Abstract
OBJECTIVE:
With the use of a new cohort of adolescent subjects, predictors from the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA) interview and the Achenbach Youth Self Report (YSR) were combined to model age of first drink (AFD).
METHODS:
Subjects consisted of 820 adolescents (ages 14–17) drawn from the current phase of the Collaborative Study on the Genetics of Alcoholism. Three Cox proportional hazards models were considered. Model 1 contained SSAGA variables equivalent to AFD predictors from our previous study: interview age, family history of alcohol dependence, and number of conduct disorder symptoms. Model 2 incorporated 2 additional SSAGA questions (best friends drink and smoked a cigarette before a reported AFD) plus 8 YSR-derived scale scores. Model 3 was a reduced version of model 2, retaining only significant predictors.
RESULTS:
Model 2 was a significant improvement over model 1. Model 3 was the best and the most parsimonious of the 3 with respect to likelihood ratio and Wald χ2 tests and retained only 5 variables from model 2. Included variables were the following: (1) best friends drink, (2) membership in a high-risk alcohol dependence family, (3) number of conduct disorder symptoms, (4) YSR externalizing score, and (5) YSR social problems score.
CONCLUSIONS:
Adding variables to those from our original study improved our ability to model the likely age of alcohol initiation. In addition to the SSAGA, the YSR appears to have utility as a research tool to predict the age of alcohol initiation.
KEY WORDS: alcohol/drug use, age of first use, predictor variables, modeling age of first use
What’s Known on This Subject:
First drink before age 15 greatly increases the likelihood for later alcohol abuse or dependence. Separate investigations have linked many variables to alcohol initiation, but few have attempted to identify the optimal combination of predictors for age of alcohol initiation.
What This Study Adds:
This article supports the screening questions selected in the joint National Institute on Alcohol Abuse and Alcoholism and the American Academy of Pediatrics initiative to identify and initiate intervention in youth at risk for early use of alcohol.
Drinking a whole standard drink of alcohol before age 15 is associated with a fourfold increase in the likelihood of a lifetime Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition1 diagnosis of alcohol dependence (AD) compared with individuals whose first drink occurs after the age of 20.2 If this relationship is causal rather than merely predictive, then delaying age of first drink (AFD) may be an effective strategy for decreasing the risk of AD. To date, identified risk factors that relate to an earlier AFD include male gender,3,4 childhood psychopathology,5–7 poor family supervision and inconsistent/harsh discipline,5,8,9 positive peer attitudes toward drinking,8,10–17 peer use of other substances,8,10,12,17 parental history of AD or antisocial personality disorder,18–20 relationships with antisocial peers,21 and previous smoking22; protective factors include age-appropriate competencies, self-regulation skills, capacity to cope with stress, and academic success.21 Unfortunately, many of these factors have not been studied in combination with each other.
The aim of the current study is to examine a population of adolescents, combining predictor variables to predict the likelihood of earlier alcohol initiation from the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA),9 a widely used research interview, and the Achenbach Youth Self Report (YSR),23 a self-completed questionnaire commonly used in pediatric settings. Such a research model should help the development of a clinical screening instrument to identify youth who may benefit from treatment aimed at delaying alcohol initiation.
Methods
Subjects
All subjects were participants in the multisite Collaborative Study on the Genetics of Alcoholism (COGA), a study designed to explore behavioral, biochemical, genetic, neuropsychological, and neurophysiologic phenomena related to AD in high-risk (HR; defined as having any adult family member in treatment for AD) and community comparison families.24 Since 2005, COGA has used a prospective design focusing on participants who were 12 to 21 years of age at the start of this phase. These predominantly non–first-degree family members (eg, nieces, nephews, grandchildren) of the original HR and comparison families are seen every 2 years. Institutional review boards at all sites reviewed and approved study design. Parents provided informed consent for all offspring <18 years; children 13 and older provided consent, and children aged 12 provided assent.
From this group, 1246 subjects (age 12–17) were interviewed during the years 2005–2007. The current study was based partly on previously identified risk factors for a known AFD in an unrelated adolescent sample.7 To build upon the findings from this study, subjects were selected to have an interview age distribution approximately similar to that of this first study; this resulted in a sample of 822 adolescents aged 14 to 17. Reported AFD was assessed from the SSAGA question: “How old were you when you had your very first whole drink–i.e. a can of beer, a glass of wine, a wine cooler, or a shot of hard liquor?” Because 2 subjects reported their first drink occurred during “infancy,” they were considered unreliable and removed. Of the final 820 subjects, a reported AFD was given by 346 (42.2%) individuals; mean AFD was 14.0 years (SD = 1.8; range, 6–17).
Variables
The version of the SSAGA interview for children aged 12 to 17 years, was administered by research assistants trained to clarify ambiguous answers. It allows the reliable establishment of most pediatric psychiatric diagnoses, including substance disorders.9 The Achenbach YSR, for children aged 11 to 18 years, is self-completed; it is not diagnostic but obtains standardized data, over the last 6 months, on a broad spectrum of competencies, behavioral syndromes, and psychiatric disorder–oriented scales. It has established reliability and validity.23 Both assessments were generally completed within 1 month of each other (95%).
The initial variables selected from the SSAGA included 2 of the 3 (of a total of 20) previously identified predictors for AFD in an unrelated sample of adolescents.7 These variables consisted of interview age and number of lifetime conduct disorder (CD) symptoms. The third variable, number of adult siblings with AD (a hypothesized measure of both environmental and familial risk for AD), was not assessed; instead, the number of AD parents (range, 0–2) and HR family membership (yes or no) were used. Based on the literature review, a new SSAGA variable, best friends drink (most or all best friends = yes, few or no best friends = no) was added. Because of an ambiguous finding between a study that demonstrated previous cigarette initiation influencing current alcohol use22 and a previous study of an unrelated sample of COGA adolescents that indicated no difference in age between initiation of alcohol and,25 a dichotomous variable was created to explore the effect of age of cigarette initiation on AFD (SSAGA age of first full cigarette - reported AFD > 0 = yes, ≤ 0 = no).
Eight Achenbach YSR scales were selected. Four scales were hypothesized to reduce the likelihood of earlier alcohol initiation (ie, considered protective). The activities competence scale (range, 0–15) is a 6-item measure of performance in sports, other recreational activities, and jobs/chores. The social competence scale (range, 0–14) is a 6-item measure of the number of group activities, the number of friends, the frequency of interactions, and the quality of these interactions. The academic performance scale is the mean (range, 0–3) self-rating in up to 7 scholastic areas. The positive qualities scale is a 14-item measure of social skills, integrity, assertiveness, and satisfaction with current life.
Four Achenbach YSR scales were hypothesized to increase the likelihood of an earlier age of alcohol initiation (ie, considered harmful). The social problems scale consists of 11 items that address difficulties with friends and peers. The attention problems scale contains 9 items that assess difficulties with concentration, poor attention, and distractibility. The internalizing scale consists of 31 questions examining negative emotions and somatic complaints. The externalizing scale contains 32 questions assessing rule breaking, verbal/physical aggression, and property destruction.
Data Analyses
Cox proportional hazards modeling (SAS PROC PHREG; SAS release 9.2, SAS Institute, Inc, Cary, NC) with the option COVSANDWICH (AGGREGATE) to adjust for correlated familial data was used to test the effect of these variables on the likely age of alcohol initiation. All model assumptions were checked for violations of the proportional hazards assumption and overall model adequacy.26 Fourteen single-predictor models estimated the hazard ratio to determine each predictor’s independent effect. Two models were subsequently considered. Model 1, containing SSAGA variables similar to our previous study, tested whether these variables were also predictive for modeling the likelihood of earlier alcohol initiation. Model 2, including the 2 new SSAGA plus the 8 Achenbach YSR variables, tested whether model 1 could be improved. Because 49 of the 91 variable pairwise comparisons yielded significant correlations (P < .01), likelihood ratio and Wald χ2 tests were used in stepwise selection and backward elimination procedures to determine those variables that actually contributed to model 2; these variables formed model 3.
Results
Subject Characteristics
Mean interview age (SD) was 15.5 (1.1) years; subjects with a known AFD were on average 0.7 years older (P < .001). Subjects were evenly distributed across the age range (14–17) of the study; not surprisingly, the proportion of subjects who reported an AFD was higher among the older subjects (P < .0001). The majority of the 820 subjects were white (63.4%), female (52.9%), and from HR families (85.8%). Fifty-eight percent had no alcohol-dependent parent (only AD father = 21%, only AD mother = 14%, and both parents alcoholic = 6%). Parents reported a median income of $40 000 to $49 999 and a median educational level of 1 year post high school (for both mothers and fathers). Mean (SD) number of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition CD symptoms was 0.74 (1.2) with an observed range of 0 to 10. Best friends drink was reported by 150 (18.3%) subjects; this was 36.7% among those who reported an AFD. Smoking at least 1 whole cigarette before having a first whole drink of alcohol was reported by 50 (14.5%) of the 346 subjects who reported an AFD. Mean raw scores (SD, range) for the 4 YSR protective scales were (a) activities competence: 9.6 (2.9, 0–15), (b) social competence: 8.6 (2.4, 0–14), (c) school competence: 2.2 (0.6, 0–3), and (d) positive qualities: 21.4 (4.2, 1–28); similarly for the 4 YSR harmful scales, the corresponding statistics were (1) social problems: 3.4 (2.9, 0–18), (2) attention problems: 5.6 (3.6, 0–16), (3) internalizing: 11.6 (8.2, 0–48), and (4) externalizing: 12.6 (8.4, 0–50).
Table 1 presents the 14 predictors’ independent effects on alcohol initiation. All SSAGA and YSR scales hypothesized to increase the likelihood of earlier alcohol initiation did so (P value range, <.0001–.018). The 4 YSR competence scales hypothesized to reduce the likelihood of earlier alcohol initiation did this as well; with the exception of YSR positive qualities, all were significant (P value range, .001–.016).
TABLE 1.
Relationship Between Predictor Variable and Likelihood of Age of Alcohol Initiation Unadjusted for Any Other Variable
| Predictor Source | Predictor | N | Estimated Hazard Ratio | 95% Confidence Interval | P | |
|---|---|---|---|---|---|---|
| SSAGA | Original | HR family member | 819 | 1.81 | 1.28–2.56 | .001 |
| No. alcohol-dependent parents | 819 | 1.31 | 1.11–1.54 | .001 | ||
| No. lifetime CD symptoms | 819 | 1.22 | 1.12–1.33 | <.0001 | ||
| Interview age | 819 | 1.16 | 1.04–1.28 | .006 | ||
| New | Best friends drink | 817 | 3.14 | 2.60–3.79 | <.0001 | |
| First cigarette before first drink | 819 | 1.81 | 1.44–2.28 | <.0001 | ||
| Achenbach YSR Scale Score | Protectivea | YSR positive qualities | 819 | 0.98 | 0.96–1.01 | .132 |
| YSR activities competence | 819 | 0.96 | 0.93–0.99 | .016 | ||
| YSR social competence | 817 | 0.95 | 0.91–0.99 | .011 | ||
| YSR school competence | 801 | 0.76 | 0.64–0.89 | .001 | ||
| Harmfula | YSR externalizing | 819 | 1.06 | 1.05–1.07 | <.0001 | |
| YSR attention problems | 819 | 1.07 | 1.04–1.09 | <.0001 | ||
| YSR social problems | 819 | 1.04 | 1.01–1.07 | .017 | ||
| YSR internalizing | 819 | 1.01 | 1.00–1.03 | .018 | ||
An estimated hazard ratio >1 increases the likelihood and an estimated hazard ratio <1 decreases the likelihood of earlier alcohol initiation for a unit increase of the predictor.
Protective variables were hypothesized to reduce the likelihood of earlier alcohol initiation. Harmful variables were hypothesized to increase the likelihood of earlier alcohol initiation.
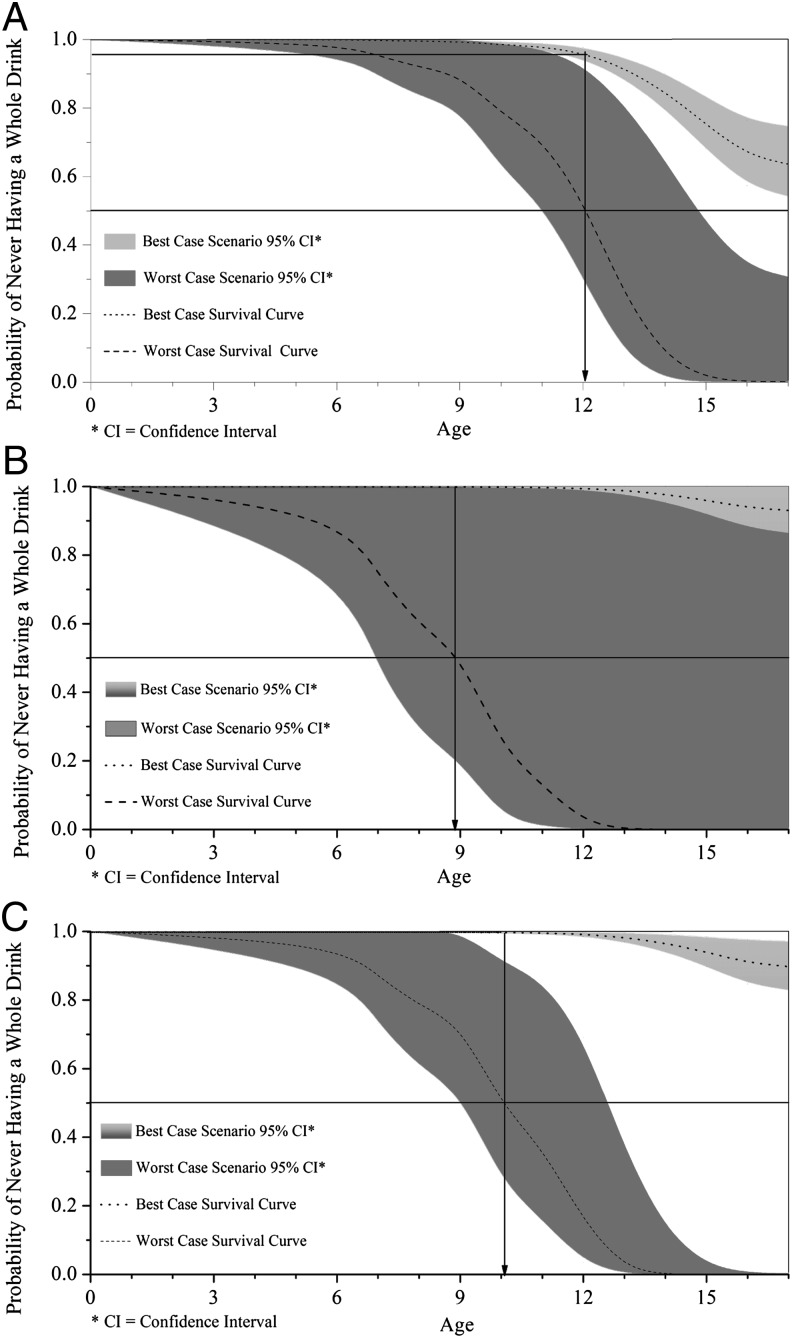
Table 2 presents the results of model 1. The estimated adjusted hazard ratios indicate that the likelihood of earlier alcohol initiation increased as the value for each predictor increased (even as the other predictors remained constant). Figure 1A shows 2 survival curves predicted by model 1: one for a best-case scenario (no CD symptoms, no AD parents, and not an HR family member) and one for a worst-case scenario (10 CD symptoms, 2 AD parents, and HR family member), with interview age held constant at 17. These curves estimate a 50% likelihood for worst-case individuals to have their first drink shortly after their 12th birthday; conversely, there is <5% likelihood for best-case individuals to start drinking at this age.
TABLE 2.
Fitted Cox Proportional Hazards Models and Predictor Values for the Best and Worst Scenario Curves Shown in Fig 1
| Predictor Variables | Estimated Hazard Ratio | 95% Confidence Interval | P | Best Case | Worst Case |
|---|---|---|---|---|---|
| Model 1 | |||||
| HR family member | 1.55 | 1.09–2.22 | .016 | No | Yes |
| No. of parents with AD | 1.23 | 1.04–1.45 | .014 | 0 | 2 |
| No. of lifetime CD symptoms | 1.21 | 1.11–1.32 | <.0001 | 0 | 10 |
| Interview age | 1.16 | 1.05–1.29 | .006 | 17 | 17 |
| Model 2 | |||||
| Best friends drink | 2.43 | 1.93–3.05 | <.0001 | No | Yes |
| HR family member | 1.42 | 0.99–2.02 | .054 | No | Yes |
| No. of CD symptoms | 1.12 | 1.03–1.22 | .008 | 0 | 10 |
| YSR school competence | 1.07 | 0.89–1.29 | .470 | 0 | 3 |
| No. of parents with AD | 1.06 | 0.89–1.28 | .496 | 0 | 2 |
| YSR externalizing | 1.05 | 1.03–1.07 | <.0001 | 0 | 50 |
| YSR social competence | 1.01 | 0.96–1.06 | .770 | 2 | 14 |
| YSR internalizing | 1.00 | 0.98–1.01 | .838 | 45 | 0 |
| Interview age | 1.00 | 0.89–1.13 | .958 | 17 | 17 |
| First cigarette before first drink | 1.00 | 0.72–1.38 | .998 | No | Yes |
| YSR attention problems | 0.99 | 0.95–1.03 | .658 | 16 | 0 |
| YSR activities competence | 0.99 | 0.95–1.02 | .408 | 15 | 0 |
| YSR positive qualities | 0.99 | 0.96–1.02 | .459 | 28 | 1 |
| YSR social problems | 0.96 | 0.92–1.00 | .073 | 18 | 0 |
| Model 3 | |||||
| Best friends drink | 2.34 | 1.90–2.88 | <.0001 | No | Yes |
| HR family member | 1.49 | 1.07–2.07 | .019 | No | Yes |
| No. of CD symptoms | 1.11 | 1.03–1.20 | .010 | 0 | 10 |
| YSR externalizing | 1.05 | 1.03–1.06 | <.0001 | 0 | 50 |
| YSR social problems | 0.95 | 0.92–0.99 | .011 | 18 | 0 |
Predictors are ordered according to the estimated hazard ratio. For a given predictor, an estimated hazard ratio >1 increases the likelihood and an estimated hazard ratio <1 decreases the likelihood of earlier alcohol initiation for a unit increase of the predictor.
FIGURE 1.
Best- and worst-case scenarios of the 3 fitted Cox proportional hazards models. The downward vertical arrows within the figures suggest that an individual at this age has a 50% chance of having his/her first whole drink of alcohol under the worst-case scenario.
Table 2 (model 2) contains these 4 variables along with the 2 new SSAGA items as well as the 8 YSR variables. The estimated adjusted hazard ratios indicate that, in this combined model, only 3 of the 14 variables were significant. Figure 1B shows 2 survival curves predicted by model 2, one for the best-case and one for the worst-case scenario, with the interview age again held constant at 17. These curves show a 50% likelihood for worst-case individuals to experience alcohol initiation shortly before their ninth birthday; conversely, the likelihood for best-case individuals at this age was <1%.
Because of the multiple correlated variables and the numerous nonsignificant variables in model 2, both stepwise selection and backward elimination procedures were used to identify the most parsimonious model. This model only included 5 variables (see model 3 in Table 2). The estimated adjusted hazard ratio for initiating drinking associated with best friends drink was 2.34. Similarly, being a member of an HR family had an estimated adjusted hazard ratio of 1.49. A unit increase in the number of CD symptoms corresponded to an increase of 1.11 in the estimated adjusted hazard ratio; there was a sizeable cumulative effect with a maximum of 2.84 for the most CD symptoms reported (10) compared with 1 for the lowest (0). The estimated adjusted hazard ratio for a unit increase in the YSR externalizing score was 1.05; again, there was a sizeable cumulative effect with a maximum of 11.47 for the highest score (50) compared with 1 for the lowest (0). By itself, the social problems score increased the likelihood of earlier alcohol initiation but, unexpectedly, in combination with other predictors, actually lowered this likelihood. A unit increase in this score reduced the estimated adjusted hazard ratio by 0.95: that is, a minimum estimated hazard ratio of 0.41 for the highest number of social problems reported (18), compared with 1 for the lowest (0). Figure 1C shows 2 survival curves predicted by model 3, one for the best-case and one for the worst-case scenario. These curves estimate a 50% likelihood for worst-case individuals to start drinking shortly after their 10th birthday, compared with ∼1% who would do so for best-case individuals. By using model 3, subjects with modal predictor values (HR family member, best friends do not use alcohol, 0 CD symptoms, social problems score of 3, and externalizing scale score of 11) would have a 43% likelihood of having their first drink by their 17th birthday.
To confirm model 3 as the best and most parsimonious model, the likelihood ratio and Wald χ2 tests were performed between pairs of nested models. The analyses indicated that model 2 was better than model 1 (χ2 = 162.66, degrees of freedom [df] = 10, P < .0001) and that model 3 was not inferior to model 2 (χ2 = 2.66, df = 9, P = .9762). Because model 3 had fewer predictors and a much narrower confidence interval, it became the preferred model for alcohol initiation.
To further explore the unexpected relationship between the social problems score and alcohol initiation in model 3, post hoc analyses restricted to drinkers were conducted; this relationship only appeared after controlling for YSR externalizing score. For the majority of drinking adolescents, their source of first alcoholic drink was from their peers. There were significantly more drinkers with a high YSR externalizing score who reported best friends drink than those with a low YSR externalizing score (χ2 = 10.4, df = 1, P = .001), but there were no differences with respect to YSR social problems score (χ2 = 0.2, df = 1, P = .6932). However, the combination of both variables in a single logistic analysis on the likelihood of reporting best friends drink was significant (χ2 = 13.7, df = 3, P = .0034). This suggests that, given YSR externalizing score, a high YSR social problems score was associated with having fewer drinking friends.
Discussion
Variables selected for model 3 were drawn from both the SSAGA (a proven research instrument for problematic alcohol use) along with the Achenbach YSR (widely used in pediatric settings). Significant predictors included 3 SSAGA variables (best friends drink, HR family member, and number of CD symptoms) and 2 YSR scores (externalizing score and social problems score). Both the YSR externalizing score and the number of lifetime SSAGA CD symptoms increased the likelihood of early alcohol initiation despite some overlap of content and statistical correlation between them. A likely explanation for this is that 25 of the 32 YSR externalizing scale items are not directly related to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition1 criteria for CD and broaden the range of disruptive behavior linked to the risk for early alcohol initiation. The effect of the YSR social problems score in model 3 was unanticipated; however, based on the observation of subjects with a known AFD, a likely explanation is that individuals with high social problems have more difficulty with friendships, have fewer drinking best friends, and subsequently have less opportunity to obtain alcohol for their first whole drink. As these individuals mature and gain more access to alcohol, it is possible that their relative social isolation may not hinder, and may even facilitate, continued drinking. This possibility needs to be addressed empirically with further follow-up.
There are limitations in this study. Our sample is weighted toward HR family members (85%), with >40% having at least 1 AD parent. Entering both HR family membership and the number of AD parents was an attempt to adjust for this bias; independent analyses based on family type could not be done because of the lack of a sufficient number of subjects from comparison families. A second limitation may be the combining of data across a 4-year period of adolescent development. Findings from the Monitoring the Future Study27 suggest that, during this period of adolescent development, alcohol initiation increases from 35% to >70%. We attempted to take these potential changes into account by including interview age as a predictor, but it was not significant in the preferred model. A third limitation is that subjects aged 12 and 13 were not included in the analyses because of our desire to keep the study sample similar in age to our previous study. Finally, although the predictors in model 3 are associated with the likely outcome of early alcohol initiation, further study is needed to determine if these variables actually influence this change, and if so, through what mechanisms.
Despite these limitations, there are a number of strengths to this study. The 3 SSAGA variables selected are clearly defined so that they could be replicated by investigators using other instruments. The YSR variables were similar to those suggested by the literature4–7,21 as affecting the age of initiating alcohol and supports our belief that the YSR has utility in future alcohol-related studies. The Cox proportional hazards model allowed the inclusion of adolescents who were still at risk for alcohol initiation and allowed a wide combination of both potential protective and harmful predictors. Finally, because of the prospective nature of the COGA study, we are in an exceptional position to monitor the development of late adolescent/early adulthood alcohol-use disorders in these subjects. We will then have the ability to further examine which of the current identified predictors for early alcohol initiation also contribute to problematic alcohol use as these subjects age over time.
The final strength of this study is its support for the recent joint National Institute on Alcohol Abuse and Alcoholism and American Academy of Pediatrics initiative28 to identify and initiate treatment steps for youth at risk for problematic drinking. Alcohol use is common among adolescents27 and can result in injuries, death, suicidal behavior, aggression, unprotected sex, academic failure, and social problems.29 The current study links a key risk factor that exists in this study (best friends drink) and 1 of the 2 screening questions in the Alcohol Screening and Brief Intervention for Youth (do your friends drink?). It suggests that friends who drink are important for both alcohol initiation and continuing use of alcohol. Furthermore, it suggests additional questions clinicians could use (eg, family history of AD treatment and adolescent problematic behavior) to detect the risk for early AFD, by itself a risk factor for later escalation of problematic drinking.2
Acknowledgments
The Collaborative Study on the Genetics of Alcoholism (COGA), Principal Investigators B. Porjesz, V. Hesselbrock, H. Edenberg, and L. Bierut, includes 9 different centers: University of Connecticut (V. Hesselbrock); Indiana University (H.J. Edenberg, J. Nurnberger, Jr, T. Foroud); University of Iowa (S. Kuperman, J. Kramer); SUNY Downstate (B. Porjesz); Washington University in St Louis (L. Bierut, A. Goate, J. Rice, K. Bucholz); University of California at San Diego (M. Schuckit); Rutgers University (J. Tischfield); Southwest Foundation (L. Almasy), and Virginia Commonwealth University (D. Dick). A. Parsian and M. Reilly are the National Institute on Alcohol Abuse and Alcoholism Staff Collaborators and Ting-Kai Li and Robert Taylor serve as consultants. We continue to be inspired by our memories of Henri Begleiter and Theodore Reich, founding PI and Co-PI of COGA, and also owe a debt of gratitude to other past organizers of COGA, including Ting-Kai Li, P. Michael Conneally, Raymond Crowe, and Wendy Reich, for their critical contributions.
Glossary
- AD
alcohol dependence
- AFD
age of first drink
- CD
conduct disorder
- COGA
Collaborative Study on the Genetics of Alcoholism
- df
degrees of freedom
- HR
high risk
- SSAGA
Semi-Structured Assessment for the Genetics of Alcoholism
- YSR
Youth Self Report
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by National Institutes of Health grant U10AA008401 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the National Institute on Drug Abuse (NIDA). Funded by the National Institutes of Health (NIH).
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). Arlington, VA: American Psychiatric Association; 2000 [Google Scholar]
- 2.Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1997;9:103–110 [DOI] [PubMed] [Google Scholar]
- 3.Disney ER, Elkins IJ, McGue M, Iacono WG. Effects of ADHD, conduct disorder, and gender on substance use and abuse in adolescence. Am J Psychiatry. 1999;156(10):1515–1521 [DOI] [PubMed] [Google Scholar]
- 4.Grant BF. The impact of a family history of alcoholism on the relationship between age at onset of alcohol use and DSM-IV alcohol dependence: results from the National Longitudinal Alcohol Epidemiologic Survey. Alcohol Health Res World. 1998;22(2):144–147 [PMC free article] [PubMed] [Google Scholar]
- 5.Boyle MH, Offord DR, Racine YA, Fleming JE, Szatmari P, Links PS. Predicting substance use in early adolescence based on parent and teacher assessments of childhood psychiatric disorder: results from the Ontario Child Health Study follow-up. J Child Psychol Psychiatry. 1993;34(4):535–544 [DOI] [PubMed] [Google Scholar]
- 6.Clark DB, Parker AM, Lynch KG. Psychopathology and substance-related problems during early adolescence: a survival analysis. J Clin Child Psychol. 1999;28(3):333–341 [DOI] [PubMed] [Google Scholar]
- 7.Kuperman S, Chan G, Kramer JR, et al. Collaborative Study on the Genetics of Alcoholism . Relationship of age of first drink to child behavioral problems and family psychopathology. Alcohol Clin Exp Res. 2005;29(10):1869–1876 [DOI] [PubMed] [Google Scholar]
- 8.Griffin KW, Botvin GJ, Epstein JA, Doyle MM, Diaz T. Psychosocial and behavioral factors in early adolescence as predictors of heavy drinking among high school seniors. J Stud Alcohol. 2000;61(4):603–606 [DOI] [PubMed] [Google Scholar]
- 9.Kuperman S, Schlosser SS, Kramer JR, et al. Risk domains associated with an adolescent alcohol dependence diagnosis. Addiction. 2001;96(4):629–636 [DOI] [PubMed] [Google Scholar]
- 10.Bekman NM, Cummins K, Brown SA. Affective and personality risk and cognitive mediators of initial adolescent alcohol use. J Stud Alcohol Drugs. 2010;71(4):570–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Botvin GJ, Malgady RG, Griffin KW, Scheier LM, Epstein JA. Alcohol and marijuana use among rural youth: interaction of social and intrapersonal influences. Addict Behav. 1998;23(3):379–387 [DOI] [PubMed] [Google Scholar]
- 12.Capaldi DM, Stoolmiller M, Kim HK, Yoerger K. Growth in alcohol use in at-risk adolescent boys: two-part random effects prediction models. Drug Alcohol Depend. 2009;105(1-2):109–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cappell H, Greeley J. Alcohol and tension reduction: an update on research and theory. In: Blane HT, Leonard KE, eds. Psychological Theories of Drinking and Alcoholics. New York, NY: Guilford Press; 1987:15–54 [Google Scholar]
- 14.Griffin KW, Botvin GJ, Scheier LM, Diaz T, Miller NL. Parenting practices as predictors of substance use, delinquency, and aggression among urban minority youth: moderating effects of family structure and gender. Psychol Addict Behav. 2000;14(2):174–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hawkins JD, Graham JW, Maguin E, Abbott R, Hill KG, Catalano RF. Exploring the effects of age of alcohol use initiation and psychosocial risk factors on subsequent alcohol misuse. J Stud Alcohol. 1997;58(3):280–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mcculler WJ, Sussman S, Dent CW, Teran L. Concurrent prediction of drug use among high-risk youth. Addict Behav. 2001;26(1):137–142 [DOI] [PubMed] [Google Scholar]
- 17.Trucco EM, Colder CR, Wieczorek WF. Vulnerability to peer influence: a moderated mediation study of early adolescent alcohol use initiation. Addict Behav. 2011;36(7):729–736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Assanangkornchai S, Geater AF, Saunders JB, McNeil DR. Effects of paternal drinking, conduct disorder and childhood home environment on the development of alcohol use disorders in a Thai population. Addiction. 2002;97(2):217–226 [DOI] [PubMed] [Google Scholar]
- 19.Kuperman S, Schlosser SS, Lidral J, Reich W. Relationship of child psychopathology to parental alcoholism and antisocial personality disorder. J Am Acad Child Adolesc Psychiatry. 1999;38(6):686–692 [DOI] [PubMed] [Google Scholar]
- 20.Legrand LN, McGue M, Iacono WG. Searching for interactive effects in the etiology of early-onset substance use. Behav Genet. 1999;29(6):433–444 [DOI] [PubMed] [Google Scholar]
- 21.Zucker RA, Donovan JE, Masten AS, Mattson ME, Moss HB. Early developmental processes and the continuity of risk for underage drinking and problem drinking. Pediatrics. 2008;121(suppl 4):S252–S272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen X, Unger JB, Palmer P, et al. Prior cigarette smoking initiation predicting current alcohol use: evidence for a gateway drug effect among California adolescents from eleven ethnic groups. Addict Behav. 2002;27(5):799–817 [DOI] [PubMed] [Google Scholar]
- 23.Achenbach TM, Rescorla L. Manual for the ASEBA School-Age Forms & Profiles: an Integrated System of Multi-informant Assessment. Burlington, VT: ASEBA; 2001 [Google Scholar]
- 24.Begleiter H, Reich T, Hesselbrock V, et al. The Collaborative Study on the Genetics of Alcoholism. Alcohol Health Res World. 1995;19(3):228–236 [PMC free article] [PubMed] [Google Scholar]
- 25.Kuperman S, Schlosser SS, Kramer JR, et al. Developmental sequence from disruptive behavior diagnosis to adolescent alcohol dependence. Am J Psychiatry. 2001;158(12):2022–2026 [DOI] [PubMed] [Google Scholar]
- 26.Box-Steffensmeier JM, Jones BS. Event History Modeling: A Guide for Social Scientists. West Nyack, NY: Cambridge University Press; 2004 [Google Scholar]
- 27.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. National survey results on drug use from the Monitoring the Future Study, 1975–2009. In: Secondary School Students. Vol 1. NIH publication 10-7584. Bethesda, MD: National Institute on Drug Abuse; 2011 [Google Scholar]
- 28.National Institute on Alcohol Abuse and Alcoholism. Alcohol Screening and Brief Intervention for Youth: A Practitioner’s Guide Rockville, MD: National Institute on Alcohol Abuse and Alcoholism Publications Distribution Center; 2011
- 29.Brown SA, McGue M, Maggs J, et al. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics. 2008;121(suppl 4):S290–S310 [DOI] [PMC free article] [PubMed] [Google Scholar]