Abstract
BACKGROUND
Models are needed for implementing weight management interventions for adolescents through readily accessible venues. This study evaluated the feasibility and efficacy of a school nurse-delivered intervention in improving diet and activity and reducing BMI among overweight and obese adolescents.
METHODS
Six high schools were randomized to either a 6-session school nurse-delivered counseling intervention utilizing cognitive-behavioral techniques or nurse contact with provision of information. Eighty-four overweight or obese adolescents in grades 9 through 11 completed behavioral and physiological assessments at baseline and 2- and 6-month follow-ups.
RESULTS
At 2 months, intervention participants ate breakfast on more days/week (difference = 1.01 days; 95% CI 0.11, 1.92), and had a lower intake of total sugar (difference = −45.79g; 95% CI −88.34, −3.24) and added sugar (difference = −51.35g; 95% CI −92.45, −10.26) compared to control participants. At 6 months, they were more likely to drink soda ≤ one time/day (OR 4.10: 95% CI 1.19, 16.93) and eat at fast food restaurants ≤ one time/week (OR 4.62: 95% CI 1.10, 23.76) compared to control participants. There were no significant differences in BMI, activity or caloric intake.
CONCLUSION
A brief school nurse-delivered intervention was feasible, acceptable, and improved selected obesogenic behaviors, but not BMI.
Adolescent obesity has increased dramatically over the past several decades, with 34% of adolescents and young adults, ages 12 to 19 currently overweight or obese.1 Overweight or obese youth are at increased risk of becoming obese adults.2 High BMI (Body Mass Index) in adolescents increases the risk of developing adult-onset diseases and health conditions such as type 2 diabetes, insulin resistance and the metabolic syndrome, and cardiovascular disease risk factors such as elevated blood pressure and serum lipids.3 Obese youth also are more likely to suffer depression and low self-esteem.4
Adolescence is marked by the establishment of greater independence, and thus, provides an opportunity to promote lifelong healthy lifestyles that will affect physical and psychosocial outcomes both during adolescence and into adulthood. Yet adolescents have been understudied and underserved in obesity treatment compared to adults and pre-adolescents.5 A recent systematic review for the US Preventive Services Task Force6 found that comprehensive behavioral interventions consistent with expert committee recommendations7 including healthy diet and physical activity counseling and behavioral management training are efficacious for decreasing BMI in youth. However, the mean age was between 11 and 12, and effective interventions were conducted in specialty health care settings such as pediatric obesity referral clinics that have limited reach.6
A tremendous need therefore exists to test models for implementing expert committee recommendations for weight management interventions8 with adolescents through readily accessible venues such as school health clinics. As the primary health professional in the school setting, school nurses are uniquely positioned to deliver weight management interventions. School nurses have the skills and credibility to offer health-related assistance, can provide ongoing support within the school setting, and are easily accessed without parental involvement, without additional cost to the family, and without the student having to leave the school grounds (95% of adolescents attend school).9 The majority of previous school-based studies have focused on obesity prevention and targeted pre-adolescents, and to our knowledge, there have been no randomized controlled school-based trials evaluating interventions targeting overweight or obese adolescents, nor any that have utilized the school nurse to deliver intervention.10 The purpose of the present study was to test the feasibility and efficacy of a school nurse-delivered weight management intervention on BMI, diet, physical activity and sedentary behavior among overweight and obese adolescents.
METHODS
Study Design
A pair-matched cluster-randomized controlled school-based trial was conducted with a convenience sample of 6 public high schools in Massachusetts. School enrollment ranged from approximately 800 to 1500 students (mean enrollment 1055 and 1159 students in control and intervention schools, respectively); approximately half the student populations were female. Race and ethnicity was similar in 4 schools with 90% or more being white, non-Hispanic; one control and one intervention was 19% and 26% Hispanic, respectively. Rates of participation in reduced or free school lunch ranged from 4.6% to 34.1% (mean rates 16.6% and 24.4% in control and intervention schools, respectively). Schools were pair matched on total enrollment, gender, race and ethnicity and percent receiving reduced or free lunch; one from each pair was then randomly assigned to either the school nurse counseling intervention group or the control group. Data were collected from October 2008 to October 2009.
Participants
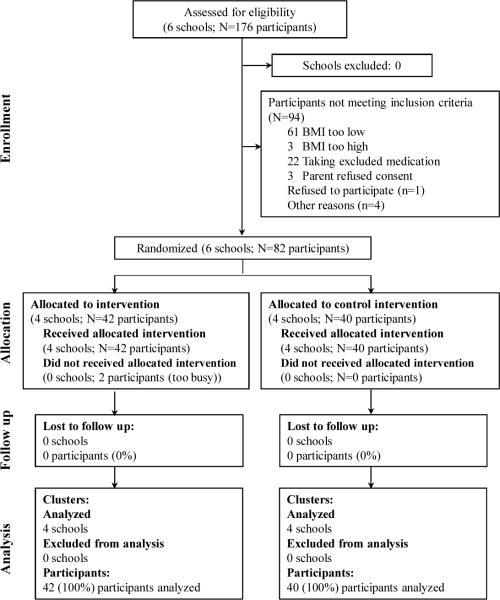
Adolescents in grades 9 through 11 were eligible to participate if they had a BMI ≥ 85th percentile for age and gender, provided assent and had parental consent, and had at least one English-speaking parent. Exclusions included planning to move out of the area; having a medical condition that precluded adherence to the intervention; diagnosis of a serious psychiatric illness; genetic or endocrine cause of obesity; taking a medication associated with weight gain; or weighing ≥ 300 pounds. Exclusions were assessed via a screening form completed by a parent. Students were recruited through school announcements, flyers and posters, and health-related school nurse encounters. There was no racial or gender bias in the recruitment or selection of participants. Participants gave informed assent and had parental consent. Assessments were completed by a research assistant who was not blinded to school condition at baseline and 2 and 6 months following baseline in the school nurse office. All counseling sessions for a student were completed prior to their completing the 2-month survey. A $25 gift certificate was provided at each assessment. The study retained 100% of participants at each follow-up. Figure 1 shows the flow of participants. Eighty-two proceeded to randomization.
Figure 1.
Consort Diagram
Treatment Groups
School nurse-delivered counseling intervention group
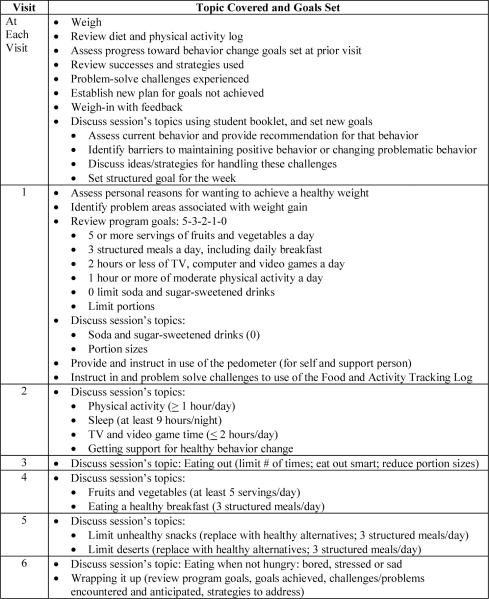
The intervention, “Lookin' Good Feelin' Good”, consisted of 6 one-on-one counseling sessions conducted over 2 months during the school day during non-academic classes in the privacy of the school nurse office. The intervention used the 5-3-2-1-0 approach to support making five key behavior changes (Figure 2). It incorporated expert committee recommendations for the prevention and treatment of child and adolescent overweight and obesity,11 along with the USDA 2005 Dietary Guidelines for Americans12 and recommendations for physical activity.13 The intervention was based on Social Cognitive Theory,14 using cognitive behavioral techniques to facilitate changes in self-management behaviors through health knowledge and the development of positive outcome expectations, self-control and behavioral capacity skills, and self-efficacy. A patient-centered counseling approach allowed school nurses to tailor the intervention to the student's needs. Formative research conducted with focus groups of overweight and obese adolescents, parents, school nurses, and school staff informed development of the intervention protocol and accompanying booklet.15 Such use of formative research to inform intervention design has been found to be valuable in other community-based obesity intervention development in the high school setting.16 School nurses were trained through a daylong group training session which included: (1) a brief didactic presentation on the scope of the problem of adolescent obesity, effects of obesity on adolescents, and expert committee recommendations for the treatment of overweight and obesity in youth; (2) review of the counseling intervention protocol and accompanying student booklet while observing a demonstration of the intervention; and (3) the conduct of role play exercises in which the nurses practiced delivering the intervention protocol, received feedback from study investigators, and processed as a group after each exercise (this portion took the majority of the training time). We have used this training procedure successfully to train school nurses and other health care providers in delivering cognitive-behavioral health behavior change protocols.
Figure 2.
Counseling Intervention Protocol: Lookin' Good Feelin' Good
Control group
Participants in the control schools had 6 one-on-one visits with the school nurse over 2 months to be weighed, review behavior changes, read 6 informational pamphlets on weight management (selected from Journeyworks (http://www.journeyworks.com/) with appropriate content for adolescents), and have questions answered. School nurses received an individual orientation to the protocol and materials.
Instruments
All assessments were conducted by research assistants. Height and weight were measured using standard methodology, wearing light clothing and no shoes. BMI was calculated as weight (kg)/height squared (in meters) for age and gender using the CDC BMI charts. Blood pressure was measured by taking the average of 2 readings with the DINAMAP® PRO 100V2 Monitor. Waist circumference was measured as the average of two measurements midway between the rib cage and superior border of the iliac crest. A Tanita Scale measured body weight and body fat using the leg-to-leg BIA system.
Dietary intake was assessed with a 24-hour dietary recall interview17 using the Interactive Nutrition Data System (NDS, Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN) conducted by phone on one randomly selected day of the week. An 8-item instrument18 was used to assess healthful and unhealthful dietary behaviors targeted by the intervention. This instrument was designed to be completed independently by adolescents and was based on literature review, expert feedback and feasibility testing, which found it to be feasible in public health and primary care settings, similar to the performance of the longer Food Habits Questionnaire and Rate Your Plate.19, 20 Physical activity was assessed by accelerometer using the ActiGraph Model GT1M for a 7-day period; average daily minutes of light, moderate and vigorous activity were calculated using published cut points.21 Sedentary behavior, TV watching and playing computer or video games on an average school day was measured using 2 items from the Youth Risk Behavior Survey (YRBS).22 Sociodemographic variables were assessed by student questionnaires. Self-efficacy or confidence in making weight related behavior changes was assessed with an 11-item questionnaire adapted from the Go Girls study (Cronbach alpha = .90).23 Barriers to eating healthy and exercising was assessed by 5 items adapted from New Moves (Cronbach alpha = .84; test-retest r = .89)24 and 2 items from Motl and colleagues.25
To assess intervention feasibility, defined as the ability of school nurses to deliver the counseling intervention as intended, the following were documented: (1) number of sessions attended by students, and (2) student report of degree to which the school nurse delivered each component of the intervention protocol (program fidelity) as assessed by the Patient Exit Interview Survey and school nurse report of intervention delivery (via a nurse checklist). To assess student acceptability of the counseling intervention, defined as their satisfaction with the intervention, participants rated the perceived helpfulness of the nurse intervention and level of comfort in discussing weight with the school nurse.
School nurses completed a self-administered survey at baseline (Fall) and follow-up (Spring) that documented their demographic information, levels of confidence and effectiveness and barriers and facilitators to assisting obese and overweight adolescents with weight-related behavior changes, as well as for intervention nurses only, their experience with implementing the intervention protocol.
Data Analysis
Baseline means were compared using t-tests or Wilcoxon rank sum tests if distributional assumptions were not met. Fisher's Exact tests were used to compare categorical variables. Continuous outcomes of physiologic measures, physical activity, diet, and psychosocial measures were compared using linear mixed models. Dichotomous outcomes for diet and activity behaviors were compared using exact logistic regression models. Percent of visits on which students rated the nurse as very helpful or felt very comfortable were compared using mixed-effects logistic regression. To account for intra-class correlation, school was included as a random effect in the linear mixed models and mixed-effects logistic regression models. Models were also adjusted for baseline level of the outcome and for any baseline characteristics that differed significantly by group at baseline including participation in reduced or free school lunch program, confidence score, soda consumption, and barriers to exercise score. Physiologic variables were also adjusted for age and gender. All analyses were conducted at the student level and carried out using Stata 10.1. (Stata, version 10.1.). A two-sided p < .05 was considered statistically significant.
RESULTS
Baseline Participant and School Nurse Characteristics
Participants were 82 adolescents with a mean age of 15.8 (SD: 1.02) years who were predominately female (70%) and of white race (77%) (Table 1). Mean BMI was 32 kg/m2 (SD: 5.7); 69.5% (78.6% of intervention vs. 60.0% of controls; p = .09) were obese, with the remainder being overweight. The majority of factors associated with obesity were similar between groups at baseline with the exception of frequency of drinking soda, proportion of students participating in reduced/free lunch, perceived barriers to exercise, and levels of confidence to make changes in healthier eating and food choices. Approximately 60% of students in both intervention and control groups felt very confident that they could lose weight.
Table 1.
Characteristics of Student Participants at Baseline
| Intervention (N=42) | Control (N=40) | p-value | |
|---|---|---|---|
| Mean Age (SD) | 15.9(1.03) | 15.7(1.01) | p < .516 |
| % Female | 64.3 | 75.0 | p < .343 |
| Race | p < .435 | ||
| %White | 73.8 | 80.0 | |
| % Black | 14.3 | 5.0 | |
| % Hispanic Ethnicity | 14.3 | 15.0 | p < 1.000 |
| % participate in reduced or free school lunch | 47.6 | 17.5 | p < .005 |
| % Obese (BMI percentile ≥ 95) | 78.6 | 60.0 | p < .093 |
| Hours watch TV on average school day in past 7 days | p < .981 | ||
| % None | 2.4 | 2.5 | |
| % < 1 hour per day | 28.6 | 25.0 | |
| % 1 hours/day | 7.1 | 10.0 | |
| % 2 hours/day | 23.8 | 22.5 | |
| % 3 or more hours/day | 38.1 | 40.0 | |
| Hours play video or computer games on average school day in past 7 days | p < .308 | ||
| % None | 21.4 | 12.5 | |
| % < 1 hour per day | 14.3 | 22.5 | |
| % 1 hours/day | 23.8 | 10.0 | |
| % 2 hours/day | 14.3 | 20.0 | |
| % 3 or more hours/day | 26.2 | 35.0 | |
| Servings of vegetables in a typical day in past 7 days | p < 1.000 | ||
| % None | 9.5 | 7.5 | |
| % 1–2 servings per day | 50.0 | 50.0 | |
| % 3 or more servings per day | 40.5 | 42.5 | |
| Servings of fruit in a typical day in past 7 days | p < .439 | ||
| % None | 4.8 | 7.5 | |
| % 1–2 servings per day | 42.9 | 55.0 | |
| % 3 or more servings per day | 52.4 | 37.5 | |
| Times drink soda (not diet) in a typical day in past 7 days | p < .020 | ||
| % None | 19.1 | 37.5 | |
| % 1–2 times per day | 66.7 | 35.0 | |
| % 3 or more times per day | 14.3 | 27.50 | |
| Times drink sugar sweetened beverages in a typical day in past 7 days | p < .064 | ||
| % None | 16.7 | 27.5 | |
| % 1–2 times per day | 40.5 | 17.5 | |
| % 3 or more times per day | 42.9 | 55.0 | |
| Times eat food from fast food restaurant in past 7 days | p < .257 | ||
| % None | 31.0 | 47.5 | |
| % 1–2 times | 54.8 | 37.5 | |
| % 3 or more times | 14.3 | 15.0 | |
| Mean # days eat breakfast in past 7 days (SD) (range from 0 to 7) | 3.1(2.4) | 3.7(2.9) | p < .327* |
| Barriers to healthy behaviors (% Strongly Agree to Agree) | |||
| % days too busy to exercise | 16.7 | 42.5 | p < .015 |
| % do not like way body feels when exercise | 23.8 | 37.5 | p < .232 |
| % feel embarrassed or awkward exercising in front of others/public | 26.2 | 47.5 | p < .066 |
| % do not feel safe walking or jogging in neighborhood | 9.5 | 15.0 | p < .514 |
| % eating healthy costs too much | 23.8 | 10.0 | p < .142 |
| % healthy food does not taste good | 21.4 | 5.0 | p < .049 |
| % healthy food is not available to me | 11.9 | 7.5 | p < .713 |
| Barriers to Nutrition Score (range 3 to 12) | 5.57(1.8) | 4.95(1.5) | p < .091 |
| Barriers to Exercise Score (range 4 to 15) | 7.52(1.9) | 8.55(2.4) | p < .036 |
| Confident can do the following (% Very Confident) | |||
| Lose Weight | 59.5 | 57.5 | p <1.000 |
| Eat smaller portions of junk food you like | 40.5 | 40.0 | p <1.000 |
| Not eat junk food when bored or depressed | 52.4 | 32.5 | p < .079 |
| Eat healthy when friends are not | 47.6 | 27.5 | p < .072 |
| Drink fewer sodas or sweetened beverages | 66.7 | 45.0 | p < .074 |
| Eat healthier meals and snacks | 71.4 | 45.0 | p < .024 |
| Eat more fruits and vegetables | 61.9 | 57.5 | p < .822 |
| Get mom, dad or adult living with you to buy healthier food | 73.8 | 67.5 | p < .629 |
| Order healthier choices when you are at a fast food or sit down restaurant | 59.5 | 30.0 | p < .009 |
| Exercise on most days of the week | 52.4 | 45.0 | p < .517 |
| Turn off the television and do something active | 50.0 | 40.0 | p < .384 |
| Mean Confidence Score (SD) (range 15 to 33) | 27.5(3.8) | 25.6(4.1) | p < .023* |
| Mean Minutes Spent in MVPA (from accelerometers) (SD) (range 5.3 to 109.7) | 38.53(22.1) | 27.33(15.5) | p < .012* |
| Mean Total Caloric Intake (SD) (range 585.0 to 3888.3) | 1724.5 (678.3) | 1881.2(695.2) | p < .314 |
| Mean % Calories from Total Fat (SD) (range 14.8 to 52.4) | 30.8(7.1) | 31.0(7.9) | p < .938 |
| Mean % Calories from Saturated fat (SD) (range 3.5 to 23.8) | 11.9(4.3) | 11.3(3.9) | p < .475 |
| Mean Sugar Intake (grams) (SD) (range 1.0 to 131.1) | 109.6(72.7) | 116.4(56.2) | p < .644 |
| Mean % Calories from Carbohydrates (SD) (range 33.3 to 70.1) | 52.8(8.5) | 53.0(9.5) | p < .946 |
| Mean Glycemic Load Glucose (SD) (range 37.7 to 342.9) | 142.4(70.1) | 147.9(57.0) | p < .260* |
| Mean BMI (SD) (range 24.3 to 49.1) | 32.8(5.9) | 31.2(5.3) | p < .161* |
| Mean % Body Fat (SD) (range 13.1 to 57.5) | 37.9(9.3) | 38.0(7.9) | p < .991 |
| Mean BMI percentile (SD) (range 84.1 to 99.7) | 96.4(3.4) | 95.3(3.8) | p < .188* |
| Mean Waist Circumference (SD) (range 72.3 to 132.1) | 99.7(13.8) | 98.2(11.6) | p < .606 |
| Mean Systolic Blood Pressure (SD) (range 95 to 145) | 117.7(10.0) | 116.3(9.9) | p < .508 |
| Mean Diastolic Blood Pressure (SD) (range 51 to 88) | 69.0(8.2) | 70.3(7.2) | p < .425 |
p value derived from Rank-Sum Test.
Seven school nurses (4 intervention and 3 control nurses) participated in the study; one intervention school had 2 nurses due to staff turnover. All nurses were female; mean age was 46.2 (SD=14.1) and 50.1 (SD=11.8) years in intervention and control schools respectively. The mean number of years working as a school nurse in any school was somewhat higher for nurses in intervention compared to control schools (10.8 years (SD=8.7) vs. 8.3 years (SD=2.9), respectively); whereas the mean number of years working in their current school was somewhat higher for nurses in control compared to intervention schools (5.0 years (SD=3.6) vs. 4.0 years (SD=4.6), respectively). None of the nurses reported having received prior training on how to counsel overweight or obese students to improve diet and physical activity to reduce their BMI.
Intervention Effects at 2 and 6 Months
Students in the intervention compared to control schools showed small, more favorable changes in various physiologic measures including waist circumference and systolic blood pressure at 6 months (Table 2). However, there were no statistically significant differences in anthropometric variables or blood pressure between groups at 2 or 6 months.
Table 2.
Intervention Effect on Physiologic Outcomes
| 2 months | 6 months | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline Mean (SD) | Unadjusted Mean Change (SD) | Adjusted Mean Change* (95% CI) | Adjusted Mean Difference in Change* (95% CI) | p-value* | Unadjusted Mean Change (SD) | Adjusted Mean Change* (95% CI) | Adjusted Mean Difference in Change* (95% CI) | p-value* | |
| BMI | p < .819 | p < .676 | |||||||
| Control | 31.24 (5.33) | 0.14 (1.14) | 0.12 (−0.37, 0.61) | 0.26 (1.59) | 0.23 (−0.46, 0.91) | ||||
| Intervention | 32.78 (5.91) | 0.01 (1.64) | 0.03 (−0.45, 0.51) | −0.09 (−0.82, 0.65) | −0.01 (1.98) | 0.01 (−0.66, 0.68) | −0.22 (−1.23, 0.80) | ||
| BMIZ | p < .781 | p < .736 | |||||||
| Control | 1.81 (0.41) | 0.01 (0.11) | 0.01 (−0.04, 0.07) | 0.01 (0.17) | 0.01 (−0.06, 0.08) | ||||
| Intervention | 1.95 (0.44) | 0.00 (0.17) | 0.00 (−0.05, 0.05) | −0.01 (−0.09, 0.07) | 0.00 (0.21) | 0.00 (−0.07, 0.07) | −0.02 (−0.12, 0.09) | ||
| Waist Circumference(cm) | p < .503 | N=81 | p < .504 | ||||||
| Control | 98.27 (11.56) | 1.33 (4.14) | 1.58 (−0.13, 3.29) | 0.70 (5.22) | 0.88 (−1.30, 3.06) | ||||
| Intervention | 99.73 (13.79) | 0.98 (4.45) | 0.72 (−0.96, 2.40) | −0.86 (−3.38, 1.66) | −0.05 (6.59) | −0.22 (−2.35, 1.91) | −1.10 (−4.34, 2.13) | ||
| % Body Fat | p < .733 | p < .391 | |||||||
| Control | 37.95 (7.86) | −0.44 (2.64) | −0.48 (−1.67, 0.71) | −1.02 (3.54) | −1.17 (−2.74, 0.40) | ||||
| Intervention | 37.93 (9.32) | −0.82 (4.68) | −0.79 (−1.96, 0.37) | −0.31 (−2.09, 1.47) | −0.26 (5.91) | −0.14 (−1.67, 1.39) | 1.03 (−1.32,3.37) | ||
| Systolic BP | p < .314 | p < .272 | |||||||
| Control | 116.28 (9.90) | −2.33 (10.49) | −2.43 (−5.74, 0.87) | 4.16 (12.30) | 4.80 (1.31, 8.29) | ||||
| Intervention | 117.74 (10.00) | −0.01 (13.09) | 0.11 (−3.11, 3.32) | 2.54 (−2.41, 7.48) | 2.49 (12.61) | 1.88 (−1.53, 5.28) | −2.93 (−8.14, 2.29) | ||
| Diastolic BP | p < .958 | p < .622 | |||||||
| Control | 70.34 (7.24) | 0.66 (8.03) | 1.12 (−2.16, 4.40) | −1.49 (10.09) | −0.64 (−3.26, 1.98) | ||||
| Intervention | 68.96 (8.20) | 1.25 (8.57) | 0.99 (−2.24, 4.22) | −0.13 (−4.93, 4.67) | 1.12 (9.88) | 0.35 (−2.21, 2.90) | 0.98 (−2.93, 4.90) | ||
Adjusted for school, age, gender, baseline measurement and the following baseline variables: participation in free lunch program, confidence score, soda consumption, barriers to exercise score.
The intervention had a positive impact on some nutrition and lifestyle factors. Dietary composition showed significant differences initially (Table 3). On average, students in intervention compared to control schools consumed a significantly lower amount of total sugar (difference = −45.79g/day; 95% CI −88.34, −3.24) and added sugar (difference = −51.35g/day; 95% CI −92.45, −10.26) at 2 months; but this was not maintained at 6 months. Caloric intake and calories from fat did not change significantly between groups. Students in intervention compared to control schools ate breakfast on significantly more days per week at 2 months, adjusted mean 4.66 days vs. 3.65 days, respectively (adjusted mean difference 1.01 days; 95% CI 0.11,1.92), but not at 6 months. The intervention had no effect on time spent in moderate to vigorous physical activity (MVPA).
Table 3.
Intervention Effect on Physical Activity, Diet and Lifestyle Factors
| 2 months | 6 months | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline Mean (SD) | Unadjusted Mean Change (SD) | Adjusted Mean Change* (95% CI) | Adjusted Mean Difference in Change* (95% CI) | p-value* | Unadjusted Mean Change (SD) | Adjusted Mean Change* (95% CI) | Adjusted Mean Difference in Change* (95% CI) | p-value* | |
| Minutes/Day in MVPA | p < .509 | p < .910 | |||||||
| Control | 27.33 (15.45) | 2.29 (16.35) | 0.55 (−6.84, 7.95) | 3.96 (13.97) | 0.22 (−4.26, 4.70) | ||||
| Intervention | 38.53 (22.08) | 1.78 (16.43) | 4.33 (−3.53, 12.18) | 3.77 (−7.43, 14.98) | −2.28 (13.70) | 0.65 (−4.77, 6.08) | 0.43 (−7.11, 7.98) | ||
| Days eat breakfast in past 7 days | p < .028 | p < .605 | |||||||
| Control | 3.73(2.88) | 0.28 (2.16) | 0.25 (−0.35, 0.85) | −0.13 (2.31) | −0.01 (−0.79, 0.77) | ||||
| Intervention | 3.10(2.36) | 1.24 (1.87) | 1.26 (0.68, 1.85) | 1.01 (0.11,1.92) | 0.40 (2.52) | 0.30 (−0.46, 1.05) | 0.31 (−0.86, 1.47) | ||
| Total Calories/Day | p < .240 | N=76 | p < .112 | ||||||
| Control | 1881.18 (695.15) | −76.11 (798.31) | 23.50 (−256.05, 303.06) | −15.67 (696.48) | 31.59 (−156.17, 219.35) | ||||
| Intervention | 1724.45 (678.30) | −120.28 (834.89) | −232.43 (−519.41, 54.55) | −255.94 (−682.92, 171.05) | −150.91 (632.55) | −202.89 (−396.34, −9.43) | −234.5 (−524.0, 55.0) | ||
| % Calories Total Fat | p < .635 | N=76 | p < .992 | ||||||
| Control | 30.97 (7.92) | 1.69 (10.26) | 1.62 (−1.43, 4.66) | 1.69 (14.51) | 1.19 (−1.92, 4.30) | ||||
| Intervention | 30.84 (7.15) | 0.48 (12.47) | 0.48 (−2.66, 3.61) | −1.13 (−5.84, 3.56) | 0.86 (9.75) | 1.21 (−1.99, 4.41) | 0.02 (−4.76, 4.81) | ||
| % Calories Saturated Fat | p < .700 | N=76 | p < .293 | ||||||
| Control | 11.26 (3.86) | 0.29 (5.09) | −0.31 (−1.61, 0.99) | −0.51 (6.17) | −1.21 (−2.78, 0.36) | ||||
| Intervention | 11.92 (4.28) | −1.36 (6.22) | −0.71 (−2.04, 0.63) | −0.39 (−2.40, 1.61) | −0.57 (5.62) | 0.06 (−1.54, 1.66) | 1.27 (−1.10,3.64) | ||
| Total Sugar (g/day) | p < .035 | N=74 | p < .241 | ||||||
| Control | 116.44 (56.17) | 0.65 (103.06) | 12.45 (−15.03, 39.92) | −19.94 (66.60) | −11.37 (−30.71, 7.96) | ||||
| Intervention | 109.58 (72.66) | −21.75 (80.75) | −33.34 (−61.70, −4.98) | −45.79 (−88.34, −3.24) | −19.81 (79.89) | −29.15 (−49.08, −9.22) | −17.78 (−47.48, 11.92) | ||
| Added Sugar (g/day) | p < .014 | N=73 | p < .469 | ||||||
| Control | 79.00 (55.75) | 13.82 (100.13) | 25.20 (−1.39, 51.78) | −14.44 (72.68) | −7.20 (−27.59, 13.19) | ||||
| Intervention | 75.67 (62.93) | −16.96 (77.74) | −26.16 (−53.57, 1.26) | −51.35 (−92.45, −10.26) | −9.79 (78.23) | −18.87 (−40.17, 2.43) | −11.67 (−43.23, 19.89) | ||
| Glycemic Load | p < .093 | N=72 | p < .352 | ||||||
| Control | 147.93 (57.05) | −6.76 (72.15) | 1.09 (−21.05, 23.23) | −15.15 (53.10) | −11.08 (−27.36, 5.20) | ||||
| Intervention | 142.41 (70.06) | −22.46 (78.88) | −28.98 (−51.18, −5.06) | −29.21 (−63.33, 4.92) | −17.73 (68.30) | −22.93 (−39.68, −6.18) | −11.85 (−36.83, 13.12) | ||
Adjusted for school, baseline participation in free lunch program, confidence score, soda consumption, barriers to exercise score, and baseline levels of each outcome variable.
In addition, students in intervention compared to control schools were over 4 times more likely to drink soda 1 or fewer times per day (87.2% vs. 62.1%, respectively; adjusted OR 4.20; 95% CI 1.19,16.93) at 6 months. The percent of students who reported eating at fast food restaurants ≤ 1 time per week was significantly greater in intervention compared to control schools (86.2% vs. 57.4%, respectively, adjusted OR 4.62: 95% CI 1.10, 23.76) at 6 months. However, comparison of the two conditions by each of the component parts of the 5-3-2-1-0 approach targeted in the intervention indicated no differences in the number of participants reporting consuming 5 servings of fruits and vegetables per day, eating 3 meals per day, getting less than 2 hours of screen time per day, being active for at least an hour a day on at least 5 days per week, or consuming no soda/sugary drinks (Table 4).
Table 4.
Intervention Effect on the 5-3-2-1-0 Intervention Targets
| Baseline | 2 Months | 6 Months | ||||
|---|---|---|---|---|---|---|
| Percent | Percent | OR (95% CI) p-value | Percent | OR (95% CI) p-value | ||
| 5 Fruits and Vegetables per Day | Control | 50.00 | 75.00 | 0.25(0.04, 1.29) | 62.50 | 0.76(0.23, 2.47) |
| Intervention | 54.76 | 66.67 | p < .115 | 57.14 | p < .797 | |
| N=78 | N=76 | |||||
| 3 Meals per Day (Including Breakfast) | Control | 65.00 | 50.00 | 1.54(0.51, 4.89) | 48.72 | 1.72(0.54, 5.64) |
| Intervention | 58.97 | 58.97 | p < .548 | 62.16 | p < .436 | |
| Less than 2 Hours of TV or Computer Time per Day | Control | 27.50 | 22.50 | 2.07(0.35, 15.51) | 25.00 | 2.97(0.66, 11.31) |
| Intervention | 28.57 | 38.10 | p < .584 | 50.00 | p < .091 | |
| Active 1 Hour per Day At Least 5 Days per Week | Control | 30.00 | 37.50 | 0.92(0.27,3.13) | 37.50 | 1.57(0.55, 4.52) |
| Intervention | 30.95 | 40.48 | p < 1.000 | 52.38 | p < .480 | |
| N=81 | ||||||
| No Soda or Sugary Drinks. | Control | 12.50 | 10.26 | 3.34(0.52, 37.85) | 2.50 | 12.33(0.58, 1251.77) |
| Intervention | 7.14 | 19.05 | p < .283 | 9.52 | p < .153 | |
ORs are from models adjusted for baseline participation in the free lunch program, confidence score, soda consumption, barriers to exercise score, and baseline evels of each outcome variable. Percentages are actual percentages at each time point. N used to compute OR is equal to 82 unless otherwise specified.
Treatment Fidelity and Acceptability
School nurses reported that the majority of students attended one or more visits (81% vs. 93% of students attended all 6 visits in intervention vs. control schools, respectively). Mean time to conduct each session ranged from 18 to 29 minutes in intervention schools and 8.5 to 9 minutes in control schools. Students in the counseling intervention reported that nurses delivered the intervention with a high level of fidelity to the protocol (on average, 97% of protocol items were covered at each visit). Students receiving the counseling intervention reported that the school nurse was very helpful in their learning how to eat healthy and be physically active, and this was significantly higher in the intervention compared to control schools (98% vs. 71% of visits, respectively; p = .003). Students who received the counseling intervention more often reported feeling very comfortable in discussing their weight-related behaviors with the nurse (88% vs. 62% of visits in intervention vs. control schools respectively; p = .01).
School nurses in the intervention schools reported generally high levels of confidence and effectiveness in their ability to counsel obese adolescents to improve diet and physical activity to reduce their BMI (mean scores 3.50 (0.58) on a 4 point response scale ranging from 1=not at all to 4=very). Nurses did not report needing to work extra hours in order to fit the intervention into their schedule; although two nurses reported hiring additional staff to cover while they delivered the intervention. Nurses did not report that lack of time was a barrier to assisting adolescents in making changes in their diet and physical activity (mean score 2.00 (SD 0.82) on a 4 point response scale ranging from 1=strongly disagree to 4=strongly agree). The majority of nurses (75%) found that it was not at all difficult to incorporate the intervention in their daily work. All nurses found the intervention protocol and materials very helpful in talking to adolescents about improving diet and physical activity and 75% reported that the adolescents were very receptive to the intervention.
DISCUSSION
A brief weight management counseling intervention was feasible for school nurses to deliver within the school health office setting and acceptable to overweight and obese adolescents. School nurses were able to deliver the 6-session treatment protocol with high fidelity and with high levels of student participation. The counseling intervention produced a number of positive changes in adolescents' self-reported obesogenic behaviors, including eating breakfast on more days per week, drinking soda ≤ 1 time per day, and eating at fast food restaurants ≤ 1 time per week. However, screen time, time spent in MVPA, and physiologic variables were not significantly affected during this short term and low intensity intervention.
Other pediatric weight management programs have found reductions in sedentary behaviors when targeted as part of the intervention, in contrast to the findings of the present study. Results of a meta-analysis of interventions targeting screen time reduction found that such interventions had a statistically significant albeit small effect in children, including adolescents.26 It appears the problem-solving conducted as part of the counseling intervention was not more effective in helping teens reduce their screen time than provision of written information, as adolescents in both groups received information about the recommended amount of screen time. This may be related to students being unable to effectively strategize to overcome barriers to physical activity, which might serve as a replacement for time spent in sedentary activity.
It is possible that the reduction in soda intake observed in our study could explain the reduction in total and added sugar, as there are on average 16 teaspoons of sugar in a 20-ounce soda. Whereas one clinical trial reported positive changes in sugar intake among obese adolescent patients in a multi-component clinic based intervention,27 no previous behavioral intervention has shown positive changes in soda consumption or breakfast consumption among overweight or obese teens. Again, teens in the control group received recommendations regarding these dietary factors and there were no differences in change in knowledge between the 2 groups. This suggests adolescents in both groups were aware of the recommendations, but counseling by the school nurse was more effective in assisting teens in making these key dietary changes. Although many of these changes were short-term, these findings suggest the potential of a more intensive intervention to have a longer-lasting impact on these mediators of BMI change. No changes were found in physical activity, suggesting that counseling alone may not be sufficient to produce changes in this behavior.
Though not statistically significant, students in the counseling intervention schools experienced modest favorable improvements in their BMI when compared to students in the control schools. This finding is consistent with a review of behavioral intervention trials6 that found weight management programs produced modest, but often non significant reductions in BMI and/or adiposity in overweight and obese youth. The largest intervention effects were found in more comprehensive, moderate- to high-intensity weight management programs (26–75 to over 75 hours of contact time) that included a structured exercise program and were conducted within specialty clinics. Less comprehensive and intensive programs, similar to our counseling intervention, showed more mixed results.6 The promising results in weight-related behavior change and trend toward modest favorable anthropometric outcomes suggests the potential for a more intensive school nurse intervention to have an impact on BMI.
Significant strengths of the current study are the randomized design, relatively large sample of students, and very high retention rate (98%). In addition, our comparison group controlled for contact with the school nurse and access to information about recommended dietary, physical activity and sedentary behaviors for weight management. Additional strengths include the carefully designed intervention based on current recommendations tailored for adolescents and extensive formative work, and use of real-world providers to deliver the intervention.
Limitations
Although both conditions involved 6 one-on-one sessions with the school nurse, variable student contact time with the nurse between school conditions could have accounted for some of the positive impact of the intervention. In addition, whereas the strong control condition was a strength in some regards, it also can be viewed as a limitation as it served in many ways as another intervention. The intensity of the control intervention may have made it difficult to identify a statistically significant improvement from the intervention condition. Had we tested the intervention against usual care for the school health clinic, which may be only BMI screening and parent notification of results, we may have been able to see statistically significant differences in improvements in anthropometric measures and/or behavioral measures. Another limitation is reliance on self-report of behavior change inherent in weight management trials, which may have affected the reliability of student responses. Although we used a cluster randomized design, the small number of schools located in one geographical area limits the generalizability of our findings.
Conclusions
This study found that a school nurse-delivered counseling intervention for overweight and obese adolescents is feasible for school nurses to deliver, acceptable to teens, and improves selected self-reported obesogenic behaviors, but not BMI. The delivery of weight management counseling to overweight and obese adolescents by school nurses has tremendous potential, leveraging existing resources by capitalizing on the placement of skilled health care providers in the school setting and reducing barriers to adolescents seeking and receiving treatment. Recent findings suggest that fairly high-intensity interventions providing substantial contact time are needed to effect weight loss.6 Future research should explore expanding the counseling intervention to include additional visits extended over a longer period of time, as well as opportunities to engage in physical activity within the school setting to enhance the impact of this innovative treatment approach.
IMPLICATIONS FOR SCHOOL HEALTH
School nurses in the school health setting are in an excellent position to tackle the growing problem of adolescent obesity, given the well-documented need for feasible, cost-effective behavioral interventions that can be delivered in readily-accessible settings. School nurses are well-positioned to contribute to this effort as they have the skills to provide counseling to support weight-related behavior change, and are easily accessible to adolescents without transportation or cost. Most adolescents in the US (95%) attend school;9 approximately half of high schools have a full-time registered nurse and another one third have a part-time nurse.28 Importantly, it is the position of the National Association of School Nurses (NASN) that “school nurses have the knowledge and expertise to promote the prevention of overweight and obesity and address the needs of overweight and obese youth in schools” and it is their role to “assist students who are overweight and obese to obtain a healthy lifestyle. School nurses are in the prime position to influence the behavior of children and adolescents in developing good-decision-making skills related to nutrition and physical activity to develop and achieve healthy lifestyles.”29
The leveraging of existing infrastructure by capitalizing on the placement of skilled health care providers in the highly accessible school setting has tremendous public health significance compared to specialty clinics, which have limited reach due to access and the expense of intensive resources required, including the cost to the family in terms of transportation, copayments and time. The present study demonstrated that a weight management counseling intervention was feasible for school nurses to deliver with high fidelity in the school health setting and was acceptable to overweight and obese adolescents. This finding, along with promising results in weight-related behavior change and a trend toward modest favorable anthropometric outcomes, suggests the potential for a more intensive school nurse intervention to have an impact on BMI. If ultimately found to be effective, a case can be made for increasing the availability of school nurses to deliver these services and potentially be recognized by the healthcare delivery system as being effective and reimbursable. In addition, additional resources could be brought to bear in schools (for example, temporary nurses to cover the clinic) to free up the school nurses to deliver this intervention to have a public health impact. Also, a broader recruitment process could be instituted in the schools to reach a greater proportion of overweight and obese students for maximal public health impact. Should an expanded and more comprehensive version of the intervention tested in this study be found to be effective in helping adolescents reduce their BMI, there would be tremendous implications for the ability of school health to contribute to the reduction of adolescent obesity in a cost effective manner.
Human Subject Approval Statement
The University of Massachusetts Medical School (UMMS) Human Subjects Institutional Review Board approved the study protocol (Docket #H12681).
ACKNOWLEDGEMENTS
Support for this research (#R21 HD053371) came from the National Institute of Child Health and Human Development. The sponsor had no role in the design, data collection, management, analysis, or interpretation of the study, nor in the preparation, review, or approval of the manuscript. We thank the research assistants who collected the data, the schools and school nurses who graciously took part in this study, and the youth who participated.
REFERENCES
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.The NS, Suchindran C, North KE, Popkin BM, Gordon-Larsen P. Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010;304(18):2042–2047. doi: 10.1001/jama.2010.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond) 2010;35(7):891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 4.Puder JJ, Munsch S. Psychological correlates of childhood obesity. Int J Obes (Lond) 2010;34(Suppl 2):S37–43. doi: 10.1038/ijo.2010.238. [DOI] [PubMed] [Google Scholar]
- 5.Whitlock EA, O'Connor EP, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management programs in children and adolescents. Evid Rep Technol Assess (Full Rep) 2008;(170):1–308. [PMC free article] [PubMed] [Google Scholar]
- 6.Whitlock EP, O'Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010;125(2):e396–e418. doi: 10.1542/peds.2009-1955. [DOI] [PubMed] [Google Scholar]
- 7.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 8.Krebs NF, Jacobson MS. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112(2):424–430. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]
- 9.US Department of Commerce [Accessed October 9, 2011];Historical statistics of the United States Colonial Times to 1970; current population reports, serios P-20, various years; and current population survey, October, 1970 through 2008 (This table was prepared August 2009) Available at: http://nces.ed.gov/programs/digest/d09/tables/dt09_007.asp.
- 10.Khambalia AZ, Dickinson S, Hardy LL, Gill T, Baur LA. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes Rev. 2011;13(3):214–233. doi: 10.1111/j.1467-789X.2011.00947.x. [DOI] [PubMed] [Google Scholar]
- 11.American Academy of Pediatrics [Accessed August 1, 2011];Prevention and treatment of childhood overweight and obesity. Available at: http://www.aap.org/obesity/policystatements.html.
- 12.US Department of Health and Human Services [Accessed January 2005];Dietary Guidelines for Americans. Available at: http://www.health.gov/dietaryguidelines/dga2005/document/default.htm.
- 13.Carrel AL, Bernhardt DT. Exercise prescription for the prevention of obesity in adolescents. Curr Sports Med Rep. 2004;3(6):330–336. doi: 10.1007/s11932-996-0008-1. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Social Foundation of Thought and Action: A Social Cognitive Theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 15.Gellar L, Druker S, Osganian SK, Gapinski MA, Lapelle N, Pbert L. Exploratory research to design a school nurse-delivered intervention to treat adolescent overweight and obesity. J Nutr Educ Behav. 2012;44(1):46–54. doi: 10.1016/j.jneb.2011.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kong AS, Farnsworth S, Canaca JA, Harris A, Palley G, Sussman AL. An adaptive community-based participatory approach to formative assessment with high schools for obesity intervention. J Sch Health. 2012;82(3):147–154. doi: 10.1111/j.1746-1561.2011.00678.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lytle LA, Nichaman MZ, Obarzanek E, Glovsky E, Montgomery D, Nicklas T, et al. Validation of 24-hour recalls assisted by food records in third-grade children. The CATCH Collaborative Group. J Am Diet Assoc. 1993;93(12):1431–1436. doi: 10.1016/0002-8223(93)92247-u. [DOI] [PubMed] [Google Scholar]
- 18.Glasgow RE, Ory MG, Klesges LM, Cifuentes M, Fernald DH, Green LA. Practical and relevant self-report measures of patient health behaviors for primary care research. Ann Fam Med. 2005;3(1):73–81. doi: 10.1370/afm.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gans KM, Hixson ML, Eaton CB, Lasater TM. Rate your plate: A dietary assessment and educational tool for blood cholesterol control. Nutr Clin Care. 2000;3(3):163–169. [Google Scholar]
- 20.Glasgow RE, Perry JD, Toobert DJ, Hollis JF. Brief assessments of dietary behavior in field settings. Addict Behav. 1996;21(2):239–247. doi: 10.1016/0306-4603(95)00056-9. [DOI] [PubMed] [Google Scholar]
- 21.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 Suppl):S531–543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 22.Grunbaum JA, Kann L, Kinchen SA, Williams B, Ross JG, Lowry R, et al. Youth risk behavior surveillance--United States, 2001. MMWR Surveill Summ. 2002;51(4):1–62. [PubMed] [Google Scholar]
- 23.Resnicow K, Taylor R, Baskin M, McCarty F. Results of go girls: a weight control program for overweight African-American adolescent females. Obes Res. 2005;13(10):1739–1748. doi: 10.1038/oby.2005.212. [DOI] [PubMed] [Google Scholar]
- 24.Neumark-Sztainer D, Story M, Hannan PJ, Rex J. New Moves: a school-based obesity prevention program for adolescent girls. Prev Med. 2003;37(1):41–51. doi: 10.1016/s0091-7435(03)00057-4. [DOI] [PubMed] [Google Scholar]
- 25.Motl RW, Dishman RK, Ward DS, Saunders RP, Dowda M, Felton G, et al. Perceived physical environment and physical activity across one year among adolescent girls: self-efficacy as a possible mediator? J Adolesc Health. 2005;37(5):403–408. doi: 10.1016/j.jadohealth.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 26.Maniccia DM, Davison KK, Marshall SJ, Manganello JA, Dennison BA. A meta-analysis of interventions that target children's screen time for reduction. Pediatrics. 2011;128(7):e193–210. doi: 10.1542/peds.2010-2353. [DOI] [PubMed] [Google Scholar]
- 27.Bean MK, Mazzeo SE, Stern M, Evans RK, Bryan D, Ning Y, et al. Six-month dietary changes in ethnically diverse, obese adolescents participating in a multidisciplinary weight management program. Clin Pediatr (Phila) 2011;50(5):408–416. doi: 10.1177/0009922810393497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Association of School Nurses [Accessed April 27, 2012];School nursing in the United States quantitative study: Burkhardt Research Services. Available at: http://www.nasn.ore/portals/0/2007/_Burkhardt_Report.pdf.
- 29.National Association of School Nurses [Accessed April 27, 2012];Overweight and obesity in youth in schools - The role of the school nurse. Available at: http://www.nasn.org/PolicyAdvocacy/PositionPapersandReports/NASNPositionStatementsFullView/tabid/462/ArticleId/39/Overweight-and-Obesity-in-Youth-in-Schools-The-Role-of-the-School-Nurse-Revised-2011.