Abstract
The pharmacodynamics of propranolol were studied in 12 cirrhotic Malay patients. Fifteen healthy Malay volunteers were selected and several clinical parameters were obtained. The effects of three doses of propranolol in reducing the heart rate (HR) of these patients were observed to be significantly different. These differences were seen at dosing of 10 mg vs 20 mg and 10 mg vs 30 mg (P<0.001 and P<0.01, respectively). However, no significant difference was seen for doses between 20 mg vs 30 mg. At 20 mg the reduction in HR is more pronounced than the effect seen with the other two doses. The effects of propranolol in reducing Vmax and Vmean of portal vein blood flow were found to be not significant at doses of 10 mg vs 30 mg, but between 10 mg vs 20 mg and 20 mg vs 30 mg there was significant difference (P<0.05 and P<0.01, respectively). Reduction of Vmax of more than 10% of baseline was achieved at doses of 10 mg and 20 mg. However, at a dose of 20 mg a more significant reduction was observed than at a dose of 10 mg. Dose-concentration-effect relationship was seen to be significantly different between HR reduction and propranolol concentration of the three steady-state levels (P<0.001). Similar results were obtained with Vmax and Vmean. The Vmax was found to be a reliable parameter for the assessment of therapeutic effect of the drugs in conferring changes in portal haemodynamics of liver cirrhotic patients. Further, Child-Pugh score is thought to be an important supporting factor in evaluating prognosis. The results of this pharmacodynamics studies suggest that the optimal dose of propranolol may be 20 mg propranolol thrice daily for cirrhotic Malay patients.
Keywords: pharmacodynamics, propranolol, post-hepatitic cirrhosis, portal hypertension
Introduction
Propranolol has been used to control the onset and recurrence of variceal haemorrhage in cirrhotic patients (1–8). It can reduce blood flow and hepatic venous gradient (HVPG) in the portal system without influencing renal function (9–10) and brain blood flow (11). In addition, propranolol also reduces variceal pressure (7), pulse rate and cardiac output without influencing arterial pressure in patients with portal hypertension (10). The dose of propranolol required to control variceal bleeding is normally higher in Caucasians than in Malays (4). In South East Asia, including Malaysia, liver cirrhosis is related to post hepatitis B infection (12–17) while in Caucasians, it is mostly caused by chronic intake of alcohol (18–23). The aim of the present study is to determine the optimal dose of propranolol required to control and prevent variceal haemorrhage in (post-hepatitis infected) cirrhotic patients and to characterise the normal values of the relevant clinical parameters among healthy Malay volunteers.
Material and method
Subjects
The study group comprised of 12 cirrhotic patients (39–62 years of age, mean weight 56.4 ± 6.5 kg) and 15 healthy volunteer subjects (41 – 62 years of age, mean weight 60.83 ± 9.51 kg) (Table 1). All subjects gave informed consent to the study. This study was approved by the Ethical Committee, Universiti Sains Malaysia. The cirrhotic patients were given randomly selected daily doses of propranolol (10 mg, 20 mg and 30 mg three times a day) for 1 week. Healthy volunteers acted as the control group. Their selection were based on comparable normal values assessed by selected clinical parameters. All subjects were fasted overnight prior to the clinical parameters assessment.
Table 1.
Healthy subjects & cirrhotic Malay patients characteristics (X̄ ± SD)
| Clinical Parameters | Healthy subjects | Cirrbotic patients | Sig |
|---|---|---|---|
| Sex | 7M & 8F | 10M & 2F | |
| Age (years) | 46.00 6.04 | 49.83 9.17 | NS |
| Body weight (kg) | 60.83 9.51 | 56.42 6.51 | NS |
| Height (cm) | 154.50 9.65 | 157.33 6.78 | NS |
| NS (Non significant) |
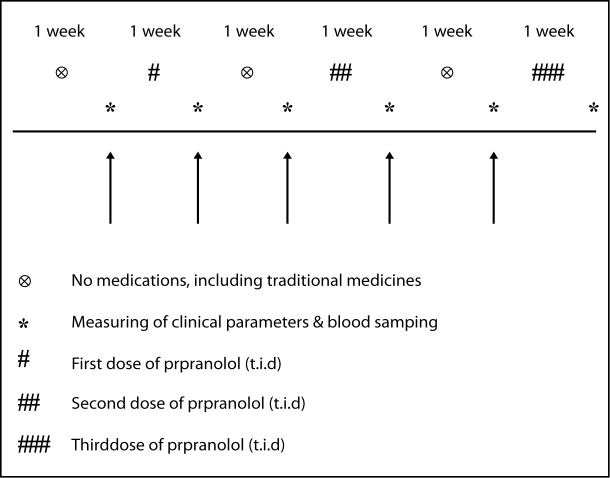
Study protocol
Cirrhotic patients were taken off the medication for 1 week prior to the study. Baseline clinical parameters of pulse rate, mean arterial pressure (MAP), maximum blood flow velocity (Vmax), mean blood flow velocity (Vmean) and diameter of portal vein (D), portal flow volume (PFV) and congestion index (CI) of the portal system were assessed. Patients were given the first dose of propranolol for 1 week and the pharmacodynamic parameters at steady-state levels were taken 3 hours post dose. This procedure was repeated in every patient for all the 3 randomly chosen doses with a washout period of a 1 week between the doses (Fig 1). The baseline (pre-dose) and steady-state clinical parameters of the 3 randomly chosen doses were statistically compared.
Figure 1.
Study protocol of different doses of propranolol in cirrhotic Malay patients
Analysis of propranolol
Propranolol analysis was done according to the Carr’s method with some modifications (24). Oxprenolol acted as an internal standard (I.S.). Blood samples for plasma propranolol assays were collected, centrifuged and frozen at −20°C until analysis. Plasma (1 ml), and 75 μl oxprenolol (100 μg/ml), were placed in 10 ml capped plastic tubes. To each tube, 100 μl H2O and 50 μl5NNaOHwere added and vortexed for 30 seconds, extracted with 3 ml of extraction solvent (1.5 ml isoamyl alcohol + 98.5 ml n-heptane) and shaken on a rotater for 20 minutes, followed by centrifugation (3000 rpm) for 15 minutes. The organic phase was transferred by aspiration to clean glass tubes. The extraction procedures were repeated with the remaining sample. A gentle flow of the nitrogen gas was used to dry the organic phase. The residue was reconstituted in 100 μl methanol by vortexing for 20 seconds and 20 μl of the samples was injected directly onto Lichrosorb C18 HPLC (12.5 cm) column with detection at 295 nm. The pH of the mobile phase (water-methanol-acetonitrile-acetic acid-triethylamine; 160 ml : 80 ml : 70 ml : 2.5 ml : 125 ml) was adjusted to pH 3.4 using 1N NaOH before the addition of triethylamine. The mobile phase flow rate was 0.5 ml/min. The HPLC system comprised of a liquid chromatograph pump (Waters TM 610), system controller (Waters TM 600), a variable wavelength UV detector (Waters TM 486), manual injector (Rheodyne 7125) and integrator (Hewlett packard 3390A). The retention times of oxprenolol and propranolol were 6.31 and 8.80 minutes respectively. With this procedure the limit of detection for propranolol was 9 ng/ml, the recovery from plasma was greater than 90%. The intra-day and inter-day coefficient of variation were 6.41 % and 3.03%, respectively over concentration range of 15 – 180 ng/ml.
Doppler measurement of diameter (D) and maximum velocity (Vmax) of blood flow in portal vein
Doppler examination was carried out with SONOS 2000 M4006 A Ultra Sound System, Hewlett Packard with a 3.5 MHz probe. The radiologist was not informed about the study protocol. The portal vein was visualised in the longitudinal section at 1 – 2 cm before branching of the portal vein. The mean value of three readings of D and Vmax of the portal vein were used. All recordings were made during air inhalation. Vmean is calculated by using a formula (eq. 1) (25). Based on Vmean, PFV and CI were calculated (eq. 2 and 3) (26).
| (Eq.1) |
| (Eq.2) |
| (Eq.3) |
Statistical analysis
The results are expressed as X ± SD. ANOVA and Student’s t test were used for statistical analysis. Results were considered significant at P < 0.05.
Results
Age, body weight and height of healthy volunteers and cirrhotic patients (pre-dose) were not statistically different (Table 1). Baseline clinical parameters of pulse rate, Vmax, Vmean, D, PFV, CI, albumin, total bilirubin and PPTT (prolonged prothrombine time) were significantly different between healthy and cirrhotic patients except MAP (Table 2).
Table 2.
Mean values (X̄ ± SD) of several clinical parameters among healthy volunteers and cirrhotic Malay patients
| Clinical Parameters | Healthy subjects | Cirrhotic patients | Sig |
|---|---|---|---|
| HR (beat/min) | 72.73 ± 3.51 | 64.17 ± 6.39 | * |
| MAP (mmHg) | 93.29 ± 4.06 | 89.02 ± 4.95 | NS |
| D of portal vein (mm) | 6.49 ± 1.18 | 9.42 ± 2.60 | * |
| V max of portal vein (cm/sec) | 19.56 ± 2.19 | 14.21 ± 1.87 | * |
| V mean of portal vein (cm/sec) | 11.15 ± 1.25 | 8.10 ± 1.07 | * |
| PFV (ml/min) | 377.97 ± 141.40 | 652.98 ± 278.87 | * |
| CI (cm/min) | 0.31 ± 0.12 | 1.01 ± 0.04 | * |
| Albumin (g/dl) | 45.00 ± 1.77 | 36.92 ± 6.26 | * |
| Total bilirubin (mg/dl) | 10.33 ± 4.06 | 31.25 ± 18.01 | * |
| PPTT (sec) | 0 | 5.08 ± 4.08 | * |
P<0.001
NS (Non significant)
The effects of different doses of propranolol on the clinical parameters (% difference between pre-dose and post-dose) showed that there were significant differences in heart rate, Vmax and Vmean (Table 3). However, there was no significant difference in MAP, D, PFV, albumin, total bilirubin and PPTT in these patients.
Table 3.
Mean values (X̄ + SD) of propranolol concentration in plasma and % difference of several clinical parameters (pre and post-doses) of propranolol in cirrhotic Malay patients
| Parameters | 10 mg t.i.d (mean ± sd) | 20 mg t.i.d (mean ± sd) | 30 mg t.i.d (mean ± sd) | Sig |
|---|---|---|---|---|
| Pmpranolol comc, in plasma (ng/ml) | 64.67 ± 67.32 | 101.99 ± 77.42 | 158.78 ± 115.62 | ** |
| HR (beat/min) | −9.27 ± 4.14 | −19.08 ± 5.36 | −17.75 ± 4.95 | *** |
| MAP (mmHg) | −3.34 ± 4.55 | −6.34 ± 3.36 | −5.35 ± 4.77 | NS |
| Diameter of portal vein (mm) | 9.02 ± 19.85 | 13.00 ± 11.80 | −3.29 ± 21.00 | NS |
| Vmax and Vmean of portal vein (cm/sec) | −15.35 ± 12.25 | −28.83 ± 9.73 | −10.94 ± 18.99 | ** |
| PFV (ml/min) | 1.36 ± 42.37 | −9.12 ± 22.20 | −8.86 ± 41.45 | NS |
| Serum albumin (g/dl) | 1.78 ± 5.47 | −2.84 ± 3.55 | −4.18 ± 8.08 | NS |
| Serum belirubin (mg/dl) | 13.35 ± 51.43 | 27.40 ± 40.59 | 14.21 ± 11.27 | NS |
| PPTT (sec) | 48.53 ± 75.47 | 31.74 ± 58.85 | 67.26 ± 153.31 | NS |
P <0.01
P <0.001
NS (Non significant)
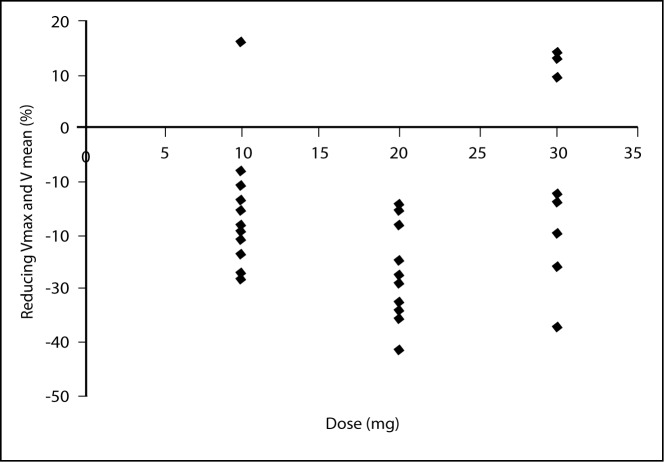
Heart rate
The effect of three doses of propranolol on heart rate analysed by one-way ANOVA showed significant difference (P < 0.001). Further analysis between dosages of 10 mg vs 20 mg and 10 mg vs 30 mg showed significant difference (P < 0.001 and P < 0.01 respectively), but there was no significant difference between 20 mg vs 30 mg dosages (Fig 2). However, it was seen that 20 mg is the dose that is able to reduce the heart rate optimally compared to the other two doses.
Figure 2.
Effects of three doses of propranolol on reducing heart rate
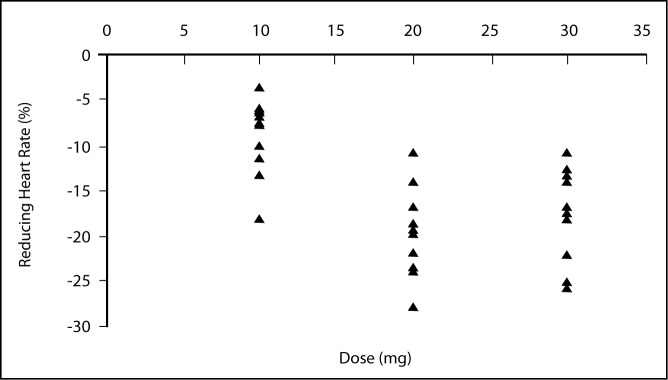
Vmax and Vmean
There was significant difference of the effects between three doses of propranolol in reducing Vmax and Vmean of portal vein (P < 0.01). No significant difference was observed for dosages of between 10 mg vs 30 mg, but between 10 mg vs 20 mg and 20 mg vs 30 mg there were significant differences (P < 0.05 and P < 0.01 respectively). Reduction of more than 10% of baseline for Vmax of the portal vein were achieved by doses of 10 mg and 20 mg. However, at the dose of 20 mg, the reduction of Vmax was more than that obtained with 10 mg (Fig. 3).
Figure 3.
Effects of three doses of propranolol on reducing Vmax
Correlation between HR and Vmax
No correlation was found between reduction of heart rate and reduction of Vmax and Vmean by propranolol (r = 0.13; R2 = 0.0176).
Correlation between Cp and effects
Mean steady-state levels of 65 ng/ml, 102 ng/ml and 159 ng/ml were achieved after taking 10 mg, 20 mg and 30 mg of propranolol thrice a day for one week. This study showed that as the dose increases, there was a corresponding increase in the blood level of the drug.
Cp vs HR
There was significant difference between HR reduction and propranolol concentration of the three steady state levels (P < 0.001).
Cp vs Vmax and Vmean
Similar findings (significant difference) were seen between effects of propranolol on Vmaxand Vmean among the three steady state levels (P < 0.01).
Cp vs MAP, PFV and D
There was no significant difference (Table 3).
Side effects
At 10 mg of propranolol, one patient experienced diarrhea and at 30 mg, one patient experienced insomnia, while three patient complained of fatigue (Table 4).
Table 4.
Side effects of different doses of propranolol in cirrhotic Malay patients
| Side effects | 10 mg t.i.d | 20 mg t.i.d | 30 mg t.i.d |
|---|---|---|---|
| Fatique | + (3 patients) | ||
| Headache | |||
| Depression | |||
| Disrhea | + (1 patient) | ||
| Nausea | |||
| Chest pain | |||
| Skin itchness | |||
| Lnsomnia | + (1 patient) | ||
| Raynaud’s phenomena | |||
| Constipation | |||
| Bradycardis | |||
| Breathless | |||
| Cold extremites | |||
| Mild encephalopathy | |||
|
| |||
| Total (%) | (8.33%) | (0%) | (33.33%) |
Discussion
Reduction of cardiac output (β1 blockade) and increase in splanchnic vascular resistance (β2 blockade) following the intake of propranolol causes a reduction in splanchnic blood flow which consequently reduces Vmax and Vmean of the portal vein (7). Based on this theory, propranolol has been used to control variceal bleeding due to portal hypertension in cirrhotic liver patients.
The present study showed that there was a good correlation between congestion index (CI) and the degree of liver cirrhosis between healthy and cirrhotic patients. Thus, the CI could act as a good predictor of early variceal bleeding. On the contrary, this parameter cannot be used to evaluate therapeutic effects of drugs that can reduce portal flow velocity due to some paradoxical effects produced by some drugs (27, 28). Propranolol is one such drug.
The present study also showed the limiting effects of propranolol on HR despite the dose being increased from 20 mg to 30 mg. This may be explained by the fact that at a dose of 20 mg, a ceiling effect was achieved and increasing the dose further does not increase the HR. Moreover, incidences of side effects increase with increasing dose. The result of the present study taken together suggest that the most suitable dose required to comply with therapeutic criteria for management of cirrhotic patients is 20 mg (5, 29, 30).
The results of our study suggest that the effects of 10 mg propranolol reduced Vmax and Vmean, subtherapetically, whereas a 30 mg dose gave a ceiling effect as increasing dose is not followed by a further increase in effect. The above finding is supported by a previous study where it was shown that an increase in propranolol blood levels did not cause extra splanchnic vasoconstriction, but in fact causes vasodilatation (31). Doses of 10 mg and 20 mg propranolol reduced Vmax at > 10% of baseline value. However, a dose of 20 mg reduced Vmax to a greater extend than at 10 mg. Consequently, the ability of propranolol (20 mg) to reduce Vmax provide evidence that fulfilled the standard acceptable criteria and therefore can be taken to be the optimal dose to reduce Vmax maximally in cirrhotic liver patients. The result is also in agreement with a previous study which used 40 mg propranolol (32, 33). Vorobioff et al (10) showed that propranolol could reduce portal pressure without influencing arterial pressure in patients with portal hypertension. However, Gaiani et al in their study showed that 40 mg of propranolol brought about reduction of HR, Vmax, Vmean and MAP significantly (9).
Several centers have reported that the control of portal hypertension induced by variceal bleeding amongst Caucasians required doses of 80 – 320 mg propranolol daily in order to achieve 25% change in HR (3, 10). However, our study showed that post-hepatitis B cirrhotic Malaysians required only 60 mg per day to meet the above criteria.
Dose-plasma concentration-effect relationship was observed in the present study whereby increasing dose correspondingly caused elevation of plasma propranolol levels with reduction of HR (10 mg vs 20 mg, P < 0. 001), reduction MAP (NS), reduction Vmax and Vmean (10 mg vs 20 mg, P < 0.01), decline PFV (20 mg vs 30 mg, NS) and increase D (NS) of portal vein. The results are in agreement with previous work described earlier (34, 35). These authors showed that increasing dose of propranolol caused a corresponding increase in plasma propranolol levels and it effects on HR and blood pressure only. However, another study found no correlation between plasma propranolol concentrations and the degree of beta-receptors blockade that caused reduction of portal blood pressure (36). Patients compliance was at an acceptable level (see Table 3) based on the observation that an increasing dose correspondingly increased plasma propranolol concentrations. Increasing the dose from 20 mg to 30 mg propranolol did not produce any change in desired effect although the plasma concentration has increased. This is attributed to the ceiling effect achieved by propranolol at 20 mg.
No correlation was seen between HR and Vmax, thus it could be concluded that HR and cardiac output are not reliable parameters in assessing portal system haemodynamics. It is reasonable to conclude further that propranolol at 20 mg thrice a day is appropriate in achieving therapeutic effect in cirrhotic Malay patients, % reduction in HR being excluded. The present study is in agreement with previous studies where the decline in HR by propranolol does not correspond to its effect on the portal blood flow (32, 37).
The present study also emphasises the measurement of Vmax and D using Doppler ultrasound as a non-invasive method which can gave precise and reproducible results (38–40). Greater than 80% of patients preferred Doppler ultrasound as compared to cathetherization technique. The Doppler ultrasound is more valuable in assessing portal hypertension. This haemodynamic measurement gives far greater contribution in the evaluation of portal hypertension as compared to catheterization (9, 41, 42). Reducing Vmax, is therefore a more reliable parameter for the assessment of therapeutic effect of drugs that cause changes in portal haemodynamics in liver cirrhotic patients. Apart from its role in determining drug effectiveness, Vmax is also an important supporting factor for the evaluation of prognosis relating to the Child-Pugh score in these patients (43).
During the course of the present study, it was also observed that ascites with Child-Pugh grade C and elevated serum bilirubin were risk factors for variceal bleeding. Incidence of variceal bleeding was also not related to age (29, 44).
Acknowledgments
This work was supported by Universiti Sains Malaysia Grant No. 331/0500/3570 and UPHA Corporation (M) Sdn. Bhd. We are grateful to En. Abdul Razak Ahmad and Cik Aminah Noor for their technical assistance. The above project has been aproved by the Ethical Committee, Universiti Sains Malaysia and thus comply with the current laws of Malaysia.
References
- 1.The Italian Multicenter Project for Propranolol in Prevention of Bleeding. Propranolol for prophylaxis of bleeding in cirrhosis patients with large varices: a multicenter, randomized clinical trial. Hepatology. 1988;8:1–5. [PubMed] [Google Scholar]
- 2.Colombo M, De Franchis R, Tommasini M, Sangiovani A, Dioguardi N. β-blockade prevents recurrent gastrointestinal bleeding in well-compensated patient with alcoholic cirrhosis: a multicenter randomised controlled trial. Hepatology. 1989;9:433–438. doi: 10.1002/hep.1840090315. [DOI] [PubMed] [Google Scholar]
- 3.Andreani T, Poupon RE, Balkan BJ, Trinchet JC, Grange J-D, Peigney N, Beaugrand M, Poupon R. Preventive therapy of first gastrointestinal bleeding in patients with cirrhosis: result of a controlled trial comparing propranolol, endoscopic sclerotheraphy and placebo. Hepatology. 1990;12:1413–1419. doi: 10.1002/hep.1840120624. [DOI] [PubMed] [Google Scholar]
- 4.Garden OJ, Mills PR, Birnie GG, Murray GD, Carter DC. Propranolol in the prevention of recurrent variceal hemorrhage in cirrhotic patients. Gastroenterology. 1990;98:185–190. doi: 10.1016/0016-5085(90)91308-s. [DOI] [PubMed] [Google Scholar]
- 5.Groszmann RJ, Bosch J, Grace ND, Conn HO, Garcia-Tsao G, Navasa M, Alberts J, Rodes J, Fischer R, Bermann M, Rofe S, Patrick M, Lerner E. Hemodynamic events in a prospective randomised trial of propranolol versus placebo in the prevention of a first variceal hemorrhage. Gastroenterology. 1990;99:1401–1407. doi: 10.1016/0016-5085(90)91168-6. [DOI] [PubMed] [Google Scholar]
- 6.Conn HO, Grace ND, Bosch J, Groszmann RJ, Wright SC, Matloff DS, Garcia-Tsao G, Fisher RL, Navasa M. Propranolol in the prevention of the first hemorrhage from esophagogastric varices : a multicenter, randomised clinical trial. Hepatology. 1991;13:902–912. [PubMed] [Google Scholar]
- 7.Feu F, Bordas JM, Luca A, Garcia-Pagan JC, Escorsell A, Bosch J, Rodes J. Reduction of variceal pressure by propranolol: Comparison of the effects on portal pressure and azygos blood flow in patients with cirrhosis. Hepatology. 1993;18:1082–1089. [PubMed] [Google Scholar]
- 8.Bernard B, Lebrec D, Mathurin P, Opolon P, Poynard T. Beta-adrenergic antagonist in the prevention of gastrointestinal rebleeding in patients with cirrhosis : A Meta-Analysis. Hepatology. 1997;25:63–70. doi: 10.1053/jhep.1997.v25.pm0008985266. [DOI] [PubMed] [Google Scholar]
- 9.Gaiani S, Bolondi L, Fenyves D, Zironi G, Rigamonti A, Barbara L. Effects of propranolol on portosystemic collateral circulation in patients with cirrhosis. Hepatology. 1991;14:824–829. doi: 10.1002/hep.1840140514. [DOI] [PubMed] [Google Scholar]
- 10.Vorobioff J, Picabea E, Gamen M, Villavicencio R, Bordato J, Bessone F, Tanno H, Pallazi J, Sarano H, Pozzoli L, Sanchez R, Giordano R. Propranolol compared with propranolol plus isosorbide dinitrate in portal-hypertensive patients: Long-term hemodynamic and renal effects. Hepatology. 1993;18:477–484. [PubMed] [Google Scholar]
- 11.Cales P, Pierre-Nicolas M, Guell A, Mauroux JL, Franco-Sempe A, Vinel J - P, Gerand G, Pascal J-P. Propranolol does not alter cerebral blood flow and functions in cirrhotic patients without previous hepatic encephalopathy. Hepatology. 1989;9:439–442. doi: 10.1002/hep.1840090316. [DOI] [PubMed] [Google Scholar]
- 12.Lopez CG. Epidemiology of persistent hepatitis B virus infection. Malaysian. J. Pathol. 1985;7:7–10. [PubMed] [Google Scholar]
- 13.Lingao AL. The relationship of hepatocellular carcinoma and liver cirrhosis to hepatitis B virus infection in Philippines. Gastroenterol. Jpn. 1989;24:425–33. doi: 10.1007/BF02774352. [DOI] [PubMed] [Google Scholar]
- 14.Sulaiman HA. Hepatitis B virus infection in liver cirrhosis and hepatocellular carcinoma in Jakarta Indonesia. Gastroenterol. Jpn. 1989;24:434–441. doi: 10.1007/BF02774353. [DOI] [PubMed] [Google Scholar]
- 15.Kudva MV, Zawawi MM. Chronic liver disease in Kuala Lumpur, Malaysia : a clinical study. Singapore. Med. J. 1990;31:368–73. [PubMed] [Google Scholar]
- 16.Gust ID. Epidemiology of hepatitis B infection in Western Pacific and South East Asia. Gut. 1996;38(Suppl 2):18–23. doi: 10.1136/gut.38.suppl_2.s18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lansang MA. Epidemiology and control of hepatitis B infection: a perspective from the Philippines, Asia. Gut. 1996;38(Suppl. 2):43–47. doi: 10.1136/gut.38.suppl_2.s43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bellentani S, Tiribelli C, Saccoccio G, Sodde M, Fratti N, De Martin C, Cristianini G. Prevalence of chronic liver disease in the general population of nothern Italy : the Dionysos Study. Hepatology. 1994;20:1442–1449. doi: 10.1002/hep.1840200611. [DOI] [PubMed] [Google Scholar]
- 19.Corrao G, Ferrazi PA, Galatola G. Exploring the role of diet in modifying the effect of known disease determinants: application to risk factor of liver cirrhosis. Am. J. Epidemiol. 1995;142:1136–1146. doi: 10.1093/oxfordjournals.aje.a117572. [DOI] [PubMed] [Google Scholar]
- 20.Medina E, Kaempffer AM. Liver cirrhosis in Chile: epidemiologic consideration. Rev. Med. Chil. 1993;121:1324–1331. [PubMed] [Google Scholar]
- 21.National Center for Chronic Disease Prevention and Health Promotion, CDC Death and hospitalization from chronic liver disease and cirrhosis-United States, 1980–1989. JAMA. 1993;269:569–572. [PubMed] [Google Scholar]
- 22.Truckenbrodt J, Schmidt H, Bohndorf HJ. Epidemiology of liver disease in the GDR, 1979–1989. (English abstract) Gastroenterol. J (Germany) 1991;51:129–131. [PubMed] [Google Scholar]
- 23.Tsega E, Nordenfelt E, Hansson BG, Mengesha B, Lindberg J. Chronic liver disease in Ethiopia: a clinical study with emphasis on identifying common cause. Ethiop. Med. J. 1992;30(2 Suppl):1–33. [PubMed] [Google Scholar]
- 24.Wood AJJ, Carr K, Vestal RE, Belcher S, Wilkinson GR, Shand DG. Direct measurement of propranolol bioavailability during accumulation to steady-state. Br. J. Clin. Pharmacol. 1978 b;6:345–350. doi: 10.1111/j.1365-2125.1978.tb00862.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moriyasu F, Ban N, Nishida O, Nakamura T, Miyake T, Uchino H, Kanematsu Y, Koizumi S. Clinical application of an ultrasonic duplex system in the quantitative measurement of portal blood flow. J. Clin. Ultrasound. 1986a;14:579–588. doi: 10.1002/jcu.1870140802. [DOI] [PubMed] [Google Scholar]
- 26.Moriyasu F, Nishida O, Ban N, Nakamura T, Sakai M, Miyake T, Uchino H. ‘Congestion index’ of the portal vein. Am. J. Roentgenol. 1986b;146:735–739. doi: 10.2214/ajr.146.4.735. [DOI] [PubMed] [Google Scholar]
- 27.Siringo S, Bolondi L, Gaiani S, Sofia S, Zironi G, Rigamonti A, Di Febo G, Miglioli M, Cavalli G, Barbara L. Timing of the first variceal hemorrhage in cirrhotic patients: prospective evaluation of Doppler flowmetry, endoscopy and clinical parameters. Hepatology. 1994a;20:66–73. doi: 10.1016/0270-9139(94)90135-x. [DOI] [PubMed] [Google Scholar]
- 28.Siringo S, Bolondi L, Gaiani S, Sofia S, Di Febo G, Zironi G, Rigamonti A, Miglioli M, Cavalli G, Barbara L. The relationship of endoscopy, portal Doppler ultrasound flowmetry, clinical and biochemical test in cirrhosis. J. Hepatol. 1994b;20:11–18. doi: 10.1016/s0168-8278(05)80461-1. [DOI] [PubMed] [Google Scholar]
- 29.Poynard T, Cales P, Pasta L, Ideo G, Pascal J-P, Pagliaro L, Lebrec D, The Franco-Italian Multicenter Study Group Beta-adrenergic-antagonist drugs in the prevention of gastrointestinal bleeding in patients with cirrhosis and oesophageal varices: an analysis of data and prognostic factors in 589 patients from four randomised clinical trials. New Engl. J. Med. 1991;324:1532–1538. doi: 10.1056/NEJM199105303242202. [DOI] [PubMed] [Google Scholar]
- 30.Tincani E, Cioni G, D’Alimonte P, et al. Effects of propranolol compared with clonidine on portal haemodynamics: a double-blind cross over study using duplex-Doppler ultrasonography. Eur. J. Gastroenterol. Hepatol. 1995;7(9):893–897. [PubMed] [Google Scholar]
- 31.Stauber RE, Heinemann A, Truner M, Krejs GJ. Divergent effect of propranolol and nadolol in isolated mesenteric arteries from normal and portal hypertensive rats. Eur. J. Clin. Invest. 1996;26:676–680. doi: 10.1111/j.1365-2362.1996.tb02152.x. [DOI] [PubMed] [Google Scholar]
- 32.Cioni G, D’Alimonte P, Zerbinati F, Ventura P, Cristani A, Vignoli A, Romagnoli R, Ventura E. Duplex-Doppler ultrasonography in evaluation of cirrhotic patients with portal hypertension and in the analysis of their response to drugs. J. Gastroenterol. Hepatol. 1992;7:388–392. doi: 10.1111/j.1440-1746.1992.tb01005.x. [DOI] [PubMed] [Google Scholar]
- 33.Sabba C, Ferraioli G, Buonamico P, Berardi E, Antonica G, Taylor KJW, Albano O. Echo-Doppler evaluation of acute flow changes in portal hypertensive patients: flow velocity as a reliable parameter. J. Hepatol. 1992b;15:356–60. doi: 10.1016/0168-8278(92)90068-z. [DOI] [PubMed] [Google Scholar]
- 34.Coelhoe JB, Dvornik D, Mullane JF, Kaufman J, Simon J, Krantz KD, Lee TY, Perdue HS, Weidler D. Dynamics of propranolol dosing schedules. Clin. Pharmacol. Ther. 1983;34:440–447. doi: 10.1038/clpt.1983.195. [DOI] [PubMed] [Google Scholar]
- 35.Dey M, Brisson J, Davis G, Enever R, Pray K, Zaim B, Dvornik D. Relationship between plasma propranolol concentration and dose in young healthy volunteers. Biophar. Drug. Dis. 1986;7:103–111. doi: 10.1002/bdd.2510070202. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Tsao G, Grace ND, Groszmann RJ, Conn HO, Bermann MM, Patrick MJC, Morse SS, Alberts JL. Short-term effects of propranolol on portal venous pressure. Hepatology. 1986;6:101–106. doi: 10.1002/hep.1840060119. [DOI] [PubMed] [Google Scholar]
- 37.Vorobioff J, Picabea E, Villavicencio R, Puccini V, Rossi O, Bordato J, Andermo M. Acute end chronic hemodynamic effects of propranolol on unselected cirrhotic patients. Hepatology. 1987;9:648–653. doi: 10.1002/hep.1840070406. [DOI] [PubMed] [Google Scholar]
- 38.Consensus conference. The value of Doppler Ultrasound in the study of hepatic hemo-dynamics. J Hepatol. 10:353–355. doi: 10.1016/0168-8278(90)90146-i. [DOI] [PubMed] [Google Scholar]
- 39.Sabba C, Ferraioli G, Sarin KS, Lerner E, Groszmann R, Taylor KJW. Feasibility spectrum for Doppler flowmetry of splanchnic vessels in normal and cirrhotic population. J. Clin. Ultrasound. 1990a;9:705–710. doi: 10.7863/jum.1990.9.12.705. [DOI] [PubMed] [Google Scholar]
- 40.Bolondi L, Gaiani S, Barbara L. Accuracy and reproducibility of portal flow measurement by Doppler Ultrasound. J. Hepatol. 1991;13:269–273. doi: 10.1016/0168-8278(91)90067-l. [DOI] [PubMed] [Google Scholar]
- 41.Ljubicic N, Duvanyak M, Rotkvic I, Kopjar B. Influence of the degree of liver failure on portal blood flow in patients with liver cirrhosis. Scand. J. Gastroenterol. 1990;25:395–400. doi: 10.3109/00365529009095505. [DOI] [PubMed] [Google Scholar]
- 42.Zironi G, Gaiani S, Fenyves D, Rigamonti A, Bolondi L, Barbara L. Value of measurement of mean portal flow velocity by Doppler flowmetry in the diagnosis of portal hypertension. J. Hepatol. 1992;16:298–303. doi: 10.1016/s0168-8278(05)80660-9. [DOI] [PubMed] [Google Scholar]
- 43.Tai D-I, Chuah S-K, Chen C-L, Lo SK, Changchien C-S, Li I-T. Inter observer variability of portal hemodynamics research by Doppler Ultrasound on three different location of portal vein. J. Clin. Ultrasound. 1996;24:61–66. doi: 10.1002/(SICI)1097-0096(199602)24:2<61::AID-JCU2>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 44.Kleber G, Sauerbruch T, Ansari H, Paumgartner G. Prediction of variceal hemorrhage in cirrhosis: a prospective follow-up study. Gastroenterology. 1991;100:1332–1337. [PubMed] [Google Scholar]