that were sized at 23×8 cm and 27×11 cm. We then placed the flaps at each side of the groin through the subcutaneous tunnel. The donor sites were closed with a split-thickness skin graft (STSG). The defects of the pubic area and the scrotum were reconstructed with bilateral gracilis myocutaneous flaps, both of which were sized at 19×6 cm. This was followed by the primary closure of all the donor sites. In the abdominal and penile defects, we performed an STSG (Fig. 2). The STSGs were stapled into place and covered with compression dressings. On hospital day 92, minor wound revision was performed three times. During the 9-month postoperative follow-up, the patient had achieved normal gait patterns and urination (Fig. 3), but the patient had not recovered sexual functions.
Fig. 1.
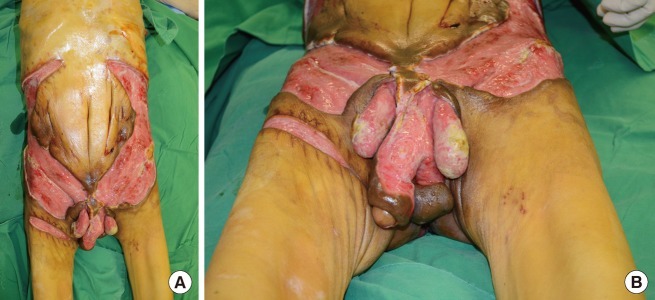
A 55-year-old man with extensive defects involving the bilateral groins, flanks, pubic area, penis, and scrotum with an exposed iliac crest and testes. (A) Gross appearance. (B) Close-up appearance.
Fig. 2.
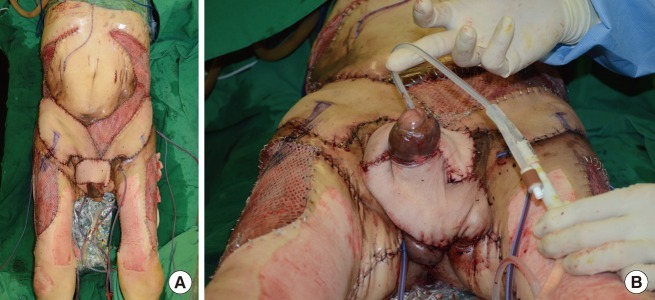
Immediate postoperative results. (A) Gross appearance. (B) Close-up appearance.
Fig. 3.
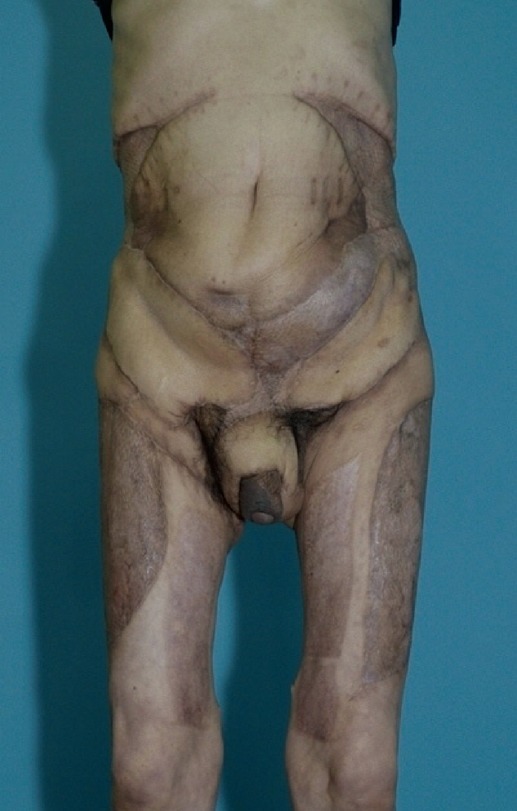
Postoperative view obtained 10 months after surgery.
FG is thought to arise from the combination of a polymicrobial infection and microthrombosis, resulting from small subcutaneous arterioles. The organism probably passes through the Buck's fascia to spread along the planes of the dartos fascia of the scrotum and penis, Colles' fascia of the perineum, and Scarpa's fascia of the abdominal wall [4]. If FG is not recognized and treated early in its course, it may produce extensive defects.
Because of the widespread breakdown of skin barriers in extensive FG defects, there are high risks of local and systemic infections. In addition, the physical and psychological stresses caused by extensive FG defects require a long time for complete wound bed preparation. Therefore, a single-stage reconstruction is recommended for extensive FG defects.
There are various solutions for covering extensive FG defects such as skin grafts and flaps [3,5]. However, skin grafts for extensive FG defects may be unsatisfactory because of 1) frequent urinary and fecal contamination causing maceration and breakdown, and 2) the exposure of bone and vital organs such as the iliac crest and testes.
Reconstruction using the free flap in extensive FG defects is restricted because of the difficulty of finding reliable recipient vessels, given the inherent potential vascular complications in the wound bed and adjacent tissues, and because the operation time can be excessively prolonged during microsurgery.
The pedicled ALT flap and the gracilis myocutaneous flap can be useful choices for reconstruction of extensive FG defects involving the groin, pubic area, and scrotum, where the bone and vital organs are exposed.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Yaghan RJ, Al-Jaberi TM, Bani-Hani I. Fournier's gangrene: changing face of the disease. Dis Colon Rectum. 2000;43:1300–1308. doi: 10.1007/BF02237442. [DOI] [PubMed] [Google Scholar]
- 2.Corman JM, Moody JA, Aronson WJ. Fournier's gangrene in a modern surgical setting: improved survival with aggressive management. BJU Int. 1999;84:85–88. doi: 10.1046/j.1464-410x.1999.00140.x. [DOI] [PubMed] [Google Scholar]
- 3.Ferreira PC, Reis JC, Amarante JM, et al. Fournier's gangrene: a review of 43 reconstructive cases. Plast Reconstr Surg. 2007;119:175–184. doi: 10.1097/01.prs.0000244925.80290.57. [DOI] [PubMed] [Google Scholar]
- 4.Schaeffer AJ. Infections of the urinary tract. In: Campbell MF, Retik AB, Vaughan ED, editors. Campbell's urology. 7th ed. Philadelphia: W.B. Saunders Co.; 1998. pp. 533–614. [Google Scholar]
- 5.Chen SY, Fu JP, Chen TM, et al. Reconstruction of scrotal and perineal defects in Fournier's gangrene. J Plast Reconstr Aesthet Surg. 2011;64:528–534. doi: 10.1016/j.bjps.2010.07.018. [DOI] [PubMed] [Google Scholar]


