Abstract
BACKGROUND
The high rates of childhood overweight and obesity in the US have generated interest in schools as sites for monitoring BMI information. This study established baseline values for a 5-year longitudinal assessment of BMI of elementary school children and examined variation across the schools, because little is known about factors that affect the distribution of overweight and obesity within school districts.
METHODS
Height and weight measurements were collected on 2,317 elementary school children in one school district. BMI was calculated using the CDC’s NutStat program. Child characteristics included gender, age, eligibility for free and reduced lunch (proxy for SES), school, grade, and ethnicity/race. Children were grouped into 2 BMI categories, < 85th percentile or ≥ 85th percentile (overweight/obesity). Logistic regression was used to examine potential predictors of overweight/obesity.
RESULTS
Prevalence of ≥ 85th percentile was 30.9%, 34.4%, 35.3%, 36.4%, 37.1%, and 44.5% for K-5 respectively. Prevalence of ≥ 85th percentile was highest among Hispanic children. Ethnicity was the strongest predictor of inclusion in the ≥ 85th percentile category followed by grade and free and reduced lunch eligibility.
CONCLUSION
The data are consistent with the prevalence of overweight/obesity among American children and Hispanic children in particular. District prevalence of overweight/obesity is higher than available state statistics. Most of the BMI variation is accounted for by ethnicity, SES, and grade. The grade effect and high prevalence of overweight/obesity provide a rationale for BMI screening retention at the schools.
Keywords: BMI prevalence, overweight and obesity predictors, elementary school children
The prevalence of child overweight and obesity has increased dramatically over the last 3 decades across all sectors of the US population, leading to one of the nation’s greatest public health challenges. Data from the Centers for Disease Control and Prevention (CDC)1 indicate that approximately 17% (or 12.5 million) of children and adolescents aged 2-19 years are obese (BMI ≥ 95th percentile).2 Among school-aged children, comparisons of data from NHANES surveys administered in 1976-1980 and 2007-2008 show that the prevalence of obesity has changed from 6.5% to 19.6% among children 6-11 years of age and from 5.0% to 18.1% for those aged 12-19 years.3 Recent findings suggest that the obesity epidemic among children may not yet have reached its plateau for some groups of children and that there are persistent and highly variable disparities in childhood overweight and obesity within and among states. Variation is also associated with socioeconomic status, school outcomes, and neighborhoods.4 Overweight (BMI ≥ 85th percentile for children of the same age and sex and < 95th percentile) and obesity (BMI ≥ 95th percentile for children of the same age and sex) during childhood and adolescence are associated with the onset of a variety of serious health conditions including Type 2 diabetes, hypertension, hyperlipidemia, fatty liver disease, asthma, sleep apnea, and certain types of cancer.5-8 Poor psychosocial adjustments also are associated with obesity among children and adolescents, including lower self-esteem, depression, and behavioral problems.9-13 This recognition of the growing prevalence of overweight and obesity among children led both the American Pediatric Society and the Institute of Medicine to urge schools to assess the BMI of their students and provide the information to parents.14,15
Currently, school-based BMI assessment for both screening and surveillance is considered a potentially important part of a multifaceted strategy for reducing both child and adolescent overweight and obesity.16,17 School-based BMI screening has the potential for parental and child health education as well as addressing the increasing levels of disparities in child obesity.18-23 Additionally, BMI screening can provide information about student health to assist districts and schools in implementing policies and programs that promote healthy behaviors appropriate to districts or specific schools.16,24 To date, however, the actual effectiveness of BMI screening in schools has not been evaluated and, frequently, efforts to introduce school-based BMI screening and reporting have met with concerns. These include questions regarding legal and reporting issues, concerns about the potential for increased rates of eating disorders, and the actual challenges of measuring BMI in schools.25,26
Consequently, there is considerable variation among states in terms of having BMI screening as part of the school policy. According to a 2010 study27 involving telephone interviews with departments of education of each state in the country, 20 states required BMI or body composition school-based screening of children and 9 other states recommended some form of BMI screening, often in association with fitness testing. The researchers found that the states that required BMI screening or fitness assessment were 3.1 percentage points higher in adolescent obesity (16.7% vs. 13.6%, p < .001) than states without screening or assessment requirements, even when enrollment rates were adjusted. The authors suggested it was possible that states with the greatest prevalence of obesity have instituted screening policies to improve the health of their children; however, they were not able to assess causality.
The information gathered in this study is from year one of a 5-year project. Oregon does not currently have legislation or practices directing a compendium of BMI statistics on children. The specific objectives of the present study were to: (1) establish baseline values for a 5-year longitudinal assessment of factors affecting BMI in elementary school children in the school district, (2) conduct an initial analysis of high BMI (≥ 85th percentile) scores using student level predictors, and (3) build upon previous research20,22,26,28 to examine variation across the elementary schools, because little is known about factors that may affect the distribution of overweight and obesity within a school district. Such information may be important for formulating district-based health policies.
METHODS
Background and Setting
Health information for Oregon indicates variable and inconsistent rates of child obesity (from 9.6% to 26.5%).29-33 A 9.6% rate for child obesity was reported in 2010 based on a representative sample of parents who reported height and weight information about their children through a telephone survey (N = 1794 children).32,33 A higher prevalence of child overweight and obesity (approximately 26.5% of the state’s children ages 10-17 years) was reported by the Child Obesity Action Network,29 which again was based on parent report of child height and weight. Finally, a 2005-2006 project in the district’s county, including the school district involved in the present study, used direct measures of height and weight for 10,853 K-8 students in 16 school districts and found 35% of students measured were overweight/obese.34
As of 2012 Oregon did not have any BMI school-based legislation. However, there are a number of state level policies and legislation that aim to encourage the development of healthy school environments as a key to reversing the obesity epidemic.30 These include limitations on when and where competitive foods may be sold in vending machines, school stores, and à la carte lines, and legislation establishing state administrative support and funding for farm-to-school programs in Oregon schools. Oregon currently does not legislatively mandate the amount of minutes required weekly for physical education in grades K-8. However, in 2007 Oregon passed House Bill 3141 that will require K-5 students to receive physical education for 150 minutes per week and students in grades 6-8 to receive 225 minutes each week of physical education. These legislative requirements are to become effective in 2017.
This study presents initial BMI measures of 2317 elementary school students recruited to the Communities and Schools Together for Childhood Obesity Prevention project (CAST), a 5-year community-based participatory research study examining the environmental and social influences on the prevalence of child overweight and obesity in a suburban Oregon school district (project website—http://castpublic.ori.org).35 This district, the third largest in the county, encompasses 31.7 square miles and borders a large metro community and an agricultural-rural section of the county. The district has one regular high school, one alternative high school, 2 middle schools, 2 K-8 schools, and 5 elementary (K-5) schools. The district serves approximately 6000 students (3000 elementary school children). Compared with the state, the district has a larger percentage of students eligible for free and reduced lunch (41.5% state vs. 46.8% district), a smaller percentage of students with English as a Second Language (ESL)36 (10.3% state vs. 2.2% district), and a slightly smaller percentage of Hispanic students36 (state 17.2% vs. 13.9% district). Academically, a higher percentage of district students exceeded state standards for reading (state 81.4% vs. district 84.4%), but did not differ from the state with respect to those exceeding mathematics standards (state 69.4% vs. district 69.3%).36 School nurses initiated BMI screening of kindergarten and third grade children in 2004 and reported the BMI information to the parents using a letter that explained the measurement process. In 2005-2006 the district participated in a one-time county BMI assessment project. At that time all elementary grades in the district were screened; the school district then reverted to screening just kindergarten and third grade children in 2007. The BMI screening used in this study was conducted by the CAST project in 2008 and included height and weight measures of students in all elementary school grades K-5.
Participants
In the first year of the CAST project, during fall of the 2008-2009 school year, all families of children in grades K-5 who attended any of the 7 elementary schools were sent a description of the CAST project by mail, using mailing labels provided by the school district. Included with the description was an opt-out card as part of a passive consent procedure. Of the 2697 families who received the materials, 189 (7%) declined to have their children participate, leaving 2,508 children in the first year cohort. District staff assigned a study ID, linked to district student ID, to all participating students. School data for participants were transferred to project databases using the study ID, with a link file relating study ID to student ID maintained only by the district. Among enrolled CAST students, 192 did not participate in height and weight measurements because they were absent during the screening period, were home-schooled, or used a wheelchair. Height and weight measures were collected for 2317 (~92%) of the year one student cohort.
School Record Data
Child characteristics used in this study included data elements extracted from the district data system including gender, age, school, grade, ethnicity, race, and eligibility for free and reduced lunch (a proxy for SES). Home addresses were used to construct a household (family) ID, and to calculate the number of elementary school siblings for each participant. Schools were categorized into types, ESL and non-ESL, based on the district’s policy of having ESL programs concentrated in 3 of the elementary schools. This variable was included since some 67% of Hispanic students in the sample attended these 3 schools.
Body Mass Index (BMI)
Height and weight data for each child were collected in conjunction with the district’s annual health screening. Measurement procedures were consistent with standardized anthropometric procedures.37 Each child was weighed using a portable digital scale (Tanita BWB-800S). Height was measured using a portable child-adult measuring stadiometer board with inch-foot measuring tape and auto head lock (ShorrBoard 420). The height measurements were done by 2 research assistants trained in anthropometric measurements. One individual did the actual measurement while the other monitored placement of the child. Both individuals read the stadiometer and if there was a discrepancy of more than 0.25 inches the child was re-measured. Since the scale was digital only one individual read and recorded the output. All data were recorded directly on the district health screening forms.
Following the collection of BMI health screening data, the health screening forms were given to a school health aide whom the district designated to enter each student’s health screening results into the district’s e-Schools database. The CAST School-Community Coordinator and school nurses conducted a 10% data entry reliability assessment to check for entry errors. Two percent of the checked records were found to have been entered incorrectly—these entries were corrected. In addition, attendance records of CAST students who were not measured were inspected to ascertain whether the student was actually present on the day of the screening. All absences were confirmed.
Data Analysis
Height and weight data were transferred to the CAST project database for data management and analysis. The Epi Info (CDC, Atlanta, Georgia) analysis tool, NutStat, a nutrition anthropometry program that calculates BMI from age and gender normed tables, was used to calculate raw BMI, z-score, and percentile equivalents. Using CDC guidelines,38 data for one student with a BMI z-score < −4.0 was excluded from further analysis for a final N of 2,316. The categorization of students into 2 groups—less than 85th percentile and greater than or equal to 85th percentile—was used in this study in order to contrast overweight/obese students with students of normal weight. This type of categorization has been used by others28 and provides a useful classification for those developing school-based interventions to address students with a high BMI (ie, it is unlikely that interventions will be developed that will not address both overweight and obese students).
The binary response variable for obesity, (0 = BMI percentile < 85, 1 = BMI percentile ≥ 85) as per O’Malley,28 was modeled using 6 predictors: gender (0 = Female*, 1 = Male); eligibility for free & reduced lunch (0* = No, 1 = Yes); Race/Ethnicity (0* = White, 1 = Hispanic, 2 = African American, Native American, Asian/Pacific Islander); grade (K*-5); the number of elementary school siblings in the household (0 = None*, 1 = 1 or more); and whether the student attended an ESL school (0 = No*, 1 = Yes), with * indicating the reference category.
The CAST BMI sample (93% of eligible district students) did not differ from the district with respect to gender or race/ethnicity. However, it did differ from the district in the percent of students participating in the free & reduced lunch program—district: 1474/2,808 = 52.5%; CAST BMI sample: 1068/2316 = 46%; χ2 (1, N = 5,124) = 20.4043, p < .00001. Using the lower participation in free and reduced lunch programs as a proxy for low SES, the CAST sample had a higher SES than did the district as a whole. Thus, if participation in the free and reduced lunch program proved to be a significant predictor of overweight/obese status for the CAST sample, this would underestimate the strength of the relationship for the district.
Initial analyses were conducted using a generalized mixed modeling approach to construct a binomial model with nesting in school. The intraclass correlation for school was less than .001. For the final logistic model, school was recoded into a categorical variable to reflect whether or not a student attended one of the three ESL schools.
RESULTS
Table 1 describes the characteristics of the 2316 CAST students with valid BMI data. Average age was 8.2 years, 51% were male, 55% had no siblings, 46% were eligible for the district’s free & reduced lunch program, and 44% attended an ESL school. The percent of students in each grade was relatively consistent (range 16% to 18). Analysis of the BMI data indicated 17.3 % of the students were in the overweight category (BMI percentile ≥ 85th and < 95th percentile) and 19.4% were in the obese category (BMI ≥ 95th percentile) (Table 2). The percent of obese children in the district was similar to the 2008 national average of 19.6%.3 When the overweight and obese categories were combined, a total of 36.7% of the children fell into the ≥ 85th percentile category. Comparison across schools (Table 2) of the percent of students in the ≥ 85th percentile showed some variation (range 32.56% to 44.44%) and 2 of the schools with the highest percentage of ≥ 85th percentile among students were ESL schools
Table 1. Demographics of Sample.
| Year 2008/09 (Total N = 2316)a | ||
|---|---|---|
| Characteristic | N | % or Mean (SD) |
| Gender | ||
| Male | 1184 | 51% |
| Female | 1132 | 49% |
| Ethnicityb | ||
| African American | 67 | 3% |
| Asian/Pacific Islander | 58 | 3% |
| Hispanic | 348 | 16% |
| Native American | 44 | 2% |
| White | 1717 | 77% |
| Age in years | 2316 | 8.2 (1.74) |
| Siblings | ||
| No grade K–5 sibs | 1272 | 55% |
| 1 or more grade K–5 sibs | 1044 | 45% |
| Free & Reduced Lunch | ||
| Yes | 1068 | 46% |
| No | 1248 | 54% |
| School ESL status | ||
| ESL–designated | 1009 | 44% |
| Non-ESL-designated | 1307 | 56% |
| Grades | ||
| K | 362 | 16% |
| 1 | 371 | 16% |
| 2 | 372 | 16% |
| 3 | 393 | 17% |
| 4 | 398 | 17% |
| 5 | 420 | 18% |
After removal of the single case who did not meet CDC criteria for inclusion.
82 students did not have ethnicity information.
Table 2. Elementary School Demographics: School Year 2008–2009.
| School |
|||||||
|---|---|---|---|---|---|---|---|
| Demographic | 1 | 2a | 3a | 4 | 5 | 6 | 7a |
| School Characteristics | |||||||
| School type | K–5 | K–5 | K–5 | K–5 | K–5 | K–8b | K–8b |
| # Students enrolled | 324 | 337 | 336 | 422 | 346 | 477 | 533 |
| % Minority students | 19.41% | 34.10% | 38.40% | 16.41% | 21.10% | 14.01% | 23.91% |
| # Students eligible | 316 | 323 | 330 | 409 | 340 | 465 | 514 |
| CAST Student participants | 300 | 297 | 306 | 387 | 309 | 429 | 480 |
| Total N | 272 | 278 | 288 | 372 | 273 | 390 | 443 |
| Annual BMI Results | |||||||
| % Underweight | 1.47% | 0.36% | 1.39% | 1.61% | 1.47% | 1.79% | 0.45% |
| % Normal | 62.13% | 58.63% | 54.17% | 62.90% | 60.44% | 65.64% | 66.82% |
| % Overweight | 15.81% | 17.99% | 21.88% | 18.01% | 16.12% | 17.69% | 14.45% |
| % Obese | 20.59% | 23.02% | 22.57% | 17.47% | 21.98% | 14.87% | 18.28% |
| % Total overweight/obese | 36.40% | 41.01% | 44.44% | 35.48% | 38.10% | 32.56% | 32.73% |
| Academic Achievement | |||||||
| Meet/Exceed reading | 83% | 77% | 83% | 89% | 82% | 89% | 83% |
| Meet/Exceed math | 80% | 72% | 75% | 86% | 79% | 89% | 83% |
| Eligibility School Meals | |||||||
| # Free lunch | 142 | 173 | 237 | 111 | 174 | 178 | 308 |
| # Reduced lunch | 38 | 44 | 36 | 43 | 50 | 53 | 100 |
| % Free & reduced lunch | 55.61% | 64.40% | 81.31% | 36.51% | 64.70% | 48.41% | 76.50% |
English as a Second language school.
Values shown for grades K–5.
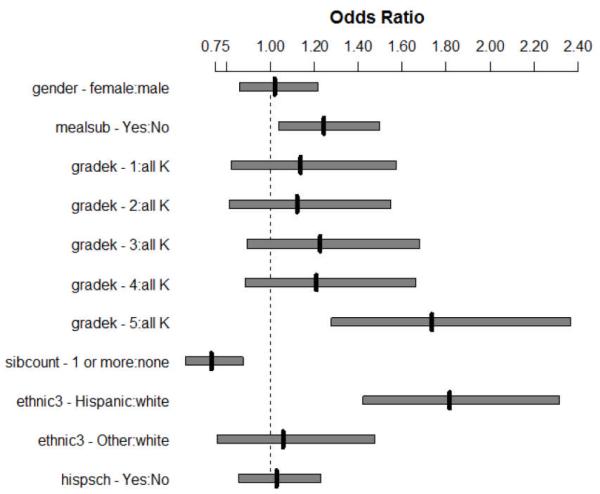
As Figure 1 shows, 4 of the 6 predictors, (ethnicity, grade, free and reduced lunch, number of siblings) in the model were significant. Of these, the strongest predictor of being in the overweight/obesity category (a BMI percentile greater than 85th percentile) was the ethnicity of the student, with Hispanic students 1.81 times as likely to be in the overweight/obese category, p < .0001, 95% CI [1.42, 2.32], than were white students. Older children were more likely to be in the ≥ 85th percentile category with fifth grade students being 1.74 times more likely to be overweight/obese than were those in kindergarten, p < .007, 95% CI [1.28, 2.36]. Students who were eligible for free and reduced lunch when compared to those who were not eligible were 1.24 times as likely to be overweight/obese, p < .02, 95% CI [1.04, 1.50]. Given that the district has a higher percentage of free and reduced meal students (52.5%) than the study’s BMI sample (46%), the effect would be even greater for the district as a whole. Finally, students with elementary school siblings were less likely (OR = .73, p < .0006, 95% CI [.61, .88]) to be overweight/obese than were students who did not have elementary school siblings.
Figure 1. Odds Ratios and 95% Confidence Intervals for 6 Predictors of BMI ≥ 85th Percentile.
DISCUSSION
This study provides information on the prevalence of overweight and obesity among elementary school children in one school district and explores some student factors that appear to predict overweight/obese status in this population. Schools have been identified as a potential site for monitoring the prevalence and distribution of childhood overweight and obesity. Additionally, understanding the variables that may affect the distribution of overweight and obesity within a school district may be important for formulating district, county, or even state-based health policies. Preliminary results of the baseline data point to individual factors as predictors of BMI. Although the district has a policy of locating English language instruction in specific schools, thus impacting the distribution of ethnicity within the district to some extent, school type was not a significant predictor. A major conclusion from this study is that overweight/obesity is prevalent in all of the schools and ethnicity itself is a more potent predictor. Although two of the ESL schools had the highest percentage of children in the ≥ 85th percentile category, the presence of Hispanic students throughout the district was a more important predictor. Similarly, within this district, low SES (through the proxy of free & reduced meal eligibility) also was associated with higher BMI.
Older children were more likely to be overweight/obese. This trend is consistent with other research.39 Although we are unable to specifically explain the trend at this time, possible factors could be an increase in body composition, specifically weight, as children begin to enter pre-pubertal and pubertal growth periods, or a decrease in activity. Hughes et al.39 suggested it might reflect differences in lifestyle at different ages, thus altering vulnerability to obesity, or differences in the extent to which the environment promoted obesity at different ages. Regardless of the cause, this result speaks to the importance of retaining or having BMI surveillance across grades in schools. Limiting measuring to specific grades such as 1 and 3 would not reveal this upward trend.
Finally, children who did not have elementary school siblings were more likely to fall into the overweight/obese group. This finding was unexpected but mirrors results found in another study. Chen and Escarce conducted a secondary analysis of the Early Childhood Longitudinal Study-Kindergarten Cohort (ECLS-K).40 The data included a nationally representative cohort of children who had entered kindergarten in 1998-1999. The researchers found family structure to be strongly associated with higher BMI scores among children. Children living in single mother families and especially children without siblings were those with the highest BMI scores. The mechanisms for these higher risks were not clear. Perhaps siblings provide more opportunities to engage in physical activity and play during the normal course of family life and reduce time spent in sedentary inactivity such as watching television. The interaction of family structure and single sibling status may be an important area of obesity risk among children and warrants further research.
Limitations
This study is limited in several ways. First, the BMI data is representative of only one time period. Prevalence of overweight and obesity within schools can vary over time and a longitudinal approach may provide a better perspective about across-school variation in this particular case. Additionally, the sample did not include any information on parent BMI or other demographic factors that may influence child BMI.
Finally, when considering the impact that schools may have on a student’s risk of overweight/obesity, it is important to account for factors associated with schools (eg, physical activity occurring in classes, relationship of recess time to lunch time, differences in cafeteria policies, food preparation). Subsequent analyses, based on student BMI measures as well as school and family characteristics collected in CAST project years 2-5 will address these issues
Conclusion
The results of the present study describe the prevalence of overweight/obesity in both boys and girls in one school district in Oregon, and establish baseline values for a 5-year longitudinal assessment of factors affecting BMI in elementary school children in the school district. Prevalence values use the Ogden cutoff3 of less than 85th percentile (underweight or normal) and greater than or equal to 85th percentile (overweight/obese). Prevalence of the overweight/obesity group varied across the schools (32.56% to 44.44%). In this district, despite the clustering of Hispanic students in the ESL schools, school of attendance is not a predictor of overweight/obesity. Most of the BMI variation lies within individuals and is accounted for by ethnicity, SES, and grade. The upward gradient of BMI as the students progress through elementary school is significant and points to the utility of BMI screening of all grades. Focusing only on specific grades would not provide adequate determination of changing trends as children age and would not give the full picture of prevalence of overweight or obesity. Finally, our examination of the variation in the prevalence of overweight/obesity across schools indicated that whereas schools varied in their prevalence of overweight/obesity, attendance in a specific school was not a significant predictor of a child’s BMI category. Examination of BMI prevalence across the elementary schools remains important because little is known about factors that may affect the distribution of overweight and obesity within a school district. Such information may be important for formulating district-based health policies.
IMPLICATIONS FOR SCHOOL HEALTH
School-based BMI assessment for both screening and surveillance is considered to be a potentially important part of a multifaceted strategy for reducing both child and adolescent overweight and obesity. However, the challenges of measuring BMI are widely recognized. The results of this study provide important information for the school districts that are situated in states that do not have BMI screening or surveillance legislation. Without a policy of its own such districts can rely only on state or national BMI and obesity information. As seen in this study for districts in Oregon such data can be unreliable since recent statistics for obesity prevalence in the state were well below those of the schools objectively measured in this study. Consequently, any district in the state attempting to initiate obesity prevention programs could be left without appropriate justification or the specific school level information required to plan, prioritize, and evaluate obesity prevention efforts. Developing a consistent, objectively measured BMI screening program and policy in schools and districts can provide important information not only for monitoring the health of the children but also for the development and evaluation of school-based and community interventions to ameliorate childhood obesity.
Human Subjects Approval Statement
This study, as well as its procedures and measures, was approved by Oregon Research Institute’s institutional review board. The board regularly monitors project activity for updates and changes to protocol.
ACKNOWLEDGEMENTS
We appreciate the assistance and work of the School District administrators, teachers, nurses and staff who willingly gave of their time to participate in the collection of the data. We thank all of the children who participated in the screening. We also greatly appreciate Susan Long who provided so much assistance with the development of the manuscript. This research was funded by grant 5 R01 HD05783 from the National Institute of Child Health and Human Development, National Institutes of Health.
Contributor Information
Geraldine Moreno, Oregon Research Institute, 1715 Franklin Blvd., Eugene, OR 97403.
Deb Johnson-Shelton, Oregon Research Institute, 1715 Franklin Blvd., Eugene, OR 97403, Phone: 541-484-2123, Fax: 541-484-1108, debj@ori.org.
Shawn Boles, Oregon Research Institute, 1715 Franklin Blvd., Eugene, OR 97403, Phone: 541-484-2123, Fax: 541-484-1108, shawn@ori.org.
REFERENCES
- 1.Centers for Disease Control (CDC) Obesity rates among all children in the United States. [Accessed August 2, 2012]. 2011. Updated April 21. Available at: http://www.cdc.gov/obesity/childhood/data.html. [Google Scholar]
- 2.Centers for Disease Control (CDC) How is childhood overweight and obesity measured? [Accessed August 2, 2012]. 2011. Basics about childhood obesity. Updated April 26. Available at: http://www.cdc.gov/obesity/childhood/basics.html. [Google Scholar]
- 3.Ogden C, Carroll M. Prevalence of obesity among children and adolescents: United States, trends 1963-1965 through 2007-2008. [Accessed August 2, 2012]. 2010. NCHS Health E-Stat. Updated June 4. Available at: http://www.cdc.gov/nchs/data/hestat/obesity_child_07_08/obesity_child_ 07_08.htm. [Google Scholar]
- 4.Bethell C, Simpson L, Stumbo S, Carle AC, Gombojav N. National, state, and local disparities in childhood obesity. Health Aff. 2010;29(3):347–356. doi: 10.1377/hlthaff.2009.0762. [DOI] [PubMed] [Google Scholar]
- 5.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(Suppl 2):S518–S525. [PubMed] [Google Scholar]
- 6.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood overweight to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108(3):712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 7.Friedlander SL, Larkin EK, Rosen CL, Palermo TM, Redline S. Decreased quality of life associated with obesity in school-aged children. Arch Pediatr Adolesc Med. 2003;157(12):1206–1211. doi: 10.1001/archpedi.157.12.1206. [DOI] [PubMed] [Google Scholar]
- 8.l’Allemand-Jander D. Clinical diagnosis of metabolic and cardiovascular risks in overweight children: early development of chronic diseases in the obese child. Int J Obesity (Lond) 2010;34(Suppl 2):S32–S36. doi: 10.1038/ijo.2010.237. [DOI] [PubMed] [Google Scholar]
- 9.Farhat T, Iannotti RJ, Simons-Morton B. Overweight, obesity, youth, and health-risk behaviors. Am J Prev Med. 2010;38(3):258–267. doi: 10.1016/j.amepre.2009.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003;111(4, pt 1):851–859. doi: 10.1542/peds.111.4.851. [DOI] [PubMed] [Google Scholar]
- 11.Vila G, Zipper E, Dabbas M, et al. Mental disorders in obese children and adolescents. Psychosom Med. 2004;66(3):387–394. doi: 10.1097/01.psy.0000126201.12813.eb. [DOI] [PubMed] [Google Scholar]
- 12.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 13.Zametkin AJ, Zoon CK, Klein HW, Munson S. Psychiatric aspects of child and adolescent obesity: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2004;43(2):134–150. doi: 10.1097/00004583-200402000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Krebs NF, Baker RD, Greer FR, et al. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 15.Koplan J, Liverman C, Kraak V. Preventing Childhood Obesity: Health in the Balance. National Academies Press; Washington, DC: 2005. [PubMed] [Google Scholar]
- 16.Stalter AM, Chaudry RV, Polivka BJ. Facilitating factors and barriers to BMI screening in schools. J Sch Nurs. 2010;26(4):320–330. doi: 10.1177/1059840510368524. [DOI] [PubMed] [Google Scholar]
- 17.Thompson J, Card-Higginson P. Arkansas’ experience: statewide surveillance and parental information on the child obesity epidemic. Pediatrics. 2009;124(Suppl 1):S73–S82. doi: 10.1542/peds.2008-3586J. [DOI] [PubMed] [Google Scholar]
- 18.Chomitz VR, Collins J, Kim J, Kramer E, McGowan R. Promoting healthy weight among elementary school children via a health report card approach. Arch Pediatr Adolesc Med. 2003;157(8):765–772. doi: 10.1001/archpedi.157.8.765. [DOI] [PubMed] [Google Scholar]
- 19.Madsen KA. School-based body mass index screening and parent notification. A statewide natural experiment. Arch Pediatr Adolesc Med. 2011;165(11):987–992. doi: 10.1001/archpediatrics.2011.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McMurty M, Jelian E. Child and Adolescent Newsletter. 1. Vol. 26. nBrown University; Providence, RI: 2010. Reporting body mass index in the schools: are we missing the mark? pp. 5–7. [Google Scholar]
- 21.Nihiser A, Lee S, Wechsler H, et al. BMI measurement in schools. Pediatrics. 2009;124(Suppl 1):S89–S97. doi: 10.1542/peds.2008-3586L. [DOI] [PubMed] [Google Scholar]
- 22.Soto C, White JH. School health initiatives and childhood obesity: BMI screening and reporting. Policy Polit Nurs Pract. 2010;11(2):108–114. doi: 10.1177/1527154410374218. [DOI] [PubMed] [Google Scholar]
- 23.West DS, Raczynski JM, Phillips MM, Bursac Z, Heath Gauss C, Montgomery BE. Parental recognition of overweight in school-age children. Obesity (Silver Spring) 2008;16(3):630–636. doi: 10.1038/oby.2007.108. [DOI] [PubMed] [Google Scholar]
- 24.Raczynski JM, Thompson J, Phillips M, Ryan K, Cleveland HW. Arkansas Act 1220 of 2003 to reduce childhood obesity: its implementation and impact on child and adolescent body mass index. J Public Health Policy. 2009;30(Suppl 1):S124–S140. doi: 10.1057/jphp.2008.54. [DOI] [PubMed] [Google Scholar]
- 25.Himes J. Challenges of accurately measuring and using BMI and other indicators of obesity in children. Pediatrics. 2009;124(Suppl 1):S3–S22. doi: 10.1542/peds.2008-3586D. [DOI] [PubMed] [Google Scholar]
- 26.Ryan KW. Surveillance, screening, and reporting children’s BMI in a school-based setting: a legal perspective. Pediatrics. 2009;124(Suppl 1):S83–S88. doi: 10.1542/peds.2008-3586K. [DOI] [PubMed] [Google Scholar]
- 27.Linchey J, Madsen KA. [Accessed July 31, 2012];State requirements and recommendations for school-based screenings for body mass index or body composition, 2010. Prev Chronic Dis. 2011 8(5):A101. Available at: http://www.cdc.gov/pcd/issues/2011/sep/11_0035.htm. [PMC free article] [PubMed] [Google Scholar]
- 28.O’Malley PM, Johnston L, Delva J, Bachman J, Schulenberg J. Variation among American secondary school students by school and school characteristics. Am J Prev Med. 2007;33(Suppl 1):S187–S194. doi: 10.1016/j.amepre.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 29.NICHQ Child Obesity Action Network . How much do you know about the childhood obesity epidemic in Oregon? [Accessed August 2, 2012]. Available at: http://www.childhealthdata.org/docs/nsch-docs/oregon04_23_508-pdf.pdf. [Google Scholar]
- 30.Trust for America’s Health . New report: Oregon is 35th most obese state in the nation. [Accessed July 31, 2012]. Available at: http://healthyamericans.org/assets/files/TFAH2011FasInFat10.pdf. [Google Scholar]
- 31.Levi J, Segal LM, St. Laurent R, Kohn D. [Accessed July 31, 2012];F as in Fat: how obesity threatens America’s future 2011. Available at: http://healthyamericans.org/assets/files/TFAH2011FasInFat10.pdf. [Google Scholar]
- 32.Rojas-Burke J. [Accessed August 2, 2012];Oregon kids show decrease in obesity rates. The Oregonian. 2010 May 03; Available at: http://www.oregonlive.com/environment/index.ssf/2010/05/oregon_kids_show_decrease_in_o.html. [Google Scholar]
- 33.Singh G, Kogan MD, van Dyck PC. Changes in state-specific childhood obesity and overweight prevalence in the United States from 2003 to 2007. Arch Pediatr Adolesc Med. 2010;164(7):598–607. doi: 10.1001/archpediatrics.2010.84. [DOI] [PubMed] [Google Scholar]
- 34.Moreno G, Brooks T. [Accessed August 2, 2012];Lane County: BMI data collection project. Lane Coalition For Healthy Active Youth. Available at: http://lchay.org/about/lane-county-data/ [Google Scholar]
- 35.Johnson-Shelton D, Moreno-Black G, Richie D. Measuring children’s activity & food environment in community-based participatory research; Poster presented at the 7th Annual Conference on Diet and Activity Methods; Washington, D.C.. 2009.Jun, [Google Scholar]
- 36.Oregon Department of Education . Oregon Education Data Book 2006-2007. Vol. 2: Detailed tables by school district. [Accessed August 2, 2012]. Available at: http://www.ode.state.or.us/data/collection/databook-vol-2--detailed-tables.pdf. [Google Scholar]
- 37.Lohman TA, Roche F, Martorell R. Anthropometric Standardization Reference Manual. Human Kinetics; Champaign, IL: 1988. [Google Scholar]
- 38.Centers for Disease Control (CDC) About BMI for children and teens. [Accessed August 1, 2012]. 2011. Updated June 2. Available at: http://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html. [Google Scholar]
- 39.Hughes AR, Sherriff A, Lawlor DA, Ness AR, Reilly JJ. Incidence of obesity during childhood and adolescence in a large contemporary cohort. Prev Med. 2011;52(5):300–304. doi: 10.1016/j.ypmed.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen AY, Escarce JJ. [Accessed January 11, 2012];Family structure and childhood obesity, Early Childhood Longitudinal Study—Kindergarten Cohort. Prev Chronic Dis. 2010 7(3):A50. Available at: http://www.cdc.gov/pcd/issues/2010/may/09_0156.htm. [PMC free article] [PubMed] [Google Scholar]