Abstract
This paper presents the complete report of the first Iranian Recommendations on Prevention, Evaluation and Management of High Blood Pressure. The purpose is to provide an evidence-based approach to the prevention, management and control of hypertension (HTN) by adapting the most internationally known and used guidelines to the local health care status with consideration of the currently available data and based on the locally conducted researches on HTN as well as social and health care requirements. A working group of national and international experts participated in discussions and collaborated in decision-making, writing and reviewing the whole report. Multiple subcommittees worked together to review the recent national and international literature on HTN in different areas. We used the evaluation tool that is called "AGREE" and considered a score of > 60% as a high score. We adapted the Canadian Hypertension Education Program (CHEP), the United Kingdom's National Institute for Health and Clinical Excellence (NICE) and the US-based joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC7). The key topics that are highlighted in this report include: The importance of ambulatory and self-measurement of blood pressure, evaluation of cardiovascular risk in HTN patients, the role of lifestyle modification in the prevention of HTN and its control with more emphasis on salt intake reduction and weight control, introducing pharmacotherapy suitable for uncomplicated HTN or specific situations and the available drugs in Iran, highlighting the importance of angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers and calcium channel blockers as the first line therapy in many situations, the non-use of beta blockers as the first time treatment except in specific conditions, treating HTN in women, children, obese and elderly patients, the patient compliance to improve HTN control, practical guidelines to improve the patient's information on knowing their risk and self-care as well as a quick reference guide that can serve as simplified guidelines for physicians. The working team decided to update these recommendations every two years.
Keywords: High Blood Pressure, Prevention, Treatment, Control, Iran
Introduction
Global perspective. Hypertension (HTN) is a major cause of disability recognized as a leading risk factor for death in the world, causing an estimated 7.5 million deaths per year (13% of all deaths).1 HTN is a known independent risk factor for cardiovascular (CVD) events. As blood pressure (BP) level increases, so does the risk of heart attack, heart failure, stroke and kidney disease.2 More specifically, according to data from the International Society of HTN3 on the global burden of blood-pressure-related disease, approximately 54% of stroke, 47% of ischemic heart disease and 25% of other CVD worldwide was attributable to high BP. For those ages 40 to 70, each increment of 20 mmHg in systolic BP or 10 mmHg diastolic BP doubles the risk of CVD across the BP range of 115/75 to 185/115 mm Hg.4 Elevations in BP can result in acute end-organ damage5 such as stroke, dementia and chronic kidney disease whilst lowering 5 mmHg diastolic BP is estimated to reduce the risk of stroke by 34% and ischemic heart disease by 21% from any pre-treatment level; however, there is no threshold.6 The benefits of lowering BP are well documented. Clinical trials have shown antihypertensive therapy to be associated with reducing stroke risk by 35-40%; myocardial infarction by 20-25%; and heart failure by over 50%.7
Iranian perspective. The current national picture for Iran suggests a high prevalence of CVD risk factors in both adult and younger populations. According to one study that examined risk factors in about 15,000 subjects in Tehran, aged 30 or older, 78% of men and 80% of women presented at least one CVD risk factor. Hypertension was presented in 20.4% of adults and 12.7% in children and adolescents. It was also concluded that the sustained hypertension is on the rise in younger generation of school age children.8 The national surveillance STEPwise study that was done by the Ministry of Health (MOH) demonstrated a prevalence of 25% for HTN among adults aged 25-64 years.9 On the other hand, HTN was introduces as the strongest risk factor for CVD events in an Iranian population.10
According to available data from Iran, awareness, treatment and control of hypertension is generally low. Many studies estimated the awareness and treatment of hypertension in Iranians to be approximately 50% and 35%, respectively, while the control rate for hypertension is less than 16% (Table 1).11
Table 1.
Awareness, treatment and control rates of hypertension in interventional and reference area: Isfahan Healthy Heart Program, 2001-2007
| Area | Awareness |
Treatment |
Control |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2007 | P | 2001 | 2007 | P | 2001 | 2007 | P | ||
| N = 12514 | N = 9572 | N = 12514 | N = 9572 | N = 12514 | N = 9572 | |||||
| Intervention | Urban | 404 (41.6) | 349 (48) | 0.009 | 341 (35.2) | 305 (42.5) | 0.002 | 77 (7.9) | 112 (15.6) | <0.001 |
| Rural | 107 (36.5) | 92 (58.2) | <0.001 | 100 (34.2) | 78 (49.7) | 0.001 | 12 (4.1) | 26 (16.6) | <0.001 | |
| Total | 511 (40.4) | 441 (49.8) | <0.001 | 441 (34.9) | 383 (43.8) | <0.001 | 89 (7.1) | 138 (15.8) | <0.001 | |
| Reference | Urban | 314 (44.1) | 212 (48.5) | 0.150 | 267 (37.5) | 190 (43.8) | 0.035 | 78 (11) | 71 (16.4) | 0.009 |
| Rural | 143 (37.1) | 232 (45.2) | 0.015 | 121 (31.5) | 188 (36.9) | 0.096 | 29 (7.6) | 61 (12) | 0.031 | |
| Total | 457 (41.7) | 444 (46.7) | 0.021 | 388 (35.4) | 378 (40) | 0.031 | 107 (9.8) | 132 (14) | 0.003 | |
Data are presented as number (percentage)
Two previous studies were conducted to compare the prevalence of hypertension in the rural and urban areas of Guilan and Isfahan provinces demonstrated that both systolic and diastolic BP were lower in the mountain villages and rural areas compared to cities in both sexes.12,13
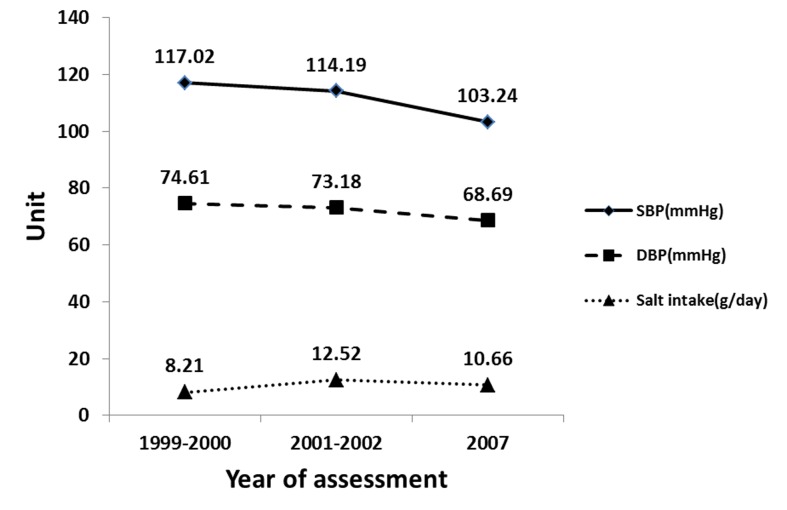
Through the education of patients and physicians, it is possible to achieve BP control in the Iranian population, just as other countries have been striving to achieve. In the US, hypertension affects an estimated 65 million people. The good news is that with implementation of national guidelines, public education programs, policies, increase the awareness, prevention, and effective treatment of hypertension significant positive results have been achieved. Hypertension control increased from 10% in NHANES II (1976-1980) to 31% a decade later (1999-2000).13 In one study in Iran, the impact of comprehensive community-based interventional strategies for CVD prevention and health promotion led to a significant reduction in blood pressure and salt intake(Figure 1).14
Figure 1.
Changes in blood pressure and salt intake during three study time points adjusted by age (Changes of all measurements were statistically significant; P < 0.01)
This document aims to provide clinicians and their patients with the necessary tools and evidence based information to better guide them in hypertension prevention and management as set forth in various guidelines from Canada, Europe, and the US. It is possible to learn from developed countries what will grant us the most success in controlling hypertension and curbing the upward trend in related cardiovascular disease in our country.
Materials and Methods
Clinical guidelines for the management of HTN have been published in various countries, including the World Health Organization's updated WHO/ISH Hypertension Guidelines (2003), the European Society for HTN (ESO), the US-based Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High BP (JNC 7), UK's National Institute for Health and Clinical Excellence (NICE) and the Canadian HTN Education Program (CHEP) Recommendations. This document draws on the evidence and wisdom of these established guidelines. The recommendations are tailored for the most part, from CHEP, NICE and JNC7 guidelines with consideration of Iranian available data and research on HTN as well as societal and health needs. A collaborative group of Iranian experts from all across the country including members from the Isfahan Cardiovascular Research Institute, Iranian Heart Association, the National Network on Cardiovascular Disease, representatives of Deputies of Health and Treatment of the Ministry of Health drafted and revised the guidelines. Executive members and internationally known HTN experts from Canada, Europe, Australia and other countries gathered to provide advice on the first national Iranian recommendations on prevention, evaluation and management of high BP. This guideline targets on general physicians, cardiologist, internists and other related specialties and was prepared in both English and Persian languages.
To develop the guideline we decided to use a comprehensive approach to review and adapt few of the most internationally known and used HTN guidelines. Therefore, we used the evaluation tool "AGREE" and considered a high score of > 60%. We adapted CHEP, NICE and JNC7 guidelines with the following outlines:
Prioritized the evidenced based recommendations
Evaluated and discussed the required field and health care gaps among the hypertension experts from all related medical specialties
Conducted a systematic evaluation of the current strategies for HTN prevention and treatment in order to ensure consistency
Considered recommendations which have flexibility to be adapted and modified for the special cases
Included the references and resources that are used
Search methods
The search strategy for this guideline was as follows:
The keywords "hypertension" and "blood Pressure" were used for search in MeSH.
In Pubmed (www.pubmed.gov) search, an advanced search setting of "practice guideline" and "guideline", all adults 19+ years, publication since 2005 on, a total number of 31 guidelines for hypertension was found.
In TRIP (www.tripdatabase.com) search, for all publication since 2005 on a total of 91 guidelines from different countries was found.
In National Guideline Clearinghouse website (www.guideline.gov) we used the keyword "hypertension" and advanced search of adults 19+ years, publication since 2005 on, "meta-analysis of RCT". A total of 13 references were found.
In Cochrane (www.cochrane.gov) when EBM guideline was searched, no guideline was found.
In NICE website (www.nice.org.uk), UK hypertension guideline was found.
No Iranian guideline on hypertension was found in manual search in the previous evidences.
From the above publications, three hypertension guidelines were selected. These three guidelines were evaluated with the "AGREE" tool by the two experts who were familiar with use of this tool. Out of the three guidelines only one rated > 60% in the "AGREE" tool. The high rated guideline then were selected.
After selection of the guideline, search was continued for all RCTs on "hypertension" in adults between years 2008 to 2011 and 47 publications were chosen.
The first draft was edited based on the searched publications and selected guideline. The draft was reevaluated with the use of "AGREE" tool and then presented in the advisory meeting.
The recommendations in this guideline are based on the scientific evidence and where there was a gap in the current evidences, the experts' panel and clinical experiences were used. Our goal is to reevaluate the current guideline in 2 years to ensure the evidences used are up-to-date and current.
This recommendation will be implemented in few sites before it is sent by the Ministry of Health to be cascaded down all over the country.
High blood pressure risk factors
Age and gender, race and ethnicity, family history, obstructive sleep apnea, lifestyle factors, salt and potassium, physical activity level and exercise, diet, medications and street drugs, kidney problems, other medical problems are all well-known risk factors for high blood pressure.15
Accurate BP measurement
-
BP measurement in the office
Blood pressure should be assessed whenever appropriate at visits, which includes when screening for hypertension, assessing cardiovascular risk and monitoring anti-hypertensive treatment. Use of standardized measurement techniques is recommended (grade D). Automated blood pressure measurements can be used in the office setting (grade D). Automated office measured systolic blood pressure (SBP) of 140 mmHg or higher or diastolic blood pressure (DBP) of 90 mmHg or higher should be considered analogous to mean awake ambulatory SBP of 140 mmHg or higher and DBP of 90 mmHg or higher, respectively (grade D).16
-
Self-measurement of BP
In much of the hypertension education information directed at consumers, a common message is "Know your numbers". Promoting awareness of hypertension and its health risks is augmented by home monitoring of BP between doctor visits. Self-measurement of BP is helpful in diagnosing hypertension. It is also a useful adjunct method of monitoring BP between in-office measurements. Regular home monitoring of BP is particularly useful for patients with diabetes mellitus, chronic kidney disease, suspected non-adherence, demonstrated white coat effect, BP controlled in the office but not at home (masked hypertension).
However, health care professionals should ensure that patients who measure their BP at home have adequate training, and if necessary, repeat training in measuring their BP. Patients should be observed to determine that they measure BP correctly and should be given adequate information about interpreting these readings.16 Patients should only use validated devices (including electronic devices), which must be regularly checked against a device of known calibration.
Home BP values for assessing white coat hypertension or sustained hypertension should be based on duplicate measures, morning and evening, for an initial seven-day period. First day home BP values should be disregarded.
Home SBP values ≥ 135 mmHg or DBP
values ≥ 85 mmHg should be considered elevated and associated with an increased overall mortality risk analogous to office SBP readings of ≥ 140 mmHg or DBP ≥ 90 mmHg.16 The method of proper self-measurement of BP is fully explained in the complete report.17
-
Ambulatory BP
Measuring ambulatory BP is useful for evaluating the possibility of office-induced, or "white coat", hypertension. When home monitoring of BP by the patient suggests white coat hypertension, its presence should be confirmed with ambulatory BP before making treatment decisions. Note that the absence of a 10-20 percent BP decrease during sleep may indicate increased CVD risk.2 Therapy adjustment should be considered in patients with a mean 24 hour ambulatory SBP of ≥ 130 mmHg or DBP of ≥ 80 mmHg or a mean awake SBP of ≥ 135 mmHg or DBP of ≥ 85 mmHg (grade C).16 After accurate BP measurement, it is classified according to table 2.
-
Identifying resistant hypertension
In some patients, high blood pressure may not respond to interventions such as lifestyle modifications and/or drug treatment. Assessing why this is happening is essential to modifying treatment recommendations to optimize the blood pressure control. A number of contributing factors may affect high BP and make it resistant to treatment, such as the improper BP measurement, excess sodium intake, inadequate diuretic therapy, medication issues (i.e. inadequate doses, drug actions and interactions), excess alcohol intake and identifiable causes of hypertension.2
Table 2.
Classification of blood pressure1
| Category | Systolic bloodpressure (mmHg) | Diastolicblood pressure (mmHg) |
|---|---|---|
| Normal | < 120 and | < 80 |
| Prehypertension | 120–139 or | 80–89 |
| Hypertension,stage 1 | 140–159 or | 90–99 |
| Hypertension,stage 2 | ≥ 160 or | ≥ 100 |
Evaluation of CVD Risk
A global cardiovascular risk should be assessed for all hypertensive patients (grade A). This approach allows a more accurate prediction of an individual's cardiovascular risk and use of more appropriate pharmacological treatment. Informing patients of their global cardiovascular risk improves effectiveness of risk factor modification and adherence to treatment (grade B). Assessment of total CVD risk should be based on epidemiologic risk factor data appropriate to the population to which it is applied.
The well-known Framingham Heart Study produced sex specific coronary heart disease risk assessment in a white middle class population. Due to its limitation in terms of generalization and the need for calibration to be used in certain populations, a new cardiovascular disease risk assessment tool was proposed by a group of Canadian and European hypertension expert.
The tool that allows clinicians to better identify patients at high total risk of developing cardiovascular disease is called Systematic Coronary Cerebrovascular Risk Evaluation (Score). The SCORE risk assessment was derived from a large dataset of prospective European studies and predicts fatal atherosclerotic cardiovascular disease over a ten-year period. This risk estimation is based on the following risk factors: gender, age, smoking, systolic blood pressure and total cholesterol. The threshold for high risk based on fatal cardiovascular events is defined as "higher than 5%", instead of the previous "higher than 20%" using a composite coronary endpoint.18
This SCORE model originally has been calibrated according to each European country's mortality statistics. In other words, if used on the entire population aged 40-65, it will predict the exact number of fatal CVD-events that eventually will occur after 10 years. This could be also adapted for Iranian population and use by our health care professionals in near future.
Laboratory Tests
In patients diagnosed with hypertension, various laboratory tests should be done at given intervals to monitor BP concerning treatment efficacy.16 In addition, testing is done to assess the possibility of target organ damage (e.g. hypertensive damage to the heart and kidneys), the presence of other diseases (e.g. diabetes) and to identify potential secondary causes of hypertension (e.g. kidney disease).19
In all patients with hypertension, routine laboratory tests should include:16
Cell blood count (grade D), urinalysis (grade D), urinary albumin excretion in patients with diabetes (grade D), biochemistry (potassium, sodium, blood urea nitrogen and creatinine) (grade D), fasting blood glucose (grade D), lipid panel including fasting serum total cholesterol and high density lipoprotein cholesterol, low density lipoprotein cholesterol and triglycerides (grade D) and standard 12-lead electrocardiography (grade C).
It is also suggested to:
Assess urinary albumin excretion in all patients (grade D)
Monitor all treated hypertensive patients for the new appearance of diabetes as per currently established diabetes guidelines (grade B)
Repeat tests during the maintenance phase of hypertension management (e.g. electrolytes, creatinine and fasting lipids) at a frequency that reflects the clinical situation (grade D)
Assess uric acid (grade D)
Secondary Hypertension
Although in more than 90% of patients with high blood pressure no underlying causes could be identified, up to 10% of hypertensives have a secondary hypertension. This emphasizes the role of screening in order to rule out underlying causes of hypertension or so-called secondary hypertension. Screening begins with a complete medical history, physical examination and laboratory investigations.20
The most common cause for secondary hypertension is chronic renal disease. Other common causes include renovascular hypertension, primary aldosteronism, and pheochromocytoma. Followings are some steps to follow when investigating the secondary causes of hypertension.
-
Kidney disease.
An elevated creatinine or reduced eGFR indicates kidney disease. Further investigations to confirm the diagnosis are kidney ultrasonography, urine analysis, electrolyte measurement and metabolic evaluation.
-
Renovascular hypertension
It is the second most common cause of secondary hypertension.21 Following findings are associated with the presence of renovascular disease:
More than 1.5 cm difference in length between the two kidneys in ultrasonography, abdominal bruit, deterioration of renal function in response to ACE inhibitors, generalized arteriosclerotic occlusive disease with hypertension, malignant or accelerated hypertension, new onset of hypertension after 50 years of age (suggestive of atherosclerotic renal stenosis), refractory hypertension, significant hypertension (diastolic blood pressure > 110 mmHg) in a young adult (< 35 years old), sudden development or worsening of hypertension.
In patients with normal renal function in initial screening test a magnetic resonance angiography and/or computed tomographic angiography of kidney is recommended as the next evaluating step. In patients with diminished renal function in initial screening a duplex Doppler ultrasonography of kidney is recommended as the next evaluating step.
-
Primary aldosteronism (PA).
If in initial screening the following conditions identified, further investigation for PA is mandatory:
Unexplained hypokalemia (spontaneous or diuretic-induced), resistant hypertension, severe hypertension (> 160 mmHg systolic or > 100 mmHg diastolic), early onset (juvenile) hypertension (< 20 years), and/or stroke (< 50 years), incidentally discovered apparently nonfunctioning adrenal mass (incidentaloma), evidence of target organ damage (left ventricular hypertrophy, diastolic dysfunction atrioventricular block, carotid atherosclerosis, microalbuminuria, endothelial dysfunction) particularly if disproportionate for the severity of hypertension.
Initial screening test after careful preparation of the patient is measurement of plasma aldosterone levels and plasma renin activity as aldosterone-to-renin ratio (ARR).
-
Pheochromocytoma.
Pheochromocytoma should be suspected in those who have one or more of the following conditions:
Hyper adrenergic spells (e.g. self-limited episodes of non-exertional palpitations, diaphoresis, headache, tremor, or pallor), resistant hypertension, a familial syndrome that predisposes to catecholamine-secreting tumors (e.g. MEN-2, NFI, VHL), a family history of pheochromocytoma, incidentaloma of adrenal, presser response during anesthesia, surgery or angiography (hypotension or hypertension with or without cardiac arrhythmia), onset of hypertension at a young age (< 20 years), idiopathic dilated cardiomyopathy, a history of gastric stromal tumor or pulmonary chondromas (carney triad), hypertension and diabetes.
Detection of secondary hypertension is important for proper management and selecting right choice of treatment.
Approach to primary prevention of hypertension
Hypertension can be prevented by complementary application of strategies that target the general population and individuals and groups at higher risk for high blood pressure. Lifestyle interventions are more likely to be successful and the absolute reductions in risk of hypertension are likely to be greater when targeted in persons who are older and those who have a higher risk of developing hypertension compared with their counterparts who are younger or have a lower risk. However, prevention strategies applied early in life provide the greatest long-term potential for avoiding the precursors that lead to hypertension and elevated blood pressure levels and for reducing the overall burden of blood pressure related complications in the community. A population-based approach that is aimed at achieving a downward shift in the distribution of blood pressure in the general population is an important component for any comprehensive plan to prevent hypertension. A small decrement in the distribution of systolic blood pressure is likely to result in a substantial reduction in the burden of blood pressure-related illness as mentioned earlier. Public health approaches, such as lowering sodium content or caloric density in the food supply, and providing attractive, safe, and convenient opportunities for exercise are ideal population-based approaches for reduction of average blood pressure in the community. Enhancing access to appropriate facilities (parks, walking trails and bike paths) and to effective behavior change models is a useful strategy for increasing physical activity in general population.22
Management of hypertension
The optimal management of hypertension includes primary prevention of CVD through lifestyle modifications as well as possibly the use of antihypertensive drug therapy. The decision to initiate pharmacological treatment and making the appropriate choice of drug(s) for each patient are guided by various criteria.
Initiate pharmacological therapy if:16
BP is ≥ 160/100 mmHg with no organ damage and no other CVD risk factors (grade A).
Diastolic BP is ≥ 90 mmHg with organ damage or other CVD risk factors; systolic BP is ≥ 140 mmHg with organ damage or other CVD risk factors (grade A).
Consider treatment in all patients with above indications regardless of age (grade B). Pay attention when managing patients who are elderly and frail.
Stage I hypertension without target organ damage or other comorbidities after 3 to 6 months of nonpharmacological treatment (grade A).
a) Setting treatment goals
Setting a blood pressure target depends on a patient's BP level (stage 1 or 2) of hypertension, as well as other medical conditions. Blood pressure targets will vary according to which of the following criteria a patient meets:16
-
Hypertension with no target organ damage or other medical condition
Target:Less than 140/90 mmHg (grade A)
-
Patients with diabetes
Target:Less than 130/80 mmHg (grade A)
-
Patients with chronic kidney disease
Target:Less than 130/80 (grade A)
Treatment compliance is a key factor in successfully meeting and maintaining of blood pressure targets. Studies showed that the good adherence to therapy is associated with lower mortality when compared to poor adherence.33 For drug therapy, single-pill antihypertensive combinations are recommended, since a simplified regimen may help increase patient treatment compliance.16
b) Lifestyle modification
Promoting and helping patients to make healthy lifestyle changes can be effective for preventing and managing hypertension, as well as for reducing cardiovascular disease risk. For patients with mild hypertension, recommending lifestyle changes may be enough to control blood pressure (grade D). Modifications can include quitting smoking, regular exercise (grade D), losing weight and reducing abdominal obesity (grade C), limiting alcohol intake (grade B) and eating a healthy diet (grade B) that is low in fat and high in fiber, decrease intake of sodium (grade B) and stress management. Losing weight, for example, can reduce blood pressure by 1.6/1.1 mmHg for every 1 kg (2.2 lb.) of weight lost.23 For patients who require treatment with medication, making lifestyle changes in addition to drug therapy, can help patients to achieve better BP control.
In addition, some patients may be motivated to make lifestyle changes if it means they can reduce or stop use of antihypertensive drug therapy. Treated patients who have a low CVD risk and well-controlled BP can be offered a trial reduction or withdrawal of therapy combined with appropriate lifestyle recommendations and continued monitoring.24
Lifestyle modifications can have a significant positive effect on blood pressure reduction:25
-
Weight reduction:
Maintain normal body weight (body mass index 18.5-24.9 kg/m2).
Average BP reduction: 5-20 mmHg/10 kg weight loss
-
Dietary sodium reduction:
Reduce dietary sodium intake to < 100 mmol per day (2.4 g sodium or 6 g sodium chloride).
Average BP reduction: 2-8 mmHg
-
DASH eating plan:
Adopt a diet rich in fruits, vegetables, and low-fat dairy products with reduced content of saturated and total fat.
Average BP reduction: 8-14 mmHg
American National Institute of Health recommended the DASH diet, which stands for dietary approaches to stop hypertension, to lower blood pressure.24 More details on DASH diet are explained in the complete report.17
-
Aerobic physical activity:
Regular aerobic physical activity (e.g., brisk walking) at least 30 minutes per day, most days of the week.
Average BP reduction: 4-9 mmHg
Aerobic type exercise is more effective than exercise type that involves resistance training, (e.g. weight lifting).26
Stress management: In patients in whom stress could be a contributing factor to their hypertension, use of relaxation technique showed to be effective (grade B).
c) pharmacologic Treatment16
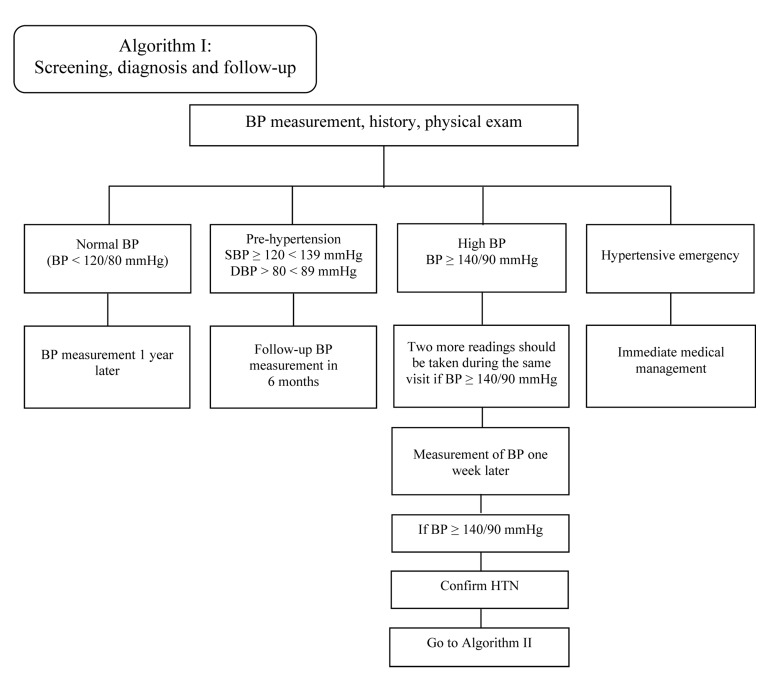
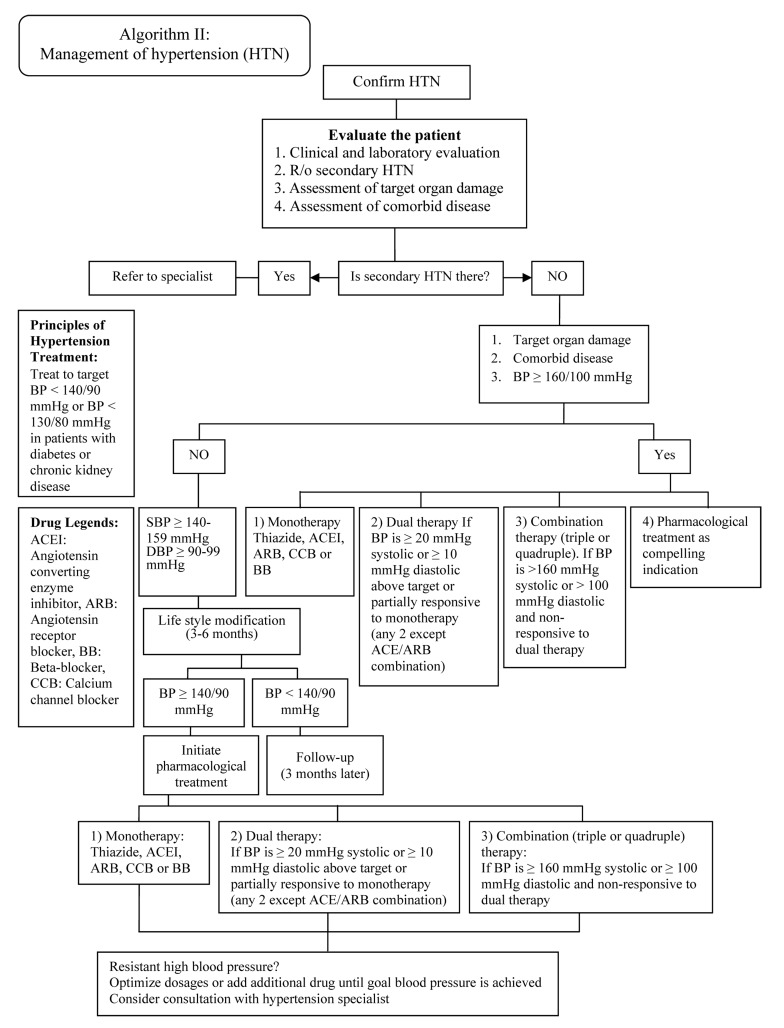
While lifestyle changes can be a very effective part of managing hypertension, patients usually need a combination of lifestyle changes and drug therapy to achieve target blood pressures. Patients often need more than one type of anti-hypertensive medication, or combination therapy to reach their blood pressure goal (See Figures 2 and 3).
Figure 2.
Algorithm I for screening and diagnosis of hypertension
Figure 3.
Algorithm II for treatment and follow-up of hypertension
Threshold BP values for pharmacological treatment indications are:27
Systolic or diastolic hypertension ≥ 160/100 mmHg
Diabetes or chronic kidney disease ≥ 130/80 mmHg
For patients at low risk with stage 1 hypertension (140-159/90-99 mmHg): Lifestyle modification can be recommended as the only therapy for the first 3 to 6 months
For patients with target organ damage (140-159/90-99 mmHg): Treat with pharmacotherapy
For patients with diabetes or chronic kidney disease with BP ≥ 130/80 mmHg: Consider pharmacotherapy
For patients with other risk factors (140-159/90-99 mmHg despite lifestyle modification): Treat with pharmacotherapy
i. Anti-hypertensive drugs and their availability in Iran
-
Angiotensin converting enzyme inhibitors (ACEIs)
ACEIs are generally well tolerated and do not have adverse effects on lipid and glucose metabolism. Their safety profile is good. ACEIs have been shown to reduce mortality and morbidity in patients with congestive heart failure and in post myocardial infarction patients with reduced left ventricular ejection fraction. In patients at increased cardiovascular risk, ACEIs have been shown to reduce morbidity and mortality as well as cardiovascular mortality in diabetic patients. In addition, they have been shown to prevent the onset of microalbuminuria, reduce proteinuria and retard the progression of renal disease as well as non-diabetic renal disease.
In patients with established vascular disease but normal left ventricular function, ACEIs reduce mortality, myocardial infarction, stroke and new onset congestive heart failure. These benefits are independent of their effects on left ventricular function and blood pressure.
Adverse effects include cough and, rarely, angioedema. In patients with renovascular disease or renal impairment, deterioration in renal function may occur. Serum creatinine should be checked before initiation and repeated within one to two weeks after initiation (for 2 months then longer). Any increase should be confirmed immediately and monitored. If there is a rise of serum creatinine of more than 30% from baseline within two months, ACEIs should be stopped. ACEIs may increase fetal and neonatal mortality and therefore are contraindicated in pregnancy, and should be avoided in those planning pregnancy (Table 3).
-
Angiotensin receptor blockers (ARBs)
ARBs are drugs that specifically block angiotensin II receptor. Unlike ACEIs, persistent dry cough is less of a problem. ARBs are recommended in ACEI intolerance patients. As with ACEIs, they are contraindicated in pregnancy and bilateral renal artery stenosis. ARBs are effective in preventing progression of diabetic nephropathy and may reduce the incidence of major cardiac events in patients with heart failure hypertensive LVH and diastolic heart failure. The Blood Pressure Lowering Treatment Trialist Collaboration (BPLTTC) in a meta-analysis of 21 randomized trial found that there were no clear differences between ACEIs and ARBs for the outcomes of stroke and heart failure. Combination of ARBs and ACEIs are not recommended except for reducing proteinuria (Table 4).
-
Calcium channel blockers (CCBs)
Long-acting CCBs have been shown to be safe and effective in lowering blood pressure, both as first-line agents and in combination with other classes of antihypertensive drugs (Table 5). There are three major classes of CCBs (phenylalkylamines, dihydropyridines and benzothiazepines) with different characteristics and all are effective in lowering BP. With few exceptions, they have no undesirable metabolic effects and their safety profile in hypertension is good. Long-acting dihydropyridine CCBs are particularly effective in reducing isolated systolic hypertension. They are also effective in reducing cerebrovascular events by 10% compared with other active therapies. Short acting CCBs are no longer recommended and should be phased out. The use of sublingual nifedipine is also discouraged. Long acting CCBs may also be useful in treating hypertensives with coronary heart disease. Adverse effects include initial tachycardia, headache, flushing, constipation and ankle edema. Unlike other dihydropyridine CCBs, verapamil may reduce heart rate and care should be exercised when used with betablockers.
-
β-Blockers
β-blockers have long been established in the treatment of hypertension. They are particularly useful in hypertensive patients with effort angina, tachyarrhythmias or previous myocardial infarction where they have been shown to reduce cardiovascular morbidity and mortality. Certain beta-blockers such as carvedilol (beta- and alpha-blocker), bisoprolol and long-acting metoprolol have been shown to be beneficial in patients with heart failure. Beta-blockers are absolutely contraindicated in patients with active obstructive airways disease and heart block (2nd and 3rd degree) and have relative contraindication in peripheral arterial disease and first-degree AV block. They are generally well tolerated. Adverse effects reported include dyslipidemia, masking of hypoglycaemia, increased incidence of new onset diabetes mellitus, erectile dysfunction, nightmares and cold extremities. However, with the advent of newer antihypertensive agents with better efficacy and better safety profile, concern has been voiced over their widespread use in the treatment of hypertension (Table 6).
-
Diuretics
The use of diuretics is well established in the treatment of hypertension (Table 7). Thiazide diuretics are especially cheap and are one of the most widely used antihypertensive agents. When used in patients with essential hypertension and relatively normal renal function, thiazides are more potent than loop diuretics to decreased hypertension. However, in patients with renal insufficiency (serum creatinine 2.5 mg/dl), thiazides are less effective and loop diuretics should be used instead. Diuretics may be used as initial therapy. They also enhance the efficacy of other classes of antihypertensive drugs when used in combination. In the elderly with no co-morbid conditions, diuretics are the drugs of choice in the treatment of systolic-diastolic hypertension and isolated systolic hypertension. Diuretics not only reduce the incidence of fatal and non-fatal strokes but also cardiovascular morbidity and mortality. Thiazide diuretics should be used with care in patients with gout with an absolute contraindication in patients presenting with active gout as they may precipitate an acute attack. Potassium-sparing diuretics may cause hyperkalemia if given together with ACEIs or ARBs or in patients with underlying renal insufficiency. Aldosterone antagonists and potassium sparing diuretics should be avoided in patients with serum potassium > 195 mg/L. Adverse effects are uncommon, unless high doses are used. These include increased serum triglyceride, glucose and uric acid; decreased potassium, sodium and magnesium levels and erectile dysfunction. Serum electrolytes, in particular potassium, should be closely monitored.
-
The α-blockers and the combined α-‚ β-blockers
The peripheral α1-adrenergic blockers lower BP by reducing peripheral resistance. They also reduce prostatic and urethral smooth muscle tone and provide symptomatic relief for patients with early benign prostatic hypertrophy (BPH). They should be the logical choice for hypertensive patients with BPH. The use of non-specific α-adrenergic blockers like phentolamine and phenoxybenzamine has been restricted to the treatment of pheochromocytoma (Tables 8-10).
Alpha-1 adrenergic blockers have favorable effects on lipid metabolism. However, postural hypotension is a known side effect, especially at initiation of therapy. Combined α‚ β-blockers offer enhanced neurohormonal blockade. Labetalol has been in use for over 20 years and is safe in pregnancy. Its intravenous formulation is useful in hypertensive emergencies, including pre-eclampsia and eclampsia. Carvedilol has been shown to be effective in hypertension and to improve mortality and morbidity in patients with heart failure. In addition, it has no adverse effects on insulin resistance and lipid metabolism. However, its safety in pregnancy has not been established. Table 9 shows direct vasodilators which used in hypertension treatment.
In some patients treated once daily, the antihypertensive effect may diminish towards the end of the dosing interval (trough effect). Blood pressure should be measured just prior to dosing to determine if satisfactory blood pressure control is obtained. Accordingly, an increase in dose or frequency may need to be considered. Appropriate drug choices in hypertensive patient with compelling indication are presented in table 11.
Table 3.
Angiotensin-converting enzyme inhibitors available in Iran
| Drug | Drug form | Initial dosage | Maximum Dose | Daily dose frequency |
|---|---|---|---|---|
| Captopril | Tab (25 mg, 50 mg) | 25 mg | 100 mg* | 2 |
| Enalapril | Tab (5 mg, 20 mg) | 5 mg | 40 mg | 1-2 |
| Lisinopril | Tab (10 mg, 20 mg) | 10 mg | 40 mg | 1 |
In patients with congestive heart failure, maximum daily dose could be 50 mg three times daily (TID)
Tablet
Table 4.
Angiotensin receptor blockers available in Iran
| Drug | Drug form | Initial dosage | Maximum dose | Daily dose frequency |
|---|---|---|---|---|
| Losartan | Tab (25 mg, 50 mg) | 25 mg | 100 mg | 1-2 |
| Valsartan | Tab (80 mg, 160 mg) | 80 mg | 320 mg | 1-2 |
| Telmisartan | Tab (80 mg) | 80 mg | 80 mg | 1 |
Tablet
Table 5.
Calcium channel blockers available in Iran
| Drug | Drug form | Initial dosage | Maximum dosage | Daily dose frequency |
|---|---|---|---|---|
| Dihydropyridine calciumchannel blockers | ||||
| Amlodipine | Tab long acting (5 and 10 mg) | 2.5 mg | 10 mg | 1 |
| Nifedipine | Extended release Cap (20 mg) | 30 mg | 60 mg | 1 |
| Non-dihydropyridine calciumchannel blockers | ||||
| Verapamil | Immediate release Tab (40 mg) | 80 mg | 320 mg | 2-3 |
| Diltiazem | Immediate release Tab (60 mg) | 30 mg | 60 mg | 3 |
| Extended release Tab (120 mg) | 120 mg | 540 mg | 1 | |
Tab: Tablet; Cap: Capsule
Table 6.
β-Blockers available in Iran
| Drug | Drug form | Initial dosage | Maximum dose | Daily dose |
|---|---|---|---|---|
| Atenolol* | Tab (50 mg, 100 mg) | 25 mg | 100 mg | 1 |
| Metoprolol* | Immediate release Tab (50 mg) | 50 mg | 200 mg | 1-2 |
| Extended release Tab (47.5 mg) | 47.5 mg | 190 mg | 1 | |
| Propanolol** | Tab (10 mg, 20 mg, 40 mg) | 40 mg | 160 mg | 2 |
| Carvedilol§ | Tab (6.25 mg, 12.5 mg, 25 mg) | 6.25 mg | 50 mg | 2 |
Selective β1–Blocker
Non-Selective β1–Blocker
If patient's weight ≥ 70 kg, carvedilol dosage is 50 mg twice a day
Tab: Tablet
Table 7.
Diuretics available in Iran
| Drug | Drug form | Initial dose | Maximum dose | Daily dose frequency |
|---|---|---|---|---|
| Hydrochlorothiazide | Tab (50 mg) | 12.5 mg | 50 mg | 1 |
| Triamterene/ Hydrochlorothiazide | Tab (50 mg/25 mg) | 1 tab/daily | 2 tab/daily | 1-2 |
| Furosemide | Tab (40 mg) injection(20 mg, 40 mg) | |||
| Spironolactone | Tab (25 mg) | 25 mg | 50 mg | 1-2 |
Tab: Tablet
Table 8.
Centrally acting adrenergic receptor agonists available in Iran
| Drug | Drug form | Initial dosage | Maximum dose | Daily dose frequency |
|---|---|---|---|---|
| Clonidine (Catapres) | Tab (0.2 mg) | 0.1 mg | 0.8 mg | 2 |
| Methyldopa | Tab (250 mg) | 250 mg | 1000 mg | 2 |
Tab: Tablet
Table 10.
α-Blockers Available in Iran
| Drug | Drug form | Initial dosage | Maximum dose | Daily dose frequency |
|---|---|---|---|---|
| Prazosin | Tab (1 mg, 5 mg) | 2 mg | 20 mg | 2-3 |
| Trazocin | Tab(2 mg, 5 mg) | 1 mg | 20 mg | 1-2 |
Tab: Tablet
Table 9.
Direct vasodilators available in Iran
| Drug | Drug form | Initial dose | Maximum dose | Daily dose frequency |
|---|---|---|---|---|
| Hydralazine* | Tab (10 mg, 25 mg, 50 mg) | 25 mg | 100 mg | 2 |
| Minoxidil* | Tab (10 mg) | 2.5 mg | 80 mg | 1-2 |
It is recommended to use in combination with diuretics and B Blockers
Tab: Tablet
Table 11.
Choice of drug therapy in hypertensive patients with comorbid conditions - drugs that may have favorable effect on comorbid conditions
| Conditions | Drugs | Comments |
|---|---|---|
| Diabetes with proteinuria | ACEI, ARB,low dose diuretics,and longacting CCBs | |
| Stable Angina | β-blockersand CCBs, ACEI, ARB | If LVEF <30% verapamil and diltiazem should be avoided |
| Heart Failure | ACEI, ARB,carvedilol, sustained release metoprolol, diuretics | |
| Supraventricular tachycardia | β-blockersand non DHP CCBs | |
| Cough from ACEI | ARBs | ARBs couldbe used as substitution for ACEIs |
| Gout | ACEI, ARB,CCBs and β-blockers | |
| Dyslipidemia | ACEI, ARB,CCBs and α-blockers | |
| Essential tremor | Non-selective β-blockers | |
| Hyperthyroidism | Β-blockers | |
| Peripheral Vascular Disease | CCBs, ACEI,ARB | |
| Migraine | Β-blockersCCBs | |
| Osteoporosis | Thiazidediuretics | |
| Perioperative hypertension | Β-blockers | |
| Acute coronary syndrome | Β-blockers,ACEI, ARB | Ifβ-blockers are contraindicated, long acting DHP CCBs should be used. |
| Prostatism | Α-blockers | |
| Renal Insufficiency | ACEI, ARB,thiazide, loop diuretics | ACEI and ARBare contraindicated in bilateral renal artery stenosis |
| Elderly (> 65 years old) with no comorbid diseases | Diuretics,CCBs, ARBs, ACEI |
ACEI: Angiotensin-converting enzyme inhibitors, ARB: Angiotensin receptor blockers, CCB: Calcium channel blockers, DHP:
ii. Pharmacotherapy in patients with no additional risk factors or disease (Target < 140/90 mmHg)
-
Diastolic +/- systolic hypertension, isolated systolic hypertension, isolated diastolic hypertension
Initial therapy: Monotherapy with thiazide diuretics (grade A), ACEIs (grade B), ARBs (grade B), or long-acting CCBs (grade B); ASA and statins may be considered for selected patients. Use of beta-blockers is not recommended in patients unless there are other indications (grade B).
Second-line therapy: If target levels are not achieved using monotherapy, other first-line agents can be used in combination (grade B), such as a thiazide diuretic (grade B) or CCBs (grade B) with either ACEI, ARB or beta-blocker. For the third choice of therapy, it may be needed to ensure that diuretics are included.
Additional notes: Caution is required when prescribing to women of childbearing potential as ACEIs, ARBs and direct renin inhibitors are potential teratogens. It is not recommended to combine an ACE inhibitor with an ARB except for special situation that will be judged by specialists (grade A).
Combination therapy using two first line agents may also be considered as initial treatment of hypertension (grade C) if systolic BP is 20 mmHg above target or if diastolic BP is 10 mmHg above target. Caution should be exercised in frail and elderly patients when using combination therapy fist line. Combination of an ACE inhibitor (or an ARB) and a dihydropyridine CCB is preferred to an ACE inhibitor (or an ARB) and hydrochlorothiazide (grade A).
-
Global vascular protection treatment for hypertensive adults with no additional disease
Statin therapy is recommended in hypertensive patients with three or more cardiovascular risk factors in patients older than 40 years old (grade A) or in patients with established atherosclerotic disease regardless of age (grade A).
Strong consideration should be given to the addition of low does acetylsalicylic acid therapy in hypertensive patients (grade A). In patients older than 50 years old caution should be exercised if BP is not controlled (grade C).
iii. Pharmacotherapy in patients with additional risk factors or diseases
In HTN patients with comorbid conditions like diabetes, coronary artery disease, heart failure, left ventricular hypertrophy, new or past stroke or transient ischemic attack, kidney diseases and peripheral vascular diseases there are specific recommendations as first or second line therapies, all presented in the full report17 and briefly presented here (Table 12).
Table 12.
Choice of drug therapy in patients with comorbid conditions - drugs that may have unfavorable effect on comorbid conditions
| Conditions | Drug |
|---|---|
| Bronchospasm | β Blockers |
| Bilateral renal vascular disease | ACEI, ARB |
| Depression | Central α-agonists (Reserpine) |
| Diabetes type I and II | β-blockers, high dose diuretics |
| Heart block 2° or 3° | Β-blockers and non-DHP CCBs |
| Heart failure | CCBs (except long acting DHP) |
| Hyperkalemia | ACEI, ARB, aldosterone blockers |
| Gout | Hydrochlorothiazide |
| Liver disease | Labetalol, methyldopa |
| Peripheral vascular disease | β-blockers |
| Pregnancy | ACEI,* ARB* |
| Renal insufficiency | Potassium sparing agents, aldosterone blockers |
Contraindicated
ACEI: Angiotensin-converting enzyme inhibitors, ARB: Angiotensin receptor blockers, CCB: Calcium channel blockers, DHP: Dihydropyridine
-
High blood pressure in paediatrics
The presence and need for management of modifiable cardiovascular risk factors, such as hypertension, dyslipidemia, diabetes and obesity, in the pediatric population is becoming increasingly apparent. Obesity in childhood is predictive of obesity in adulthood, and is a major cardiovascular risk factor. While childhood obesity is most widespread in the most industrialized countries, it is also becoming a fast-growing problem in developing countries, such as Iran.27 The childhood obesity epidemic appears to be associated with the increasing prevalence of HTN.
Systolic blood pressure has been recognized as a stronger predictor of mortality than diastolic blood pressure in middle aged and older adults. However, in younger population, isolated diastolic hypertension is more common. According to some studies, elevated diastolic blood pressure (with a risk threshold of 90 mmHg) in adolescent males was more consistently related to mortality than systolic hypertension.28
Hypertension guidelines such as the European Society of Hypertension (2009) and the US (JNC 7) have recognized the significance of hypertension in children and adolescents, and how it contributes to the growing burden of cardiovascular disease worldwide.
Pediatric BP targets are:29
In general:
BP < 90th age, sex and height specific percentile
BP < 75th percentile in children without proteinuria
BP < 50th percentile in cases of proteinuria
24-hour ambulatory BP (ABP) measurements is strongly recommended
Most common causes of hypertension by age group in pediatrics are presented in the full report.17
-
High blood pressure in obesity
Recent epidemiological studies have revealed that the prevalence of obesity in Iran is equal to or higher than Europe and the United States and it is the primary cause of the rising prevalence of important comorbid states such as hypertension, cardiovascular and renal disease. This is also in line with the present etiologies of death in Iran with cardiovascular disease and cancer accounting for nearly 60% of causes of non-traumatic death. The prevalence of obesity in Iran has reached epidemic proportions and is specifically affecting women and younger age groups too. Increasing prevalence of obesity and metabolic syndromes might therefore be expected. Thus, it is not surprising that death from cardiovascular diseases is presently the most common cause of mortality in Iran and constitutes 45% of etiologies for all types of death in this country. Different age and sex groups lead to large variation in the prevalence of obesity in Iran. The prevalence of obesity in those less than 18 year olds was about 5.5% and 21.5% in the older group. In adults, women reported higher prevalence of obesity in comparison to men. The difference between women and men regarding obesity prevalence was increased by age.30-40
Obesity (body mass index ≥ 30 kg/m2) in hypertensive patients presents a unique challenge to optimal management of blood pressure. It is an increasingly common risk factor for both hypertension and CVD. The overall prevalence of hypertension increases in relation to rising obesity levels.41 In treated patients, obesity may be associated with poor response to antihypertensive therapy16 and can be a secondary cause of resistant hypertension. An epidemiological study found that as weight increased, greater levels of BP (from 145.5/84.5 to 149.5/89 mmHg), worse control over BP (from 29.6% to 15.4%) and a greater prevalence of metabolic syndrome (from 20.8% to 66.9%) were observed.42 In addition, an increase in both body mass index and abdominal obesity was associated with worse control of BP. Reducing abdominal obesity and achieving a healthy weight should be encouraged in all hypertensive patients.
-
High blood pressure in elderly
Hypertension in elderly might deserve more attention. Hypertension occurs in more than two-thirds of individuals after age 65 years and is the population with the lowest rates of BP control. Treatment recommendations for older people with hypertension, including those who have isolated systolic hypertension, should follow the same principles outlined for the general care of hypertension. However, when treating the elderly for hypertension, it is also necessary to consider the other medical conditions that they may have. Some of these conditions may make the patients more prone to side effects from the medications. It is recommended that the antihypertensive medications be started at low doses and increased slowly to avoid a too rapid or excessive lowering of blood pressure; however, standard doses and multiple drugs are needed in the majority of older people to reach appropriate blood pressure targets.2
-
High blood pressure in sleep apnea
The seventh report of the Joint National Committee2 identified obstructive sleep apnea as an important identifiable cause of hypertension. As many as half of all patients with sleep apnea may have underlying hypertension, and many patients with hypertension, particularly resistant hypertension, may have obstructive sleep apnea. In fact, there seems to be an interaction between obstructive sleep apnea severity and resistance to antihypertensive medications. The first-line treatment for obstructive sleep apnea-induced hypertension is treatment of sleep apnea and antihypertensive medications as indicated. The most effective methods of treatment of sleep apnea include continuous positive airway pressure, postural adjustments and weight control. Tracheostomy is considered a last resort in difficult-to-treat, medically complicated obstructive sleep apnea.43
-
High blood pressure in women
In women, use of oral contraceptive pills may increase blood pressure and the risk of hypertension increases with duration of use. Therefore, in women taking oral contraceptives, regular blood pressure measuring should be conducted. In women with hypertension or the risk of development of hypertension, other forms of contraception might be considered. In contrast, menopausal hormone therapy does not raise blood pressure.
Women with hypertension who become pregnant should be followed carefully because of increased risks to mother and fetus. Methyldopa, β-blockers, and vasodilators are preferred medications for the safety of the fetus. ACEIs and ARBs should not be used during pregnancy because of the potential risk for the fetus and should be avoided in women who are likely to become pregnant.
Preeclampsia, which occurs after the 20th week of pregnancy, is characterized by new-onset or worsening hypertension, albuminuria, and hyperuricemia, sometimes with coagulation abnormalities. In some patients, preeclampsia may develop into a hypertensive urgency or emergency and may require hospitalization, intensive monitoring, early fetal delivery, and parental antihypertensive and anticonvulsant therapy.2
Hypertension crisis
Definition
Hypertensive crisis is defined as acute (severe, rapid) elevation of BP, with a systolic blood pressure usually greater than 180 mmHg (in HTN emergency it is often higher than 220 mmHg) or a diastolic blood pressure greater than 110 mmHg (in HTN emergency it is often higher than 120 mmHg). The rapidity of the rise may be more important than the absolute level in producing acute vascular damage.
Hypertensive crisis is divided into two categories based on the presence or absence of target organ damage (TOD). When acute evidence of impending or ongoing damage of a target organ (i.e. cardiovascular, renal, central nervous system) is present, the condition is considered a hypertensive emergency and the rapid reduction of BP is indicated to minimize TOD. Examples include hypertensive encephalopathy, intracranial hemorrhage, acute myocardial infarction, unstable angina, acute left ventricular failure with pulmonary edema, dissecting aneurysm, acute renal failure and eclampsia of pregnancy.
If no acute clinical evidence of TOD is present in patients with severely elevated BP, the condition is considered hypertensive urgency. In this situation, evidence of TOD is often present, but non-progressive. Examples include upper levels of stage II hypertension (usually higher than 180/110 mmHg) associated with severe headache, shortness of breath, epistaxis, pedal edema, severe anxiety.
Accelerated hypertension is defined as a recent significant increase over baseline BP that is associated with TOD. This is usually seen as vascular damage on funduscopic examination, such as flame-shaped hemorrhages or soft exudates, but without papilledema. In contrast to hypertensive emergency, no evidence suggests a benefit from rapid and aggressive reduction in BP in patients with hypertensive urgency. In fact, such aggressive therapy may harm the patient, resulting in cardiac, renal, or cerebral hypoperfusion.
The primary goal of the emergency physician is to determine which patients with acute hypertension are exhibiting symptoms of end-organ damage and require immediate intravenous (IV) parenteral therapy. In contrast, patients presenting with acutely elevated BP without symptoms should have initiation of medical therapy and close follow-up in the outpatient setting. The emergency physician must be capable of appropriately evaluating patients with an elevated BP, correctly classifying the hypertension, determining the aggressiveness and timing of therapeutic interventions, and making disposition decisions.
Etiology
The rapidity of onset suggests a triggering factor superimposed on pre-existing hypertension. Most patients with a HTN crisis have already diagnosed but uncontrolled (primary) hypertension and have recent or abrupt discontinuation of previously prescribed antihypertensive therapy or have poor adherence to the medications. The lack of a primary care physician and failure to adhere to prescribed antihypertensive regimens are major risk factors for hypertensive emergencies.
History and physical examination
The symptoms and signs of hypertensive crises vary from patient to patient (Table 13). The most common presentations of hypertensive emergencies at an emergency room are neurologic symptoms and signs of hypertensive encephalopathy (headache, altered level of consciousness) and/or focal neurologic signs or cerebral infarction, acute left ventricular failure (pulmonary edema or merely dyspnea) and coronary ischemic syndromes (chest discomfort, acute myocardial infarction). In some patients, severe injury to the kidneys may lead to acute renal failure with oliguria and/or hematuria.
Table 13.
Clinical characteristics of the hypertensive crisis
| Blood pressure (mmHg) | Usually > 220/120-140 mmHg |
| Funduscopic findings | Retinal changes grade III (hemorrhages, exudates), or grade IV(papilledema) |
| Neurologic status | Headache, confusion, somnolence, stupor, visual loss, seizures,focal neurologic deficits, coma |
| Cardiac findings | Prominent apical pulsation, cardiac enlargement, congestive heartfailure |
| Renal symptoms | Azotemia, proteinuria, oliguria |
| Gastrointestinal symptoms | Nausea, vomiting |
| Hematologic findings | Microangiopathic hemolysis |
A patient with hypertension emergencies almost always has retinal papilledema as well as flame-shaped hemorrhages and exudates.
BP must be checked in both arms to screen for aortic dissection. Furthermore, screen for carotid or renal bruits, palpate the precordium, looking for sustained left ventricular lift; and auscultate for a third or fourth heart sound or murmurs (Table 14).
Table 14.
The evaluation of hypertension urgency and emergency
| Parameter | Severe hypertension (Urgency) |
Hypertension emergency | |
|---|---|---|---|
| Asymptomatic | Symptomatic | ||
| Blood pressure | > 180/110 mmHg | > 180/110 mmHg | Usually ≥ 220/140 mmHg |
| Symptoms | Headache, anxiety, often asymptomatic | Severe headache, shortness of breath, nose bleeding | Shortness of breath, chest discomfort, nocturia, dysarthria,weakness, altered consciousness |
| Examination | No TOD, no clinical cardiovascular disease | TOD; clinical cardiovascular disease present, stable | Encephalopathy, pulmonary edema, renal insufficiency,cerebrovascular accident, cardiac ischemia |
| Therapy | Observe 1-3 hours, initiate or resume medication, increase dosage ofinadequate agent | Observe 3-6 hours, lower BP with short-acting oral agent, adjustcurrent therapy | Baseline laboratory tests, intravenous line, monitor BP, mayinitiate parenteral therapy in emergency room |
| Plan | Arrange follow-up within 3-7 days | Arrange follow-up evaluation in less than 72 hours | Immediate admission to critical care unit, treat to initial goal BP,additional diagnostic studies |
TOD: Target organ damage
Laboratory evaluation
A complete blood count and smear (to exclude a microangiopathic anemia), electrolytes, blood urea nitrogen, creatinine, urinalysis (to evaluate for renal impairment), and electrocardiogram should be obtained in all patients. Chest radiography should be obtained in patients with shortness of breath or chest pain, and a brain computed tomography scan should be obtained in patients with neurologic symptoms. In patients with unequal pulses and/or evidence of a widened mediastinum on the chest radiograph, a chest computed tomography or magnetic resonance imaging should be considered.
Medical management
An important point to remember in the management of the patient with any degree of BP elevation is to "treat the patient and not the number" and the Hippocratic edict "first, do no harm" is advisable.
Patients with hypertension emergencies are usually admitted to a critical care unit for continuous cardiac monitoring, frequent assessment of neurologic status and urine output, and administration of intravenous antihypertensive medications and fluids.
On the other hand, patients with hypertensive urgencies do not mandate admission to the hospital. The goal of therapy in these cases is to reduce BP within 24 hours, which can be achieved as an outpatient.
The initial goal of treatment in hypertension emergencies is to reduce the mean arterial pressure by no more than 25% within 30-60 minutes and, then if stable, to reach a goal BP of 160/100-110 mmHg within 2 to 6 hours. However, the BP should not be lowered to normal levels at first 24 hours.43 If this level of BP is well tolerated and the patient is clinically stable, further gradual reductions toward a normal BP can be implemented in the next 24-48 hours. There are exceptions to this rule:
Acute ischemic stroke: Excessive or rapid reductions in BP should be avoided in acute stroke. In patients with intracerebral hematomas, the controlled lowering of the BP is currently recommended only when the SBP is > 200 mmHg or the DBP is > 110 mmHg.44
Aortic dissection: In these patients, the SBP should be lowered to below 100-110 mmHg if tolerated within 10-20 minutes.
Patients who urgently need thrombolytic therapy must have their BPs lowered sufficiently, and it should be lowered to 160/110 mmHg before initiating thrombolytics.
In hypertensive urgency, goal of lowering of BP by about 20% should be achieved over 24 to 48 hours and it makes sense to initiate a medication that will be indicated for long-term use. Excessive falls in pressure that may precipitate renal, cerebral, or coronary ischemia should be avoided. For this reason, short-acting nifedipine (oral and sublingual) is no longer considered acceptable in the initial treatment of hypertensive emergencies or urgencies and are not recommended. Clonidine and angiotensin-converting enzyme inhibitors are long acting and poorly titratable, but these agents are particularly useful in the management of hypertensive urgencies.
Critical care nurses should monitor BP every 5 to 10 minutes until goals are reached.
As mentioned, most patients with hypertensive emergencies are volume depleted. After initial reduction of BP, gentle volume repletion with intravenous crystalloid will serve to restore organ perfusion and prevent the precipitous fall in blood pressure that may occur with antihypertensive therapy.44 Oral therapies can be started as the intravenous agents are slowly titrated down.
To follow and reassess, the next visit should be done for all of the patients within 1-2 weeks to ensure that the BP is improving and there are no further complications of uncontrolled hypertension.
In pregnant patients, SBP persistently ≥ 180 mmHg or DBP persistently ≥ 110 mmHg (105 mmHg in some institutions) are considered hypertensive crises (hypertensive emergency) and require immediate pharmacologic management using intravenous drugs. In the vast majority of the cases, this process can only be terminated by delivery.44 Before delivery, it is desirable to maintain the DBP greater than 90 mmHg in these patients because this pressure allows for adequate utero-placental perfusion, and prevents acute fetal distress and progressing to an in utero death or to perinatal asphyxia.44
Treatment
No single ideal agent exists. Drugs are chosen based on their rapidity of action, ease of use, special situations, and convention as well as the target organ that is involved.44 In selected hypertensive emergency settings, choice drugs and target BP are presented in table 15. All treatment agents whether intravenous or oral ones, their dose, side effects and contraindications are presented in the full report.17
High blood pressure in perioperative patients
Peri-operative hypertension is commonly encountered in patients who undergo surgery. Despite many attempts in order to standardize the method to characterize the intraoperative hemodynamics, these methods still vary widely. In addition, there is a lack of consensus concerning treatment thresholds and appropriate therapeutic targets, which makes absolute recommendations about treatment difficult. Nevertheless, perioperative hypertension requires careful management. When treatment is necessary, therapy should be individualized for the patients.
The goal of controlling perioperative hypertension is to protect organ function, and is currently recommended based on the assumption that the risk of complications will be reduced and outcomes improved. However, the treatment of acute elevations in blood pressure (defined as an increase in systolic BP, diastolic BP, or mean arterial pressure by > 20% over baseline in the perioperative period) is without a uniform approach. In general, the treatment goal should be based on the patient's preoperative BP. A conservative target would be approximately 10% above that baseline; however, a more aggressive approach to lowering blood pressure may be warranted for patients at very high risk of bleeding or with severe heart failure who would benefit from afterload reduction. Careful monitoring of patient response to therapy, and adjustment of treatment, are paramount to safe and effective treatment of perioperative hypertension. After surgery, the clinician can safely transmit the patient to an effective oral antihypertensive regimen to manage the long-term risks of hypertension and cardiovascular diseases. The ideal choices, methods of administration and new agents are explained in the full report.17
How to improve patient compliance
Poor adherence to prescribed therapies is common in patients with hypertension, and should be considered in the evaluation of the hypertensive patient with poor blood pressure control. When initiating treatment in patients newly diagnosed with hypertension and when monitoring patients with existent disease, providers should identify barriers to medication adherence and actively engage patients in shared decision-making regarding their treatment. These activities will facilitate adherence, which may lead to improved outcomes for patients with hypertension and other chronic cardiovascular diseases.
When possible, the following strategies may be of help in improving patient compliance: simplifying the prescribed medication to once daily dosing, replacing multiple pill antihypertensive combinations with single pill combinations, educating patients and their families about their disease and prescribed medication, assessing adherence to pharmacological and non-pharmacological treatment in each office visit.
When to refer to specialists
Most patients can be effectively managed by the general practitioners; some patients however, should be referred to the specialist for further assessment and appropriate management. Patients with the following conditions are recommended to be referred to appropriate specialists:
Patient with accelerated or malignant hypertension, that blood pressure is usually higher than 180/110 mmHg, with signs of papilledema and/or retinal hemorrhage.
Patient with resistant hypertension in whom hypertension may often be associated with subclinical organ damage and added cardiovascular risk.
If blood pressure goals are not achieved within 6 months, or a previously good control is lost.
Pregnant women with hypertension should be referred to an obstetrician for further management.
De novo onset of hypertension or aggravation of BP levels during the postpartum period, especially if there is significant proteinuria.
Patient with recent onset of target organ damage
Children < 18 years old
Younger patients (i.e. < 40 years) with uncomplicated stage 1 hypertension also are recommended to refer to a specialist for exclusion of secondary causes of hypertension and detailed evaluation of target organ damage.
Hypertensive patients who do not reach targets or whose HDL-cholesterol or triglyceride levels remain abnormal
Patient information
For patients, understanding why they need to monitor, prevent, and manage high blood pressure is a challenge. Since elevated BP does not usually produce any symptoms, it is not the kind of ailment that convinces patients to see their physician, such as a pain condition. Because hypertension is a silent condition, physicians need to impress upon patients how it relates to cardiovascular risk and other diseases. A quick, simple and practical educational package targeting patients and their families have accompanied these recommendations with the main goals of:
The whole educational package was introduced in the full report.17
Even if you already have high blood pressure, healthy lifestyle measures can help you to control it better and maybe even reduce or remove the need for blood-pressure medication. Managing your blood pressure can also help you prevent cardiovascular disease and other health conditions so you can be healthier for longer.
Table 15.
Preferred drugs for selected hypertensive emergencies
| Emergency | Drugs of choice | Target blood pressure |
|---|---|---|
| Cerebrovascular situations | ||
| Hypertensive encephalopathy (manifestations of cerebral edema) | -Labetalol-Esmolol-Nitroprusside (only if necessary) | 20-25% in 2-3 hours |
| Subarachnoid hemorrhage | -Nimodipine-Labetalol | 20-25% in 2-3 hours |
| Ischemic stroke | -Nimodipine-Labetalol | 10–15% in the first 24 hours |
| Cardiac situations | ||
| Aortic dissection | -Nitroprusside + beta blockers (esmolol, labetalol) | 100-110 mmHg SBP as soon as possible |
| Acute coronary syndrome | -Beta blocker-Nitroglycerin | Secondary to ischemia relief |
| Pulmonary edema with systolic dysfunction | -Nitroglycerin + loop diuretic | Improve symptoms 10-15% in 1-2 hours |
| Pulmonary edema with diastolic dysfunction | -Beta blockers (esmolol, metoprolol, labetalol) + low-dosenitroglycerin + loop diuretic | |
| Renal situations | ||
| Hypertensive emergency with acute or chronic renal failure | -Labetalol-Nitroprusside (with caution) | Target BP 20-25% in 2-3 hours |
| Other situations | ||
| Catecholamine excess (sympathetic crisis/cocaine overdose) | -Labetalol-Verapamil, diltiazem, or nicardipine in combination with abenzodiazepine | Control paroxysms 10-15% in 1-2 hours |
| Eclampsia | -Hydralazine-Labetalol(all in conjunction with magnesium sulfate) | |
| Postoperative hypertension | -Esmolol-Labetalol | |
| Withdrawal of antihypertensive treatment | -Reinstitution of clonidine or beta blockers-Nitroprusside + IV propranolol or labetalol |
Acknowledgments
We would like to acknowledge the support we received from Canadian Hypertension Education Program task force especially Dr. Norm Campbell, Dr. Ross Feldman and Dr. Guy Tremblay for their sincere collaboration all the way through the process of development of these recommendations.
The authors would like to thank Miss Elham Khosravi, Miss Mahnaz Jozan, Miss Sonia Zarfeshani and Mr Hassan Alikhasi for Kind cooperation.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
The First Recommendation on High Blood Pressure Working Group National Committee:
Chair:Professor Feridoun Noohi
Co-chairs:Professor Nizal Sarrafzadegan, Associate Professor Alireza Khosravi
Secretary General:Dr. Elham Andalib, Professor Masoud Pourmoghaddass (Isfahan), Professor Mehdi Peighambari (Tehran), Professor Ebrahim Nematipour (Tehran), Dr.mahmood Tabandeh (Shiraz), Professor Hossein Malek Afzali (Tehran), Associate Professor Masoumeh Sadeghi (Isfahan), Associate Professor Ebrahim Kassaeian (Tehran), Associate Professor Mohammad saadatnia (Isfahan), Assistant Professor Mohammad Ostovan (Shiraz), Associate Professor Abdolrahim Ghassemi (Tehran), Associate Professor Sakineh Hajebrahimi (Tabriz), Assistant Professor Arash Rashidian (Tehran), Associate Professor Jalal Zamani (Shiraz), Assistant Professor Lili Nosrati (Tabriz), Dr. Sattar Sadeghiyan (Isfahan), Associate Professor Mojtaba Salarifar (Tehran), Professor Aliakbar Tavassoli (Isfahan), Associate Professor Mojgan Mortazavi (Isfahan), Assistant Professor Alireza Merrikhi (Isfahan), Assistant Professor Jamshid Najafian (Isfahan), Assistant Professor Bijan Iraj (Isfahan), Associate Professor Jafar Golshahi (Isfahan), Assistant Professor Shahin Shirani (Isfahan), Associate Professor Mehdi Hassanzadeh (Mashhad), Professor Mojdeh Ghabaee (Tehran), Assistant Professor Morteza Abdar (Isfahan), Assistant Professor Ahmad Assareh (Ahvaz), Professor Hassan Arefi (Tehran), Dr. Hamid Roohafza (Isfahan), Dr. Ahmad Bahonar (Isfahan), Dr. Soheila Kanani (Isfahan), Mrs. Mojgan Gharipour (Isfahan), Mrs. Nooshin Mohammadifard (Isfahan)
International Advisory Board:Professor George Fodor (Canada), Professor Norman C. Campbell (Canada), Professor Renata Cifkova (Czech Republic), Professor Kathryn Anne Taubert (USA), Dr. Sylvie Stachenko (Canada), Professor Charlotte Jones (Canada), Professor Antti Jula (Finland), Dr. Leo M. Nherera (England), Dr. Andrew Hayen (Australia)
Additional Contributors: Associate Professor Ahmad Esmailzadeh (Isfahan), Associate Professor Lila Azadbakht (Isfahan), Dr. Armin Shirani (Tehran), Mr. Hamed Dehnavi (Tehran), Dr. Fatemeh Rakhshani (Tehran), Dr. Tahereh Samavat (Tehran), Dr. Saeed Sadeghiyan (Tehran), Dr. Zahra Abdollahi (Tehran), Professor Mahmoud Momtahen (Tehran), Assistant Professor Zahra Ojaghi (Tehran), Professor Ali Haghdoost (Kerman), Professor Mohammad Hossein Mandegar (Tehran), Professor Mohammad Ali Yousefnia (Tehran)
National contributing organizations: Iranian Neurology Association, Iranian Nephrology Association, Nutrition Department, Ministry of Health and Medical Education, Technology Assessment, Standardization and Tariff for Health Services Office, Iranian Center for Evidence Based Medicine, National Institute for Health Research, Iran Endocrine Society, Iranian Society of General Physicians, Iranian Stroke Association
REFERENCES
- 1.World Health Organization . Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 2.National Heart Lung and Blood Institute. 2003. Available from: http://www.nhlbi.nih.gov/guidelines/hypertension/
- 3.Lawes CM, Vander HS, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371(9623):1513–8. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 4.Whelton PK, He J, Appel LJ, Cutler JA, Havas S, Kotchen TA, et al. Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288(15):1882–8. doi: 10.1001/jama.288.15.1882. [DOI] [PubMed] [Google Scholar]
- 5.Marik PE, Varon J. Hypertensive crises: challenges and management. Chest. 2007;131(6):1949–62. doi: 10.1378/chest.06-2490. [DOI] [PubMed] [Google Scholar]
- 6.Law M, Wald N, Morris J. Lowering blood pressure to prevent myocardial infarction and stroke: a new preventive strategy. Health Technol Assess. 2003;7(31):1–94. doi: 10.3310/hta7310. [DOI] [PubMed] [Google Scholar]
- 7.Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists' Collaboration. Lancet. 2000;356(9246):1955–64. doi: 10.1016/s0140-6736(00)03307-9. [DOI] [PubMed] [Google Scholar]
- 8.Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M, et al. Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (phase 1). Soz Praventivmed. 2002;47(6):408–26. doi: 10.1007/s000380200008. [DOI] [PubMed] [Google Scholar]
- 9.Esteghamati A, Abbasi M, Alikhani S, Gouya MM, Delavari A, Shishehbor MH, et al. Prevalence, awareness, treatment, and risk factors associated with hypertension in the Iranian population: the national survey of risk factors for noncommunicable diseases of Iran. Am J Hypertens. 2008;21(6):620–6. doi: 10.1038/ajh.2008.154. [DOI] [PubMed] [Google Scholar]
- 10.Sarrafzadegan N, Talaei M, Sadeghi M, Kelishadi R, Oveisgharan S, Mohammadifard N, et al. The Isfahan cohort study: rationale, methods and main findings. J Hum Hypertens. 2011;25(9):545–53. doi: 10.1038/jhh.2010.99. [DOI] [PubMed] [Google Scholar]
- 11.Khosravi A, Mehr GK, Kelishadi R, Shirani S, Gharipour M, Tavassoli A, et al. The impact of a 6-year comprehensive community trial on the awareness, treatment and control rates of hypertension in Iran: experiences from the Isfahan healthy heart program. BMC Cardiovasc Disord. 2010;10:61. doi: 10.1186/1471-2261-10-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nadim A, Barzegar MA, Daneshpajooh M. Comparison of the prevalence of hypertension in the rural and urban areas of Guilan Province, Northern Iran. Acta Cardiol. 1978;33(1):31–42. [PubMed] [Google Scholar]
- 13.Sarrafzadegan N, AminiNik S. Blood pressure pattern in urban and rural areas in Isfahan, Iran. J Hum Hypertens. 1997;11(7):425–8. doi: 10.1038/sj.jhh.1000448. [DOI] [PubMed] [Google Scholar]
- 14.Khosravi AR, Kelishadi R, Sarrafzadegan N, Boshtam M, Nouri F, Zarfeshani S, et al. Impact of a community-based lifestyle intervention program on blood pressure and salt intake of normotensive adult population in a developing country. J Res Med Sci. 2012;17(3):235–41. [PMC free article] [PubMed] [Google Scholar]
- 15.Zahraie M, Farzamfar B, Bayanolhagh S, Rahimi AA, Matinizadeh M, Heshmat R. The Arg16Gly polymorphism of â2-Adrenergic receptor gene and its association with hypertension in Iranian subjects. International Journal of Pharm Tech Research. 2010;2(4):2139–42. [Google Scholar]
- 16.On behalf of the Canadian Hypertension Education Program 2011 Canadian Hypertension Education Program recommendations an annual update. Canadian Family Physician. 2011;57(12):1393–139. [PMC free article] [PubMed] [Google Scholar]
- 17.Isfahan Cardiovascular Research Institute. 2012. Available from: [In Persian].
- 18.SCORE Canada. Available from: http://www.scorecanada.ca/
- 19.National Institute for Health and Clinical Evidence (NICE) Clinical Guideline 34. 2006. Available from: http://www.nice.org.uk/CG034/
- 20.Gaziano TA, Steyn K, Cohen DJ, Weinstein MC, Opie LH. Cost-effectiveness analysis of hypertension guidelines in South Africa: absolute risk versus blood pressure level. Circulation. 2005;112(23):3569–76. doi: 10.1161/CIRCULATIONAHA.105.535922. [DOI] [PubMed] [Google Scholar]
- 21.Gilani KA, Madani A, Rahimzadeh N, Esfahani S, Esfeh JM. Enalapril induced reversible acute renal failure detected by (99m) Tc-DMSA renal scan in a patient with bilateral renal artery stenosis: a case report. Cases J. 2009;2:7509. doi: 10.4076/1757-1626-2-7509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Heart Lung and Blood Institute. 2002. Available from: http://www.nhlbi.nih.gov/about/nhbpep/index.htm/
- 23.Staessen J, Fagard R, Lijnen P, Amery A. Body weight, sodium intake and blood pressure. J Hypertens Suppl. 1989;7(1):S19–S23. doi: 10.1097/00004872-198902001-00006. [DOI] [PubMed] [Google Scholar]
- 24.National Institute for Health and Clinical Excellence. Available from: http://www.nice.org.uk/
- 25.National Institutes of Health . Your Guide to Lowering Your Blood Pressure With DASH. New York: Smashbooks; 2006. [Google Scholar]
- 26.Halbert JA, Silagy CA, Finucane P, Withers RT, Hamdorf PA, Andrews GR. The effectiveness of exercise training in lowering blood pressure: a meta-analysis of randomised controlled trials of 4 weeks or longer. J Hum Hypertens. 1997;11(10):641–9. doi: 10.1038/sj.jhh.1000509. [DOI] [PubMed] [Google Scholar]
- 27.Kelishadi R, Pour MH, Sarraf-Zadegan N, Sadry GH, Ansari R, Alikhassy H, et al. Obesity and associated modifiable environmental factors in Iranian adolescents: Isfahan Healthy Heart Program - Heart Health Promotion from Childhood. Pediatr Int. 2003;45(4):435–42. doi: 10.1046/j.1442-200x.2003.01738.x. [DOI] [PubMed] [Google Scholar]
- 28.Sundstrom J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011;342:d643. doi: 10.1136/bmj.d643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, et al. Management of high blood pressure in children and adolescents: recommendations of the European Society of Hypertension. J Hypertens. 2009;27(9):1719–42. doi: 10.1097/HJH.0b013e32832f4f6b. [DOI] [PubMed] [Google Scholar]
- 30.Malekzadeh R, Mohamadnejad M, Merat S, Pourshams A, Etemadi A. Obesity Pandemic: An Iranian Perspective. Arch Iranian Med. 2005;8(1):1–7. [Google Scholar]
- 31.Naghavi M. Etiology of death in 18 provinces of Iran in year 2001. Tehran, Iran: Deputy for Health, Ministry of Health and Medical Education Iran; 2001. p. 75. [Google Scholar]
- 32.Mirzazadeh A, Sadeghirad B, Haghdoost AA, Bahrein F, Rezazadeh Kermani M. The Prevalence of Obesity in Iran in Recent Decade; a Systematic Review and Meta-Analysis Study. Iran J Public Health. 2009;38(3):1–11. [Google Scholar]
- 33.Barzigar A, Shojaei Tehrani H. Prevalence of atherosclerosis risk factors in Sowme Sara district of Gilan in 1996. J Kerman Univ Med Sci. 1997;4(4):182–9. [Google Scholar]
- 34.Ghorbani R, Nazari A. Prevalence of obesity and some factors associated with in Semnan population aged 20-55 years. Koomesh. 2000;1(2):19–24. [Google Scholar]
- 35.Mojibian M, Ghilian Z. Prevalence of obesity among women in Yazd city in. 2000. J Shaheed Sadoughi Univ Med Sci. 2001;9(4):36–42. [Google Scholar]
- 36.Sazavar SH, Mohammadi MA. Obesity prevalence and its relation with some cardiovascular risk factors in ardabil city in 2000. J Ardabil Univ Med Sci. 2002;1(2):21–6. [Google Scholar]
- 37.Gheibi SS, Fakoor Z, Alizadegan M, Pashpour N, Hamzenejad A, Mohadesi H. The prevalevce of obesity among girl students in Urmia in 2002-3. Iran J Pediatr. 2003;13 [Google Scholar]
- 38.Karandish M, Mohammadpour Ahranjani B, Kalantari N, Eshraghian Mr, Rashidi MA. Prevalence of Overweight and Obesity among Adolescent Students, 1999-2000 in Tehran. Hakim. 2004;7(3):38–43. doi: 10.1079/phn2003593. [DOI] [PubMed] [Google Scholar]
- 39.Rahmati F, Moghadass Tabrizi Y, Shidfar F, Habibi F, Jafari MR. Prevalence of obesity and hypertension among Tehran University students. J Kerman Univ Med Sci. 2004;3(2):123–30. [Google Scholar]
- 40.Tavassoli A, Gharipour M, Toghianifar N, Sarrafzadegan N, Khosravi A, Zolfaghari B, et al. The impact of obesity on hypertension and diabetes control following healthy Lifestyle Intervention Program in a developing country setting. J Res Med Sci. 2011;16 (Suppl 1):S368. [PMC free article] [PubMed] [Google Scholar]
- 41.Bramlage P, Pittrow D, Wittchen HU, Kirch W, Boehler S, Lehnert H, et al. Hypertension in overweight and obese primary care patients is highly prevalent and poorly controlled. Am J Hypertens. 2004;17(10):904–10. doi: 10.1016/j.amjhyper.2004.05.017. [DOI] [PubMed] [Google Scholar]
- 42.Romero R, Bonet J, De La Sierra A, Aguilera MT. Undiagnosed obesity in hypertension: clinical and therapeutic implications. Blood Press. 2007;16(6):347–53. doi: 10.1080/08037050701715117. [DOI] [PubMed] [Google Scholar]
- 43.Kapa S, Sert Kuniyoshi FH, Somers VK. Sleep apnea and hypertension: interactions and implications for management. Hypertension. 2008;51(3):605–8. doi: 10.1161/HYPERTENSIONAHA.106.076190. [DOI] [PubMed] [Google Scholar]
- 44.Varon J, Marik PE. Clinical review: the management of hypertensive crises. Crit Care. 2003;7(5):374–84. doi: 10.1186/cc2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Who Is at Risk? The National Heart Lung and Blood Institute. 2012. Available from: http://www.nhlbi.nih.gov/health/dci/Diseases/Hbp/HBP_WhoIsAtRisk.html/
- 46.How Can High Blood Pressure Be Prevented? TheNational Heart Lung and Blood Institute, Diseases and Conditions Index: High Blood Pressure. 2006. Available from: http://www.nhlbi.nih.gov/health/dci/Diseases/Hbp/HBP_Prevention.html/