Abstract
Burkholderia pseudomallei is the causative agent of melioidosis. Treatment of melioidosis is suboptimal and developing improved melioidosis therapies requires animal models. In this report, we exposed male BALB/c mice to various amounts of aerosolized B. pseudomallei 1026b to determine lethality. After establishing a median lethal dose (LD50) of 2,772 colony forming units (cfu)/animal, we tested the ability of doxycycline administered 6 hours after exposure to a uniformly lethal dose of ~20 LD50 to prevent death and eliminate bacteria from the lung and spleens. Tissue bacterial burdens were examined by PCR analysis. We found that 100% of mice treated with doxycycline survived and B. pseudomallei DNA was not amplified from the lungs or spleens of most surviving mice. We conclude the BALB/c mouse is a useful model of melioidosis. Furthermore, the data generated in this mouse model indicate that doxycycline is likely to be effective in post-exposure prophylaxis of melioidosis.
Burkholderia pseudomallei is a Gram-negative, motile, non-spore-forming, aerobic bacteria found in contaminated water, soil, and on market produce. It is the causative agent of melioidosis, an important infectious disease with highly endemic regions in southeast Asia and northern Australia and expanding known global distribution1,2. The primary reservoir of B. pseudomallei is the soil and water. Transmission from the environment to humans most commonly occurs via open wounds and skin abrasions as well as via inhalation during severe weather and can also occur via ingestion although this occurs more in animals than humans2,3,4. Melioidosis can manifest a broad range of symptoms, with both acute and chronic manifestations. Acute disease can be severe, including fever, weight loss, pneumonia, and death5. In addition to acute disease, asymptomatic chronic infections can exist for up to 62 years6. Although there is no documented history of the use of B. pseudomallei as a biological weapon, Ken Alibek claimed the Soviet Union weaponized B. pseudomallei7. Because of heightened concerns about the use of B. pseudomallei as a biological weapon, ongoing research is aimed at developing novel and safe anti-bacterial therapeutics.
B. pseudomallei is naturally resistant to a diversity of antibiotics, including penicillin, ampicillin, first and second generation cephalosporins, gentamicin, tobramycin, streptomycin, and polymixin2,3,8. Treatment involves an intensive intravenous infusion phase using either ceftazidime, meropenem, or imipenem for 10 to 14 days followed by a lengthy eradication phase of oral teimethoprim-sulfamethoxazole for up to 6 months2,3,9,10. Given the multidrug resistance of B. pseudomallei and lengthy treatment for melioidosis, there is a need to develop improved therapies. This requires well-characterized animal models of melioidosis with defined endpoints relevant to human disease for preclinical testing of new therapeutics and for screening of potential vaccine candidates. Additionally, given the low incidence of naturally acquired melioidosis in most parts of the world, the testing of new candidate vaccines and therapeutics may require demonstration of efficacy for licensure via the FDA Animal Rule (21 CFR 601.90–95). Therefore, the overall goal of our research is aimed at developing animal models to identify and evaluate treatments for melioidosis.
Numerous mouse models of B. pseudomallei infections have been developed, although most of these models used intranasal, intraperitoneal, or intravenous routes of infection, with LD50 ranging from < 5 to 1.5 × 104 cfu/animal11,12,13,14,15,16,17. Differences in LD50 values are attributable to a number of factors include mouse strain, B. pseudomallei strain, and route of infection. Given the likelihood a biological weapon will utilize aerosol dissemination18 and the route of B. pseudomallei infection impacts disease manifestation16, an aerosol model has benefits not found in parenteral challenges. There have been recent efforts to develop mouse models of aerosolized B. pseudomallei infections19,20,21,22. We expand the nose-only exposure of male BALB/c mice to aerosolized B. pseudomallei, including the efficacy of post-exposure antibiotic administration. In particular, we examined doxycycline as it was used in older treatment protocols23, we have our experience with administering doxycycline treatments in mice24, and the vast majority of B. pseudomallei strains are susceptible to this antibiotic25,26,27,28. We report on the mouse model of inhalational melioidosis and the efficacy of post-exposure doxycycline administration in preventing the development of melioidosis.
Results
Lethality of the aerosol exposure
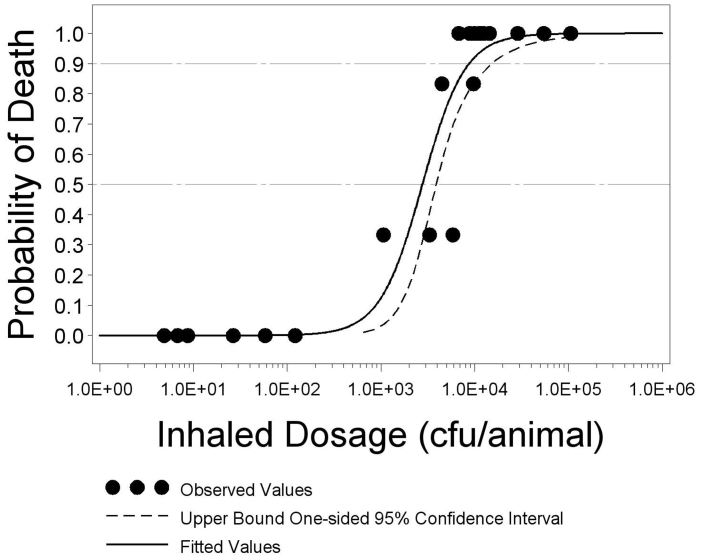
In order to have the greatest confidence in the LD50 estimate, we desired the maximum number of mice to be exposed to a dose near to the actual LD50. To best target the aerosol dose, mice were divided into three phases, with the targeted doses for phases II and III being determined by the cumulative lethality results from the previous phase(s). The targeted and actual aerosol doses are shown in Table 1. The average mass median aerodynamic diameter (MMAD) of the aerosol particles generated for phases I, II, and III was 2.34 μm, 2.03 μm, and 1.80 μm, respectively. The MMAD of the aerosol particles generated for this study are consistent with lower respiratory tract deposition. There were two animals (one in group I-E and one in group II-D) that were found dead immediately after removal from the aerosol exposure system and were excluded from all analyses. Analysis of these data found a statistically significant dose-response relationship (p = 0.0001) with higher dosages of the agent resulting in a higher probability of death. Figure 1 depicts the dose lethality curve. The LD50 was estimated at 2,772 cfu/animal with an upper 95 percent confidence bound of 3,888 cfu/animal. The LD90 was estimated to be 8,728 cfu/animal with an upper 95 percent confidence bound of 15,159 cfu/animal.
Table 1. Lethality results.
| Phase | Dosage Group | No. of Animals | Target Challenge Dosage (cfu/animal) | Calculated Inhaled Dosage (cfu/animal) | No. of Animals Died |
|---|---|---|---|---|---|
| I | I-A | 6 | 5 | 7 | 0 |
| I-B | 6 | 10 | 9 | 0 | |
| I-C | 6 | 25 | 5 | 0 | |
| I-D | 6 | 50 | 58 | 0 | |
| I-E | 6 | 100 | 27 | 0 | |
| I-F | 5 | 500 | 122 | 0 | |
| I-G | 6 | 1,000 | 1,068 | 2 | |
| I-H | 6 | 5,000 | 5,854 | 2 | |
| II | II-A | 6 | 7,000 | 8,910 | 6 |
| II-B | 6 | 8,000 | 12,408 | 6 | |
| II-C | 6 | 10,000 | 9,966 | 6 | |
| II-D | 5 | 25,000 | 28,896 | 5 | |
| II-E | 6 | 50,000 | 54,824 | 6 | |
| II-F | 6 | 100,000 | 106,260 | 6 | |
| III | III-A | 6 | 2,000 | 3,309 | 2 |
| III-B | 6 | 3,000 | 4,488 | 5 | |
| III-C | 6 | 4,000 | 6,798 | 6 | |
| III-D | 6 | 5,000 | 9,725 | 5 | |
| III-E | 6 | 7,000 | 11,286 | 6 | |
| III-F | 6 | 8,000 | 14,424 | 6 |
Figure 1. Estimated logistic regression curve and 95 percent confidence interval with points showing the proportion of animals that died.
The probability of death of each group of male BALB/c mice is plotted against the inhaled dosage of B. pseudomallei 1026b in cfu. The percentage of animals alive 14 days after exposure to aerosolized B. pseudomallei 1026b in each dose group is depicted as ·. A logistic dose-response model was fit to the data and the solid black curve represents the results of this model, such that any B. pseudomallei 1026b dose has a corresponding probability of death. The dashed curve represents the upper 95% confidence bound of the logistic dose-response model. The horizontal dashed lines at 0.5 and 0.9 probability of death represent the median lethality and 90th percentile of lethality, respectively. The points at which the solid black curve intersects the dashed horizontal lines represent the LD50 and LD90.
Survival of mice with or without doxycycline
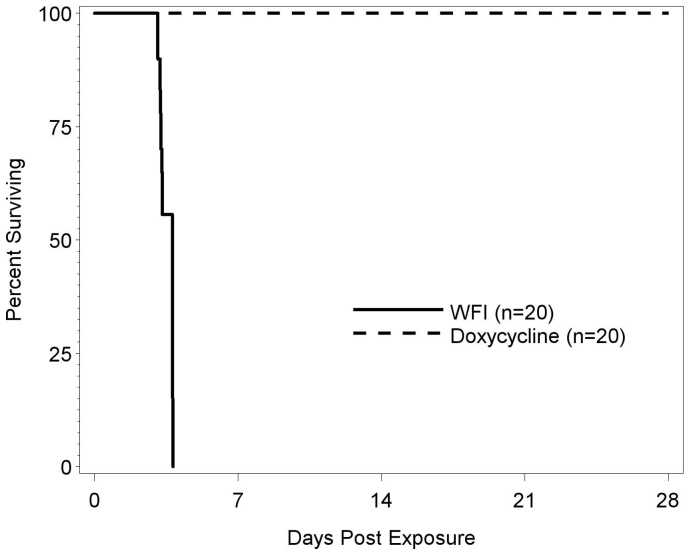
Having established the LD50, we next wanted to examine the efficacy of doxycycline in preventing death following exposure to aerosolized B. pseudomallei 1026b. Mice inhaled an estimated 1.17 − 1.30 × 105 cfu aerosolized B. pseudomallei 1026b. One group of mice was treated with doxycycline twice daily for 14 days beginning 6 hours after aerosol exposure. The control group received sterile water for injection on the same schedule. Figure 2 plots the Kaplan-Meier curves for the time-to-death data. All doxycycline treated mice survived 28 days after exposure to aerosolized B. pseudomallei 1026, while all water treated mice died 3–4 days after exposure. Fisher's exact comparing the survival rate between the two groups was performed and the differences in survival were significant (p < 0.0001).
Figure 2. Survival of mice with or without doxycycline treatment following exposure to B. pseudomallei 1026b.
Two groups of twenty male BALB/c mice were exposed to aerosolized B. pseudomallei 1026b via a nose-only exposure system. The animals were exposed to an inhaled dose range of 1.17 − 1.30 × 105 cfu over a period of 10 minutes. Six hours after exposure, one group of mice was treated with doxycycline (dashed line) and the control group was treated with WFI (solid line). The 40 mg/kg doxycycline was administered twice daily for 14 days. The percentage of mice in each group surviving on each day following exposure to B. pseudomallei 1026b is shown.
Impact of doxycycline on B. pseudomallei in tissues
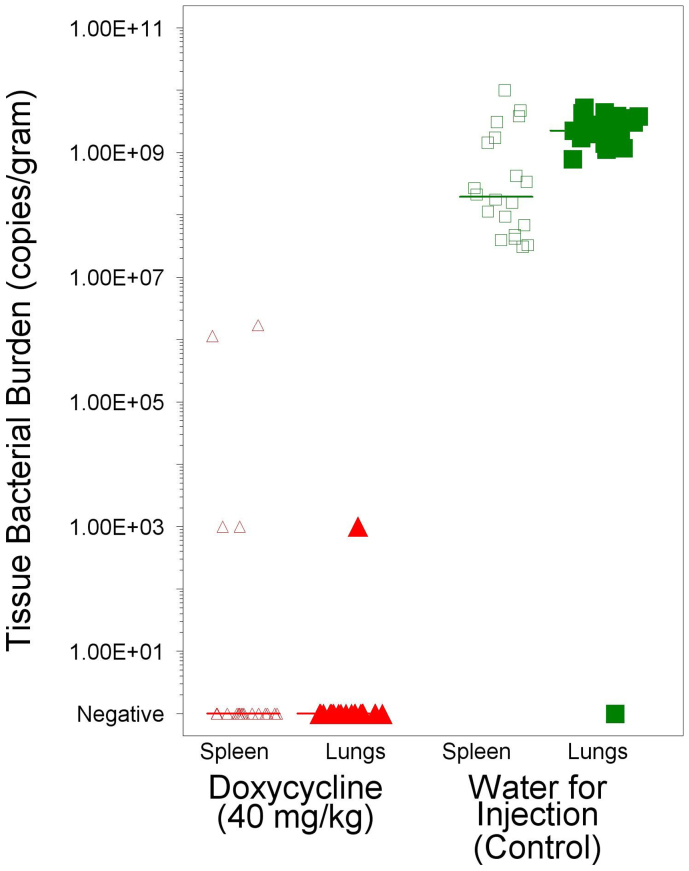
As B. pseudomallei infections can manifest as either a lethal acute infection or a sub-lethal chronic infection, we wanted to assess the number of bacteria present in the lungs and spleens of animals at the time of death or at euthanasia 28 days after aerosol exposure. As shown in Figure 3, the specimens from mice found dead in the WFI treatment group had a median 1.95 × 108 copies of rpoB/gram of spleen and 2.25 × 109 copies of rpoB/gram of lung. In comparison, 16 of 20 spleen specimens and 19 of 20 lung specimens had no detectable copies of rpoB. These results indicate that doxycycline greatly reduced B. pseudomallei tissue burdens and likely eradicated infection in 80% of mice.
Figure 3. Tissue bacterial burden in the lungs and spleen.
The copies of B. pseudomallei gene/g of tissue was determined for the spleen and lungs from each animal at the time of death or when euthanatized 28 days after exposure to B. pseudomallei. Copies/g were determined by real-time PCR and each symbol represents the results for an individual tissue. Triangle represent doxycycline treated mice and squares represent WFI treated controls. Open symbols represent spleen tissue results and filled symbols represent lung tissue results. The bars represent the mean copies/g in a given tissue for a given treatment group. Doxycycline treatment significantly reduced the copies/g in both the spleen and lungs (p < 0.0001).
Discussion
Similar to previous studies, we show that B. pseudomallei causes a lethal disease in BALB/c mice and that doxycycline can be used as a treatment. Doxycycline treatment resulted in no detectable bacteria in 19 of 20 lungs and 16 of 20 spleens. In previous reports, whole body exposure to aerosolized B. pseudomallei 1026b resulted in an LD50 1 × 101 cfu/mouse, well below 2.8 × 103 we found for nose-only aerosol in male BALB/c mice. While this difference may be attributable to the differences in the B. pseudomallei aerosolized, differences in route of exposure (whole body vs. nose only), and sex differences also existed. It is important to note that we examined male BALB/c mice rather than females used in six previous reports19,20,22,29,30,31. It is worth noting that 70–75% of melioidosis cases are male, indicating a sex difference in melioidosis susceptibility5,32,33. However, it has been suggested that sex differences observed in clinical melioidosis may be due to increased exposure due to outdoor occupations of men33.
Doxycycline was effective at preventing death from exposure to aerosolized B. pseudomallei, similar to what was shown by Sivalingam et al., who demonstrated that 100% of mice survived when doxycycline was administered at the time of challenge and 80% of mice survived when doxycycline was administered 10 hours after challenge34. The sterility achieved in the lungs in 19 of 20 mice was similar to what was previously shown with no bacteria being detected by nine days post-challenge. In conclusion, the BALB/c mouse is a useful model of melioidosis and post-exposure prophylaxis by doxycycline is likely to be effective, based on the mouse model.
Methods
Aerosolization of B. pseudomallei
B. pseudomallei 1026b was obtained from BEI Resources (cat #NR-4074) and a working cell bank of single use glycerol stock vials are cryopreserved at −70°C at Battelle. The B. pseudomallei was propagated from frozen culture in Luria broth plus 4% glycerol. Mid to late-log phase cultures were used to generate aerosols. The aerosol exposure system used for the mouse aerosol challenge testing consisted of a system capable of exposing multiple animals (up to 30) with the addition of impinger samplers, an aerosol particle size analyzer, temperature and humidity monitoring, mass flow meters (MFM) and mass flow controllers (MFC) to monitor the aerosol flows. To generate B. pseudomallei 1026b containing aerosols, forced air entered Battelle's custom system through high efficiency particulate air (HEPA) filters and was divided into a continuous air stream (continuous air) and an air stream that either flowed into the Collison nebulizer (during aerosol generation) or by-passes it (between aerosol generations). Mass flow controllers (MFC) regulated the flow for each of the air streams. The B. pseudomallei aerosol, created by the nebulizer, was allowed to mix with continuous air before being delivered to the exposure chamber. A nose-only aerosol exposure system (CH Technologies Tower) was utilized to deliver the desired B. pseudomallei aerosol. From the exposure chamber the aerosol was sampled for concentration dose determination of B. pseudomallei using an impinger (model 7541, Ace Glass, Inc.). The liquid in the nebulizer and impinger was diluted and enumerated by the spread plate and/or filtering technique to quantify viable B. pseudomallei bacteria counts per mL. The B. pseudomallei concentration (based on enumerations) of the nebulizer and impinger samples were used to determine the actual exposure dose for each challenge group. Using Guyton's formula and the concentration of B. pseudomallei collected from air sampled from the exposure system, the inhaled dose was determined from the enumeration results.
Animals
A total of 160 male BALB/c mice approximately 6–8 weeks of age were obtained from Charles River. Mice were obtained at different times for either the LD50 determination or for the efficacy of doxycycline determination. Mice were observed twice daily throughout the experiments for signs of morbidity and mortality. Animal use protocols were approved by Battelle's Institutional Animal Care and Use Committee (IACUC) and the Department of Defense Animal Care and Use Review Office (ACURO).
LD50 determination
A total of 120 male BALB/c mice were used to estimate the LD50, in three phases. In phase I, eight groups of six mice were exposed to escalating targeted doses of aerosolized B. pseudomallei 1026b ranging from 5 to 5,000 cfu/mouse. Phase II consisted of six groups of six mice were exposed to escalating targeted doses of aerosolized B. pseudomallei 1026b ranging from 7,000 to 100,000 cfu/mouse. Phase III consisted of six groups of six mice were exposed to escalating targeted doses of aerosolized B. pseudomallei 1026b ranging from 2,000 to 8,000 cfu/mouse. LD50 estimates were made following each phase to plan targeted doses for the subsequent phase.
Antibiotic efficacy testing
A total of 40 male BALB/c mice were used to test the efficacy of doxycycline in post-exposure prophylaxis. Mice were divided into doxycycline and sterile water for injection (WFI) groups of 20 mice each. Five mice from each group were exposed to aerosolized B. pseudomallei 1026b on four different runs to a target of 5.6 × 104 cfu (~20 LD50). Following the aerosol challenge, antibiotic therapy began approximately 6 (±1 hr) hours post median challenge time. Mice in the doxycycline treatment group received doxycycline at a dose of 40 mg/kg twice a day (BID) for 14 days [every 12 (±1 hr) hours]. This dosing regimen was selected to ensure that the area under the concentration time curve for a 24 hour period (AUC0–24) was similar in mice compared to the human label dose. This approach is favored as the antimicrobial pattern of doxycyline predicts that AUC0–24 will determine efficacy35. Doxycycline dose label indicates 100 mg every 12 hours for the average person. However, published human data was only available for a 200 mg dose, with an AUC0–12 of 30 μg*h/mL (based on trapezoidal calculation using data from Newton 200536). This data was used as the basis of a 100 mg twice daily regimen and calculated the AUC0–24 was approximately 30 μg*h/mL. In mice, the AUC0–6 has been reported to be 13.7 μg*h/mL with a dose of 25 mg/kg37. In order to achieve an AUC0–24 near 30 μg*h/mL, BID dosing of 40 mg/kg was used. Doxycycline (Vibramycin® calcium syrup oral suspension, Pfizer Labs, NY, NY) was obtained from a local pharmacy. Control mice received WFI for 14 days [every 24 (±1 hr) hours] or until death at a volume of 5 mL/kg QD. Dosing occurred via orogastric intubation. Mice were observed for clinical signs of disease and survival for 28 days following aerosol exposure.
Tissue bacterial burden
The bacterial burden in the lungs and spleen was determined by quantitative PCR from all mice found dead or euthanized from the antibiotic efficacy testing. At the time a mouse was found dead or following euthanasia, a specimen of lung and spleen at gross necropsy was collected for bacterial burden analysis. The lung and spleen specimens were weighed, manually homogenized using a tissue grinder and total nucleic acid was isolated using the NucliSens easyMAG (bioMerieux, Durham, NC). Briefly, 100 μL of sample was added to sample vessels that were loaded into the instrument. The instrument then dispensed easyMAG Lysis Buffer (bioMerieux, Durham, NC) and incubated the samples for 10 minutes. Afterwards, easMAG Magnetic Silica (bioMerieux, Durham, NC) was added to the samples. The instrument then incubated the samples for 10 minutes, collected the silica into pellets, and washed them subsequently with easyMAG Extraction Buffer 1 (bioMerieux, Durham, NC), easyMAG Extraction Buffer 2 (bioMerieux, Durham, NC), and easyMAG Extraction Buffer 3 (bioMerieux, Durham, NC). The purified nucleic acid was then eluted from the silica with 100 μL of easyMAG Extraction Buffer 3(bioMerieux, Durham, NC) and assayed. Based on published sequence data, oligonucleotides were designed to amplify a small fragment within the coding region of the rpoB gene product on the B. pseudomallei chromosome. We selected the rpoB target because it contained a 1026b sequence that was not identified in other B. pseudomallei strains with previously published genome sequences. Thus, oligonucleotide sequences were submitted to Applied Biosystems for the generation of a TaqMan® Gene Expression Assay which generated a forward primer of 5'-CCGGCGGCAGTTCGT-3', a reverse primer of 5'-AGCTCGAAGCGATCAAGAACTC-3' and a probe of 6'FAM-CGAACTGGTGGCGCT-MGBNFQ-3′. Qualitative real-time PCR reactions consisted of 1× TaqMan® Gene Expression Master Mix [AmpliTaq Gold® DNA Polymerase, AmpErase® UNG, dNTPs with dUTP, Passive Reference, and optimized buffer components (Applied Biosystems Inc., Foster City, CA)], 1× Gene Expression Assay mixture [900 nM forward primer, 900 nM reverse primer, and 250 nM probe (dual-labeled with FAMTM at the 5′ and a non-fluorescent quencher at the 3′ end)], dIH20, and 5 μL isolated genomic DNA in a total volume of 50 μL. Qualitative real-time PCR was performed using an ABI PRISM® Sequence Detection System (Applied Biosystems Inc., Foster City, CA) with the following conditions: 2 min at 50°C, 10 min at 95°C, followed by 40 cycles of 95°C for 15 seconds and 60°C for 1 min. All reactions were performed in triplicate, and each run contained known negative (genomic DNA isolation procedure using dIH20) and positive (genomic DNA isolated from a B. pseudomallei vegetative culture) controls. Following acquisition, data was analyzed using Version 2.3 of the Sequence Detection System software (Applied Biosystems Inc., Foster City, CA). A quantity was reported for any sample that demonstrated a quantity ≥ 2 copies/μL. For samples < 2 copies/μL, the sample was considered negative.
Statistical methods
The cumulative data from all completed phases were fitted to a logistic regression model to obtain a preliminary estimate of the LD50 to define the next phase. Once all three phases were completed, all data were fitted to a logistic regression model whereby the probability of lethality was modeled against the base-10 logarithm of the inhaled dose. All models were fitted in SAS® (ver. 9.1) using PROC PROBIT with a logistic link function. Estimated parameters of the logistic model were used to compute the LD50 and LD90 while Fieller's method was used to compute an upper one-sided 95 percent confidence bound for each estimate.
For antibiotic efficacy testing, survival rates were calculated for each group. A two-sided Fisher's exact test was used to compare the survival rates between the groups. Then, a time-to-death model was fitted using the treatment and control group. The Kaplan-Meier curves were plotted and the log-rank test was computed to determine if the difference was statistically significant. To determine if there were significant differences in the distribution of tissue bacterial burden levels between the treated and control groups, a two-sample Kolmogorov-Smirnov test was performed on the tissue bacterial burden data for each specimen location.
Author Contributions
H.C.G. and D.C.S. wrote the main manuscript text, M.S.A. designed and conducted statistical analysis and wrote the statistical methods section, D.A.F. designed and conducted the aerosol exposure, M.T.F., Z.X. and D.C.S. designed the studies. All authors reviewed the manuscript.
Acknowledgments
We would like to acknowledge Rachelle Stammen, Jean Truxall, Roy Barnewall, Brock Miniard and Dennis Pak for excellent technical assistance. This work was supported by the Defense Threat Reduction Agency under Transformational Medical Technologies Initiative contract # HDTRA-08-C-0049 (Principal Investigator: Ze-Qi Xu).
References
- Currie B. J., Dance D. A. & Cheng A. C. The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg 102 Suppl 1, S1–4 (2008) [DOI] [PubMed] [Google Scholar]
- Wiersinga W. J., Currie B. J. & Peacock S. J. Melioidosis. N Engl J Med 367, 1035–44 (2012). [DOI] [PubMed] [Google Scholar]
- Cheng A. C. & Currie B. J. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev 18, 383–416 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie B. J. & Jacups S. P. Intensity of rainfall and severity of melioidosis, Australia. Emerg Infect Dis 9, 1538–42 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie B. J., Ward L. & Cheng A. C. The epidemiology and clinical spectrum of melioidosis: 540 cases from the 20 year Darwin prospective study. PLoS Negl Trop Dis 4, e900 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngauy V., Lemeshev Y., Sadkowski L. & Crawford G. Cutaneous melioidosis in a man who was taken as a prisoner of war by the Japanese during World War II. J Clin Microbiol 43, 970–2 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alibek K. & Handelman S. Biohazard: The Chilling True Story of the Largest Covert Biological Weapons Program in the World--Told from Inside by the Man Who Ran It Random House, 1999. [Google Scholar]
- Thibault F. M., Hernandez E., Vidal D. R., Girardet M. & Cavallo J. D. Antibiotic susceptibility of 65 isolates of Burkholderia pseudomallei and Burkholderia mallei to 35 antimicrobial agents. J Antimicrob Chemother 54, 1134–8 (2004). [DOI] [PubMed] [Google Scholar]
- Currie B. J., Fisher D. A., Anstey N. M. & Jacups S. P. Melioidosis: acute and chronic disease, relapse and re-activation. Trans R Soc Trop Med Hyg 94, 301–4 (2000). [DOI] [PubMed] [Google Scholar]
- White N. J. Melioidosis. Lancet 361, 1715–22 (2003). [DOI] [PubMed] [Google Scholar]
- Veljanov D., Vesselinova A., Nikolova S., Najdenski H., Kussovski V. & Markova N. Experimental melioidosis in inbred mouse strains. Zentralbl Bakteriol 283, 351–9 (1996). [DOI] [PubMed] [Google Scholar]
- Leakey A. K., Ulett G. C. & Hirst R. G. BALB/c and C57Bl/6 mice infected with virulent Burkholderia pseudomallei provide contrasting animal models for the acute and chronic forms of human melioidosis. Microb Pathog 24, 269–75 (1998). [DOI] [PubMed] [Google Scholar]
- Hoppe I., Brenneke B., Rohde M., Kreft A., Haussler S., Reganzerowski A. & Steinmetz I. Characterization of a murine model of melioidosis: comparison of different strains of mice. Infect Immun 67, 2891–900 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santanirand P., Harley V. S., Dance D. A., Drasar B. S. & Bancroft G. J. Obligatory role of gamma interferon for host survival in a murine model of infection with Burkholderia pseudomallei. Infect Immun 67, 3593–600 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauthier Y. P., Hagen R. M., Brochier G. S., Neubauer H., Splettstoesser W. D., Finke E. J. & Vidal D. R. Study on the pathophysiology of experimental Burkholderia pseudomallei infection in mice. FEMS Immunol Med Microbiol 30, 53–63 (2001). [DOI] [PubMed] [Google Scholar]
- Liu B. Koo G. C., Yap E. H., Chua K. L. & Gan Y. H. Model of differential susceptibility to mucosal Burkholderia pseudomallei infection. Infect Immun 70, 504–11 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Zandt K. E. Tuanyok A. Keim P. S. Warren R. L. & Gelhaus H. C. An Objective Approach for Burkholderia pseudomallei Strain Selection as Challenge Material for Medical Countermeasures Efficacy Testing. Front Cell Infect Microbiol 2, 120 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy C. J. & Pitt M. L. Infectious Disease Aerobiology: Aerosol Challenge Methods. in: J. R. Swearengen, (Ed.), Biodefense Research Methodology and Animal Models, CRC Press, Boca Raton, FL, 2006, pp. 61–76. [Google Scholar]
- Lever M. S., Nelson M., Stagg A. J., Beedham R. J. & Simpson A. J. Experimental acute respiratory Burkholderia pseudomallei infection in BALB/c mice. Int J Exp Pathol 90, 16–25 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeddeloh J. A., Fritz D. L., Waag D. M., Hartings J. M. & Andrews G. P. Biodefense-driven murine model of pneumonic melioidosis. Infect Immun 71, 584–7 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieves W., Asakrah S., Qazi O., Brown K. A., Kurtz J., Aucoin D. P., McLachlan J. B., Roy C. J. & Morici L. A. A naturally derived outer-membrane vesicle vaccine protects against lethal pulmonary Burkholderia pseudomallei infection. Vaccine 29, 8381–9 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan G. Y., Liu Y., Sivalingam S. P., Sim S. H., Wang D., Paucod J. C., Gauthier Y. & Ooi E. E. Burkholderia pseudomallei aerosol infection results in differential inflammatory responses in BALB/c and C57Bl/6 mice. J Med Microbiol 57, 508–15 (2008). [DOI] [PubMed] [Google Scholar]
- Chaowagul W., Chierakul W., Simpson A. J., Short J. M., Stepniewska K., Maharjan B., Rajchanuvong A., Busarawong D., Limmathurotsakul D., Cheng A. C., Wuthiekanun V., Newton P. N., White N. J., Day N. P. & Peacock S. J. Open-label randomized trial of oral trimethoprim-sulfamethoxazole, doxycycline, and chloramphenicol compared with trimethoprim-sulfamethoxazole and doxycycline for maintenance therapy of melioidosis. Antimicrob Agents Chemother 49, 4020–5 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelhaus H. C. Barnewall R. Cross J. Lindsay A. S. & Lockman, H. Qualification of a Mouse Model of Tularemia by Confirming Doxycycline Efficacy, 50th Interscience Conference on Antimicrobial Agents and Chemotherapy, Boston, MA, 2010.
- Kenny D. J., Russell P., Rogers D., Eley S. M. & Titball R. W. In vitro susceptibilities of Burkholderia mallei in comparison to those of other pathogenic Burkholderia spp. Antimicrob Agents Chemother 43, 2773–5 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenney A. W., Lum G., Fisher D. A. & Currie B. J. Antibiotic susceptibility of Burkholderia pseudomallei from tropical northern Australia and implications for therapy of melioidosis. Int J Antimicrob Agents 17, 109–13 (2001). [DOI] [PubMed] [Google Scholar]
- Fisher M. W., Hillegas A. B. & Nazeeri P. L. Susceptibility in vitro and in vivo of Pseudomonas pseudomallei to rifampin and tetracyclines. Appl Microbiol 22, 13–6 (1971). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W. H. & Manion R. E. Antibiotic susceptibility of Pseudomonas pseudomallei. Antimicrob Agents Chemother 4, 193–5 (1973). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar-Tyson M., Smither S. J., Harding S. V., Atkins T. P. & Titball R. W. Protective efficacy of heat-inactivated B. thailandensis, B. mallei or B. pseudomallei against experimental melioidosis and glanders. Vaccine 27, 4447–51 (2009). [DOI] [PubMed] [Google Scholar]
- Ulrich R. L., Deshazer D., Brueggemann E. E., Hines H. B., Oyston P. C. & Jeddeloh J. A. Role of quorum sensing in the pathogenicity of Burkholderia pseudomallei. J Med Microbiol 53, 1053–64 (2004). [DOI] [PubMed] [Google Scholar]
- Nelson M., Prior J. L., Lever M. S., Jones H. E., Atkins T. P. & Titball R. W. Evaluation of lipopolysaccharide and capsular polysaccharide as subunit vaccines against experimental melioidosis. J Med Microbiol 53, 1177–82 (2004). [DOI] [PubMed] [Google Scholar]
- Hassan M. R., Pani S. P., Peng N. P., Voralu K., Vijayalakshmi N., Mehanderkar R., Aziz N. A. & Michael E. Incidence, risk factors and clinical epidemiology of melioidosis: a complex socio-ecological emerging infectious disease in the Alor Setar region of Kedah, Malaysia. BMC Infect Dis 10, 302 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie B. J., Jacups S. P., Cheng A. C., Fisher D. A., Anstey N. M., Huffam S. E. & Krause V. L. Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop Med Int Health 9, 1167–74 (2004). [DOI] [PubMed] [Google Scholar]
- Sivalingam S. P. Sim S. H. Jasper L. C. Wang D. Liu Y. & Ooi E. E. Pre- and post-exposure prophylaxis of experimental Burkholderia pseudomallei infection with doxycycline, amoxicillin/clavulanic acid and co-trimoxazole. J Antimicrob Chemother 61, 674–8 2008. [DOI] [PubMed] [Google Scholar]
- Craig W. A. Pharmacodynamics of antimicrobials: general concepts and applications. in: C. H. Nightingale, T. Murakawa, and P. G. Ambrose, (Eds.), Antimicrobial pharmacodynamics in theory and clinical practice., Marcel Dekker, Inc. New York, NY, 2002, pp. 1–22. [Google Scholar]
- Newton P. N., Chaulet J. F., Brockman A., Chierakul W., Dondorp A., Ruangveerayuth R., Looareesuwan S., Mounier C. & White N. J. Pharmacokinetics of oral doxycycline during combination treatment of severe falciparum malaria. Antimicrob Agents Chemother 49, 1622–5 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heine H. S., Louie A., Sorgel F., Bassett J., Miller L., Sullivan L. J., Kinzig-Schippers M. & Drusano G. L. Comparison of 2 antibiotics that inhibit protein synthesis for the treatment of infection with Yersinia pestis delivered by aerosol in a mouse model of pneumonic plague. J Infect Dis 196, 782–7 (2007). [DOI] [PubMed] [Google Scholar]